Abstract
Objectives
To evaluate the most up-to-date burden of traumatic brain injury (TBI) and spinal cord injury (SCI) and analyse their leading causes in different countries/territories.
Design
An analysis of Global Burden of Disease (GBD) data.
Setting
The epidemiological data were gathered from GBD Results Tool (1 January, 1990─31 December 2019) covering 21 GBD regions and 204 countries/ territories.
Participants
Patients with TBI/SCI.
Main outcomes and measures
Absolute numbers and age-standardised rates/estimates of incidence, prevalence and years lived with disability (YLDs) of TBI/SCI by location in 2019, with their percentage changes from 1990 to 2019. The leading causes (eg, falls) of TBI/SCI in 204 countries/territories.
Results
Globally, in 2019, TBI had 27.16 million new cases, 48.99 million prevalent cases and 7.08 million YLDs. SCI had 0.91 million new cases, 20.64 million prevalent cases and 6.20 million YLDs. Global age-standardised incidence rates of TBI decreased significantly by −5.5% (95% uncertainty interval −8.9% to −3.0%) from 1990 to 2019, whereas SCI had no significant change (−6.1% (−17.3% to 1.5%)). Regionally, in 2019, Eastern Europe and High-income North America had the highest burden of TBI and SCI, respectively. Nationally, in 2019, Slovenia and Afghanistan had the highest age-standardised incidence rates of TBI and SCI, respectively. For TBI, falls were the leading cause in 74% (150/204) of countries/territories, followed by pedestrian road injuries (14%, 29/204), motor vehicle road injuries (5%, 11/204), and conflict and terrorism (2%, 4/204). For SCI, falls were the leading cause in 97% (198/204) of countries/territories, followed by conflict and terrorism (3%, 6/204).
Conclusions
Global age-standardised incidence rates of TBI have decreased significantly since 1990, whereas SCI had no significant change. The leading causes of TBI/SCI globally were falls, but variations did exist between countries/territories. Policy-makers should continue to prioritise interventions to reduce falls, but priorities may vary between countries/territories.
Keywords: epidemiology, neurology, orthopaedic & trauma surgery, public health
STRENGTHS AND LIMITATIONS OF THIS STUDY.
One of the strengths of this study was that it provided the most up-to-date global, regional and national burden of traumatic brain injury (TBI)/spinal cord injury (SCI) from 1990 to 2019.
Another strength of this study was that it presented the variations of leading causes of TBI/SCI in 204 countries/territories, which have not been assessed before.
One of the limitations was that this study might underestimate the true incidence and period prevalence of TBI/SCI; was unable to calculate lifetime prevalence of TBI/SCI through the Global Burden of Disease (GBD) data.
The second limitation was that the estimates of TBI/SCI for some data-sparse countries/territories in this study should be interpreted carefully.
The third limitation was that this study could not assess associations between risk factors and TBI/SCI burden through the GBD data.
Introduction
Traumatic brain injury (TBI) and spinal cord injury (SCI) continue to pose challenges to the global public health systems, and the resulting disabilities have brought a huge economic burden to patients, public health systems and societies.1 2 Compared with the previous Global Burden of Disease (GBD) 2016 Study,3 4 new available data sources and improved statistical methods in the GBD 2019 Study led to the GBD 2019 results superseding those from previous rounds of GBD.5 Besides, nine additional countries/territories were first incorporated in the calculation of disease burden in the GBD 2019 Study.5 An update on the 2016 results of the burden of TBI/SCI is therefore warranted.
Ding et al reported the burden of SCI at the global and regional levels through the GBD 2019 data, but did not mention the disease burden in individual countries/territories.6 However, it will not allow for identifying variations that can exist between countries/territories within a same world or a same geographical region. Take the previous GBD 2016 Study as an example, the leading cause of TBI in the region, North Africa and Middle East, was concluded to be falls.4 It was true in Saudi Arabia, whereas it did not reflect the reality in other countries/territories within North Africa and Middle East, such as Afghanistan, where conflict and terrorism was the leading cause of TBI.4 Failure to present the data in individual countries/territories can prevent policymakers from identifying which causes should be targeted; wasting resources and reducing effectiveness of any interventions.7
Therefore, in this study, we aimed to provide the most up-to-date burden of TBI/SCI through the GBD 2019 data. Also, we analysed the leading causes of TBI/SCI in 204 countries/territories. Finally, the associations between the burden of TBI/SCI and Socio-demographic Index (SDI) in 204 countries/territories was explored.
Methods
Overview
This study of global health estimates followed the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) Statement and the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement.8 9 The GBD 2019 Study estimated burden of 369 diseases and injuries and 87 risk factors through multiple epidemiological measures, including incidence, prevalence, mortality, years of life lost (YLLs), years lived with disability (YLDs) and disability-adjusted life-years by age, sex, cause, year and location from 1990 to 2019.5 Our methods used for estimation of the burden of TBI and SCI were based on the framework of the GBD 2019 Study, which had already been described comprehensively elsewhere.5 10 Although TBI/SCI could cause death, they were not defined as a cause-of-death in the GBD 2019 Study.5 Therefore, in this study, we provided the burden of TBI/SCI by incidence, prevalence and YLDs, but not mortality or YLLs.
Case definitions
Based on the framework of the GBD 2019 Study,5 the definitions of TBI/SCI in this study relied on the International Classification of Diseases, 9th Revision (ICD-9) and the International Classification of Diseases, 10th Revision (ICD-10), which had also been described in details in the previous GBD 2016 Study published in The Lancet Neurology.4 Additionally, a clarification from the GBD 2019 Study is that TBI and SCI are both defined as a nature-of-injury but not a cause-of-injury.5 For example, TBI/SCI could be caused by a fall, the fall was therefore defined as a cause-of-injury and TBI/SCI as a nature-of-injury.
Data source
The data for 21 GBD regions and 204 countries/territories between 1 January 1990 and 31 December 2019 were available from the GBD Results Tool (https://vizhub.healthdata.org/gbd-results/). The data used in this study were from patients requiring medical care in hospital and emergency department records.5 Furthermore, compared with the GBD 2016 study, new available data sources were incorporated into estimates of non-fatal injuries in the GBD 2019 iteration, such as injury claims data from the Accident Compensation Corporation in New Zealand, national survey data from China, Ghana, India, Mexico, Russian Federation and South Africa from the WHO’s Study on Global AGEing and Adult Health, and literature studies data from India and South Africa based on inputs from the GBD collaborator network.5 Each data source was assigned a unique identifier and included in the Global Health Data Exchange (https://ghdx.healthdata.org/gbd-2019/data-input-sources). Additionally, considering that there are variations in quality of data by each country and territory, estimates in some data-sparse countries/territories were modelled and predicted by borrowing estimates from data-rich countries/territories.5 Detailed data sources used to estimate the burden of non-fatal injuries from each country and territory were listed in online supplemental etable 1. More details of the data sources and model strategies have been published elsewhere.5 10
bmjopen-2023-075049supp008.pdf (235.8KB, pdf)
Calculation of incidence, prevalence and YLD
The features of data processing used to calculate incidence, prevalence and YLDs in this study were consistent with the framework of the GBD 2019 Study.5 First, the data inputs of different cause-of-injury were incorporated and modelled by a Bayesian meta-regression tool, DisMod-MR 2.1, to infer the incidence of each cause-of-injury. Second, the GBD severity hierarchy for nature-of-injury (online supplemental etable 2) was used to establish a point-to-point relationship between cause-of-injury and nature-of-injury, which means that when multiple nature-of-injuries were caused by one cause-of-injury, nature-of-injury with the highest rank in the GBD severity hierarchy was selected to match it. Based on the framework of the GBD 2019 Study,5 because SCI had a higher rank in the GBD severity hierarchy than TBI, SCI was chosen if both conditions happened to an individual in our study, which was also consistent with the calculation process of the previous GBD 2016 Study published in The Lancet Neurology.4 Third, for the short-term disability (the duration was less than 1 year), the prevalence was approximately calculated as the incidence multiplied by the average duration. For the long-term disability (the duration was more than 1 year), DisMod-MR 2.1 was used to convert incidence to prevalence. Fourth, the GBD disability weights (online supplemental etable 3) were used to calculate YLDs. The GBD disability weights were evaluated on a 0–1 scale, with 0 representing complete health and 1 representing death.11 For the short-term disability, YLDs were calculated as the prevalence multiplied by the GBD disability weights. For the long-term disability, YLDs were calculated with the similar process but adjusted by comorbidity correction. Finally, the incidence, prevalence and YLDs were aggregated to calculate the all-cause incidence, prevalence and YLDs of TBI/SCI. Due to some sampling errors and non-sampling variances, we calculated the 95% uncertainty interval (UI) using the same methods described previously in the GBD 2019 Study.5 Generally, UIs were from 1000 draw-level estimates for each parameter, and 95% UIs were defined by the 25th and 975th values of the ordered 1000 estimates.
bmjopen-2023-075049supp009.pdf (670.8KB, pdf)
bmjopen-2023-075049supp010.pdf (110.3KB, pdf)
Statistical analysis
First, according to the GBD location hierarchy (online supplemental etable 4) in the GBD 2019 Study,5 we calculated absolute numbers and age-standardised rates/estimates of incidence, prevalence and YLD of TBI/SCI in 21 GBD regions and 204 countries/territories in 2019. The age-standardised rate/estimate is calculated by , where is the age-specific rate/estimate of the age group , and is the weight of the age group derived from the GBD 2019 world population standard (online supplemental etable 5).12 Second, based on the framework of the GBD 2019 Study,5 we used percentage changes of age-standardised rates/estimates of incidence, prevalence and YLD to calculate trends in the burden of TBI/SCI from 1990 to 2019. If the 95% UI of a percentage change did not include zero, it was determined to be a significant change, and vice versa.13 Third, according to the GBD cause hierarchy (online supplemental etable 6) in the GBD 2019 Study,5 we analysed the leading causes (eg, falls, pedestrian road injuries, motor vehicle road injuries, conflict and terrorism) for age-standardised incidence rates of TBI/SCI in 204 countries/territories in 2019, and we also analysed trends in age-standardised incidence rates of TBI/SCI caused by the leading causes in the corresponding countries/territories from 1990 to 2019 (except three causes: conflict and terrorism, exposure to forces of nature, and executions and police conflict, which were considered as fatal discontinuities and defined as random events due to not having predictable time trends in the GBD 2019 Study5). More details about definitions of causes and corresponding ICD-9/ICD-10 codes had already been described elsewhere.5 Fourthly, based on one prior GBD paper by GBD Fracture Collaborators,14 we reported the top three countries/territories with age-standardised incidence rates caused by each cause, and the top three countries/territories with both the largest increase and the largest decrease to explore potential reasons for their cause-specific disease burden. Finally, considering that the data were non-normal distributed (Shapiro-Wilk test had a p<0.001), the associations between SDI (a composite indicator of income per capita, years of schooling, and fertility rate; SDI ranges from 0 to 1 in the GBD 2019 Study, where 0 represents the lowest income per capita, the fewest years of schooling, and the highest fertility rate, and vice versa,5 online supplemental etable 7) and the age-standardised YLD rates in 204 countries/territories in 2019 were analysed by Spearman correlation tests to examine the effect of SDI on the disease burden.15–17 All statistical analyses and figures drawing were conducted in R program (V.4.1.3) and GraphPad Prism (V.7.0.0). Statistical significance was defined as two-tailed p<0.05.
bmjopen-2023-075049supp011.pdf (143KB, pdf)
bmjopen-2023-075049supp012.pdf (100KB, pdf)
bmjopen-2023-075049supp013.pdf (78.7KB, pdf)
bmjopen-2023-075049supp014.pdf (150.2KB, pdf)
Patient and public involvement
None.
Results
Global, regional and national disease burden
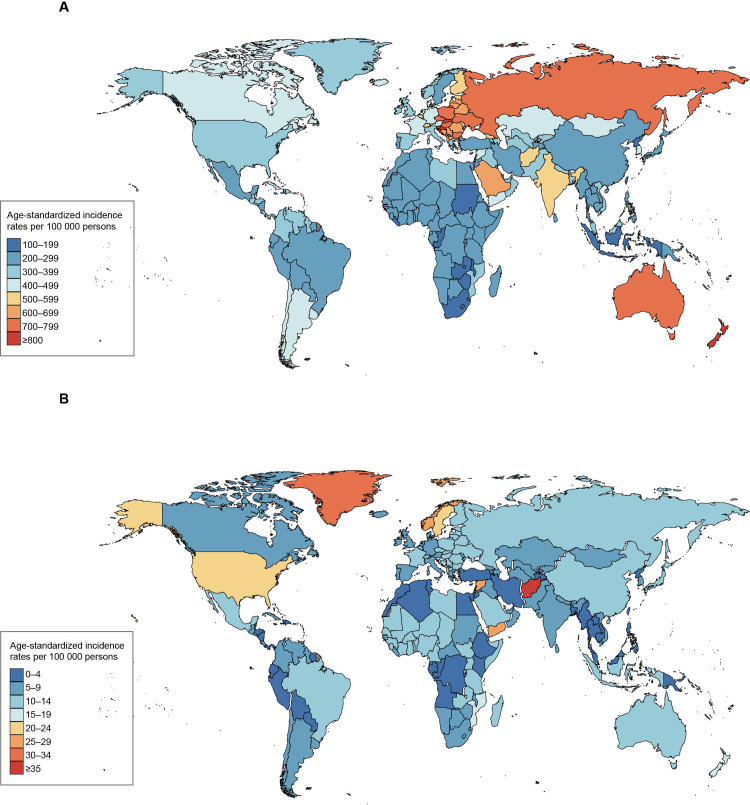
Globally, TBI had 27.16 (95% UI 23.36 to 31.42) million new cases, 48.99 (46.84 to 51.32) million prevalent cases and 7.08 (5.00 to 9.59) million YLDs in 2019 (table 1; online supplemental etables 8–10). There were 346 (95% UI 298 to 401) cases per 100 000 population, 599 (573 to 627) cases per 100 000 population and 87 (61 to 117) YLDs per 100 000 population for age-standardised incidence rates, age-standardised prevalence estimates and age-standardised YLD rates of TBI in 2019, respectively (figure 1; online supplemental efigures 1–3). SCI had 0.91 (0.71 to 1.16) million new cases, 20.64 (18.93 to 23.61) million prevalent cases, and 6.20 (4.47 to 8.16) million YLDs in 2019 (table 2; online supplemental etables 11–13). There were 12 (9 to 15) cases per 100 000 population, 253 (231 to 290) cases per 100 000 population, and 76 (55 to 100) YLDs per 100 000 population for age-standardised incidence rates, age-standardised prevalence estimates, and age-standardised YLD rates of SCI in 2019, respectively (online supplemental efigures 4–6). Global age-standardised incidence rates of TBI decreased significantly by −5.5% (95% UI −8.9% to −3.0%) from 1990 to 2019. By contrast, there was no significant change in global age-standardised incidence rates of SCI (−6.1% (−17.3% to 1.5%)) from 1990 to 2019. Regional and national TBI/SCI burden were described in the online supplemental eresults.
Table 1.
Incidence of traumatic brain injury in 1990 and 2019, and percentage changes of age-standardised rates by location, 1990–2019
| Location | Incidence | ||||
| Numbers (95% UI) | Age-standardised rates per 100 000 (95% UI) | Percentage change of age-standardised rates (95% UI) | |||
| (Year 1990) | (Year 2019) | (Year 1990) | (Year 2019) | (Year 1990–Year 2019) | |
| Global | 1 88 53 869 (1 62 15 389 to 2 18 06 108) | 2 71 60 708 (2 33 57 251 to 3 14 15 052) | 366 (317 to 421) | 346 (298 to 401) | −5.5% (−8.9% to −3.0%) |
| High-income North America | 11 20 251 (9 15 712 to 13 86 641) | 13 43 020 (11 30 550 to 16 33 382) | 392 (318 to 491) | 339 (280 to 416) | −13.7% (−17.1% to −10.0%) |
| Australasia | 1 43 293 (1 21 566 to 1 72 676) | 2 27 584 (1 94 914 to 2 70 506) | 710 (596 to 863) | 729 (613 to 889) | 2.6% (−0.9% to 6.0%) |
| High-income Asia Pacific | 6 82 610 (5 76 222 to 8 18 678) | 6 84 210 (5 85 181 to 8 07 782) | 386 (326 to 468) | 337 (282 to 414) | −12.8% (−15.8% to −9.6%) |
| Western Europe | 19 00 129 (16 58 576 to 22 11 597) | 22 11 884 (18 87 690 to 26 13 432) | 459 (398 to 536) | 413 (352 to 494) | −10.0% (−13.2% to −6.4%) |
| Southern Latin America | 2 02 139 (1 74 596 to 2 38 831) | 2 82 368 (2 45 426 to 3 31 894) | 409 (354 to 481) | 420 (363 to 497) | 2.9% (0.0% to 5.8%) |
| Eastern Europe | 21 11 822 (18 29 230 to 24 31 948) | 15 96 337 (13 80 438 to 18 51 604) | 913 (788 to 1057) | 737 (633 to 857) | −19.3% (−20.9% to −17.5%) |
| Central Europe | 10 50 449 (9 18 891 to 12 08 699) | 8 60 390 (7 50 474 to 9 86 981) | 846 (738 to 979) | 729 (631 to 857) | −13.8% (−16.4% to −11.0%) |
| Central Asia | 2 86 651 (2 49 571 to 3 32 136) | 3 54 124 (3 07 249 to 4 10 664) | 410 (358 to 472) | 374 (325 to 433) | −8.7% (−11.1% to −6.5%) |
| Central Latin America | 6 14 132 (5 14 302 to 7 38 706) | 7 65 677 (6 49 993 to 9 07 182) | 369 (315 to 437) | 306 (260 to 363) | −17.2% (−21.4% to −14.1%) |
| Andean Latin America | 1 03 322 (87 106 to 1 27 542) | 1 54 311 (1 35 039 to 1 78 003) | 268 (229 to 325) | 243 (213 to 279) | −9.5% (−23.6% to 0.1%) |
| Caribbean | 1 04 915 (91 947 to 1 19 513) | 1 55 545 (1 37 052 to 1 77 959) | 299 (263 to 338) | 325 (286 to 373) | 8.5% (4.6% to 12.2%) |
| Tropical Latin America | 4 02 255 (3 23 726 to 4 99 391) | 5 25 871 (4 27 539 to 6 47 705) | 261 (213 to 323) | 231 (187 to 286) | −11.5% (−14.6% to −8.6%) |
| East Asia | 1777 529 (14 57 606 to 21 80 900) | 34 12 591 (28 24 709 to 41 37 435) | 146 (120 to 178) | 207 (170 to 253) | 41.5% (34.7% to 48.6%) |
| Southeast Asia | 12 21 270 (10 35 226 to 14 28 941) | 16 53 210 (14 30 159 to 19 07 523) | 270 (232 to 312) | 246 (213 to 284) | −8.8% (−13.7% to −5.1%) |
| Oceania | 12 373 (10 780 to 14 206) | 29 408 (25 561 to 33 939) | 213 (186 to 242) | 244 (214 to 280) | 14.8% (11.1% to 18.8%) |
| North Africa and Middle East | 12 82 547 (10 94 820 to 15 00 156) | 19 11 495 (16 24 871 to 23 05 162) | 373 (320 to 432) | 319 (272 to 382) | −14.5% (−24.8% to −4.0%) |
| South Asia | 43 00 736 (36 94 519 to 49 84 977) | 87 75 756 (75 23 034 to 1 01 53 936) | 450 (388 to 515) | 508 (438 to 587) | 13.1% (9.7% to 16.1%) |
| Southern Sub-Saharan Africa | 1 15 447 (93 813 to 1 40 794) | 1 47 127 (1 20 571 to 1 77 386) | 233 (192 to 280) | 190 (157 to 230) | −18.4% (−21.4% to −15.8%) |
| Western Sub-Saharan Africa | 3 82 027 (3 11 502 to 4 64 214) | 9 11 247 (7 45 370 to 11 10 360) | 224 (187 to 269) | 233 (194 to 277) | 3.6% (−0.4% to 6.6%) |
| Eastern Sub-Saharan Africa | 9 15 689 (6 14 243 to 15 58 449) | 9 04 591 (7 57 646 to 10 80 346) | 491 (344 to 789) | 246 (209 to 286) | −49.8% (−67.5% to −30.4%) |
| Central Sub-Saharan Africa | 1 24 283 (1 03 595 to 1 54 993) | 2 53 964 (2 18 605 to 2 93 993) | 244 (207 to 294) | 217 (189 to 246) | −11.3% (−19.9% to −5.1%) |
UI, uncertainty interval.
Figure 1.
Age-standardised incidence rates per 100 000 persons of traumatic brain injury (A) and spinal cord injury (B) by countries/territories, 2019.
Table 2.
Incidence of spinal cord injury in 1990 and 2019, and percentage changes of age-standardised rates by location, 1990–2019
| Incidence | |||||
| Numbers (95% UI) | Age-standardised rates per 100 000 (95% UI) | Percentage change of age-standardised rates (95% UI) | |||
| (Year 1990) | (Year 2019) | (Year 1990) | (Year 2019) | (Year 1990–Year 2019) | |
| Global | 5 95 228 (4 71 497 to 7 66 656) | 9 09 001 (7 06 953 to 11 56 410) | 12 (10 to 16) | 12 (9 to 15) | −6.1% (−17.3% to 1.5%) |
| High-income North America | 67 501 (52 610 to 87 116) | 1 14 001 (85 370 to 1 55 645) | 22 (17 to 28) | 23 (17 to 30) | 4.6% (−0.9% to 10.5%) |
| Australasia | 2714 (2200 to 3280) | 4996 (3949 to 6243) | 13 (11 to 16) | 14 (11 to 17) | 8.1% (3.3% to 13.2%) |
| High-income Asia Pacific | 24 139 (19 331 to 29 846) | 32 690 (25 123 to 43 125) | 13 (11 to 16) | 12 (9 to 15) | −9.8% (−13.9% to −6.4%) |
| Western Europe | 46 448 (36 453 to 59 098) | 61 215 (45 912 to 80 682) | 10 (8 to 13) | 10 (8 to 12) | −5.6% (−9.8% to −2.2%) |
| Southern Latin America | 3665 (3016 to 4385) | 5305 (4326 to 6394) | 8 (6 to 9) | 8 (6 to 9) | 1.7% (−2.6% to 5.2%) |
| Eastern Europe | 36 775 (29 156 to 46 344) | 30 092 (23 743 to 37 989) | 16 (12 to 20) | 13 (11 to 16) | −15.7% (−18.3% to −12.9%) |
| Central Europe | 19 087 (15 495 to 23 162) | 17 227 (13 648 to 21 504) | 15 (12 to 18) | 13 (11 to 16) | −13.0% (−16.2% to −9.8%) |
| Central Asia | 4887 (4059 to 5797) | 6252 (5146 to 7468) | 7 (6 to 9) | 7 (6 to 8) | −6.8% (−9.5% to −4.3%) |
| Central Latin America | 19 015 (14 979 to 24183) | 24 749 (19 700 to 30982) | 13 (10 to 17) | 10 (8 to 13) | −23.4% (−34.3% to −17.9%) |
| Andean Latin America | 2898 (1837 to 5488) | 2871 (2381 to 3389) | 8 (5 to 14) | 5 (4 to 5) | −39.5% (−66.5% to −11.2%) |
| Caribbean | 2137 (1747 to 2618) | 3459 (2814 to 4227) | 7 (5 to 8) | 7 (6 to 9) | 8.2% (0.9% to 15.1%) |
| Tropical Latin America | 21 365 (16 580 to 27710) | 33 477 (25 278 to 44097) | 16 (12 to 20) | 14 (11 to 19) | −8.1% (−11.5% to −5.1%) |
| East Asia | 1 04 274 (79 266 to 1 34 082) | 2 36 241 (1 73 443 to 3 15 144) | 10 (7 to 13) | 13 (10 to 18) | 39.8% (32.0% to 48.0%) |
| Southeast Asia | 36 808 (28 373 to 48545) | 47 473 (37 736 to 59770) | 9 (7 to 12) | 7 (6 to 9) | −18.7% (−31.8% to −10.7%) |
| Oceania | 253 (203 to 313) | 569 (466 to 697) | 5 (4 to 6) | 5 (4 to 6) | 10.3% (−2.6% to 19.0%) |
| North Africa and Middle East | 42 700 (28 665 to 64843) | 52 776 (34 780 to 97680) | 14 (9 to 21) | 9 (6 to 17) | −32.7% (−60.7% to 8.9%) |
| South Asia | 81 527 (64 240 to 1 03 563) | 1 56 382 (1 20 425 to 2 01 426) | 9 (7 to 11) | 9 (7 to 12) | 5.1% (−7.8% to 12.8%) |
| Southern Sub-Saharan Africa | 4607 (3525 to 6118) | 6590 (5072 to 8666) | 10 (8 to 14) | 9 (7 to 12) | −12.0% (−16.5% to −8.4%) |
| Western Sub-Saharan Africa | 16 168 (11 877 to 22347) | 38 162 (28 265 to 51944) | 11 (8 to 15) | 11 (8 to 15) | 3.4% (−5.4% to 8.0%) |
| Eastern Sub-Saharan Africa | 54 804 (22 784 to 1 33 741) | 29 156 (22 453 to 37652) | 30 (14 to 69) | 9 (7 to 12) | −69.8% (−86.8% to −36.8%) |
| Central Sub-Saharan Africa | 3457 (2080 to 6799) | 5318 (3976 to 7773) | 7 (4 to 12) | 5 (4 to 6) | −29.1% (−48% to −10.3%) |
UI, uncertainty interval.
bmjopen-2023-075049supp015.pdf (239.4KB, pdf)
bmjopen-2023-075049supp016.pdf (205.8KB, pdf)
bmjopen-2023-075049supp017.pdf (233.8KB, pdf)
bmjopen-2023-075049supp001.pdf (344.3KB, pdf)
bmjopen-2023-075049supp002.pdf (547.4KB, pdf)
bmjopen-2023-075049supp003.pdf (544.9KB, pdf)
bmjopen-2023-075049supp018.pdf (176.9KB, pdf)
bmjopen-2023-075049supp019.pdf (201.2KB, pdf)
bmjopen-2023-075049supp020.pdf (194KB, pdf)
bmjopen-2023-075049supp004.pdf (348.2KB, pdf)
bmjopen-2023-075049supp005.pdf (548.2KB, pdf)
bmjopen-2023-075049supp006.pdf (548.1KB, pdf)
bmjopen-2023-075049supp023.pdf (91.3KB, pdf)
Leading causes by country and territory
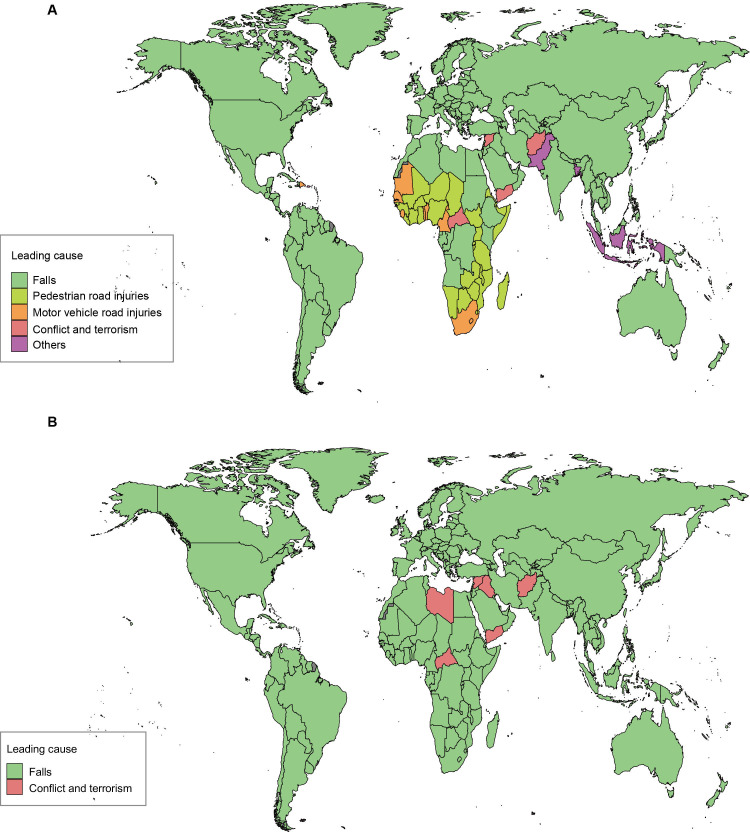
Considering the cause-specific age-standardised incidence rates of TBI in 2019, falls were the leading cause in 74% (150/204) of countries/territories, followed by pedestrian road injuries (14%, 29/204), motor vehicle road injuries (5%, 11/204) and conflict and terrorism (2%, 4/204) (figure 2; online supplemental etables 14). The top three countries/territories with age-standardised incidence rates by falls were Finland (418 (324 to 539) cases per 100 000 population), Slovenia (401 (320 to 504) cases per 100 000 population) and Croatia (400 (318 to 501) cases per 100 000 population) (out of 150 countries/territories), by pedestrian road injuries were Mozambique (103 (76 to 134) cases per 100 000 population), Ghana (83 (61 to 109) cases per 100 000 population) and Guinea-Bissau (71 (50 to 95) cases per 100 000 population) (out of 29 countries/territories), by motor vehicle road injuries were Comoros (86 (61 to 117) cases per 100 000 population), Mauritania (79 (56 to 109) cases per 100 000 population) and Cameroon (75 (52 to 103) cases per 100 000 population) (out of 11 countries/territories), and by conflict and terrorism were Afghanistan (356 (134 to 798) cases per 100 000 population), Yemen (256 (103 to 590) cases per 100 000 population) and Syrian Arab Republic (180 (68 to 394) cases per 100 000 population) (out of 4 countries/territories) (figure 3).
Figure 2.
The leading causes for age-standardised incidence rates of traumatic brain injury (A) and spinal cord injury (B) by countries/territories, 2019
Figure 3.
Number of countries/territories by the leading causes for age-standardised incidence rates of traumatic brain injury (TBI) (A) and spinal cord injury (SCI) (B); total countries/territories=204; the listed are the top three countries/territories with age-standardised incidence rates caused by each cause, 2019; and the top three with both the largest increase and the largest decrease, 1990–2019.
bmjopen-2023-075049supp021.pdf (815.2KB, pdf)
For SCI, falls were the leading cause for age-standardised incidence rates in 97% (198/204) of countries/territories in 2019, followed by conflict and terrorism (3%, 6/204) (online supplemental etables 15). The top three countries/territories with age-standardised incidence rates by falls were Greenland (23 (15 to 34) cases per 100 000 population), Norway (21 (14 to 33) cases per 100 000 population) and Sweden (19 (12 to 29) cases per 100 000 population) (out of 198 countries/territories), and by conflict and terrorism were Afghanistan (40 (8 to 128) cases per 100 000 population), Yemen (22 (5 to 66) cases per 100 000 population) and Syrian Arab Republic (21 (4 to 64) cases per 100 000 population) (out of 6 countries/territories). Percentage changes of cause-specific TBI/SCI burden were described in the online supplemental eResults.
bmjopen-2023-075049supp022.pdf (764.3KB, pdf)
Disease burden by Socio-demographic Index
Generally, a positive association was found between age-standardised YLD rates of TBI and SDI in 204 countries/territories in 2019 (ρ=0.42, p<0.001) (online supplemental efigure 7). SCI on the other hand, had no statistical association with SDI (ρ=−0.05, p=0.49), although the SCI burden in a few countries/territories, such as Afghanistan, far exceeded those of others.
bmjopen-2023-075049supp007.pdf (532.7KB, pdf)
Discussion
This study provided the most up-to-date burden of TBI and SCI using GBD 2019 data. It also presented the variations between the leading causes of TBI/SCI in 204 countries/territories. Finally, it explored the associations between each national SDI and the burden of TBI/SCI.
Incidence of TBI/SCI
Globally, the age-standardised incidence rates of TBI significantly decreased since 1990. This improvement may reflect the benefits of global initiatives to reduce TBI rates. For example, major efforts have focused on road safety and reduced road-related injuries, a leading cause of TBI globally.18 In 2004, the United Nations General Assembly and the WHO passed resolutions calling for preventive measures against road injuries.19 The resolutions were championed in many countries/territories successively.19 The age-standardised TBI incidence rates decreased significantly from 1990 to 2019 by −7.2% (−11.9% to −2.0%) in Oman, −20.3% (−22.5% to −17.9%) in Russia and −9.8% (−13.6% to −5.4%) in Sweden, demonstrating the effectiveness of their interventions.
Unfortunately, the global age-standardised SCI incidence rates did not significantly change despite the decreases in TBI. Although we used the same GBD 2019 data, this conclusion differs from Ding et al’s finding that the global age-standardised incidence rates of SCI decreased since 1990.6 Ding et al calculated the temporal trends of the global age-standardised incidence rates of SCI using the estimated annual percentage change (EAPC).6 The EAPC was based on a linear regression mode of the age-standardised rates and the calendar year.20 However, EAPC can be biased in modelling injuries from natural disasters or wars; if included, it inflates estimates in volatile regions.21 Furthermore, Ding et al misinterpreted their statistical results.6 The EAPC was −0.08 but had a 95% confidence interval (CI) of −0.24 to 0.09.6 By focusing only on the point estimate of −0.08 and neglecting the CI, they failed to convey that the CI crossed zero. That approach may confuse and bring biased information to policy-makers.22 Our study showed a non-significant change in the global age-standardised incidence rates of SCI (−6.1% (−17.3% to 1.5%)). The lack of SCI change may be because motor vehicle accidents are a major cause of TBI but not SCI. As discussed below, other interventions may be required to reduce SCI.23 24
Causes of TBI/SCI
One challenge in any global effort to reduce falls is the ageing population. The global population over the age of 65 rose from 6.2% in 1990 to 9.1% in 2019.25 Falls are more common in older than younger adults owing to sarcopenia, osteoporosis, sleeping disturbance, multimorbidity and frailty.13 Several countries/territories with high age-standardised incidence rates of TBI/SCI by falls also have percentages of older adults that far exceeds the world average of 9.1% of the population. Examples include Finland (22.1% of the population over the age of 65 in 2019), Slovenia (20.2%), Croatia (20.9%), Norway (17.3%) and Sweden (20.2%).25 Although some components of falls are modifiable, some countries/territories have unique challenges due to their geographical features. Finland, Norway and Sweden have cold climates and unique environmental risk factors (ie, icy sidewalks) that may increase their populations’ fall risk.26 27 Environmental risks may need to be prioritised in these countries/territories, particularly as their populations age.
This study also examined changes in age-standardised incidence rates by falls. Turkey had the largest increases from 1990 to 2019 (TBI: 100.3% (88.8% to 114.5%), SCI: 110.5% (97.3% to 125.4%)). Armenia had a significant decrease in both TBI (−35.1% (−41.2% to −28.4%)) and SCI (−33.9% (−39.3% to −27.9%)). The reasons for this change were unknown but may be related to changes in resource allocation. The gross domestic product (GDP, current USD) in Armenia increased from US$2.26 billion in 1990 to US$13.86 billion in 2019, leading to increased healthcare spending that may have improved public healthcare education.28–30 By contrast, Turkey faced economic difficulty in recent years; its GDP decreased from US$957.78 billion in 2013 to US$761 billion in 2019, which may have contributed to the significant increases in this study.30
Road injuries were the leading cause of TBI in 20% (40/204) of the countries/territories. There was a higher prevalence in African countries/territories. One possible reason for the high prevalence in Africa may be the rapid increase in motor vehicle ownership,31 without sufficient road infrastructure (ie, roads and traffic safety).32–35 A previous study found non-adherence to traffic regulations, poorly maintained roads, inadequate traffic signage and a lack of pedestrian protections as possible reasons behind Mozambique’s high age-standardised incidence rates of TBI.36 The lack of sufficient safety around motor vehicles is not limited to Africa. The Dominican Republic also recorded high age-standardised TBI incidence rates; this was also attributed to traffic safety, although the reported reasons were high rates of people driving while intoxicated and limited policing of traffic violations.37 The high burden of TBI by road injuries in these countries/territories demonstrates that despite some countries/territories having successfully reduced their road injuries, challenges remain in others. Furthermore, the variations in causes and rates of TBI in this study suggest that global initiatives to reduce rates of motor vehicle accidents or TBI need to consider the unique challenges faced by each country and territory rather than a generalist approach to rate reduction.19
Finally, conflict and terrorism was the most common cause of TBI/SCI in 2% (4/204) and 3% (6/204) of countries/territories, respectively, such as Afghanistan, Yemen and Syrian Arab Republic, which are likely attributable to the ongoing armed conflicts that have occurred in these countries/territories over many years.38–40
TBI/SCI burden by SDI
The burden of TBI was generally higher in countries/territories with higher SDI. One of the reasons for the difference may be disparities in access to healthcare resources.4 Medical resources are sufficient and easily available in locations with higher SDI, so patients with TBI can be treated and recorded in time. However, medical resources are insufficient in locations with lower SDI, and patients may die of treatable TBI and even fail to receive a diagnostic code. Furthermore, data from countries/territories with higher SDI may be more reliable than locations with lower SDI, so estimates in locations with higher SDI may be closer to the true disease burden.5
Strengths and limitations
This study had some strengths. First, it provided the most up-to-date global, regional and national burden of TBI/SCI from 1990 to 2019. The findings can help policy-makers acquire the most up-to-date epidemiological characteristics of TBI/SCI in 21 GBD regions and 204 countries/territories. Second, it presented variations of leading causes of TBI/SCI in 204 different countries/territories even within a same geographical region. For example, the leading cause of TBI in the sub-Saharan Africa region varied from falls in Angola to pedestrian road injuries in Namibia to motor vehicle road injuries in South Africa and conflict and terrorism in the Central African Republic. Falls were also the leading cause of SCI in most countries/territories in the North Africa and Middle East (eg, Saudi Arabia, Egypt, Qatar); however, conflict and terrorism were the leading cause in Afghanistan, Iraq, Libya, Syrian Arab Republic and Yemen. The presentation of variations in different countries/territories can provide richer information than a regional analysis and help policy-makers identify which causes should be targeted to improve the effectiveness of preventive interventions.
This study also had some limitations. First, the data sources relied on patients having medical records, so reported estimates would underestimate the true incidence. For example, there was a discrepancy between the annual worldwide estimation of new TBI cases in this study (27.16 million) and other recent expert sources (more than 50 million).7 The underestimation may be attributed to two reasons.
The first reason for underestimation is that the register-based data may not cover all cases. For example, the Nordic countries and the USA are considered to have reliable statistics, but there are still patients treated at facilities that are not covered by registries (eg, private healthcare).7 41 Further, many patients with mild TBI go untreated and, therefore, unrecorded; population-based studies with a broad definition of TBI show significantly higher TBI incidence rates than those based on hospital discharge rates.7 The second reason for underestimation is that clinical diagnosis codes may not accurately match injuries, especially in patients with multitrauma. For example, some patients may experience both TBI/SCI from a traumatic event, but TBI would not be matched to the individual because SCI had a higher rank than TBI in the GBD severity hierarchy.5 This is because after the GBD TBI and SCI collaborators tried to apportion co-occurring non-fatal injuries using regression methods, they found that many long-term disabilities were assigned to seemingly trivial non-fatal injury categories (eg, open wounds/bruises), thus pulling disability away from more serious non-fatal injury outcomes (eg, TBI/SCI).4 Therefore, this study followed the method that assigns one non-fatal injury case to the most severe of any co-occurring non-fatal injuries according to the GBD severity hierarchy.4 5 This method was also used in the paper by the GBD TBI and SCI collaborators published in the Lancet Neurology.4
Second, this study might also underestimate the true period prevalence. The GBD 2019 Study calculated the period prevalence of non-fatal injuries through probabilities of permanent health loss.5 Permanent health loss relates to the probability of patients (1 year after the injury) returning to a health status with more disability than their preinjury health status.5 However, the probabilities of permanent health loss assessed in the GBD Study may be grossly underestimated, especially for TBI, because accurate TBI prevalence data are even more limited than incidence data, especially in low-income/middle-income countries; and TBI is not an isolated event but can have variable long-term consequences, including dementia, stroke, parkinsonism and epilepsy.7 For example, a large study from a Swedish registry found higher probabilities of premature mortality, psychiatric inpatient admission/outpatient visits, disability pension, welfare recipiency and low educational attainment after even a mild TBI compared with uninjured siblings.42 Furthermore, the associations between TBI and long-term neurological diseases remain poorly understood; many sequelae other than those mentioned above have not been considered, leading to an underestimation of the true TBI period prevalence.7 Referring to the reviewer’ comments, we also attempted but could not calculate the lifetime prevalence of TBI/SCI through the GBD data because, while longitudinal cohort or survey analysis is commonly used to calculate lifetime prevalence,43 44 the GBD Study is a cross-sectional analysis conducted iteratively on an annual basis.5 Short-term disability caused by non-fatal injuries is assumed to last less than 1 year in the GBD Study, which means that the short-term disability after TBI/SCI in a given year may not be calculated for prevalence in future iterations.5
Third, a weakness of this study is the ability to estimate incidence in countries with lower-quality data. Estimates in some data-sparse countries/territories were modelled and predicted by borrowing estimates from data-rich countries/territories.5 Therefore, the estimates of the data-sparse countries/territories (eg, Democratic People’s Republic of Korea) might have a greater deviation than the true incidence. Furthermore, the cause-specific burden (that is, the leading cause) of TBI/SCI in some data-sparse countries/territories should be interpreted carefully. For example, it is logically difficult to explain why falls have surpassed traffic accidents as the leading cause of SCI in many population-rich Asian countries/territories (eg, Malaysia) with chaotic traffic.
Fourth, the GBD 2019 Study did not link TBI/SCI with risk factors such as behavioural factors (eg, alcohol use), so we could not assess any associations between the two (eg, disease burden attributable to certain risk factors).45
Finally, the GBD TBI and SCI collaborators defined TBI/SCI by ICD-9/ICD-10 codes through physician review. However, with reference to the reviewer’s comments, there may be a minor error probably not reflected in the results in the Lancet Neurology paper; the ICD-10 code S06.0 (concussion) can be considered a mild TBI, but S06.1 (traumatic cerebral oedema) in the published paper cannot.4
Implications for future studies
First, population-based epidemiological studies may be improved in the future through standardised definitions (eg, standardised criteria for diagnosis), methods (eg, case ascertainment based on multiple, overlapping sources of information, such as hospitals, outpatient clinics, general practitioners and death certificates), and data presentation (eg, collection of a complete calendar year of data).7 These improvements would be especially helpful in data-sparse locations to facilitate comparisons between countries/territories. Second, there is a need for better ways to characterise the currently under-recognised risk of long-term disabling sequelae to bring estimates closer to the true period prevalence, especially for mild TBI. Furthermore, we hope that the GBD collaborators include lifetime prevalence in future iterations to estimate the global impact of TBI/SCI accurately. Last, we hope that the GBD collaborators will include the burden of TBI/SCI attributable to risk factors; this would provide more detailed results on the causes of TBI/SCI and allow for more targeted preventative strategies.
Conclusions
In conclusion, the global age-standardised incidence rates of TBI had a significant decrease since 1990, whereas SCI had no significant change. Falls were the leading cause of TBI/SCI in 74% (150/204) and 97% (198/204) of countries/territories, respectively, but the variations of leading causes of TBI/SCI did exist between countries/territories, even within a same geographic region. Although declining, high burden of TBI remained a concern in both higher and lower SDI countries/territories. High burden of SCI from falls in almost all countries/territories demonstrates the need for falls reduction to be a global priority now and into the future, but priorities may vary between countries/territories.
Supplementary Material
Acknowledgments
We thank the Institute for Health Metrics and Evaluation at the University of Washington and all collaborators involved in the GBD 2019 Study to make the data accessible to the public.
Footnotes
BG and DBA contributed equally.
Contributors: HZ, SF and LC contributed to the conception and design of the study. BG and DBA contributed to the acquisition, analysis and interpretation of data. BG and DBA contributed to drafting the text or preparing the figures. All authors reviewed the manuscript. All authors accepted full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish.
Funding: This study was funded by Taishan Scholars Program of Shandong Province-Young Taishan Scholars (tsqn201909197).
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request. All data relevant to the study are included in the article or uploaded as online supplemental information.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Maas AIR, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol 2008;7:728–41. 10.1016/S1474-4422(08)70164-9 Available: [DOI] [PubMed] [Google Scholar]
- 2. Ahuja CS, Wilson JR, Nori S, et al. Traumatic spinal cord injury. Nat Rev Dis Primers 2017;3:17018. 10.1038/nrdp.2017.18 Available: 10.1038/nrdp.2017.18 [DOI] [PubMed] [Google Scholar]
- 3. GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: a systematic analysis for the global burden of disease study 2016. The Lancet 2017;390:1211–59. 10.1016/S0140-6736(17)32154-2 Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. GBD 2016 Traumatic Brain Injury and Spinal Cord Injury Collaborators . Global, regional, and national burden of traumatic brain injury and spinal cord injury, 1990-2016: a systematic analysis for the global burden of disease study 2016. The Lancet Neurology 2019;18:56–87. 10.1016/S1474-4422(18)30415-0 Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. GBD 2019 Diseases and Injuries Collaborators . Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. The Lancet 2020;396:1204–22. 10.1016/S0140-6736(20)30925-9 Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ding W, Hu S, Wang P, et al. Spinal cord injury: the global incidence, prevalence, and disability from the global burden of disease study 2019. Spine 2022;47:1532–40. 10.1097/BRS.0000000000004417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Maas AIR, Menon DK, Adelson PD, et al. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. The Lancet Neurology 2017;16:987–1048. 10.1016/S1474-4422(17)30371-X Available: [DOI] [PubMed] [Google Scholar]
- 8. Stevens GA, Alkema L, Black RE, et al. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet 2016;388:e19–23.:S0140-6736(16)30388-9. 10.1016/S0140-6736(16)30388-9 Available: [DOI] [PubMed] [Google Scholar]
- 9. von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. The Lancet 2007;370:1453–7. 10.1016/S0140-6736(07)61602-X Available: [DOI] [PubMed] [Google Scholar]
- 10. GBD 2019 Universal Health Coverage Collaborators . Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet 2020;396:1250–84. 10.1016/S0140-6736(20)30750-9 Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Salomon JA, Haagsma JA, Davis A, et al. Disability weights for the global burden of disease 2013 study. Lancet Glob Health 2015;3:e712–23. 10.1016/S2214-109X(15)00069-8 [DOI] [PubMed] [Google Scholar]
- 12. GBD 2019 Demographics Collaborators . Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: a comprehensive demographic analysis for the global burden of disease study 2019. The Lancet 2020;396:1160–203. 10.1016/S0140-6736(20)30977-6 Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ye P, Er Y, Wang H, et al. Burden of falls among people aged 60 years and older in Mainland China, 1990-2019: findings from the global burden of disease study 2019. Lancet Public Health 2021;6:e907–18. 10.1016/S2468-2667(21)00231-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. GBD 2019 Fracture Collaborators . Global, regional, and national burden of bone fractures in 204 countries and territories, 1990-2019: a systematic analysis from the global burden of disease study 2019. Lancet Healthy Longev 2021;2:e580–92. 10.1016/S2666-7568(21)00172-0 Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Srivastav A, Richard CL, McRell AS, et al. The unintended consequence of novel Coronavirus (COVID-19) pandemic on racial inequities associated with adverse childhood experiences (aces): findings from a population-based study. Front Public Health 2021;9:701887. 10.3389/fpubh.2021.701887 Available: 10.3389/fpubh.2021.701887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. GBD 2016 Stroke Collaborators . Global, regional, and national burden of stroke, 1990-2016: a systematic analysis for the global burden of disease study 2016. The Lancet Neurology 2019;18:439–58. 10.1016/S1474-4422(19)30034-1 Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Jin X, Ren J, Li R, et al. Global burden of upper respiratory infections in 204 countries and territories, from 1990 to 2019. EClinicalMedicine 2021;37:100986. 10.1016/j.eclinm.2021.100986 Available: 10.1016/j.eclinm.2021.100986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. World Health Organization . Road traffic injuries, Available: https://www.who.int/news-room/fact-sheets/detail/road-traffic-injuries
- 19. Hyder AA, Hoe C, Hijar M, et al. The political and social contexts of global road safety: challenges for the next decade. Lancet 2022;400:127–36. 10.1016/S0140-6736(22)00917-5 [DOI] [PubMed] [Google Scholar]
- 20. Liu Z, Jiang Y, Yuan H, et al. The trends in incidence of primary liver cancer caused by specific Etiologies: results from the global burden of disease study 2016 and implications for liver cancer prevention. J Hepatol 2019;70:674–83. 10.1016/j.jhep.2018.12.001 [DOI] [PubMed] [Google Scholar]
- 21. Mohammadi E, Villeneuve LM, Smith ZA. Letter to the editor: "spinal cord injury the global incidence, prevalence, and disability from the global burden of disease study 2019. Spine (Phila Pa 1976) May 22, 2023. 10.1097/BRS.0000000000004726 Available: [DOI] [PubMed] [Google Scholar]
- 22. Greenland S, Senn SJ, Rothman KJ, et al. Statistical tests, P values, confidence intervals, and power: a guide to Misinterpretations. Eur J Epidemiol 2016;31:337–50. 10.1007/s10654-016-0149-3 Available: 10.1007/s10654-016-0149-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. World Health Organization . Falls. Available: https://www.who.int/news-room/fact-sheets/detail/falls
- 24. World Health Organization . Spinal cord injury, Available: https://www.who.int/news-room/fact-sheets/detail/spinal-cord-injury
- 25. The World Bank . Population (age group as % of total population). Available: https://genderdata.worldbank.org/indicators/sp-pop-zs/?age=65%2B&view=trend
- 26. Ala-Seppälä H, Heino I, Frantzén J, et al. Injury profiles, demography and Representativeness of patients with TBI attending a regional emergency Department. Brain Inj 2016;30:1062–7. 10.3109/02699052.2016.1170880 Available: 10.3109/02699052.2016.1170880 [DOI] [PubMed] [Google Scholar]
- 27. WorldAtlas . Nordic Countries, Available: https://www.worldatlas.com/articles/nordic-countries.html
- 28. Chekijian S, Truzyan N, Stepanyan T, et al. Healthcare in transition in the Republic of Armenia: the evolution of emergency medical systems and directions forward. Int J Emerg Med 2021;14:5. 10.1186/s12245-020-00328-3 Available: 10.1186/s12245-020-00328-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Peek-Asa C, Coman MA, Zorn A, et al. Association of traumatic brain injury severity and time to definitive care in three low-middle-income European countries. Inj Prev 2022;28:54–60. 10.1136/injuryprev-2020-044049 Available: 10.1136/injuryprev-2020-044049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. The World Bank . GDP (current US$). Available: https://data.worldbank.org/indicator/NY.GDP.MKTP.CD?page=1
- 31. Ukonze FI, Nwachukwu MU, Mba HC, et al. Determinants of vehicle ownership in Nigeria. SAGE Open 2020;10:215824402092297. 10.1177/2158244020922970 Available: 10.1177/2158244020922970 [DOI] [Google Scholar]
- 32. Embolo FN, Bellamkonda N, Dickson D, et al. A epidemiology of traumatic brain injury based on clinical symptoms amongst inhabitants of the Southwest region of Cameroon: a community-based study. Brain Inj 2021;35:1184–91. 10.1080/02699052.2021.1957150 Available: 10.1080/02699052.2021.1957150 [DOI] [PubMed] [Google Scholar]
- 33. Takoukam R, Kanmounye US, Robertson FC, et al. Prehospital conditions and outcomes after Craniotomy for traumatic brain injury performed within 72 hours in central Cameroon: A cross-sectional study. World Neurosurg 2020;142:e238–44. 10.1016/j.wneu.2020.06.182 [DOI] [PubMed] [Google Scholar]
- 34. Laeke T, Tirsit A, Kassahun A, et al. Prospective study of surgery for traumatic brain injury in Addis Ababa, Ethiopia: trauma causes, injury types, and clinical presentation. World Neurosurg 2021;149:e460–8. 10.1016/j.wneu.2021.02.003 [DOI] [PubMed] [Google Scholar]
- 35. Ackah M, Gazali Salifu M, Osei Yeboah C. Estimated incidence and case fatality rate of traumatic brain injury among children (0-18 years) in sub-Saharan Africa. A systematic review and meta-analysis. PLoS One 2021;16:e0261831. 10.1371/journal.pone.0261831 Available: 10.1371/journal.pone.0261831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Nizamo H, Meyrowitsch DW, Zacarias E, et al. Mortality due to injuries in Maputo city, Mozambique. Int J Inj Contr Saf Promot 2006;13:1–6. 10.1080/17457300500151705 Available: 10.1080/17457300500151705 [DOI] [PubMed] [Google Scholar]
- 37. Reddy SP, Walsh MS, Paulino-Ramirez R, et al. A neurologic injuries following road traffic accidents in the Dominican Republic: examining causes and potential solutions. Traffic Inj Prev 2019;20:690–5. 10.1080/15389588.2019.1643016 Available: 10.1080/15389588.2019.1643016 [DOI] [PubMed] [Google Scholar]
- 38. The Lancet . Afghanistan: the international community must act. Lancet 2021;398. 10.1016/S0140-6736(21)02535-6 Available: [DOI] [PubMed] [Google Scholar]
- 39. The United Nations . UN News Global perspective Human stories, Available: https://news.un.org/en/story/2021/09/1101162
- 40. International Committee of The Red Cross . War in Yemen. Available: https://www.icrc.org/en/war-yemen
- 41. Cota MR, Moses AD, Jikaria NR, et al. Discordance between documented criteria and documented diagnosis of traumatic brain injury in the emergency Department. J Neurotrauma 2019;36:1335–42. 10.1089/neu.2018.5772 Available: 10.1089/neu.2018.5772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Sariaslan A, Sharp DJ, D’Onofrio BM, et al. Long-term outcomes associated with traumatic brain injury in childhood and adolescence: A nationwide Swedish cohort study of a wide range of medical and social outcomes. PLoS Med 2016;13:e1002103. 10.1371/journal.pmed.1002103 Available: 10.1371/journal.pmed.1002103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. McKinlay A, Grace RC, Horwood LJ, et al. Prevalence of traumatic brain injury among children, adolescents and young adults: prospective evidence from a birth cohort. Brain Inj 2008;22:175–81. 10.1080/02699050801888824 Available: 10.1080/02699050801888824 [DOI] [PubMed] [Google Scholar]
- 44. Whiteneck GG, Cuthbert JP, Corrigan JD, et al. Prevalence of self-reported lifetime history of traumatic brain injury and associated disability: A statewide population-based survey. J Head Trauma Rehabil 2016;31:E55–62. 10.1097/HTR.0000000000000140 Available: [DOI] [PubMed] [Google Scholar]
- 45. GBD 2019 Risk Factors Collaborators . Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet 2020;396:1223–49. 10.1016/S0140-6736(20)30752-2 Available: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2023-075049supp008.pdf (235.8KB, pdf)
bmjopen-2023-075049supp009.pdf (670.8KB, pdf)
bmjopen-2023-075049supp010.pdf (110.3KB, pdf)
bmjopen-2023-075049supp011.pdf (143KB, pdf)
bmjopen-2023-075049supp012.pdf (100KB, pdf)
bmjopen-2023-075049supp013.pdf (78.7KB, pdf)
bmjopen-2023-075049supp014.pdf (150.2KB, pdf)
bmjopen-2023-075049supp015.pdf (239.4KB, pdf)
bmjopen-2023-075049supp016.pdf (205.8KB, pdf)
bmjopen-2023-075049supp017.pdf (233.8KB, pdf)
bmjopen-2023-075049supp001.pdf (344.3KB, pdf)
bmjopen-2023-075049supp002.pdf (547.4KB, pdf)
bmjopen-2023-075049supp003.pdf (544.9KB, pdf)
bmjopen-2023-075049supp018.pdf (176.9KB, pdf)
bmjopen-2023-075049supp019.pdf (201.2KB, pdf)
bmjopen-2023-075049supp020.pdf (194KB, pdf)
bmjopen-2023-075049supp004.pdf (348.2KB, pdf)
bmjopen-2023-075049supp005.pdf (548.2KB, pdf)
bmjopen-2023-075049supp006.pdf (548.1KB, pdf)
bmjopen-2023-075049supp023.pdf (91.3KB, pdf)
bmjopen-2023-075049supp021.pdf (815.2KB, pdf)
bmjopen-2023-075049supp022.pdf (764.3KB, pdf)
bmjopen-2023-075049supp007.pdf (532.7KB, pdf)
Data Availability Statement
Data are available on reasonable request. All data relevant to the study are included in the article or uploaded as online supplemental information.