Abstract
Introduction
Health education, as a crucial strategic measure of disease prevention and control in the 21st century, has become an important part of healthcare. As the main deliverers of patient health education, nursing personnel’s patient health education competence (PHEC) has received much attention. Instruments for assessing the PHEC of nursing personnel have been developed internationally, but there is a lack of systematic reviews and evaluations of the psychometric properties of these instruments. To effectively select appropriate PHEC assessment instruments in specific contexts, a systematic and comprehensive review and evaluation of these measurement instruments are needed. The goal of this systematic review is to systematically evaluate the psychometric properties of existing PHEC instruments.
Methods and analysis
In this study, eight databases will be searched between 1 March 2023 and 31 2023 to retrieve studies that include instrument(s) measuring the PHEC of nursing personnel. Two researchers will independently perform literature screening, data extraction and literature evaluation. In case of disagreement, a third researcher will be involved in the resolution. The measurement properties of PHEC assessment instruments will be systematically reviewed based on the consensus-based standards for the selection of health measurement instruments (COMSIN) methodology and guideline.
Ethics and dissemination
Ethical approval is not applicable for this study. We will share the findings from the study at national and/or international conferences and in a peer-reviewed journal in the fields of health education and/or patient education.
PROSPERO registration number
CRD42023393293.
Keywords: Health Education, PUBLIC HEALTH, Primary Health Care, Nurses
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The Preferred Reporting Items for Systematic reviews and Meta-analyses protocols (PRISMA-P) 2015 checklist and the Preferred Reporting Items for Systematic reviews and Meta-analyses (PRISMA) 2020 checklist will be used to guide the reporting of the protocol and systematic review, respectively.
The consensus-based standards for the selection of health measurement instruments (COSMIN) methodology will be used to evaluate the methodological quality of included studies on measurement properties of the instruments and the quality of included instruments.
The systematic review may fail to include relevant literature published outside of the searched databases.
Introduction
Health education has been identified by the WHO as one of the three crucial strategic measures of disease prevention and control in the 21st century, and it is the most economical and effective measure for improving public health.1 Health education for patients can improve their understanding of their own health status and disease management measures, which can relieve patients’ anxiety and improve their compliance and satisfaction with medical staff, thus improving their health status and quality of life.2 These better patient outcomes could reduce the burden of disease on patients and society at the economic level.3 4 As the world’s largest group of health professionals and the health professionals who have the closest contact with patients, nursing staff plays an important role in patient health education.3 5 Nurses often develop profound connections with their patients, rendering them optimal conveyors of health information and proponents of constructive behavioural transformations.6 Their consistent and sustained patient interactions afford them an intimate grasp of individual needs, preferences and hurdles, enabling the delivery of tailored patient health education that accommodates these divergent factors.6 7 This education encompasses instructing patients on health preservation, preventive measures and autonomous health management. Consequently, patients are empowered to make enlightened choices and enhance compliance with treatment regimens. Functioning as integral healthcare team members, nurses proficiently facilitate intercommunication among patients, physicians and allied healthcare professionals.8 Their adeptness at translating medical jargon and disseminating information empowers patients to comprehend medical language, thereby expediting the formulation and execution of efficacious treatment strategies.7 Therefore, nurses have an integral and important role in patient health education.
Patient health education competency (PHEC) refers to the specific qualities that health educators should have to conduct effective health education activities with patients.9 10 PHEC is an essential professional competency for nursing staff and determines the quality of patient education.11–14 However, in existing studies, the PHEC of clinical nurses is often the lowest-rated area of nursing competency.15 16 Therefore, the development and strengthening of PHEC for nurses are extremely important to improve the quality of patient education, patient care, patient safety and the development of nursing careers. In addition, we should pay attention to nursing students’ PHEC because they are the primary reserve of the clinical nurse workforce.
Accurate measurement of PHEC is important because it can be used to assess the PHEC status of nursing personnel and to develop targeted strategies based on the nursing personnel’s PHEC. Moreover, it can be used in research to assess the effectiveness of relevant PHEC interventions. Currently, relevant measurement instruments have been developed internationally: for example, a scale for measuring the PHEC of registered nurses developed by Lin and wang in 2017,17 a PHEC competency assessment scale developed by Hwang et al based on a literature review and the Delphi method,18 and a Spanish version of the nurse PHEC scale developed by Pueyo-Garrigues et al.19 Although related instruments are available for assessing PHEC in nursing personnel, these evaluation instruments have been developed in different settings and their validation varies considerably, with none considered the gold standard.
In this study, we defined PHEC as the specific qualities that must be possessed by nursing personnel to provide health education to patients, including knowledge, skills, beliefs or attitudes, self-concept, personality qualities and motivation. Although there has been a review of PHEC measurement instruments for nursing staff, this review has some limitations on its rigour.20 First, this review included both measurement instruments for PHEC and also systems for evaluating PHEC, which are different from measurement instruments. Second, this review did not systematically evaluate the measurement properties of instruments for measuring PHEC based on related guidelines. However, a systematic and comprehensive review of PHEC measurement instruments is crucial for guiding the selection of instruments and/or guiding the development and refinement of high-quality instruments in the future. The consensus-based standards for the selection of health measurement instruments (COSMIN) methodology provides resources to systematically review measurement instruments and evaluate them in terms of both methodological quality and quality of measurement properties to select instruments that are of high quality for study purposes and provide an evidence-based foundation for future high-level instrument development.21 Eskolin et al conducted a review on instruments assessing nurses’ competence in the empowerment of patient education.22 However, in this review, the author did not give a clear and specific definition of ‘empowering patient education competence of nurses’. This may lead to an unclear research boundary. Their investigation encompassed both instruments appraising nurses’ PHEC and also instruments evaluating the quality of patient education provided by healthcare professionals. Furthermore, they included tools for measuring nurses’ attitudes towards patient education. Considering the importance of nursing personnel in patient health education, and to ensure a more distinct scope and targeted content, our study will focus specifically on the PHEC measurement instruments, which are designed specifically for nursing personnel, including both nurses and nursing students. Furthermore, in our review, we will incorporate Chinese databases, unveiling more qualified instruments that align with our stringent criteria. Thus, this study is designed to conduct a comprehensive and rigorous systematic review of PHEC assessment instruments based on the COSMIN methodology, to evaluate the measurement properties of these instruments, provide a reference for nursing personnel and researchers to accurately and effectively assess PHEC, and provide recommendations for researchers to develop and improve PHEC assessment instruments.
This systematic review will address the following questions: (1) What instruments are available for assessing the PHEC of nursing personnel? (2) What are the characteristics of these instruments? (3) What is the methodological quality of studies on the measurement properties of these instruments? (4) What are these instruments’ measurement properties, interpretability and feasibility? (5) What are the similarities and differences between these instruments? (6) What are the knowledge and research gaps in the assessment of PHEC of nursing personnel?
Methods
The COSMIN guideline for systematic reviews of PROMs will be used to guide the implementation of the systematic review. PRISMA-P 2015 checklist andPRISMA 2020 checklist will be used to guide the reporting of the protocol and systematic review, respectively.21 23 24 The inconsistency between this protocol and that registered on PROSPERO and the reasons for this are shown in online supplemental table S1.
bmjopen-2023-072905supp001.pdf (201.6KB, pdf)
Inclusion and exclusion criteria of studies
Inclusion criteria
Studies will be included if they (1) address instrument(s) for measuring the PHEC of nurses or nursing students, (2) describe the processes of development and evaluation of one or more measurement properties for eligible instrument(s), (3) discuss instruments designed to measure the PHEC of health professionals (the literature explicitly mentions that it applies to nursing personnel as well) and (4) have full-text availability. If full-text versions of the studies are not available online, the authors of these articles will be contacted, and articles for which valid information was not available after contacting the authors will be excluded. We will limit the included studies to those written in English and Chinese.
Exclusion criteria
Studies will be excluded if they are (1) not primary studies (eg, biographies, addresses and editorials) or are case studies, (2) reports that used the instruments only for outcome measurements, (3) secondary studies (eg, reviews and/or systematic reviews), or (4) duplicate published studies.
Search strategy
A systematic search will be performed between 1 March 2023 and 31 March 2023 in six English databases (ie, CINAHL, EMBASE, Ovid Medline, PubMed, PsycINFO and Web of Science) and two Chinese databases (ie, CNKI and WANFANG DATA). We include Chinese databases since the researchers speak Chinese as their native language. We will also search for and screen references of all eligible literature. The search time limit is from the library’s creation date to 31 March 2023. A literature search will be conducted using a combination of subject terms and free words. The major search concepts will be nursing, health education, competence, instrument and measurement properties. Related comprehensive and sensitive search strategies developed by other researchers will also be used in this literature search, including (1) the search filter developed by the University of Oxford for finding PROMs,25 (2) the sensitive PubMed search filter for measuring attributes developed by Terwee et al, and (3) corresponding search filters applicable to other databases.26 We will examine results reported by nurses or nursing students, so the first filter will be adjusted appropriately (eg, we will remove those sections that are relevant to the quality of life and patient-reported outcomes). The search strategy constructed for PubMed is described in online supplemental table S2. The search strategy for the Chinese databases is shown in online supplemental table S3.
Study screening
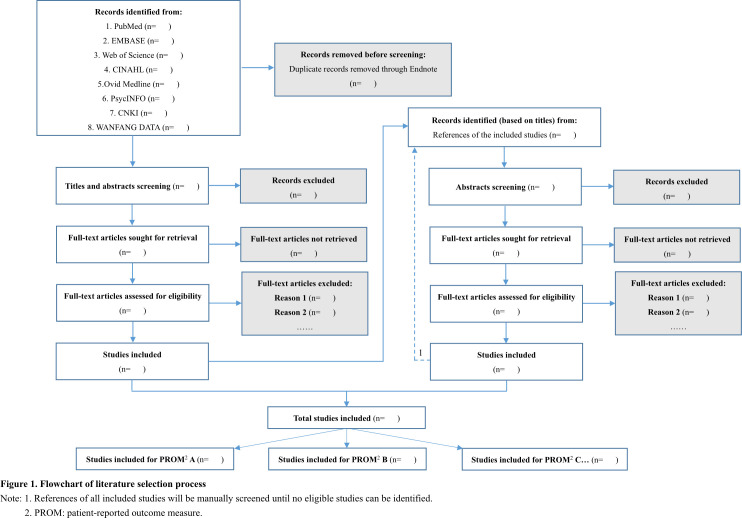
Covidence will be used to manage the references.27 First, duplicates from the eight databases will be removed with Covidence. After the initial screening, both researchers will independently review and screen titles, abstracts and full-text articles with the support of Covidence. In case of disagreement, a third researcher will be consulted to screen the literature. The screening processes of this study are shown in figure 1.
Figure 1.
Flowchart of literature selection process.
Data extraction
The two researchers will independently extract data from the included papers and resolve their differences through discussion. We will extract the data about the characteristics of the instruments (including instrument name, developer(s)/year developed, construct(s), targeted population, mode of administration, recall period, (sub)scale(s)/(number of items), response options, range of scores/scoring, original language and available translations; see online supplemental table S4, the characteristics of the included populations (including sample size, mean of age, gender, setting, country and language; see online supplemental table S5), the results on the psychometric properties (online supplemental table S6) and information about the interpretability (online supplemental table S7) and feasibility (online supplemental table S8) of the included instruments.
The term ‘outcome measure instrument development’ will be used instead of the original ‘patient-reported outcome measure development’ to more accurately reflect the inclusion of studies that examined outcomes reported by nurses or nursing students rather than patients.
Quality appraisal and data synthesis
Two researchers will independently assess the quality of eligible studies using the COSMIN Risk of Bias checklist, which is divided into three sections: content validity (instrument development and content validity), internal structure (structural validity, internal consistency and cross-cultural validity/measurement invariance) and other measurement properties (reliability, measurement error, criterion validity, hypothesis testing for construct validity and responsiveness).21 23 28 Each measurement property will be evaluated by different items provided by the COSMIN Risk of Bias checklist, and the items will be rated on a five-level score of ‘very good’, ‘adequate’, ‘doubtful’, ‘inadequate’ or ‘not applicable’.23 28 Based on the ‘the worst score counts’ principle, each measurement property’s overall methodological quality score is expressed by taking the lowest rating of any standard in the box.23 29 Subsequently, the two researchers will apply the updated criteria for good measurement properties alone to evaluate the reliability and validity of the instruments themselves, and the quality of the evidence will be graded using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach.23 29 In case of disagreement, a third researcher will be consulted.
We will work using the following three steps. In the first step, two investigators will apply the COSMIN Risk of Bias checklist to evaluate the methodological quality of each eligible study individually.28 The final consensus on the results of the methodological quality will be presented in online supplemental table S9,S9-1. In the second step, the updated criteria for good measurement properties will be applied to evaluate the quality of evidence for each measured property, and the evaluation results will be shown in online supplemental table S6,S6-1.23 29 This section mainly evaluates the strengths and weaknesses of the measurement properties. Among these, the quality of content validity will be evaluated according to the COSMIN methodology for content validity in three aspects: the relevance, comprehensiveness and comprehensibility of items, which can be ‘sufficient (+)’, ‘insufficient (−)’, ‘indeterminate (?)’ or ‘inconsistent (±)’.29 30 The quality of the remaining measurement properties (structural validity, internal consistency, cross-cultural validity, measurement invariance, reliability, measurement error, criterion validity, construct validity and responsiveness) will be evaluated by applying the COSMIN quality criteria, which can be ‘sufficient (+)’, ‘insufficient (−)’ and ‘indeterminate (?)’.23 The corresponding results will be reported in the rating columns of online supplemental table S6, and the results of rating content validity will be presented separately in online supplemental table S6-1 . In the third step, a modified GRADE approach will be used to rate the quality of the above evidence, reflecting the level of confidence in the quality of the evidence. To evaluate the content’s validity, three of these factors are applicable: risk of bias, inconsistency and indirectness.29 Assuming that the level of evidence quality for each of the remaining measurement properties is high, the quality of the evidence will be downgraded by considering the following factors: risk of bias, inconsistency, imprecision and indirectness.23 The quality of evidence will be divided into four levels: ‘high’, ‘moderate’, ‘low’ or ‘very low’.21 23 The corresponding results will be displayed in online supplemental table S10. Two investigators will independently grade and cross-check the results. In case of disputes, final decisions will be made in consultation with the third investigator.
Patient and public involvement
Neither patients nor the public will be involved in this study.
Ethics and dissemination
Ethical approval is not applicable for this study. We will share the findings from the study at national and/or international conferences and in a peer-reviewed journal in the fields of health education and/or patient education.
Discussion
To the best of our knowledge, this will be the first COSMIN-based systematic review of PHEC assessment instruments for nursing personnel, which will be reported following the Preferred Reporting Items for Systematic Reviews and Meta-analyses protocols (PRISMA-P) 2020 checklist. This systematic review will provide a comprehensive rating of the level of evidence for each measurement property of the PHEC assessment instruments, which will be based on an evaluation of the measurement properties of all included instruments and the methodological quality of the studies. Through this study, we will be able to develop recommendations on the use of existing qualified instruments in clinical practice and research that could assist nursing personnel and researchers in the accurate and valid assessment of PHEC. This review may provide an evidence-based foundation for the development, design, validation and use of future instruments by identifying problems in instrument development and validation and therefore help researchers to develop and improve these instruments.
Supplementary Material
Footnotes
Contributors: All authors have read and agreed to the published version of the manuscript. Conceptualisation: QC, ST and SW; methodology: QC, ST and ZS; data curation: QC, SW and KL; writing—original draft preparation: SW, KL and QC; writing—review and editing: QC, ST and ZS; supervision: QC and ST.
Funding: This work was supported by the National Natural Science Foundation of China (No. 72104250) and the Natural Science Foundation of Hunan Province (No. 2022JJ40642).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Not applicable.
References
- 1.World Health Organisation . Health education: theoretical concepts, effective strategies and core competencies: a foundation document to guide capacity development of health educators, . 2012Available: https://apps.who.int/iris/bitstream/handle/10665/119953/EMRPUB_2012_EN_1362.pdf?sequen [Accessed 11 Sep 2023].
- 2.Turner A, Anderson JK, Wallace LM, et al. An evaluation of a self-management program for patients with long-term conditions. Patient Educ Couns 2015;98:213–9. 10.1016/j.pec.2014.08.022 [DOI] [PubMed] [Google Scholar]
- 3.Lin P, Gao C, Su S, et al. Teaching principles: the applications in nursing practice. Taipei: Farseeing, 2005. [Google Scholar]
- 4.Siegel KR, Ali MK, Zhou X, et al. Cost-effectiveness of interventions to manage diabetes: has the evidence changed since 2008 Diabetes Care 2020;43:1557–92. 10.2337/dci20-0017 [DOI] [PubMed] [Google Scholar]
- 5.Koutsopoulou S, Papathanassoglou EDE, Katapodi MC, et al. Nurses as information providers to cancer patients: critical review of the evidence. J Clin Nurs 2010;19:749–65. 10.1111/j.1365-2702.2009.02954.x [DOI] [PubMed] [Google Scholar]
- 6.Feo R, Rasmussen P, Wiechula R, et al. Developing effective and caring nurse-patient relationships. Nurs Stand 2017;31:54–63. 10.7748/ns.2017.e10735 [DOI] [PubMed] [Google Scholar]
- 7.Kwame A, Petrucka PM. A literature-based study of patient-centered care and communication in nurse-patient interactions: barriers, Facilitators, and the way forward. BMC Nurs 2021;20:158. 10.1186/s12912-021-00684-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ghiyasvandian S, Zakerimoghadam M, Peyravi H. Nurse as a Facilitator to professional communication: a qualitative study. Glob J Health Sci 2014;7:294–303. 10.5539/gjhs.v7n2p294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hwang H-L, Kuo T-Y. Competency in delivering health education: a concept analysis. J Interprofessional Educ Pract 2018;11:20–5. 10.1016/j.xjep.2018.02.005 [DOI] [Google Scholar]
- 10.Karimi Moonaghi H, Emami Zeydi A, Mirhaghi A. Patient education among nurses: bringing evidence into clinical applicability in Iran. Invest Educ Enferm 2016;34:137–51. 10.17533/udea.iee.v34n1a16 [DOI] [PubMed] [Google Scholar]
- 11.Flinkman M, Leino-Kilpi H, Numminen O, et al. Nurse competence scale: a systematic and psychometric review. J Adv Nurs 2017;73:1035–50. 10.1111/jan.13183 [DOI] [PubMed] [Google Scholar]
- 12.Ko Y, Yu S. Core nursing competency assessment tool for graduates of outcome-based nursing education in South Korea: a validation study. Jpn J Nurs Sci 2019;16:155–71. 10.1111/jjns.12223 [DOI] [PubMed] [Google Scholar]
- 13.Nilsson J, Engström M, Florin J, et al. A short version of the nurse professional competence scale for measuring nurses' self-reported competence. Nurse Educ Today 2018;71:233–9. 10.1016/j.nedt.2018.09.028 [DOI] [PubMed] [Google Scholar]
- 14.Wilkinson CA. Competency assessment tools for registered nurses: an integrative review. J Contin Educ Nurs 2013;44:31–7. 10.3928/00220124-20121101-53 [DOI] [PubMed] [Google Scholar]
- 15.Cowan DT, Jenifer Wilson-Barnett D, Norman IJ, et al. Measuring nursing competence: development of a self-assessment tool for general nurses across Europe. Int J Nurs Stud 2008;45:902–13. 10.1016/j.ijnurstu.2007.03.004 [DOI] [PubMed] [Google Scholar]
- 16.Pueyo-Garrigues M, Whitehead D, Pardavila-Belio MI, et al. Health education: a Rogerian concept analysis. Int J Nurs Stud 2019;94:131–8. 10.1016/j.ijnurstu.2019.03.005 [DOI] [PubMed] [Google Scholar]
- 17.Lin LY, Wang RH. Patient education competence scale for registered nurses in Taiwan: scale development and Psychometric validation. Jpn J Nurs Sci 2017;14:117–25. 10.1111/jjns.12141 [DOI] [PubMed] [Google Scholar]
- 18.Hwang HL, Kuo ML, Tu CT. Health education and competency scale: development and testing. J Clin Nurs 2018;27:e658–67. 10.1111/jocn.14116 [DOI] [PubMed] [Google Scholar]
- 19.Pueyo-Garrigues M, Pardavila-Belio MI, Whitehead D, et al. Nurses’ knowledge, skills and personal attributes for competent health education practice: an instrument development and Psychometric validation study. J Adv Nurs 2021;77:715–28. 10.1111/jan.14632 [DOI] [PubMed] [Google Scholar]
- 20.Mi Y, Wu D, Wei ZZ, et al. Research progress on evaluation tool for health education competency of nursing staff. Chinese Nursing Research 2020;34:1983–7. 10.12102/j.issn.1009-6493.2020.11.023 [DOI] [Google Scholar]
- 21.Prinsen CAC, Mokkink LB, Bouter LM, et al. COSMIN guideline for systematic reviews of patient-reported outcome measures. Qual Life Res 2018;27:1147–57. 10.1007/s11136-018-1798-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Eskolin S-E, Inkeroinen S, Leino-Kilpi H, et al. Instruments for measuring empowering patient education competence of nurses: systematic review. J Adv Nurs 2023;79:2414–28. 10.1111/jan.15597 [DOI] [PubMed] [Google Scholar]
- 23.Mokkink LB, Prinsen C, Patrick DL, et al. COSMIN methodology for systematic reviews of patient-reported outcome measures (Proms). User Manual 2018;78:6–63. Available: https://www.cosmin.nl/wp-content/uploads/COSMIN-syst-review-for-PROMs-manual_version-1_feb-2018-1.pdf [Accessed 11 Sep 2023]. [Google Scholar]
- 24.Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and Exemplars for reporting systematic reviews. BMJ 2021;372:160. 10.1136/bmj.n160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mackintosh A, Comabella C, Hadi M, et al. PROM group construct & instrument type filters. Oxford: Department of Public Health, University of Oxford, 2010. Available: https://cosmin.nl/wp-content/uploads/prom-search-filter-oxford-2010.pdf [accessed 11 Sep 2023]. [Google Scholar]
- 26.Terwee CB, Jansma EP, Riphagen II, et al. Development of a methodological pubmed search filter for finding studies on measurement properties of measurement instruments. Qual Life Res 2009;18:1115–23. 10.1007/s11136-009-9528-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Babineau J. Product review: Covidence (systematic review software). J Can Health Libr Assoc 2014;35:68. 10.5596/c14-016 [DOI] [Google Scholar]
- 28.Mokkink LB, de Vet HCW, Prinsen CAC. COSMIN risk of bias checklist for systematic reviews of patient-reported outcome measures. Qual Life Res 2018;27:1171–9. 10.1007/s11136-017-1765-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Terwee CB, Prinsen C, Chiarotto A. COSMIN methodology for assessing the content validity of PROMs–user manual. Amsterdam: VU University Medical Center, 2018. Available: https://cosmin.nl/wp-content/uploads/COSMIN-methodology-for-content-validity-user-manual-v1.pdf [Google Scholar]
- 30.Terwee CB, Prinsen CAC, Chiarotto A. COSMIN methodology for evaluating the content validity of patient-reported outcome measures: a Delphi study. Qual Life Res 2018;27:1159–70. 10.1007/s11136-018-1829-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-072905supp001.pdf (201.6KB, pdf)