ABSTRACT
This study aimed to investigate the basic data on the effectiveness and safety of the system in healthy subjects using an immersive virtual reality (VR) exercise system specialized for therapeutic exercise therapy during dialysis or hospital use. A total of 15 healthy adult subjects performed four exercises, namely lifting and rowing exercises using VR and each movement exercise without VR (control). The simulator sickness questionnaire (SSQ) was administered pre- and post-operatively to assess for VR sickness. Blood pressure, heart rate (HR), rating of perceived exhaustion, Profile of Mood States 2nd Edition Japanese version, and muscle activity (iEMG) were measured using electromyography. The correlation between changes in mood states and HR or iEMG results was examined. The SSQ measured post-VR exercise was 11.2 (18.7–7.5) and 11.2 (7.5–29.9) points in the lifting and rowing VR, respectively. The HR in lifting (VR, 82.5 ± 12.7 vs control, 71.6 ± 10.6 bpm, P<0.05) and rowing (VR, 94.2 ± 13.1 vs control, 83.5 ± 12.0, P<0.05) with VR exercise was significantly higher than in control. No significant differences were observed between the other variables. There was a positive correlation between HR and negative mood in the lifting VR condition (r=0.64, P<0.05), but not in the control group. Contrastingly, there was a positive correlation between iEMG and negative mood in rowing control (r=0.56), but not VR. Safety was confirmed, with no VR sickness or discontinuation of the system. Exercise therapy using VR resulted in a higher exercise load. This VR system has the potential for additional effective intradialytic exercises and hospital use.
Key Words: virtual reality, game, inpatient, hemodialysis, rehabilitation
INTRODUCTION
The exercise experience in the virtual reality (VR) space with game elements provides an experience that makes the subjects feel as if they were real. Exercise therapy using VR is expected to lead to the continuation of exercise by providing enjoyment that cannot be achieved with conventional exercise therapy. In a study of healthy adults, cycling exercise with VR was less fatiguing, more enjoyable, and more self-efficacious than regular cycling exercise.1 VR-based exercise therapy is expected to be further developed in the areas of medical and rehabilitation sciences.
However, there are some limitations to exercise therapy using VR with respect to medicine and rehabilitation. In particular, exercise therapy using VR is expected to be an effective intradialytic exercise for dialysis patients who are forced to rest in bed for 4 h three times a week; however, dedicated equipment and evidence are lacking. In previous studies,1-6 exercise therapy using VR was performed with an ergometer and treadmill, or with patients who could sit, stand, or walk. Notably, immersive VR devices used in previous studies require a computer,1 cords, and the game itself, separate from VR goggles, which are often peripheral devices.2-7 However, these devices are not suitable for use in dialysis or small hospital rooms because of their various peripheral devices. Immersive VR was completed only with a VR device, and minimal equipment was necessary for patients who had difficulty leaving their bed, such as patients undergoing hemodialysis.
We developed an immersive VR exercise therapy system using a stand-alone VR device, assuming exercise during dialysis or in a hospital bed. This exercise therapy system focused on therapeutic strength training to improve the functional decline of the lower limbs, assuming patients were in the supine bed position. This report aims to provide basic data on the safety and effectiveness of this system in healthy subjects, which can be used as a basis for future applications in patients.
MATERIALS AND METHODS
Study design and subjects
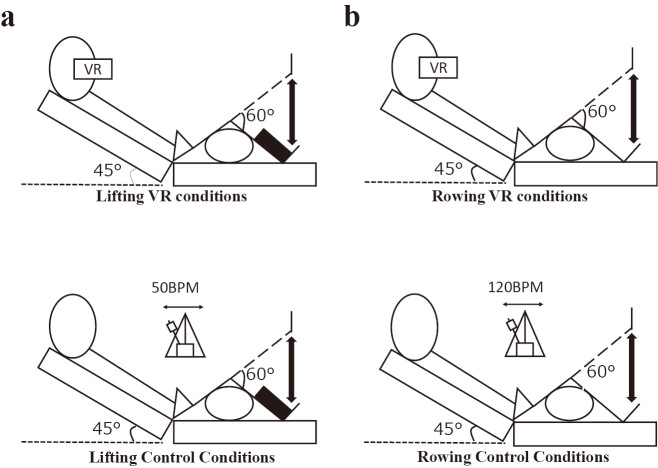
This was a crossover study. The subjects participated in four types of exercise conditions with or without VR (lifting or rowing exercises); 1) lifting VR condition, 2) rowing VR condition, 3) lifting control condition, and 4) rowing control condition. Each exercise was performed in a randomized order at intervals of at least 2 days (Figure 1). The subjects were 15 university students (men/women: 3/12, age: 21.9 ± 0.3 years, Body mass index (BMI): 20.2 ± 1.9 kg/m2). The eligibility criteria for the subjects were as follows: 1) Healthy university students enrolled at Seirei Christopher University. The exclusion criteria were individuals having (1) underlying diseases, such as hypertension, diabetes, or hyperlipidemia; (2) central nervous system diseases or orthopedic problems that interfere with exercise; and (3) who could not provide their consent for research or withdrew consent and requested for discontinuation. The Ethics Committee approved the study of Seirei Christopher University (approval number 21026).
Fig. 1.
Study design
This study was conducted in a crossover study. Subjects participated in four periods of four different exercise conditions: 1) lifting VR condition, 2) rowing VR condition, 3) lifting control condition, and 4) rowing control condition. Each exercise was randomly performed at least 2 days apart to exclude fatigue.
Configuration of VR equipment
The central equipment of the VR device consisted of VR goggles, a remote control, and a six-axis accelerometer (Figure 2). The VR device/remote control was the “Lenovo Mirage Camera with Daydream “(Mirage Solo with Daydream, Lenovo, China) and the supplied remote control. This stand-alone VR device required no peripheral equipment other than a remote control and can be used only with VR equipment. The remote control was used to set up the start of the game, and was not used for in-game operations. The six-axis accelerometer used was the “M5StickC” (M5Stack Technology Co, Ltd, China), which was linked to the VR device via Bluetooth. An accelerometer is a device that measures the vibration of an object or the acceleration of its motion. One device was placed above each ankle of the subject to sense the motion of the lower limbs, which was reflected in the VR device images.
Fig. 2.
VR system overview
Fig. 2a: Data from the 6-axis accelerometer accompanying the movement of the lower limbs were input into the VR device and reflected in the movement of the lower-limb avatar. An explanation of the 6-axis acceleration setting is displayed on the external surface before the game starts, and the user fixes the 6-axis accelerometers to both ankles by themselves.
Fig. 2b: A VR exercise therapy system does not require a computer and can only be completed using a VR device. Games can be selected by lifting and rowing when the VR device is turned on.
System setup
The procedure of the VR exercise therapy system used in this study was as follows: (1) wearing a VR system; (2) launching the lifting or rowing application; (3) instructions for the posture in the game, mounting, and synchronization of the accelerometer, and a signal to start the VR space was displayed on the screen; (4) setting the difficulty level; and (5) starting the game. The operations required on the subject’s side were (3)–(5). Operations (3)–(5) did not require remote control operations; the subject gazes at the icons, and the game progresses.
Game design
The two-game designs for the exercise therapy system developed in this study were lifting and rowing. The lifting and rowing programs were designed as a similar movement of lower extremities exercise as typical resistance and aerobic exercise, adding a game element and improving the program’s fun. Lifting is a game in which the players compete by lifting a soccer ball that falls in front of them in the VR space and kicking it up in time with the timing of its fall. Lifting requires kicking the foot up, just as the ball and avatar of the foot collide. If the subject lifts his/her foot harder, the ball kicks higher. The difficulty level of lifting can be set and the number of balls can be increased by increasing the difficulty level. When used as exercise therapy in clinical settings, it is intended to be performed as resistance training by loading dead weights on both the lower limbs.
Rowing is a game in which the players boarded a boat floating on a lake in a VR space. The subjects were required to collect the coins scattered around the boat repeatedly. The subject was required to perform rhythmic extension movements of both knee joints to move the boat forward. Manipulation of the boat was performed by varying the number of times the knees of both lower limbs were extended. When only the right lower limb was moved, the boat turned to the left. The boat can move faster by increasing the knee extension of both lower limbs larger and faster. The game had a time limit, and the subjects were instructed to collect as many coins as possible within the time limit. When used as exercise therapy in a clinical setting, it was intended to be performed as an aerobic exercise.
Safety considerations
The VR device is equipped with an external camera. Subjects can immediately stop the game by staring at the avatar’s arm on either side of the screen. The game can subsequently be resumed. This allows the user to suspend and resume the game in a lying position without assistance (Figure 3). This technology has been patented in Japan (Japanese Patent Application No. 2021-101961: https://ipforce.jp/patent-jp-A-2021-101961).
Fig. 3.

Safety considerations
An arm avatar is observed to appear during the implementation of the VR exercise therapy system. Starting with the arm, the avatar can interrupt the game and return from the VR space to the actual space.
STUDY PROTOCOL
Lifting VR conditions
The subjects wore the VR goggles and were instructed to kick the ball up as much as possible during the ball drop. The subject was set in a semi-Farrer position (bed gatch up 45°), hip flexion at 45°, knee flexion at 60°, and knee extension in hip flexion. The measurement protocol consisted of 5 min of rest followed by a 1 min exercise at 40% 1 Repetition Maximum of ankle weight load (Figure 4).
Fig. 4.
The study protocol
Lifting control conditions
The lifting control condition consisted of 5 min of rest, followed by 1 min of knee extension exercise. The exercise load was an ankle weight of 1 Repetition Maximum 40% under the same lifting VR condition. The exercise was performed with a metronome sounding at 50 bpm in the same position as in the lifting VR exercise condition. Knee extension and flexion were performed alternately on each side for 30 s each for 1 min (Figure 4).
Rowing VR conditions
There are so many coins on the lake in VR space that is difficult to collect them all in the game time. Subjects were instructed to “collect as many coins as possible” within the time limit of 3 min and maneuvered the boat by rhythmic knee extension and flexion movements of both the lower extremities. Ankle weight loading was not applied. The subject’s limb position was the same as in the lifting condition (Figure 4).
Rowing control conditions
The rowing control condition consisted of 5 min of rest and 3 min of repetitive knee extension and flexion exercises. The exercise was performed with a metronome at 120 bpm and a rhythm of alternating knee extension and flexion on each side. The limb position measurement was the same as that for the other conditions (Figure 4).
DATA COLLECTION
A simulator sickness questionnaire (SSQ) was administered at the beginning and end of the exercise to evaluate the VR sickness. The SSQ is an objective evaluation index for visual induced sickness, consisting of 16 items that are subjectively rated on a 4-point scale from 0 to 3, depending on the severity of the participant’s symptoms. The SSQ is divided into three subscales (nausea, oculomotor symptoms, and disorientation). Each subscale is weighted, and the score is calculated by adding the scores answered to the corresponding items and multiplying by 3.74.8The cutoff value for VR sickness was reported as 33.3 points.9 Higher SSQ scores indicate greater VR sickness.
Total Score = (Nausea point + Oculomotor point + Disorientation point) × 3.74
Sex, age, and body mass index (BMI) were used as the basic attributes. Systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), and rating of perceived exertion (RPE) in the lower limb and chest by Borg scales were measured before, during, and after exercise. SBP and DBP were measured using a mercury sphygmomanometer, and HR was measured by the value displayed on an electrocardiogram monitor (bedside monitor BMS2401, NIHON KOUDEN, Tokyo, Japan).
The muscle activity was measured using electromyography as an objective evaluation of exercise using an electromyogram system (TeleMyo G2, Noraxon, Arizona, USA). The electrodes (Blue Sensor, Ambu, Baltorpbakken, Denmark) were affixed to the bilateral vastus lateralis, with the electrode center distance set at 30 mm. The sampling frequency was 1500 Hz. The analysis was performed using an electromyography analysis software (Myo Research XP, Noraxon, Arizona, USA). After smoothing using the root mean square (RMS), integrated electromyography (iEMG) values were obtained at rest and during exercise.
Mood changes were measured prior to and after each exercise using the Profile of Mood States 2nd Edition Japanese version (POMS2). The Japanese version of the POMS2 is a questionnaire that measures anger-hostility (AH), confusion–bewilderment (CB), depression–dejection (DD), fatigue–inertia (FI), tension–anxiety (TA), vigor–activity (VA), and friendliness (F). Seven items were scored on a 5-point scale (0 to 4), from “not at all” to “very much” for each item, covering a wide range of mood states.10 The total mood disturbance (TMD) score, which represents the overall negative mood state, is calculated by summing all items, except VA and subtracting VA as follows:
TMD = AH + CB + DD + FI + TA - VA
In addition, the amount of change in the TMD score pre- and post-exercise was calculated to assess the change in negative mood state.
STATISTICAL ANALYSIS
All the data were tested for normality using the Shapiro–Wilk test. Normally distributed data are presented as the mean ± standard deviation, and non-normally distributed data are presented as the median and interquartile range (IQR). The unpaired t-test or Mann–Whitney U test was performed as an inter-conditional comparison between the VR and control conditions. A paired t-test or Wilcoxon signed-rank sum test was also performed as a pre-and post-comparison of each exercise.
To examine the relationship between objective biological responses to exercise and the subjective mood, the correlation between the absolute value and change in TMD score and HR or iEMG during exercise was examined using Pearson’s product-moment correlation coefficient or Spearman’s rank correlation coefficients. The significance level was set at less than 5%.
RESULTS
None of the participants dropped out of the study because of VR sickness, and VR sickness was not confirmed. The SSQ measured post-VR conditions was 11.2 (18.7–7.5) points in the Lifting VR condition and 11.2 (7.5–29.9) points in the Rowing VR condition (Table 1).
Table 1.
Simulator Sickness Questionnaire change pre- and post-VR conditions
| Lifting VR conditions | Rowing VR conditions | ||||||
| Pre | Post | P-value | Pre | Post | P-value | ||
| Simulator Sickness
Questionnaire |
16.7 ± 14.1 | 12.5 ± 8.6 | 0.112 | 15.0 (1.9–29.9) | 11.2 (7.5–29.9) | 0.414 | |
In a group comparison between the VR and control conditions, the HR of the lifting VR condition during exercise (82.5±12.7 bpm) was significantly higher than that of the lifting control condition (71.6±10.6 bpm) (P<0.05). The HR of the rowing VR condition at post-exercise (94.2±13.1 bpm) was significantly higher than that in the rowing control condition (83.5±12.0 bpm) (P<0.05). The SBP, DBP, RPE (lower limbs/chest), iEMG, and each sub-item score of POMS2 and TMD showed no statistically significant difference in both VR conditions compared to each control condition (Table 2).
Table 2.
Outcome comparison between lifting VR/control condition and rowing VR/control condition
| Lifting | Rowing | |||||||
| VR conditions | Control conditions | P-value | VR conditions | Control conditions | P-value | |||
| Pre exercise | SBP (mmHg) | 105.3 ± 11 | 108.5 ± 8.9 | 0.433 | 107.0 ± 10.2 | 106.9 ± 9.4 | 0.97 | |
| DBP (mmHg) | 70.1 ± 9.3 | 68.5 ± 8.6 | 0.647 | 69.6 ± 6.0 | 69.1 ± 9.0 | 0.85 | ||
| HR(Bpm) | 72.1 ± 14.4 | 68.3 ± 12.5 | 0.446 | 73.4 ± 15.3 | 68.2 ± 13.1 | 0.327 | ||
| RPE (lower limbs) | 6.0 (6.0 – 6.5) | 6.0 (6.0 – 6.0) | 0.866 | 6.0 (6.0 – 6.0) | 6.0 (6.0 – 6.0) | 0.916 | ||
| RPE(Chest) | 6.0 (6.0 – 6.0) | 6.0 (6.0 – 6.0) | 0.55 | 6.0 (6.0 – 6.0) | 6.0 (6.0 – 6.0) | 0.577 | ||
| During exercise | SBP (mmHg) | 108.2 ± 10.5 | 112.5 ± 13 | 0.394 | 108.7 ± 10.7 | 110.4 ± 10.9 | 0.777 | |
| DBP (mmHg) | 68.8 ± 9.1 | 68.8 ± 8.9 | 1 | 71.3 ± 6.1 | 68.7 ± 9.0 | 0.451 | ||
| HR (Bpm) | 82.5 ± 12.7* | 71.6 ± 10.6 | 0.0166 | 80.1 ± 16.1 | 69.5 ± 12.1 | 0.0511 | ||
| RPE (lower limbs) | 9.0 (8.0 – 12.5) | 13.0 (11.0 – 13.0) | 0.0574 | 10.0 (7.0 – 11.0) | 10.0 (7.0 – 13.0) | 0.503 | ||
| RPE (Chest) | 7.0 (6.0 – 8.0) | 6.0 (6.0 – 9.0) | 0.7 | 7.0 (6.0 – 9.5) | 8.0 (6.0 – 9.0) | 1 | ||
| Post exercise | SBP (mmHg) | 109.1 ± 11.5 | 111.6 ± 9.6 | 0.529 | 115.3 ± 10.8 | 111.9 ± 10.3 | 0.375 | |
| DBP (mmHg) | 70.2 ± 7.7 | 72.0 ± 6.0 | 0.484 | 71.9 ± 6.5 | 71.7 ± 9.4 | 0.929 | ||
| HR (Bpm) | 87.1 ± 11.6 | 83.0 ± 9.8 | 0.308 | 94.2 ± 13.1* | 83.5 ± 12.0 | 0.0274 | ||
| RPE (lower limbs) | 7.0 (7.0 – 9.0) | 8.0 (7.0 – 11.5) | 0.419 | 8.0 (7.0 – 9.0) | 9.0 (6.0 – 11.5) | 0.411 | ||
| RPE (Chest) | 6.0 (6.0 – 7.0) | 6.0 (6.0 – 8.5) | 0.578 | 8.0 (6.0 – 9.0) | 7.0 (6.0 – 9.0) | 1 | ||
| Δ | SBP (During – Pre) | 2.9 ± 6.3 | 4.1 ± 7.1 | 0.626 | –2.0 (–4.5 – 9.5) | 1.0 (0.0 – 5.0) | 0.261 | |
| SBP (Post – Pre) | 3.8 ± 6.9 | 3.1 ± 5.1 | 0.766 | 8.0 (1.0 – 13.0) | 6.0 (2 – 8) | 0.37 | ||
| DBP (During – Pre) | –1.3 ± 7.8 | 0.2 ± 6.5 | 0.564 | 1.7 ± 7.6 | –0.3 ± 3.0 | 0.352 | ||
| DBP (Post – Pre) | 0.1 ± 6.5 | 3.5 ± 7.2 | 0.192 | 2.3 ± 6,8 | 2.6 ± 5.5 | 0.906 | ||
| HR (During – Pre) | 8.0 (6.0 – 12.0)* | 3.0 (–0.5 – 7) | 0.006 | 6.7 ± 14.4 | 1.2 ± 6.8 | 0.199 | ||
| HR (Post – Pre) | 14.9 ± 8.6 | 14.7 ± 8.6 | 0.933 | 20.8 ± 13.3 | 15.3 ± 9.3 | 0.203 | ||
| RPE (lower limbs) (During – Pre) | 3.0 (2.0 – 5.5) | 6.0 (4.5 – 7.0) | 0.08 | 2.0 (1.0 – 4.5) | 4.0 (1.0 – 6.0) | 0.346 | ||
| RPE (lower limbs) (Post – Pre) | 1.0 (0.0 – 3.0) | 2.0 (1.0 – 4.0) | 0.32 | 1.0 (0.0 – 2.5) | 3.0 (0.0 – 5.5) | 0.235 | ||
| RPE (Chest) (During – Pre) | 0.0 (0.0 – 1.0) | 0.0 (0.0 – 2.0) | 0.574 | 1.0 (0.0 – 3.5) | 2.0 (0.0 – 3.0) | 0.983 | ||
| RPE (Chest) (Post – Pre) | 1.0 (0.0 – 1.5) | 0.0 (0.0 – 1.5) | 0.619 | 2.0 (0.0 – 3.0) | 1.0 (0.0 – 3.0) | 0.983 | ||
| EMG | iEMG | 6184 ± 2703.7 | 4633.7 ± 1783.8 | 0.137 | 12388.0 ± 4554.5 | 10778.5 ± 5178.6 | 0.52 | |
| Salivary amylase | Pre | 3.0 (2.0 – 6.0) | 3.0 (2.0 – 4.5) | 0.578 | 3.0 (3.0 – 8.0) | 3.0 (2.0 – 13.5) | 0.881 | |
| Post | 7.0 (2.5 – 17.0) | 3.0 (2.0 – 7.0) | 0.176 | 5.0 (3.0 – 25.5) | 3.0 (3.0 – 4.5) | 0.22 | ||
| Δ | 0 (–1.0 – 1.0) | 1.0 (–1.0 – 10.0) | 0.336 | –1.0 (–7.0 – 1.5) | 1.0 (0.0 – 22.5) | 0.081 | ||
| POMS2 (Points) | ||||||||
| AH | Pre | 2.0 ± 2.8 | 2.0 ± 3.7 | 0.661 | 1.0 (0.0 – 3.5) | 2.0 (0 – 4.0) | 0.795 | |
| Post | 1.0 (0.0 – 1.0) | 0.0 (0.0 – 3.5) | 0.858 | 2.5 ± 3.0 | 2.9 ± 3.1 | 0.723 | ||
| Δ | –0.93 ± 1.87 | –0.87 ± 2.39 | 0.933 | 0.67 ± 1.84 | 0.20 ± 2.08 | 0.52 | ||
| CB | Pre | 10.8 ± 5.8 | 12.0 ± 6.9 | 0.61 | 13.7 ± 6.6 | 13.7 ± 5.7 | 0.977 | |
| Post | 10.7 ± 5.0 | 11.3 ± 6.4 | 0.777 | 13.1 ± 6.4 | 12.6 ± 5.0 | 0.802 | ||
| Δ | 7.0 (4.5 – 9.0) | 8.0 (6.0 – 9.5) | 0.404 | 0 (–2.0 – 0.5) | 0 (–2.5 – 1.0) | 0.817 | ||
| DD | Pre | 2.0 (0 – 4.5) | 4.0 (1.0 – 6.0) | 0.362 | 2.0 (0.5 – 9.5) | 5.0 (1.0 – 10) | 0.402 | |
| Post | 1.0 (0.0 – 4.0) | 2.0 (0.0 – 3.5) | 0.733 | 2.0 (0.0 – 10.5) | 3.0 (1.0 – 7.5) | 0.737 | ||
| Δ | –1.20 ± 2.46 | –0.47 ± 1.36 | 0.32 | –1.07 ± 2.87 | –0.33 ± 2.35 | 0.45 | ||
| FI | Pre | 3.0 (1.5 – 9.0) | 3.0 (1.5 – 9.0) | 0.884 | 6.9 ± 5.7 | 6.5 ± 5.0 | 0.84 | |
| Post | 4.0 (1.0 – 8.0) | 5.0 (1.5 – 9.0) | 0.818 | 6.9 ± 6.3 | 5.9 ± 5.1 | 0.637 | ||
| Δ | 0.0(–2.0 – 0.0) | 0.0 (–1.5 – 0.5) | 0.8 | –1.0 (–1.0–1.5) | 0.0 (–0.5 – 1.0) | 0.436 | ||
| TA | Pre | 9.5 ± 5.1 | 9.1 ± 5.7 | 0.814 | 11.3 ± 7.5 | 11.5 ± 4.9 | 0.931 | |
| Post | 8.1 ± 5.3 | 7.0 (3.5 – 10) | 0.812 | 10.4 ± 6.2 | 10.2 ± 4.6 | 0.921 | ||
| Δ | –1.40 ± 3.18 | –1.40 ± 2.69 | 1 | –1.33 ± 2.55 | –0.93 ± 2.37 | 0.66 | ||
| VA | Pre | 10.5 ± 6.2 | 7.9 ± 6.4 | 0.27 | 10.7 ± 5.0 | 11.0 ± 5.4 | 0.862 | |
| Post | 9.7 ± 7.1 | 10.7 ± 7.4 | 0.727 | 8.7 ± 7.1 | 9.4 ± 6.3 | 0.787 | ||
| Δ | 1.0 (–0.5 – 6.0) | 0.0 (–3.0 – 1.0) | 0.079 | –1.0 (–3.0 – 0.5) | –2.0 (–3.5 – 0.0) | 0.489 | ||
| F | Pre | 11.0 (7.0 – 13.5) | 10.0 (8.0 – 11.0) | 0.867 | 10.1 ± 4.1 | 11.8 ± 5.3 | 0.325 | |
| Post | 10.0 (10.0 – 12.0) | 10.0 (9.0 – 12.0) | 0.802 | 9.7 ± 4,6 | 10.7 ± 4.9 | 0.572 | ||
| Δ | 0.0 (–1.0 – 1.5) | 0.0 (–1.0 – 1.5) | 0.899 | –1.0 (–2.0 – 0.0) | 0.0 (–2.5 – 1.0) | 0.706 | ||
| TMD | Pre | 20.3 ± 21.3 | 26.5 ± 25.8 | 0.479 | 29.3 ± 27.5 | 29.1 ± 22.5 | 0.983 | |
| Post | 18.3 ± 19.9 | 19.0 ± 27.6 | 0.934 | 28.2 ± 29.1 | 27.2 ± 22.0 | 0.916 | ||
| Δ | –3.0 (–14.5 – 1.5) | –1.0 (–3.5 – 3.0) | 0.262 | 0.0 (–5.5 – 5.0) | –1.0 (–6.0 – 4.5) | 0.901 | ||
*p<0.05
SBP: systolic blood pressure
DBP: diastolic blood pressure
HR: heart rate
RPE: rating of perceived exertion
EMG: electromyography
iEMG: integrated electromyography
POMS2: Profile of Mood States 2nd Edition
AH: anger-hostility
CB: confusion–bewilderment
DD: depression–dejection
FI: fatigue–inertia
TA: tension–anxiety
VA: vigor–activity
F: friendliness
TMD: total mood disturbance
A positive correlation was observed between the HR during exercise and post-TMD in the lifting VR condition (r=0.64, P<0.05), but not in the lifting control condition. No correlation was found between iEMG and ΔTMD in the rowing VR condition; however, a positive correlation (r=0.56) between iEMG and ΔTMD was found in the rowing control condition (P<0.05) (Table 3). No other significant correlations were observed between the other variables.
Table 3.
The relationship between TMD and HR or iEMG during exercise
| Lifting VR
conditions |
Lifting control
conditions |
Rowing VR
conditions |
Rowing control
conditions |
||
| HR | Post | 0.635* | 0.093 | 0.226 | 0.056 |
| Δ (Post – Pre) | –0.033 | –0.068 | 0.013 | –0.349 | |
| iEMG | Post | –0.263 | 0.201 | –0.2 | 0.345 |
| Δ (Post – Pre) | 0.358 | 0.331 | –0.179 | 0.555* |
*p<0.05
HR: heart rate
iEMG: integrated electromyography
TMD: total mood disturbance
DISCUSSION
This study showed that VR exerts no virtual sickness and discontinuations and affects a higher workout load measured by HR in the VR exercise condition than in the control condition, even though subjective fatigue was comparable to that in the control condition. In addition, this study showed that the effects on the mood of an individual may differ depending on the VR exercise category. VR technology is also an important innovation for operations in busy medical settings.
The effects of exercise therapy with VR have been investigated in various subjects, such as elderly patients with muscle weakness,2 stroke patients for upper limb function training,3 cognitive tasks for dementia patients,4 balance training for traumatic lower limb amputation patients,5 daily living training for cerebral palsy patients,6 and intradialytic exercise for hemodialysis patients.7 Since exercise therapy with VR could enhance the physical feedback on VR, it is difficult to perform exercise therapy, such as game competitions, increase motivation, and are expected to develop. However, exercise therapy for rehabilitation conducted in hospitals is still limited.
Preventing VR sickness is critical in patient applications. There was no significant difference in SSQ between pre and post-VR exercise therapy systems since the cutoff value of SSQ was 33.3 points9; no VR sickness was observed in this VR exercise therapy system. A previous study reported that game designs prone to VR sickness have large sensory conflicts.9 Sensory conflict is the discrepancy between expected sensory input information based on the actual experience and actual sensory input information in terms of sensory correspondence among the visual, auditory, somatosensory, and vestibular sensory information.11 Specific game designs, such as fast-moving stimuli, involvement of three or more axes (X, Y, and Z axes) in the movement, high graphic realism, and implementation time of 10 min or more12 may have to elicit sensory conflict in previous studies. In this game design, both lifting and rowing were performed in 2-axis motion, for a duration of less than 10 min, and with acceleration sensors attached to the legs. Additionally, it is thought that sensory conflict was unlikely to occur, and VR sickness was not observed.
The VR condition resulted in a significantly higher HR than the control condition, although there were no significant differences in the iEMG or RPE compared to the control condition. These results indicate that VR exercise could impose a higher exercise load on the cardiopulmonary system, even if the work for the lower limbs did not differ between conditions. In exercise therapy, an increase in the HR indicates higher exercise performance and a greater exercise load.13 Previous studies have reported that VR improves the performance in exercise stress tests14 and high-intensity interval training.15 The immersive experience and fun of VR focus on sensory feedback, such as exercise-related fatigue.16 Exercise with VR improves the physical performance and mental tension, resulting in increased HR.17 Exercise with high HR may benefit from increased peripheral, cutaneous, cerebral, and coronary blood flow18-20 compared to the control exercise. The VR exercise conditions did not change fatigue compared to the control conditions, and exercise therapy with a higher exercise load on the cardiopulmonary system could be performed, which may be expected to improve the peripheral blood flow associated with an increased HR.
Subjects with a higher exercise load and higher HR were more likely to be in a negative mood only in the VR lifting condition performed as resistance training, not in the control lifting condition. Previous studies have shown that a low-to moderate-intensity training volume (50–70% 1 Repetition Maximum) improves the emotion, anxiety, and mood,21 while high-intensity exercise mainly produces discomfort.22 Thus, resistance exercise with VR tended to increase the negative mood at higher exercise loads compared with the control condition. In contrast, the rowing control condition as aerobic exercise showed a negative effect, which was shown to increase in subjects with higher physical activity, but not in the rowing VR condition. In the control condition, aerobic exercise has been reported to cause an increase in tension, anxiety, and fatigue with higher intensity exercises.23 This previous study supports the results of this control condition. In comparison, the rowing VR condition did not correlate with iEMG and ΔTMD. This mechanism may be due to the enjoyment of VR, which has distracted attention from sensory feedback, such as fatigue from exercise,16 even in subjects with a high exercise load. Aerobic exercise therapy with VR may reduce the negative mood effects of an increased aerobic exercise load.
Exercise therapy using non-immersive VR for hemodialysis patients has increased physical activity24 and improved physical function.25-27 The immersive VR exercise therapy system used in this study was developed with the primary goal of providing intradialytic exercises and hospital use. Because the system uses only VR equipment, it can easily be used at medical institutions with a small number of units. The safety and effectiveness of this system should be verified in hemodialysis patients and inpatients in the future.
This study had some limitations. The subjects of this study were healthy, and further research is needed to adapt the system to patients. In addition, since only one set of exercises was conducted this time, it is necessary to improve the game design by considering the number of sets, exercise types, rest periods, and other exercise prescriptions, and consider increasing the number of types of games.
CONCLUSION
This study examined the safety and effectiveness of a VR exercise therapy system developed for healthy patients during dialysis. The safety was confirmed by the absence of VR sickness or discontinuation of the system. Exercise therapy using VR resulted in a higher exercise load. This VR system has the potential for more effective intradialytic exercises and hospital use.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study protocol complied with the Helsinki Declaration standards and was approved by the Ethical Committee of Seirei Christopher University (approval number 21026). Written informed consent was obtained from the subjects after a detailed explanation of the study objectives.
DATA PRESENTATION
We have presented a subset of our findings at Japanese Society for Technology of Blood purification. It has not been published in entirety and is not under consideration by another journal.
AUTHOR DISCLOSURE STATEMENT
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
FUNDING INFORMATION
The study was not funded.
ACKNOWLEDGEMENTS
We thank members of Seirei Christopher University for participated and measurement.
Abbreviations
- HR
heart rate
- iEMG
integrated electromyography
- SSQ
simulator sickness questionnaire
- VR
virtual reality
REFERENCES
- 1.Zeng N, Pope Z, Gao Z. Acute Effect of Virtual Reality Exercise Bike Games on College Students’ Physiological and Psychological Outcomes. Cyberpsychol Behav Soc Netw. 2017;20(7):453–457. doi: 10.1089/cyber.2017.0042. [DOI] [PubMed]
- 2.de Vries AW, Willaert J, Jonkers I, van Dieën JH, Verschueren SMP. Virtual Reality Balance Games Provide Little Muscular Challenge to Prevent Muscle Weakness in Healthy Older Adults. Games Health J. 2020;9(3):227–236. doi: 10.1089/g4h.2019.0036. [DOI] [PubMed]
- 3.Domínguez-Téllez P, Moral-Muñoz JA, Salazar A, Casado-Fernández E, Lucena-Antón D. Game-Based Virtual Reality Interventions to Improve Upper Limb Motor Function and Quality of Life After Stroke: Systematic Review and Meta-analysis. Games Health J. 2020;9(1):1–10. doi: 10.1089/g4h.2019.0043. [DOI] [PubMed]
- 4.Torpil B, Şahin S, Pekçetin S, Uyanık M. The Effectiveness of a Virtual Reality-Based Intervention on Cognitive Functions in Older Adults with Mild Cognitive Impairment: A Single-Blind, Randomized Controlled Trial. Games Health J. 2021;10(2):109–114. doi: 10.1089/g4h.2020.0086. [DOI] [PubMed]
- 5.Abbas RL, Cooreman D, Al Sultan H, El Nayal M, Saab IM, El Khatib A. The Effect of Adding Virtual Reality Training on Traditional Exercise Program on Balance and Gait in Unilateral, Traumatic Lower Limb Amputee. Games Health J. 2021;10(1):50–56. doi: 10.1089/g4h.2020.0028. [DOI] [PubMed]
- 6.Şahin S, Köse B, Aran OT, Bahadır Ağce Z, Kayıhan H. The effects of virtual reality on motor functions and daily life activities in unilateral spastic cerebral palsy: a single-blind randomized controlled trial. Games Health J. 2020;9(1):45–52. doi: 10.1089/g4h.2019.0020. [DOI] [PubMed]
- 7.Maynard LG, de Menezes DL, Lião NS, et al. Effects of Exercise Training Combined with Virtual Reality in Functionality and Health-Related Quality of Life of Patients on Hemodialysis. Games Health J. 2019;8(5):339–348. doi: 10.1089/g4h.2018.0066. [DOI] [PubMed]
- 8.Kennedy RS, Lane NE, Berbaum KS, Lilienthal MG. Simulator Sickness Questionnaire: An Enhanced Method for Quantifying Simulator Sickness. Int J Aviat Psychol. 1993;3(3):203–220. doi: 10.1207/s15327108ijap0303_3. [DOI]
- 9.Chang E, Kim HT, Byounghyun Y. Virtual reality sickness: a review of causes and measurements. Int J Hum Comput Interact. 2020;36(17):1658–1682. doi: 10.1080/10447318.2020.1778351. [DOI]
- 10.Lin S, Hsiao YY, Wang M. Test Review: The Profile of Mood States 2nd Edition. J Psychoeduc Assess. 2014;32(3):273–277. doi: 10.1177/0734282913505995. [DOI]
- 11.Ng AKT, Chan LKY, Lau HYK. A study of cybersickness and sensory conflict theory using a motion-coupled virtual reality system. Displays. 2020;61:101922. doi: 10.1016/j.displa.2019.08.004. [DOI]
- 12.Saredakis D, Szpak A, Birckhead B, Keage HAD, Rizzo A, Loetscher T. Factors Associated With Virtual Reality Sickness in Head-Mounted Displays: A Systematic Review and Meta-Analysis. Front Hum Neurosci. 2020;14:96. doi: 10.3389/fnhum.2020.00096. [DOI] [PMC free article] [PubMed]
- 13.Yamagata K, Hoshino J, Sugiyama H, et al. Clinical practice guideline for renal rehabilitation: systematic reviews and recommendations of exercise therapies in patients with kidney diseases. Ren Replace Ther. 2019;5(1):28. doi: 10.1186/s41100-019-0209-8. [DOI]
- 14.Rutkowski S, Szary P, Sacha J, Casaburi R. Immersive Virtual Reality Influences Physiologic Responses to Submaximal Exercise: A Randomized, Crossover Trial. Front Physiol. 2021;12:702266. doi: 10.3389/fphys.2021.702266. [DOI] [PMC free article] [PubMed]
- 15.Farrow M, Lutteroth C, Rouse PC, Bilzon JLJ. Virtual-reality exergaming improves performance during high-intensity interval training. Eur J Sport Sci. 2019;19(6):719–727. doi: 10.1080/17461391.2018.1542459. [DOI] [PubMed]
- 16.Wender CLA, Ahn SJ, O’Connor PJ. Interactive Virtual Reality Reduces Quadriceps Pain during High-Intensity Cycling. Med Sci Sports Exerc. 2019;51(10):2088–2097. doi: 10.1249/MSS.0000000000002016. [DOI] [PubMed]
- 17.Perrin T, Faure C, Nay K, et al. Virtual Reality Gaming Elevates Heart Rate but Not Energy Expenditure Compared to Conventional Exercise in Adult Males. Int J Environ Res Public Health. 2019;16(22):4406. doi: 10.3390/ijerph16224406. [DOI] [PMC free article] [PubMed]
- 18.Thomas KN, Kissling LS, Gibbons TD, Akerman AP, van Rij AM, Cotter JD. The acute effect of resistance exercise on limb blood flow. Exp Physiol. 2020;105(12):2099–2109. doi: 10.1113/EP088743. [DOI] [PubMed]
- 19.Ogoh S, Ainslie PN. Regulatory mechanisms of cerebral blood flow during exercise: new concepts. Exerc Sport Sci Rev. 2009;37(3):123–129. doi: 10.1097/JES.0b013e3181aa64d7. [DOI] [PubMed]
- 20.Duncker DJ, Bache RJ. Regulation of coronary blood flow during exercise. Physiol Rev. 2008;88(3):1009–1086. doi: 10.1152/physrev.00045.2006. [DOI] [PubMed]
- 21.Cavarretta DJ, Hall EE, Bixby WR. The acute effects of resistance exercise on affect, anxiety, and mood—Practical implications for designing resistance training programs. IntRev Sport Exerc Psychol. 2019;12(1):295–324. doi: 10.1080/1750984X.2018.1474941. [DOI]
- 22.Arent SM, Landers DM, Matt KS, Etnier JL. Dose-response and mechanistic issues in the resistance training and affect relationship. J Sport Exerc Psychol. 2005;27(1):92–110. doi: 10.1123/jsep.27.1.92. [DOI]
- 23.Steptoe A, Cox S. Acute effects of aerobic exercise on mood. Health Psychol. 1988;7(4):329–340. doi: 10.1037/0278-6133.7.4.329. [DOI] [PubMed]
- 24.Segura-Ortí E, García-Testal A. Intradialytic virtual reality exercise: Increasing physical activity through technology. Semin Dial. 2019;32(4):331–335. doi: 10.1111/sdi.12788. [DOI] [PubMed]
- 25.Segura-Ortí E, Pérez-Domínguez B, Ortega-Pérez de Villar L, et al. Virtual reality exercise intradialysis to improve physical function: A feasibility randomized trial. Scand J Med Sci Sports. 2019;29(1):89–94. doi: 10.1111/sms.13304. [DOI] [PubMed]
- 26.Martínez-Olmos FJ, Gómez-Conesa AA, García-Testal A, et al. An intradialytic non-immersive virtual reality exercise program: a crossover randomized controlled trial. Nephrol Dial Transplant. 2022;37(7):1366–1374. doi: 10.1093/ndt/gfab213. [DOI] [PubMed]
- 27.Cho H, Sohng KY. The effect of a virtual reality exercise program on physical fitness, body composition, and fatigue in hemodialysis patients. J Phys Ther Sci. 2014;26(10):1661–1665. doi: 10.1589/jpts.26.1661. [DOI] [PMC free article] [PubMed]