Abstract
Objectives
To compare the repeatability of Cone Location and Magnitude Index expanded (CLMI.X) parameters of 2 mm diameter zone of greatest corneal curvature (Cspot-Axi) and 1 mm diameter zone of thinnest pachmymetry (Spot-Pach) with the maximum single point keratometry (Kmax), 3 mm Zonal Kmax (Z-Kmax3), and thinnest single point pachymetry (TP) in keratoconus (KC).
Methods
In this Comparative repeatability study, data from 36 eyes of 36 normal individuals and 72 eyes of 72 KC patients (28 eyes with ≤50.0D and 44 eyes with >50.0D Z-Kmax3) were analyzed. For each enrolled eye, imaging was done 6 times (3 consecutive acquisitions with a half hour break). For each parameter, the within-subject standard deviation (Sw) was calculated from the data of the six exams.
Results
In the normal group, Cspot-Axi-Sw was different from Kmax-Sw (p = 0.0004). Also, Z-Kmax3-Sw was different from Kmax-Sw (p = 0.0297). The difference between Cspot-Axi-Sw and Z-Kmax3-Sw was statistically significant (p = 0.0482). In the KC group, Sw were significantly different between Cspot-Axi and Kmax (p < 0.0001), and between Z-Kmax3 and Kmax (p < 0.0001). In the Z-Kmax3 ≤ 50.0D subgroup, Sw were different between Cspot-Axi and Kmax (p = 0.0002). In the Z-Kmax3 > 50.0D subgroup, Sw were different between Cspot-Axi and Kmax (p < 0.0001), and between Z-Kmax3 and Kmax (p < 0.0001). Sw differences between Spot-Pach and TP were not significant in any of the study groups (all P > 0.05).
Conclusions
In the diagnosis and follow up of KC, the zonal averages of Cspot-Axi and Z-Kmax3 are more reliable than the single point Kmax. The repeatability of Spot-Pach is similar to TP and both variables should suit the purpose equally.
Subject terms: Diseases, Medical research
Introduction
Keratoconus (KC) is a corneal ectatic condition that manifests as progressive corneal thinning and steepening [1]. Corneal curvature and thickness values are important parameters for KC diagnosis, they are measured in different manners in that thickness is normal to the surface [2], and curvature may be measured for the anterior and posterior surfaces of the cornea. Single-point indices such as maximum keratometry (Kmax) and thinnest pachymetry (TP) are routinely used in the diagnosis of KC and early KC to prevent post refractive surgery ectasia [3, 4]. State-of-the-art imaging devices perform 3-dimensional mapping of these indices rather than providing single-point estimates to optimize their diagnostic ability [5]. These novel indices include the 3, 4, and 5 mm zonal Kmax, the pachymetric progression index, and the Ambrósio relational thickness [6], as well as the 2 mm zonal average curvature of Cspot [7].
Studies in normal subjects have shown good repeatability for single-point indices such as Kmax and TP [8, 9]. However, there is concern regarding their repeatability in KC subjects, especially in more advanced cases of the disease, such that that measurement repeatability decreases as the severity of the disease increases [10]. This has important implications, not only in the diagnosis of disease, but also monitoring the effectiveness of treatments such as corneal cross-linking (CXL). In a pilot study of CXL failure and success in young Down syndrome patients, we found that the zonal Kmax in the 3 mm area around Kmax (Z-Kmax3) is a more reliable index for the assessment of results than the Kmax which reflects the maximum curvature as a single point of measurement, and changed the conclusions of the study [11].
The Cone Location and Magnitude Index (CLMI) is a robust index developed and expanded (CLMI.X) by the Collaborative Longitudinal Evaluation of Keratoconus Study group to extend the capabilities of The Ohio State University Corneal Topography Tool (OSUCTT) which is software for processing topographic data from multiple topographic machines [7, 12, 13] in a similar manner to minimize device-specific issues such as spatial resolution. The CLMI.X finds the area-corrected average steepest 2-mm-diameter circle (Cspot) by searching the central 8 mm region and compares that area to the rest of the map to determine whether the steepest area represents a cone. To the best of our knowledge, the repeatability of CLMI.X parameters has not yet been compared to other zonal and single-point indices.
In this study, the repeatability of Cspot from CLMI.X applied to axial curvature and thickness parameters was determined and compared with Kmax, Z-Kmax3, and TP in normal and KC subjects. Furthermore, to study the effect of KC stage, the variability of these parameters was evaluated in two KC groups with Z-Kmax3 ≤ 50.0D and >50.0 D.
Methods
Patients and sampling
This cross-sectional study was conducted in 2020 at Noor Ophthalmology Hospital in Tehran, Iran. Normal subjects were recruited from those on the waiting list for elective refractive surgery and had no signs of ectasia. Participants in the KC group were patients from the Keratoconus Clinic who had a diagnosis of definite KC. The inclusion criteria were age between 20 and 40 years and having no history of corneal surgery, corneal scarring, or pterygium. From each participant, only one eye was enrolled in the study. In unilateral KC cases, the eye with definitive KC was selected. In normal and bilateral KC cases, random selection was applied.
Ethical considerations
The protocol of this study was approved by the Ethics Committee of Tehran University of Medical Sciences (IR.TUMS.MEDICINE.REC.1400.622), and the tenets of the Helsinki Declaration were adhered to at all steps. The objectives and methods of the study were explained to the participants, and they signed informed consents before enrolment.
Examinations
In addition to routine diagnostic tests, participants underwent imaging with Pentacam HR (Oculus Optikgeräte GmbH, Wetzlar, Germany). All images were acquired between 8 AM and 1 PM by the same optometrist. The participants were first seated in a room with mesopic light conditions for 10 min. After moving to the device, they were asked to focus on the blue fixation light in the centre and to blink several times right before imaging was done. To evaluate the repeatability, three images were acquired from the enrolled eye without moving the head, and the same steps were repeated half an hour later. Only photos with quality specification displayed as “OK” (minimum valid data: 93.0%) were accepted.
Indices
From each exam, the KMax, Z-Kmax3, and TP were extracted from Pentacam outputs. The raw data files (U12) of all exams were also imported to OSUCTT to calculate CLMI.X parameters of Cspot in Axial Curvature (Cspot-Axi) which represents the average steepest curvature value in a 2 mm diameter region on the anterior axial map and the Spot Pachymetry (Spot-Pach) which is the average thinnest pachymetry in a 1 mm diameter region on the pachymetry map [13]. To characterize corneas in this sample, in addition to main indices, we used indices for the assessment of keratoconus including Fourier irregularity, Belin Ambrósio display-total deviation (BAD-D), maximum Ambrósio’s relational thickness (ART-max), inferior-superior asymmetry (I-S value), index of surface variance (ISV), index of vertical asymmetry (IVA), keratoconus index (KI), centre keratoconus index (CKI), index of height asymmetry (IHA), and index of height decentration (IHD). The Fourier irregularity index is a measure of corneal irregularity that is based on wave components that cannot be corrected with sphere, cylinder, or, prism, and they may require rigid contact lenses when high.
Statistical Analysis
KC cases were further sub-grouped by severity using a 50.0 D threshold for Z-Kmax3. The repeatability of the five parameters of interest was determined in each group and subgroup. First, we used the test-retest method and determined intraclass correlation coefficients (ICC) which can demonstrate reproducibility by comparing the mean and variance of a repeated test. However, this test is a unitless value, and even with adequate ICC, there may be clinically significant differences in repeatability that are important in evaluating single patients. Therefore, for each of the five parameters, two new variables were calculated using the data of the six exams per eye: all exam average (avg) and within-subject standard deviation (Sw). The Sw of the curvature parameters (Cspot-Axi, Z-Kmax3, and Kmax) and the thickness parameters (Spot-Pach and TP) were compared using repeated measures ANOVA. A contrast profile was used to determine if Cspot-Axi-Sw was different from Z-Kmax3-Sw and if Z-Kmax3-Sw was different from Kmax-Sw. Lastly, Bland-Altman plots were produced to visualize the repeatability of the parameters.
Results
Data from 108 eyes under study were analysed from 36 normal individuals and 72 eyes from 72 KC patients (28 eyes in the Z-Kmax3 ≤ 50.0D subgroup and 44 eyes in the Z-Kmax3 > 50.0D subgroup). Comparison of the demographic, vision, refraction, and tomography indices are summarized in Table 1. All indices were significantly different between normal and KC subgroups (all P < 0.001), except gender and age (both P > 0.05). The range of Fourier irregularity index was 0.008 to 0.042 in the normal group, 0.010 to 0.183 in the KC Z-Kmax3 ≤ 50.0D subgroup, and 0.013 to 0.140 in the KC Z-Kmax3 > 50.0D subgroup.
Table 1.
Demographic, vision, refraction, and tomographic parameters in the three study groups.
| Normal group | Keratoconus group | ||
|---|---|---|---|
| Z-Kmax3 ≤ 50.0D | Z-Kmax3 > 50.0D | ||
| Number of eyes | 35 | 28 | 44 |
| Age (year) | 27.80 ± 6.08 | 33.12 ± 5.27 | 32.48 ± 7.04 |
| Gender (% female) | 43.3% | 53.8% | 34.8% |
| UDVA (LogMar) | 0.88 ± 0.42 (~20/150) | 0.70 ± 0.55 (~20/100) | 1.07 ± 0.50 (~20/250) |
| CDVA (LogMar) | 0.00 ± 0.02 (~20/20) | 0.15 ± 0.22 (~20/30) | 0.44 ± 0.31 (~20/60) |
| SE (D) | −2.59 ± 1.57 | −3.40 ± 2.61 | −7.12 ± 2.95 |
| Astigmatism (D) | −0.81 ± 0.59 | −3.17 ± 1.75 | −5.11 ± 2.43 |
| BAD-D | 1.18 ± 0.72 | 5.61 ± 7.09 | 11.60 ± 7.54 |
| ART-max (µm) | 427.00 ± 82.84 | 230.44 ± 103.77 | 135.65 ± 48.90 |
| Fourier irregularity | 0.016 ± 0.006 | 0.027 ± 0.024 | 0.035 ± 0.019 |
| I-S value (D) | 0.20 ± 0.56 | 2.41 ± 2.10 | 6.62 ± 3.68 |
| ISV | 16.97 ± 4.84 | 47.46 ± 15.54 | 100.07 ± 33.35 |
| IVA | 0.11 ± 0.05 | 0.45 ± 0.25 | 0.96 ± 0.37 |
| KI | 1.02 ± 0.02 | 1.09 ± 0.06 | 1.25 ± 0.13 |
| CKI | 1.01 ± 0.01 | 1.02 ± 0.02 | 1.08 ± 0.06 |
| IHA | 5.09 ± 4.87 | 18.37 ± 14.62 | 34.70 ± 24.74 |
| IHD | 0.01 ± 0.01 | 0.05 ± 0.03 | 0.14 ± 0.06 |
Z-Kmax3 mean keratometry in the 3-mm zone around the anterior steepest point, UDVA uncorrected distance visual acuity, CDVA corrected distance visual acuity, SE spherical equivalent, D dioptre, BAD-D Belin Ambrósio display-total deviation, ART-max maximum Ambrósio’s relational thickness, I-S value inferior-superior asymmetry, ISV index of surface variance, IVA index of vertical asymmetry, KI keratoconus index, CKI centre keratoconus index, IHA index of height asymmetry, IHD index of height decentration.
Repeatability of keratometry parameters
The ICC range was above 0.96 to 1.00 with narrow CI (range: 0.96 to 1.00) for all indices in the normal group and KC subgroups.
In the normal group, Cspot-Axi-Sw was different from Kmax-Sw (0.129 vs. 0.195, p = 0.0004). Also, Z-Kmax3-Sw was different from Kmax-Sw (0.149 vs. 0.195, p = 0.0297). The difference between Cspot-Axi-Sw and Z-Kmax3-Sw was statistically significant (p = 0.0482) (Table 2), but not clinically relevant with a mean difference of 0.019 Dioptres.
Table 2.
Mean, within-subject standard deviation (Sw), and the 95% confidence limit (CL) of Sw indices for normal and keratoconus (KC) group.
| Group | Variable | N | Mean | Minimum | Maximum | Std Dev | Variable | N | Sw | Lower CL | Upper CL |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Normal | Cspot-Axi-avg | 35 | 44.30 | 40.90 | 47.43 | 1.43 | Cspot-Axi-Sw | 35 | 0.129 | 0.076 | 0.183 |
| Z-Kmax3-avg | 35 | 44.10 | 40.56 | 47.11 | 1.43 | Z-Kmax3-Sw | 35 | 0.149 | 0.096 | 0.201 | |
| Kmax-avg | 35 | 44.63 | 41.09 | 47.96 | 1.43 | Kmax-Sw | 35 | 0.195 | 0.117 | 0.272 | |
| TP-avg | 35 | 534.08 | 458.00 | 616.33 | 41.66 | TP-Sw | 35 | 2.535 | 2.063 | 3.008 | |
| Spot-Pach-avg | 35 | 535.21 | 459.16 | 617.55 | 41.72 | Spot-Pach-Sw | 35 | 2.515 | 2.037 | 2.993 | |
| KC | Cspot-Axi-avg | 72 | 53.28 | 44.24 | 75.11 | 5.94 | Cspot-Axi-Sw | 72 | 0.222 | 0.185 | 0.258 |
| Z-Kmax3-avg | 72 | 52.46 | 43.60 | 73.51 | 5.69 | Z-Kmax3-Sw | 72 | 0.223 | 0.193 | 0.254 | |
| Kmax-avg | 72 | 54.98 | 44.77 | 78.65 | 6.79 | Kmax-Sw | 72 | 0.347 | 0.293 | 0.400 | |
| TP-avg | 72 | 456.06 | 171.17 | 560.17 | 56.63 | TP-Sw | 72 | 3.260 | 2.578 | 3.937 | |
| Spot-Pach-avg | 72 | 459.62 | 231.83 | 561.35 | 52.16 | Spot-Pach-Sw | 72 | 3.220 | 2.514 | 3.924 |
Cspot-Axi average steepest curvature value in a 2 mm diameter region on the anterior axial map, Z-Kamx3 mean keratometry in the 3-mm zone around the anterior steepest point, TP thinnest pachymetry, Spot-Pach average thinnest pachymetry in a 1mm diameter region on the pachymetry map, avg average, std Dev standard deviation.
In the KC group, Cspot-Axi-Sw was different from Kmax-Sw (0.222 vs. 0.347, p < 0.0001), and Z-Kmax3-Sw was different from Kmax-Sw (0.223 vs. 0.347, p < 0.0001). The difference between Cspot-Axi-Sw and Z-Kmax3-Sw was not significant (p = 0.8564) (Table 2).
In the KC subgroup with Z-Kmax3 ≤ 50.0 D, Cspot-Axi-Sw was different from Kmax-Sw (0.142 vs. 0.200, p = 0.0002), but Z-Kmax3-Sw (0.164) was not different from Kmax-Sw (0.200), and the difference between Cspot-Axi-Sw and Z-Kmax3-Sw was statistically significant (p = 0.0481) (Table 3), but not clinically relevant with a mean difference of 0.023 Dioptres.
Table 3.
Means, within-subject standard deviation (Sw), and the 95% confidence limit (CL) of Sw indices for low grade of keratoconus (Z-Kmax3 ≤ 50.0D) and high grade of keratoconus (Z-Kmax3 > 50.0D) group.
| Subgroup | Variable | N | Mean | Minimum | Maximum | Std Dev | Variable | N | Sw | Lower CL | Upper CL |
|---|---|---|---|---|---|---|---|---|---|---|---|
| ≤50.0 | Cspot-Axi-avg | 28 | 48.25 | 44.24 | 51.40 | 1.77 | Cspot-Axi-Sw | 28 | 0.142 | 0.110 | 0.173 |
| Z-Kmax3-avg | 28 | 47.72 | 43.60 | 49.81 | 1.69 | Z-Kmax3-Sw | 28 | 0.164 | 0.131 | 0.198 | |
| Kmax-avg | 28 | 49.15 | 44.77 | 53.34 | 2.07 | Kmax-Sw | 28 | 0.200 | 0.154 | 0.247 | |
| TP-avg | 28 | 480.20 | 297.17 | 560.17 | 49.51 | TP-Sw | 28 | 2.430 | 1.633 | 3.218 | |
| Spot-Pach-avg | 28 | 482.39 | 302.35 | 561.35 | 48.98 | Spot-Pach-Sw | 28 | 2.380 | 1.639 | 3.122 | |
| >50.0 | Cspot-Axi-avg | 44 | 56.48 | 50.67 | 75.11 | 5.41 | Cspot-Axi-Sw | 44 | 0.272 | 0.221 | 0.323 |
| Z-Kmax3-avg | 44 | 55.47 | 50.22 | 73.51 | 5.28 | Z-Kmax3-Sw | 44 | 0.261 | 0.218 | 0.304 | |
| Kmax-avg | 44 | 58.69 | 51.40 | 78.65 | 6.11 | Kmax-Sw | 44 | 0.440 | 0.370 | 0.509 | |
| TP-avg | 44 | 440.7 | 171.17 | 512.67 | 56.00 | TP-Sw | 44 | 3.788 | 2.805 | 4.770 | |
| Spot-Pach-avg | 44 | 445.1 | 231.83 | 515.62 | 49.32 | Spot-Pach-Sw | 44 | 3.753 | 2.708 | 4.797 |
Cspot-Axi average steepest curvature value in a 2 mm diameter region on the anterior axial map, Z-Kamx3 mean keratometry in the 3-mm zone around the anterior steepest point, TP thinnest pachymetry, Spot-Pach average thinnest pachymetry in a 1 mm diameter region on the pachymetry map, avg average, std Dev standard deviation.
In the KC subgroup with Z-Kmax3 > 50.0 D, Cspot-Axi-Sw was different from Kmax-Sw (0.272 vs. 0.440, p < 0.0001), Z-Kmax3-Sw was different from Kmax-Sw (0.261 vs. 0.440, p < 0.0001), but the difference between Cspot-Axi-Sw and Z-Kmax3-Sw was not significant (p = 0.4425) (Table 3).
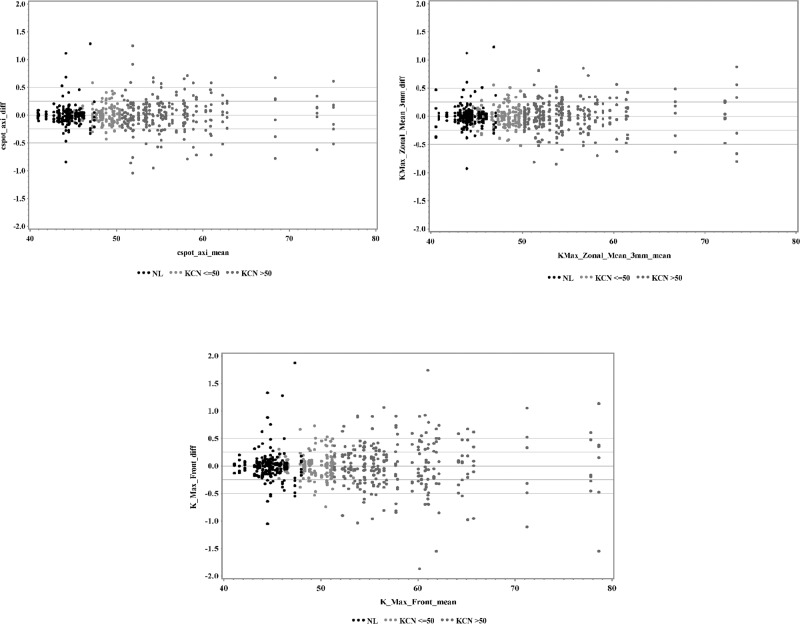
Bland-Altman plots for the repeatability of Cspot-Axi, Z-Kmax3, and Kmax are illustrated in Fig. 1. Less variation is observed for Cspot-Axi and Z-Kmax3 compared to Kmax.
Fig. 1. Repeatabilty of different types of keratometric indices in normal (NL) eye, keratoconus (KC) eyes with Z-Kmax3 ≤ 50.0D and KC eyes with Z-Kmax3 > 50.0D.
Cspot-Axi: average steepest curvature value in a 2 mm diameter region on the anterior axial map (upper left); Kmax_zonal_Mean_3 mm/Z-Kmax3: mean keratometry in the 3-mm zone around the anterior steepest point (upper right); K-Max_Front: anterior maximum keratometry (lower).
Thickness repeatability
The ICC range for both indices was 0.99 to 1.00 with a narrow CI (range: 0.98 to 1.00), in the normal group and KC subgroups. The difference between Spot-Pach-Sw and TP-Sw was not significant in any of the study groups (normal and KC subgroups) (all P > 0.05) (Tables 2 and 3). Bland-Altman plots for these indices are provided in Fig. 2.
Fig. 2. Repeatabilty of pachymetric indices in normal (NL) eye, keratoconus (KC) eyes with Z-Kmax3 ≤ 50.0 D and KC eyes with Z-Kmax3 > 50.0 D.
Spot_pach: average thinnest pachymetry in a 1 mm diameter region on the pachymetry map (left); Thinnest pachy: thinnest pachymetry (right).
Discussion
Two important considerations are due in regard to KC. One is the diagnosis of disease progression which determines the need for CXL, and the other is assessing the effectiveness or failure of CXL to decide on the next plan of action. Typically, disease progression and CXL failure are defined based on a 1.0D increase in Kmax [14] or 20.0% reduction in the thinnest pachymetry [15]. Despite advances in diagnostic ability, there is still debate about the clinically acceptable range for these two main indices, because the repeatability of these single-point measurements is questionable in irregular corneas. Studies have shown that the size of the measurement zone affects repeatability [16]. In addition to the position of Kmax (y-coordinate), fixation, composition and distribution of the tear film, and misalignment [17, 18], the effect can vary by corneal irregularities (peaks and troughs of the cornea) in more severe cases of the disease [16]. Therefore, if measurements are averaged over a given diameter instead of a single point, repeatability of measurements is higher.
CLMI.X parameters were introduced and expanded to allow KC detection. CLMI.X indicates asymmetry between Cspot-Axi and the equivalent 180 degrees from the location of Cspot-Axi. CLMI.X includes parameters, Cspot and Spot-Pach that describes the steepest and thinnest area of the cornea in a certain diameter (2.0 mm for curvature and 1.0 mm for thickness), respectively [13]. In contrast, for zonal average indices, the steepest single point is first identified, and then the average is determined for the surrounding area [19]. For CLMI.X, in addition to analysing the anterior surface of the cornea, posterior surface data and corneal thickness are incorporated, and the sensitivity, specificity, and accuracy of KC diagnosis is improved to 89.2%, 98.8%, and 95.0% [13]. In this study, CLMI.X parameters were compared with zonal average Kmax and single-point Kmax for the first time, but instead of mean, within subject std was used to directly compare the repeatability of the indices.
Although the ICCs indicated excellent repeatability for all three indexes in the normal and KC groups, this is not necessarily translated to clinical interpretation for individual subjects, and Sw pointed to different results. Given that the ICC is calculated using the formula (Sb2 − Sw2)/SD2, where Sb is the between-subject standard deviation and Sw is the within-subject standard deviation [20], the smaller the Sw, the larger the ICC. In other words, the ICC is influenced by the distribution of the variable and Sw. But Sw indicates the variance of the variable in repeated measurements, and thus, it suits our purpose better. Another advantage is that Sw is easier to interpret clinically. For example, in the present study, Sw shows what part of the changes observed in the index is related to measurement error and what part is due to KC progression. In a study Asroui et al. [16] the Sw for 3 repeated measurements of Z-Kmax3 was 0.33 and 0.67 in their ≤50.0D and >50.0D groups, respectively. In our study, these figures were respectively 0.164 and 0.261 for 6 repeated measurements. The inter-study difference could be due to the number of repetitions as well as differences in the degree of corneal irregularity in the samples of the two studies. As shown in Table 1, as the degree of irregularity increases from normal to more advanced forms of KC, the Sw for all three indices increases as well.
Based on Sw, in both normal and KC subjects, the repeatability of Cspot-Axi and Z-Kmax3 was similarly better than Kmax. As shown in Table 2, as the degree of irregularity increases, the gap between the Sw of these two indexes and the Sw of Kmax increases as well. Theoretically, calculating the average of multiple points, as is done for in zonal averages, reduces the random error of a single point measurement. From a clinical point of view, the repeatability of zonal and single-point indices is different beyond an area of 0.5 mm in diameter [16]. The similarity between the two CLMI.X indices and zonal keratometry can be due to precise localization of the steepest zone or similar corneal irregularity in 2 and 3 mm diameters on the axial map.
No differences were detected between the average zonal values of Spot-Pach and the single-point value of TP for any study group. The difference between pachymetry and curvature is that curvature is a second-derivative function and therefore more sensitive to noise than pachymetry which is based on anterior and posterior elevation. Evaluating zonal averages for curvature eliminates the influence of random noise, which according to our study results, is not necessary for pachymetry.
One limitation of this study is that the sample did not comprise cases of progressive KC with six- or twelve-month monitoring, but cross-sectional patient data was used instead. Performing this study with longitudinal data could aid interpretation. Nonetheless, our results show the contribution of measurement repeatability. Since the overall observed changes include actual disease progression and measurement repeatability, accounting for the latter can reveal changes related to disease progression.
In conclusion, Cspot-Axi and Z-Kmax3 are more reliable indices for the diagnosis of KC progression than single point Kmax in cases with Fourier irregularity in the range of 0.01 to 0.14, and are more suitable in diagnosis of disease progression. It is recommended that they be used instead of Kmax, since it has been shown that conclusions of studies may be altered [10]. Since these indices are independent of the platform, they can be used with any tomographic device. The repeatability of Spot-Pach (smaller Sw for Spot-Pach) was not statistically significant and both variables detect KC and its progression similarly.
Summary
What was known before
Single point Kmax is a reliable index in the diagnosis of KC and KC progression.
Thinnest pachymetry is a reliable index in the diagnosis of KC and KC progression.
What this study adds
In the diagnosis and follow up of keratoconus:
Cspot-Axi is more reliable than Z-Kmax3.
Z-Kmax3 is more suitable than single-point Kmax.
Both Spot-Pach and thinnest pachymetry have equal diagnostic value.
Author contributions
Concept and design (HH, CJR), acquisition of data (HH, SA), statistical analysis (AMM), interpretation of result (HH, CJR, SM, and SA), drafting the manuscript (SA, CJR, and SM), critical revision and final approve (all authors).
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Competing interests
CJR is consultant for Oculus Optikgeräte GmbH and Ziemer Ophthalmic Systems AG, Germany. None of the remaining authors have any financial disclosures.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Gomes JA, Tan D, Rapuano CJ, Belin MW, Ambrósio R, Jr., Guell JL, et al. Global consensus on keratoconus and ectatic diseases. Cornea. 2015;34:359–69. doi: 10.1097/ICO.0000000000000408. [DOI] [PubMed] [Google Scholar]
- 2.Roberts. Error in the estimation of ablation centration using pachymetric difference maps. J Refract Surg. 2015;31:138–9. doi: 10.3928/1081597X-20150122-10. [DOI] [PubMed] [Google Scholar]
- 3.Miraftab M, Fotouhi A, Hashemi H, Jafari F, Shahnazi A, Asgari S. A modified risk assessment scoring system for post laser in situ keratomileusis ectasia in topographically normal patients. J Ophthalmic Vis Res. 2014;9:434–8. doi: 10.4103/2008-322X.150806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Randleman JB, Russell B, Ward MA, Thompson KP, Stulting RD. Risk factors and prognosis for corneal ectasia after LASIK. Ophthalmology. 2003;110:267–75. doi: 10.1016/S0161-6420(02)01727-X. [DOI] [PubMed] [Google Scholar]
- 5.Piñero DP, Nieto JC, Lopez-Miguel A. Characterization of corneal structure in keratoconus. J Cataract Refrct Surg. 2012;38:2167–83. doi: 10.1016/j.jcrs.2012.10.022. [DOI] [PubMed] [Google Scholar]
- 6.Ambrosio R, Jr., Caiado AL, Guerra FP, Louzada R, Sinha RA, Luz A, et al. Novel pachymetric parameters based on corneal tomography for diagnosing keratoconus. J Refract Surg. 2011;27:753–8. doi: 10.3928/1081597X-20110721-01. [DOI] [PubMed] [Google Scholar]
- 7.Mahmoud AM, Roberts CJ, Lembach RG, Twa MD, Herderick EE, McMahon TT, CLEK Study Group. CLMI: the cone location and magnitude index. Cornea. 2008;27:480–7. doi: 10.1097/ICO.0b013e31816485d3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Crawford AZ, Patel DV, McGhee CNJ. Comparison and repeatability of keratometric and corneal power measurements obtained by Orbscan II, Pentacam, and Galilei corneal tomography systems. Am J Ophthalmol. 2013;156:53–60. doi: 10.1016/j.ajo.2013.01.029. [DOI] [PubMed] [Google Scholar]
- 9.Guber I, McAlinden C, Majo F, Bergin C. Identifying more reliable parameters for the detection of change during the follow-up of mild to moderate keratoconus patients. Eye Vis. 2017;4:24. doi: 10.1186/s40662-017-0089-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hashemi H, Yekta A, Khabazkhoob M. Effect of keratoconus grades on repeatability of keratometry readings: Comparison of 5 devices. J Cataract Refract Surg. 2015;41:1065–72. doi: 10.1016/j.jcrs.2014.08.043. [DOI] [PubMed] [Google Scholar]
- 11.Hashemi H, Asgari S, Roberts CJ. Zonal Kmax Is More Reliable Than Single-Point Kmax. J Refract Surg. 2021;37:286–7. doi: 10.3928/1081597X-20210204-02. [DOI] [PubMed] [Google Scholar]
- 12.Mahmoud AM, Roberts C, Henderick EE. The Ohio State University Corneal Topography Tool. Investig Ophthalmol Vis Sci. 2000;41:S677. [Google Scholar]
- 13.Mahmoud AM, Nuñez MX, Blanco C, Koch DD, Wang L, Weikert MP, et al. Expanding the cone location and magnitude index to include corneal thickness and posterior surface information for the detection of keratoconus. Am J Ophthalmol. 2013;156:1102–11. doi: 10.1016/j.ajo.2013.07.018. [DOI] [PubMed] [Google Scholar]
- 14.Ferdi AC, Nguyen V, Gore DM, Allan BD, Rozema JJ, Watson SL. Keratoconus natural progression: a systematic review and meta-analysis of 11 529 eyes. Ophthalmology. 2019;126:935–45. doi: 10.1016/j.ophtha.2019.02.029. [DOI] [PubMed] [Google Scholar]
- 15.Burns DM, Johnston FM, Frazer DG, Patterson C, Jackson AJ. Keratoconus: an analysis of corneal asymmetry. Br J Ophthalmol. 2004;88:1252–5. doi: 10.1136/bjo.2003.033670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Asroui L, Mehanna CJ, Salloum A, Chalhoub RM, Roberts CJ, Awwad ST. Repeatability of Zone Averages Compared to Single-Point Measurements of Maximal Curvature in Keratoconus. Am J Ophthalmol. 2021;221:226–34. doi: 10.1016/j.ajo.2020.08.011. [DOI] [PubMed] [Google Scholar]
- 17.Hick S, Laliberté JF, Meunier J, Chagnon M, Brunette I. Effects of misalignment during corneal topography. J Cataract Refract Surg. 2007;33:1522–9. doi: 10.1016/j.jcrs.2007.05.029. [DOI] [PubMed] [Google Scholar]
- 18.Miháltz K, Kránitz K, Kovács I, Takács A, Németh J, Nagy ZZ. Shifting of the line of sight in keratoconus measured by a hartmann-shack sensor. Ophthalmology. 2010;117:41–48. doi: 10.1016/j.ophtha.2009.06.039. [DOI] [PubMed] [Google Scholar]
- 19.Kreps EO, Jimenez-Garcia M, Issarti I, Claerhout I, Koppen C, Rozema JJ. Repeatability of the Pentacam HR in Various Grades of Keratoconus. Am J Ophthalmol. 2020;219:154–62. doi: 10.1016/j.ajo.2020.06.013. [DOI] [PubMed] [Google Scholar]
- 20.Liljequist D, Elfving B, Skavberg Roaldsen K. Intraclass correlation—a discussion and demonstration of basic features. PLoS One. 2019;14:e0219854. doi: 10.1371/journal.pone.0219854. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.