Abstract
Background
Digital tools like digital box trainers and VR seem promising in delivering safe and tailored practice opportunities outside of the surgical clinic, yet understanding their efficacy and limitations is essential. This study investigated Which digital tools are available to train surgical skills, How these tools are used, How effective they are, and What skills they are intended to teach.
Methods
Medline, Embase, and Cochrane libraries were systematically reviewed for randomized trials, evaluating digital skill-training tools based on objective outcomes (skills scores and completion time) in surgical residents. Digital tools effectiveness were compared against controls, wet/dry lab training, and other digital tools. Tool and training factors subgroups were analysed, and studies were assessed on their primary outcomes: technical and/or non-technical.
Results
The 33 included studies involved 927 residents and six digital tools; digital box trainers, (immersive) virtual reality (VR) trainers, robot surgery trainers, coaching and feedback, and serious games. Digital tools outperformed controls in skill scores (SMD 1.66 [1.06, 2.25], P < 0.00001, I2 = 83 %) and completion time (SMD -1.05 [−1.72, −0.38], P = 0.0001, I2 = 71 %). There were no significant differences between digital tools and lab training, between tools, or in other subgroups. Only two studies focussed on non-technical skills.
Conclusion
While the efficacy of digital tools in enhancing technical surgical skills is evident - especially for VR-trainers -, there is a lack of evidence regarding non-technical skills, and need to improve methodological robustness of research on new (digital) tools before they are implemented in curricula.
Key message
This study provides critical insight into the increasing presence of digital tools in surgical training, demonstrating their usefulness while identifying current challenges, especially regarding methodological robustness and inattention to non-technical skills.
Keywords: Residency, Skills, Training, Digital training, Systematic review, Meta-analysis
Highlights
-
•
There are six digital tools available to train surgical skills
-
•
Digital tools’ effectivity is comparable to training in a wet/dry lab and more effective compared to a control group
-
•
Most evidence is available for VR trainers which are equally effective as box trainers and training in a wet/dry lab
-
•
The methodological robustness of studies needs to improve, before digital tools are utilized based on educational research
-
•
Unlike technical skills, evidence on training non-technical skills digitally is lacking, revealing an educational blind spot.
Introduction
Surgical residents need sufficient clinical training experiences to develop their skills, achieve proficiency, and ultimately become competent surgeons. While clinical training is critical to achieve these goals, it is affected by available case-load, exposure, and most importantly, patient safety [1,2]. As a result, residents also need training outside of the daily clinical practice and operating rooms (OR) which can be tailored to their educational needs, and provide them with the opportunity to practice and learn from mistakes without endangering patients [3,4].
Digital tools, such as virtual reality (VR), digital box trainers, and applications for mobile platforms (apps), can provide these training opportunities, and are increasingly used by surgical educators – especially since the COVID-19 pandemic [[5], [6], [7], [8], [9]]. There are myriad studies that introduce or validate a digital tool, and several reviews which evaluate these tools based on the technology used [[10], [11], [12], [13], [14]]. However, before these tools are implemented in surgical curricula and relied on to improve training, an overview of available tools, their merits, and the skills they aim to train is essential – and currently missing.
Technical skills are an important aspect of surgical training, well incorporated in surgical curricula, and widely discussed in literature. Conversely, although non-technical skills have been shown to negatively affect performance and surgical outcome, they are often regarded as being more difficult to identify and teach [[15], [16], [17], [18], [19]]. Therefore, this systematic review and meta-analysis aims to answer the following three questions: Which digital tools are available to train surgical skills and what is their efficacy, How are these tools used, and What skills (technical and/or non-technical) do these tools aim to train?
Material and methods
This systematic review and meta-analysis was performed in accordance with the Cochrane Handbook for Systematic Reviews of Interventions version 6.0 and PRISMA-guidelines [20,21].
Literature search
MEDLINE, EMBASE, and Cochrane databases were reviewed for studies assessing digital skill training tools for surgical residents, published since January 1st 2010 up until the last search update of December 7th, 2022. Keywords related to digital training, skills, and competencies were incorporated in the search, the full search can be found in the Supplementary Material. Included articles were cross-referenced for additional relevant studies. Digital training was defined according to the European Commission definition: the pedagogical use of digital technologies to support and enhance learning, teaching and assessment [22]. Skills were defined according to Merriam-Webster dictionary: “a learned power of doing something competently: a developed aptitude or ability” [23].
Randomized clinical trials (RCTs) were included in this review to attain the highest level of evidence and to enable comparison of digital tools. RCTs were eligible if they were published in Dutch or English, assessed digital training tools aimed at skill acquisition, and used objective performance indicators such as computed metrics or scoring tools. Studies which used subjective outcomes, such as participant questionnaires or self-evaluation tools, were excluded. Additionally, studies reporting on conference proceedings, study protocols, and studies which evaluated multiple digital tools without assessing each source separately were excluded. Two authors (TM and SvdS) assessed all titles and abstracts and included studies for full-text appraisal when both reviewers agreed on inclusion. Disagreements were resolved by consulting a third reviewer (MPS). A standardized form was used to systematically extract data from the studies including; trained skills, study design, characteristics of participants and digital tools, addressed skills, outcomes, and factors affecting the efficacy of the training tool.
Data analysis and synthesis
Tool availability, efficacy, and use
Studies were categorized according to the digital tool they examined. Overall efficacy was evaluated through meta-analyses of post-test outcomes on skill scores (checklist scores and computed metrics) and time (task completion time). Based on these data, digital tools were compared with a control group (receiving traditional and/or no additional training), and with training in a wet or dry lab. Within these comparisons, subgroups were created based on the studied digital tool to evaluate the efficacy of individual tools and the heterogeneity therein. If sufficient studies were available, digital tools were compared to other digital tools. To examine how the utilization factors of digital tools affected outcomes, study data were pooled according to their training structure (self-directed versus prescribed training or training to proficiency) and training duration (minutes-days versus weeks-months).
Meta-analyses on pooled data were performed using Cochrane's Review Manager (RevMan) 5.4 [24]. All extracted data were converted to standardized mean differences (Hedges g effect size). When mean and standard deviation(SD) were not available, reported outcomes (p-values, median, range, P-value, and 95 % Confidence Interval (CI)) were used to estimate the effect size. If none of these data were provided, a study was excluded from the meta-analysis. A random-effects model was used in al analyses due to expected methodological (arising from the broad literature search) and statistical heterogeneity, which was quantified by calculating the I2 statistic. Effect sizes were presented with 95 % CI's and deemed significant if P < 0.05. Because this review presents the minimally available evidence, outcomes of meta-analyses were reported even in the light of high heterogeneity [21].
Skills trained using digital tools
Studies were evaluated based on the skills they primarily aim to train: technical skills, general non-technical competencies (according to the CanMEDS framework), and non-technical surgical skills (according to the NOTSS taxonomy) [25,26]. The CanMEDS framework identifies seven competencies (roles) each physician should master, based on the needs of the people they serve. The Medical Expert is identified as the role in which the six intrinsic roles are integrated: the Communicator, Collaborator, Leader, Health Advocate, Scholar, and Professional roles. The framework provides key- and enabling competencies, which were used to assess reported outcome measures in this review. The NOTSS taxonomy is aimed specifically at non-technical skills in the OR. The taxonomy defines four skill categories (situation awareness, decision making, communication & teamwork, and leadership), which are all subdivided in three elements. The NOTSS system handbook described these categories and elements in-depth, and was used to assess the primary outcome measures in this review [27]. A graphical overview of the CanMEDS framework roles and NOTSS taxonomy categories can be found in Table 1. TMF and SvdS evaluated which skills were trained in the study, and whether this skill was included as the primary outcome of the study or assessed in any way by the authors.
Table 1.
Definition of the seven CanMEDS roles and four NOTSS competencies.
| CanMEDS | Medical expert | Integrating all of the CanMEDS Roles in the provision of high-quality and safe patient-centred care |
| Communicator | Forming relationships with patients and their families that facilitate the gathering and sharing of essential information for effective health care | |
| Collaborator | Working effectively with other health care professionals to provide safe, high-quality, patient-centred care | |
| Leader | Engaging with others to contribute to a vision of a high-quality health care system and take responsibility for the delivery of excellent patient care | |
| Health Advocate | Working with those they serve to determine and understand needs, speak on behalf of others when required, and support the mobilization of resources to effect change | |
| Scholar | Demonstrating a lifelong commitment to excellence in practice through continuous learning and by teaching others, evaluating evidence, and contributing to scholarship | |
| Professional | Commitment to the health and well-being of individual patients and society through ethical practice, high personal standards of behaviour, accountability to the profession and society, physician-led regulation, and maintenance of personal health | |
| NOTTS | Situation awareness | Developing and maintaining a dynamic awareness of the situation in OR. Elements are gathering information, understanding information, and projecting and anticipating future state |
| Decision making | Diagnosing the situation and reaching a judgement in order to choose an appropriate course of action. Elements are: considering options, selecting and communicating options, implementing and reviewing decisions | |
| Communication and teamwork | Working to ensure that the team has an acceptable shared picture of the situation and can complete tasks effectively. Elements are: exchanging information, establishing a shared understanding, coordinating team activities | |
| Leadership | Providing directions to the team, demonstrating high standards of clinical practice and care, and being considerate about the needs of individual team members. Elements are: setting and maintaining standards, supporting others, and coping with pressure |
Methodological quality and bias
The methodological quality of the included studies was assessed using the revised Cochrane risk of bias tool for randomized trials (RoB 2 tool), which determines an overall risk of bias of randomized trials based on five bias domains; selection of reported result, measurement of outcome, missing outcome data, deviations from intended interventions, and randomization process [28].
Results
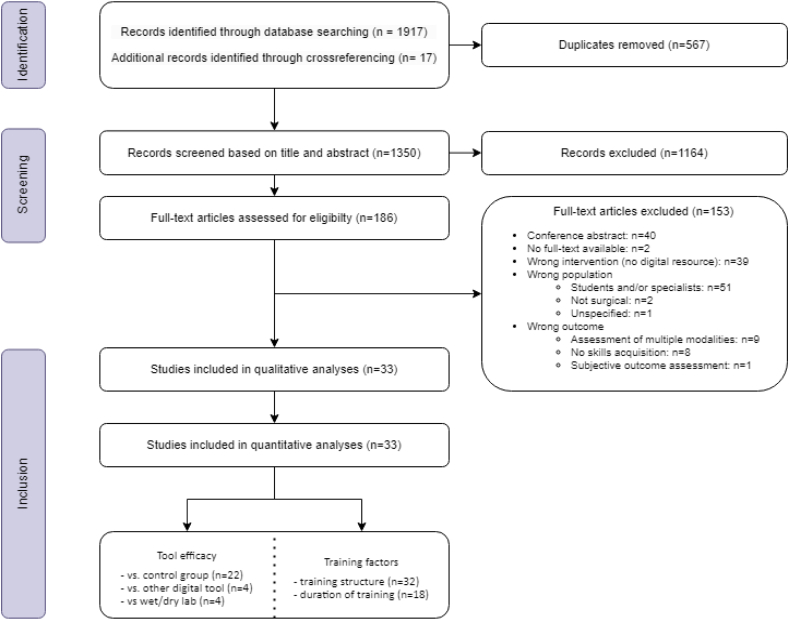
Eighteen hundred and fifty-one studies were screened based on title and abstract. A total of 178 full-texts were reviewed, resulting in the inclusion of 33 studies comprising 927 residents [[29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61]]. .Fig. 1 depicts the PRISMA flow diagram of included studies and Table 2 summarizes the study characteristics and describes demographics, study setting, and intervention protocols.
Fig. 1.
PRISMA flow diagram of included studies.
Table 2.
Characteristics of included studies.
| Author | Year | Country | Participants |
Tools |
Assessed skills |
|||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No | % female | Specialty | Level / experience (%) | Intervention(s) | Control | Other | Technical | CanMEDSa | NOTSSa | |||
| Ahlborg [29] | 2013 | Sweden | 19 | NS | Obstetrics and Gynaecology | Not specified | VR trainer | No additional training | Tubal occlusions | – | – | |
| Akdemir [30] | 2014 | Turkey | 60 | 25 % | Gynaecology | PGY 1 and 2 | VR trainer | No additional training | Analogue box-trainer | Bilateral Tubal Ligation | – | (Decision making) |
| Araujo [31] | 2014 | Brazil | 14 | 14,3 % | Surgery | No experience with laparoscopic colectomy | VR trainer | No additional training | Laparoscopic skills | – | (Decision making) | |
| Borahay [32] | 2013 | USA | 16 | 83,3 % | Obstetrics and Gynaecology | 8 PGY 1 8 PGY 2 |
Robot trainer | Analogue box-trainer | Laparoscopic skills | – | – | |
| Brown [33] | 2017 | USA | 26 | NS | 10 General surgery, 7 Urology, 9 Obstetrics and Gynaecology |
8 PGY 1 (30,1 %) 5 PGY 2 (19,2 %) 6 PGY 3 (23,1 %) 5 PGY 4 (19,2 %) 2 PGY 5 (7,7 %) |
2 robot trainers | Basic robotic surgery skills | – | – | ||
| Camp [34] | 2016 | USA | 57 | NS | Orthopaedic surgery | 9 PGY 1 (15,8 %) 12 PGY 2 (21,1 %) 6 PGY 3 (10,6 %) 9 PGY 4 (15,8 %) 9 PGY 5 (15,8 %) |
VR trainer | No additional training | Cadaver training | Arthroscopy | – | (Decision making) |
| Cannon [35] | 2014 | USA | 48 | NS | Orthopaedic surgery | PGY 3 | VR trainer | No additional training | Arthroscopy | – | – | |
| Daly [36] | 2013 | USA | 21 | NS | Ophthalmology | PGY 2 | VR trainer | Wet lab training | Cataract surgery | – | – | |
| Dickerson [37] | 2019 | USA | 42 | 26,2 % | Orthopaedic surgery | PGY 1–5 (mean PGY 2.3–2.7) |
Post-op coaching session with POV-video of surgery | Post-op coaching session without POV-video of surgery | Intra-articular distal tibial fracture reduction | (Collaborator) | (Decision making) | |
| Fried [38] | 2010 | USA | 25 | NS | Ear Nose Throat surgery | PGY 1–2 | VR trainer | “Access to conventional material” | Endoscopic Sinus Surgery | (Communication and Teamwork) | ||
| Garfjeld Roberts [39] | 2019 | UK | 28 | 46,7 % | Trauma / orthopaedic surgery | 24 PGY 2 (80 %) 6 PGY 3 (20 %) |
Box trainer | “Normal deanery-provided training” | Knee arthroscopy | (Collaborator) | (Decision making) | |
| Graafland [40] | 2017 | Netherlands | 31 | 41.7 % | General surgery | 3 PGY 1 (9,7 %) 20 PGY 2 (64,5 %) 1 PGY 3 (3,2 %) |
Basic laparoscopic training course with serious game | Basic laparoscopic training course without serious game | Situational awareness in OR | (Communication and Teamwork) | ||
| Hauschild [41] | 2021 | USA | 38 | NS | Orthopaedic surgery | PGY 1–5 | VR trainer | Dry lab training | Shoulder arthroscopy | – | – | |
| Hooper [42] | 2019 | USA | 14 | 35.7 % | Orthopaedic surgery | PGY 1 | Immersive VR trainer | “Standard study materials” | Shoulder Arthroscopy | – | Situation awareness | |
| Hou [43] | 2018 | China | 10 | 40 % | NS | No experience | VR trainer | “Traditional teaching method” | Cervical pedicle screw placement | – | (Decision making) | |
| Huri [44] | 2020 | Turkey | 34 | 0 % | Orthopaedic surgery | NS | VR trainer | Cadaver training | Shoulder Arthroscopy | (Collaborator) | (Decision making) | |
| Jensen [45] | 2014 | Denmark | 30 | 64.3 % | Urology, General surgery, Cardiothoracic surgery, Orthopaedic surgery | NS | VR trainer | Analogue box trainer | Shoulder Arthroscopy | (Communication and Teamwork) | ||
| Kantar [46] | 2020 | USA | 13 | 23.1 % | Plastic Surgery | 3 PGY 1 (23,1 %) 3 PGY2 (23,1 %) 3 PGY 3 (23,1 %) 4 PGY 4 (30,8 %) |
VR trainer | Learning from text-book | Unilateral cleft lip repair | – | – | |
| Korets [47] | 2011 | USA | 16 | NS | Urology | 10 PGY 1–3 (62,5 %) 6 PGY 4–5 (37,5 %) |
Robot trainer with digital coaching vs. robot trainer with mentor | No additional training | Basic surgical skills | – | – | |
| Korndorffer [48] | 2012 | USA | 20 | 50 % (80 % digital, 20 % analogue) | General Surgery | PGY 1–5 (mean PGY 2.3–2.8) |
Digital boxtrainer | Analogue boxtrainer | Basic laparoscopic skills | – | – | |
| Kun [49] | 2019 | China | 50 | 54 % | NS | PGY 2–3 | Robot trainer with self-coaching with exercise videos | Robot trainer with self-coaching without videos of the exercise | Basic Robotic skills | (Collaborator) | (Decision making) | |
| Logishetty [50] | 2019 | UK | 28 | 29,2 % | Surgery Orthopaedic surgery | PGY 3–5 | Immersive VR trainer | “Conventional preparatory materials” | Total hip arthroplasty | (Communication and Teamwork) | ||
| Lohre [51] | 2020 | Canada | 16 | NS | Orthopaedic surgery | 6 PGY 4 (37,5 %) 10 PGY 5 (62,5) |
Immersive VR trainer | “Traditional learning using a technical journal article” | Shoulder arthroplasty | (Collaborator) | (Decision making) | |
| McKinney [61] | 2022 | USA | 22 | NS | Orthopaedic surgery | 7 PGY 1 (31,8 %) 7 PGY 2 (31,8 %) 3 PGY 3 (13,6 %) 3 PGY 4 (13,6 %) 2 PGY 5 (9,1 %) |
Immersive VR trainer | “Reading the technique guide” | Knee arthroplasty | – | (Decision making) | |
| Orzech [52] | 2012 | Canada | 24 | NS | General Surgery | PGY >2, median PGY 2.6–3.2 | VR trainer | Analogue boxtrainer | Advanced laparoscopic skills | (Communication and Teamwork) | ||
| Palter [53] | 2013 | Canada | 16 | NS | General Surgery | 14 PGY 1 (87,5 %) 2 PGY 2 (12,5 %) |
VR trainer | Normal residency curriculum, without additional training. | Basic laparoscopic skills Laparoscopic cholecystectomy |
– | – | |
| Sharifzadeh [60] | 2021 | Iran | 46 | 100 % | Obstetrics and Gynaecology | PGY 2–3 | Serious game | No additional training | Basic ynaecological skills | – | (Decision making) | |
| Sloth [54] | 2021 | Denmark | 46 | 69,6 % | General surgery Urology Gynaecology |
PGY 1, no previous simulation training, <50 supervised laparoscopic procedures | Digital boxtrainer at home vs digital boxtrainer in hospital | Intracorporeal suturing | – | – | ||
| Valdis [55] | 2016 | Canada | 40 | 30 % | General Surgery | < 10 h on robotic surgical simulator, mean year of training: 4–5 | VR trainer | No additional training | Wet lab training Dry lab training |
Basic robotic skills | (Decision Making) | |
| van Det [56] | 2011 | Netherlands | 10 | NS | General Surgery | No experience with laparoscopic surgery | Video-enhanced intraoperative feedback | Traditional intraoperative feedback | Nissen fundoplication | (Communication and Teamwork) | ||
| Varras [57] | 2020 | Greece | 20 | 45 % | Obstetrics and Gynaecology | < 10 laparoscopic surgeries, no experience with VR simulators | Digital boxtrainer VR trainer |
Basic laparoscopic skills | – | Decision making | ||
| Waterman [58] | 2016 | USA | 22 | 4,5 % | Orthopaedic surgery | PGY 1–4, median PGY 3.0 | VR trainer | “Standard practice” | Basic laparoscopic skills | (Collaborator) | (Decision making) | |
| Yiasemidou [59] | 2017 | UK | 25 | NS | General Surgery | ST3-ST4, <15 laparoscopic cholecystectomies as primary surgeon | VR trainer | Analogue box trainer | Laparoscopic cholecystectomy | (Communication and Teamwork) | ||
When non-technical skills are presented between brackets, they were assessed by the authors but outcomes specific for that non-technical skill are not presented in the manuscript.
Study characteristics and available tools
The 33 included studies addressed six digital tools;
-
1.
Digital box trainers (n = 4, 12.1 %): Training box with a camera, instruments and training exercises, enhanced by digital computations of performance metrics.
-
2.
Virtual Reality (VR) trainers (n = 18, 54.5 %): Computer- and screen-based software and hardware, which mimics surgical environments.
-
3.
Immersive VR trainers (n = 4, 12.1 %): Computer-based system, which combines a VR-headset and handheld consoles to interact with digital surroundings.
-
4.
Robot surgery trainers (n = 4, 12.1 %): Computer- and screen-based software and hardware, training robotic skills completely digital or in combination with analogue exercises.
-
5.
Coaching and feedback (n = 5, 15.1 %): Tool which provides feedback on performed exercises, either by enabling recording and (re-)viewing of the exercise, or by analysing computed exercise metrics.
-
6.
Serious games (n = 2, 6.1 %): “An interactive computer application … that has a challenging goal, is fun to play and engaging, incorporates some kind of scoring mechanism, and supplies the user with skills, knowledge or attitudes useful in reality” [62].
Digital tools versus a control group
Twenty-three (70 %) studies compared digital tools with a control group which received traditional and/or no additional training [[29], [30], [31],34,35,[37], [38], [39], [40],42,43,46,47,[50], [51], [52], [53],55,56,58,60,61]. Seventeen of these were included in the meta-analysis based on skills [30,31,34,35,42,46,[50], [51], [52], [53],58,61] and nine were included in the meta-analysis based on time [29,30,34,38,39,[50], [51], [52],58]. In these analyses (Fig. 2, Fig. 3), residents using digital tools achieved higher skill scores (SMD 1.66[1.06, 2.25], P < 0.00001, I2 = 83 %) and required less time (SMD -1.05 [−1.72, −0.38], P = 0.0001, I2 = 71 %) than residents in a control group – although individual effect sizes varied widely and heterogeneity for both outcomes was high.
Fig. 2.
a: Effects of digital tools versus controls on skill outcomes
b: Effects of digital tools versus controls on time outcomes.
Fig. 3.
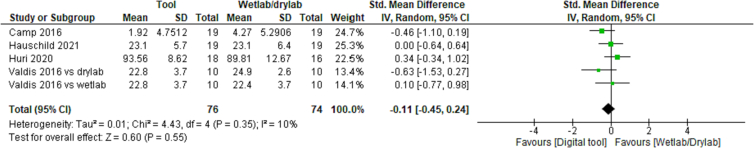
Effects of digital tools versus wet and dry lab on skill scores.
Digital tools compared to wet lab and dry lab training
Of all studies, four (12.5 %) studies compared a digital tool with training in a wet and/or dry lab; three compared a VR trainer with wet/dry lab training [34,41,44]. Valdis et al. compared a robot trainer with training in both a wet lab and a dry lab [55]. .As depicted in Fig. 3, digital tools were equally effective with regard to skill scores (SMD -0.11 [−0.45, 0.24], P = 0.55, I2 = 10 %). Insufficient data was available to perform a comparison on skill completion time.
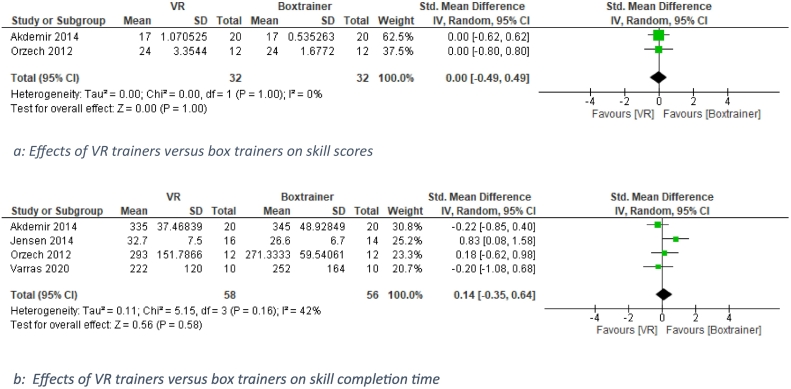
Comparison of different tools: VR-trainer versus box trainers
Four of the five (15.2 %) studies which compared a VR trainer with a box trainer were included in the analysis [30,45,48,52,57,59]. As depicted in Fig. 4, there were no significant differences between VR and box trainers in skills score (n = 2, SMD 0.00 [−0.49, 0.49], P = 1.00, I2 = 0 %) and skill completion time (N = 4, SMD 0.14 [−0.35, 0.64]. P = 0.58, I2 = 42 %).
Fig. 4.
a: Effects of VR trainers versus box trainers on skill scores.
b: Effects of VR trainers versus box trainers on skill completion time.
Subgroup analyses
Results of subgroup analyses are presented in Table 3, individual Forest-plots can be found in supplemental Figs. 2–7.
Table 3.
Meta-analysis of subgroup analyses on skill scores and performance time.
| Number of studies | SMD [95 % CI] | P-value | I2-value | |
|---|---|---|---|---|
| Tool subgroups | ||||
| Vs. control group - skill score | ||||
| Overall test for differences | 16 | 0.32 | 15.1 % | |
| VR trainer | 8 | 1.63 [0.72, 2.54] | 0.0004 | 87 % |
| Immersive VR trainer | 4 | 1.56 [−0.42, 3.54] | 0.12 | 91 % |
| Robot trainer | 2 | 1.89 [0.22, 3.56] | 0.03 | 70 % |
| Coaching and Feedback tool | 2 | 2.24 [1.03, 3.46] | 0.0003 | 0 % |
| Serious game | 1 | – | – | – |
| Vs control group – performance time | ||||
| Overall test for differences | 9 | 0.93 | 0 % | |
| Digital box trainer | 1 | – | – | – |
| VR trainer | 6 | -1.07 [−1.87, −0.28] | 0.008 | 80 % |
| Immersive VR trainer | 2 | −1.05 [−1.72, −0.38] | 0.0.002 | 0 % |
| Trainings factors subgroups | ||||
| Training structure | ||||
| Skill score (vs control group) | 17 | 0.06 | 70.7 % | |
| Prescribed | 10 | 2.03 [1.02, 3.04] | <0.00001 | 88 % |
| Self-directed | 7 | 1.06 [0.45,1.68] | 0.0007 | 63 % |
| Performance time (vs control group) | 9 | 0.36 | 0 % | |
| Prescribed | 6 | −1.21 [−1.88, −0.54] | 0.0004 | 62 % |
| Self-directed | 3 | −0.68 [−1.59, 0.22] | 0.14 | 72 % |
| Training duration | ||||
| Skill score (vs control group) | 16 | 0.06 | 70.7 % | |
| Hours-days | 9 | 1.11 [0.47, 1.75] | 0.0006 | 74 % |
| Weeks-months | 7 | 2.38 [1.19, 3.58] | <0.0001 | 88 % |
| Performance time (vs control group) | 6 | 0.10 | 64.1 % | |
| Hours-days | 2 | −0.21 [−1.05, 0.62] | 0.61 | 38 % |
| Weeks-months | 4 | −1.12 [−1.79, −0.46] | 0.0009 | 62 % |
Tool subgroups
Heterogeneity in outcomes of digital tools versus a control group is not explained by the different tools. There were no significant differences between subgroups in skill scores (P = 0.32, I2 = 15.1 %) and task completion time (P = 0.93, I2 = 0 %). Significant pooled effects of the tools on skill scores were observed for VR trainers (Skills: SMD 1.63 [0.72, 2.54], P < 0.00001, I2 = 87 %, time: SMD −1.07 [−1.87, −0.28], P = 0.0008, I2 = 80 %), robot trainers (skill: SMD 1.89 [0.22, 3.56], P = 0.03, I2 = 70 %), and coaching and feedback tools (skill: SMD 2.24 [1.03, 3.46], P = 0.0003, I2 = 0 %) – yet heterogeneity was a high for most of these outcomes. While pooled effects of using an immersive VR trainers were highly heterogeneous and not significant with regard to skills (SMD 1.56 [−0.42, 3.54], P = 0.12, I2 = 91 %), pooled effects on time were significant in the two studies assessing these outcomes (SMD 1.63 [0.72, 2.54], P < 0.00001, I2 = 87 %). Insufficient data was available for digital skills trainers and serious games.
Training factors subgroups
Differences in training structure and training duration do not explain the heterogeneity in outcomes of digital tools versus a control group. Studies using a prescribed training structure (i.e. training for a defined amount of time or training to proficiency), achieved slightly higher final scores an needed slightly less time – but differences with a studies using a self-directed approach to using the digital tool were not significant (skill subgroup differences: P = 0.11, I2 = 61 %), time subgroup differences: P = 0.36, I2 = 0 %). The same differences were observed for pooled results based on training duration (hours to days versus weeks to months); while there were small differences between subgroup outcomes these differences were not significant (skill subgroup differences: P = 0.06, I2 = 70.7 %), time subgroup differences: P = 0.10, I2 = 64.1 %).
Assessed skills
Only Graafland et al. and Lohre et al. used non-technical skills in their primary outcomes; situation awareness and decision making, both within the NOTSS framework (Fig. 5) [40,51]. Components of the ‘Medical Expert’ and ‘Scholar’ CanMEDS roles overlapped with technical skills trained and measured by all other studies. Fifteen (54.5 %) studies used skills checklists, such as the OSATS (Objective Structured Assessment of Technical Skills), ASSET (Arthroscopic Surgical Skill Evaluation Tool), and GOALS (Global Operative Assessment of Laparoscopic Skills). These checklists include non-technical skills such as “use of assistants” and “flow of operation and forward planning” – which were assigned to the “collaborator” role within CanMEDS, and “situation awareness”, “communication and teamwork”, and “decision making” components within NOTSS. However, none of these studies reported on the non-technical skills item in their outcomes [30,31,34,37,41,42,46,47,50,52,53,56,58,60,61]. The NOTSS component ‘Leadership’ and the CanMEDS roles ‘Leader’, ‘Communicator’, ‘Health Advocate’ and ‘Professional’ were not reported or measured by any study.
Fig. 5.
CanMEDS roles and NOTSS components in included studies.
Methodological quality of included studies
There were only two studies with an overall low risk of bias (Supplemental fig. 8) [39,57]. All other studies had at least some concerns as they suffer from the lack of a pre-specified study protocol (n = 30), insufficient specification of the randomization process and/or insufficiently blinded outcome assessors (n = 27).
Discussion
Research, development, and implementation of digital training tools for surgical residents has increased substantially in recent years, and has gained much attention during the COVID-19 pandemic. This systematic review and meta-analysis reveals that digital tools are widely and readily available, that most evidence is available for VR trainers, and that very few studies address non-technical skills. Most digital tools had positive effects on skill scores and performance time when compared to a control group, and significant effects of training factors were not observed in this study. While this study presents the best available evidence, caution is needed in interpreting these results due to high associated (>70 %) heterogeneity.
In this light, there are two results which can be interpreted with more certainty; VR trainers were equally effective as using a box trainer and as training in a wet or dry lab in this review. While the first outcome is accordance with earlier systematic reviews, no precedent of the latter is available in current literature [13]. Based on these results, box trainers, VR trainers and wet/dry labs are all valid training methods, yet there are differences to consider; wet/dry labs perform better with regard to training efficiency (the speed in which new skills are acquired), but do not have the advantage of training in your own time that the two digital tools have [34,55]. Box trainers are widely available in different configurations and from different manufacturers, are probably the least costly training tool of the three, yet are often primarily aimed at novices [52,63]. When the aim is to support residents in working more autonomously, clinically relevant training tools (such as wet/dry labs or VR trainers) may be necessary before the skills can be transferred to the OR [64]. VR-training does not have these disadvantages, but can be expensive and time consuming to develop [52]. Therefore, it is worth it to consider if there appropriate VR-systems are available, before deciding to develop a new system for a training objective.
Most studies in this review compared a digital tool with a control-group (receiving no additional training). While comparing an intervention with a placebo is a common and useful methodology in studies that evaluate medical interventions, this approach introduces several problems when it is used in educational research. Many digital tools had to be used in a structured way, dedicated time was provided, and the effects of their use was evaluated, while the control group received no additional training and none of this attention. While we believe embedding digital tools is of the utmost important to optimize their use, this difference in the provision of the intervention in this approach is problematic for the validity of the results. In essence, what all of these studies prove is that if resident training is monitored, skills will likely improve. Due to inherently introduced attention bias, it is unclear whether this effect originates from the digital tool itself or from the imposed training. A remarkable example of this is the study of Adams et al., who observed that it is more effective for technical skills acquisition to train on a gaming console than on a box trainer, provided that more hours are trained [65]. In subgroup analysis we therefore aimed to evaluate the effects of training structure and duration. While we found suggestions of differences in training effects of these factors, the effects were not significant and associated heterogeneity was high. While this makes it challenging to interpret outcomes, it clearly reveals the need to improve the quality of research on digital tools. “Proving” that a digital tool works in a study with these biases and unclarity should not be enough support to implement and adopt the tool in surgical curricula – let alone to use it as a way to improve training and its' efficiency.
We therefore highly advocate improving the robustness of studies on digital tools. A start would be to adhere to reporting guidelines (most studies suffered from overall risk of bias due to the lack of a protocol and information on randomization), and diminishing the effects of attention bias by providing equal training schedules to all interventions. Exemplary are the immersive VR studies which all compared the intervention with the reading of textbooks and journals [42,50,51,61]. When comparing these studies with the study by Orzech et al. [52] – who compared a box trainer with a VR trainer and with training in the OR, including a cost-analysis – the external validity and meaningfulness of the results of the latter are evident.
In recent years, it has become clear that a surgeon lacking non-technical skills, affects not only the performance in surgical teams, but may lead to avoidable incidents, and thus impact postoperative outcome [[15], [16], [17], [18],66]. However, there is little focus on teaching and evaluating non-technical skills [67]. No digital tools could be identified in this review, yet it seems improbable that these non-technical skills are not trained at all. Attitudes and non-technical skills are more likely to be trained on the job itself, or using non-digital simulation [68,69]. Yet there is no reason other than the blind-spot of the developer or educator not to develop tools to support both technical and non-technical skill, or not to evaluate the effect of digital resources on non-technical skills with the same objective methodology as their technical equivalent [67,70,71]. Promising technologies to this regard are VR, AR (augmented reality), MR (mixed reality) and telementoring solutions; as well as use of the Metaverse and medical data recorders in the OR. VR, AR and MR training have shown to increase both knowledge and motivation, and to provide insight in work ethics, personality, and communication skills of various trainees in medicine [72,73]. Additionally, telementoring can support both mentee and mentor, and reduce the strain of giving written feedback. Use of data output coming from a medical data recorder may help to qualify and, upon analysis, improve non-technical skills performance of surgical teams. It is known that using such a system benefits surgical teams and influences human factors that relate positively to performance of surgery [17,74].
Increasing scientific data related to the question if, and how, digital tools can help enhance the skills and traits as described in the intrinsic CanMEDS roles and NOTSS would be a first step [67]. Upcoming innovative educational tools such as virtual rounds, video-based learning, livestreamed surgical cases, Artificial Intelligence-based analysis of surgical performances, and many others tools and resources may prove invaluable in surgical resident training in the future [[75], [76], [77], [78]]. It is therefore up to surgical educators and residents to stay on top of these innovations and identify training requirements, thereby targeting specific didactic needs and providing a tailored education.
A possible approach to support digital training of non-technical skills in surgery is to follow the introduction template of the OSATS-checklist back in 1996 [79,80]. Projection of the OSATS approach onto the CanMEDS roles and NOTSS skills requires explication into standardized, measurable non-technical skill indicators – specific to surgical practice. An initial step would be to implement non-technical scoring systems digitally into surgical curricula. The result of combining this non-technical skills checklist with technical skills assessments such as the OSATS, will be a more comprehensive overall surgical skills assessment of the resident. Currently, new systems are being developed to digitally advance education and evaluation of technical and non-technical skills, such as use of the OR Black Box™ outcome report in which the rating scales are embedded, and immersive VR and MR training systems [74,81,82].
There are several limitations to this study. Included studies suffered from variation in study methodology, overall risk of bias and heterogeneity, and most studies suffered from confounding of novelty, availability, attention, and/or compliance – to name a few. While the meta-analyses are therefore of suboptimal value, we chose to perform them nevertheless to provide the best available evidence and reveal its limitations. Including studies which report on subjective outcomes may have resulted in identifying and including more studies focussing on non-technical skills. However, resources are consistently evaluated objectively on their technical outcomes in controlled studies. For them to be truly advantageous they need to be able to improve real life skills – including non-technical skills. We therefore believe that their effect on non-technical skills needs to be evaluated in the with the same methodological setup. Lastly, very little information is available on the effects of PGY on outcomes, only one study differentiated between different PGY's. They found inconsistent results, and their study was not powered on this outcome [41].
While the efficacy of digital tools in enhancing technical surgical skills is evident - especially for VR-trainers -, there is a lack of evidence regarding non-technical skills, and need to improve methodological robustness of research on new (digital) tools before they are implemented in curricula.
CRediT authorship contribution statement
Conceptualisation: TF, MS; Data collection and analysis: TF, SvdS; Writing: TF; Supervision: JB, ENvD, MS; Editing: TF, SvdS, EB, JB, ENvD, MS.
Ethical statement
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of competing interest
The authors declare no conflict of interest.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.sopen.2023.10.002.
Contributor Information
Tim M. Feenstra, Email: tm.feenstra@amsterdamumc.nl.
Marlies P. Schijven, Email: m.p.schijven@amsterdamumc.nl.
Appendix A. Supplementary data
Supplementary figures
References
- 1.Poulose B.K., Ray W.A., Arbogast P.G., Needleman J., Buerhaus P.I., Griffin M.R., et al. Resident work hour limits and patient safety. Ann Surg. 2005;241(6):847–856. doi: 10.1097/01.sla.0000164075.18748.38. [discussion 56-60] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tonelli C.M., Cohn T., Abdelsattar Z., Luchette F.A., Baker M.S. Association of resident independence with short-term clinical outcome in core general surgery procedures. JAMA Surg. 2023;158(3):302–309. doi: 10.1001/jamasurg.2022.6971. PMID: 36723925; PMCID: PMC9996403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mazzone E., Puliatti S., Amato M., Bunting B., Rocco B., Montorsi F., et al. A systematic review and meta-analysis on the impact of proficiency-based progression simulation training on performance outcomes. Ann Surg. 2021;274(2):281–289. doi: 10.1097/SLA.0000000000004650. [DOI] [PubMed] [Google Scholar]
- 4.Wynn G., Lykoudis P., Berlingieri P. Development and implementation of a virtual reality laparoscopic colorectal training curriculum. Am J Surg. 2018;216(3):610–617. doi: 10.1016/j.amjsurg.2017.11.034. [DOI] [PubMed] [Google Scholar]
- 5.Kapila A.K., Farid Y., Kapila V., Schettino M., Vanhoeij M., Hamdi M. The perspective of surgical residents on current and future training in light of the COVID-19 pandemic. Br J Surg. 2020;107(9):e305. doi: 10.1002/bjs.11761. Epub 2020 Jun 22. PMID: 32567688; PMCID: PMC7361412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Shafi A.M.A., Atieh A.E., Harky A., Sheikh A.M., Awad W.I. Impact of COVID-19 on cardiac surgical training: our experience in the United Kingdom. J Card Surg. 2020;35(8):1954–1957. doi: 10.1111/jocs.14693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Porpiglia F., Checcucci E., Amparore D., Verri P., Campi R., Claps F., et al. Slowdown of urology residents’ learning curve during the COVID-19 emergency. BJU Int. 2020;125(6) doi: 10.1111/bju.15076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.An T.W., Henry J.K., Igboechi O., Wang P., Yerrapragada A., Lin C.A., et al. How are Orthopaedic surgery residencies responding to the COVID-19 pandemic? An assessment of resident experiences in cities of major virus outbreak. J Am Acad Orthop Surg. 2020;28(15) doi: 10.5435/JAAOS-D-20-00397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Royal College of Surgeons of England (RCS) RCS online learning. 2020. https://vle.rcseng.ac.uk/ Available from.
- 10.Guedes H.G., Camara Costa Ferreira Z.M., Ribeiro de Sousa Leao L., Souza Montero E.F., Otoch J.P., Artifon E.L.A. Virtual reality simulator versus box-trainer to teach minimally invasive procedures: a meta-analysis. Int J Surg. 2019;61:60–68. doi: 10.1016/j.ijsu.2018.12.001. [DOI] [PubMed] [Google Scholar]
- 11.Mazur T., Mansour T.R., Mugge L., Medhkour A. Virtual reality-based simulators for cranial tumor surgery: a systematic review. World Neurosurg. 2018;110:414–422. doi: 10.1016/j.wneu.2017.11.132. [DOI] [PubMed] [Google Scholar]
- 12.Barsom E.Z., Graafland M., Schijven M.P. Systematic review on the effectiveness of augmented reality applications in medical training. Surg Endosc. 2016;30(10):4174–4183. doi: 10.1007/s00464-016-4800-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alaker M., Wynn G.R., Arulampalam T. Virtual reality training in laparoscopic surgery: a systematic review & meta-analysis. Int J Surg. 2016;29:85–94. doi: 10.1016/j.ijsu.2016.03.034. [DOI] [PubMed] [Google Scholar]
- 14.Ahmet A., Gamze K., Rustem M., Sezen K.A. Is video-based education an effective method in surgical education? a systematic review. J Surg Educ. 2018;75(5):1150–1158. doi: 10.1016/j.jsurg.2018.01.014. [DOI] [PubMed] [Google Scholar]
- 15.Gillespie B.M., Harbeck E., Kang E., Steel C., Fairweather N., Chaboyer W. Correlates of non-technical skills in surgery: a prospective study. BMJ Open. 2017;7(1) doi: 10.1136/bmjopen-2016-014480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Siu J., Maran N., Paterson-Brown S. Observation of behavioural markers of non-technical skills in the operating room and their relationship to intra-operative incidents. Surgeon. 2016;14(3):119–128. doi: 10.1016/j.surge.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 17.Adams-McGavin R.C., Jung J.J., van Dalen A.S.H.M., Grantcharov T.P., Schijven M.P. System factors affecting patient safety in the OR: an analysis of safety threats and resiliency. Ann Surg. 2021;274(1):114–119. doi: 10.1097/SLA.0000000000003616. PMID: 31592890. [DOI] [PubMed] [Google Scholar]
- 18.Gostlow H., Marlow N., Thomas M.J., Hewett P.J., Kiermeier A., Babidge W., et al. Non-technical skills of surgical trainees and experienced surgeons. Br J Surg. 2017;104(6):777–785. doi: 10.1002/bjs.10493. [DOI] [PubMed] [Google Scholar]
- 19.Hull L., Arora S., Aggarwal R., Darzi A., Vincent C., Sevdalis N. The impact of nontechnical skills on technical performance in surgery: a systematic review. J Am Coll Surg. 2012;214(2):214–230. doi: 10.1016/j.jamcollsurg.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 20.Moher D., Liberati A., Tetzlaff J., Altman D.G., Group P Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535. doi: 10.1136/bmj.b2535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.JPT Higgins, Thomas J., Chandler J., Cumpston M., Li T., Page M.J., et al. Cochrane handbook for systematic reviews of interventions version 6.2 (updated February 2021). Cochrane. 2021. www.training.cochrane.org/handbook Available from.
- 22.European Commission/EACEA/Eurydice . Publications Office of the European Union; Luxembourg: 2019. Digital education at school in Europe. Eurydice report. [Google Scholar]
- 23.Skill Merriam-Webster.com. 2011. https://www.merriam-webster.com (3 May 2022)
- 24.Review Manager (RevMan) [Computer program] 2020. Version 5.4. The cochrane collaboration. [Google Scholar]
- 25.CanMEDS . Royal College of Physicians and Surgeons of Canada; Ottawa: 2015. Physician competency framework; p. 2015. [Google Scholar]
- 26.Crossley J., Marriott J., Purdie H., Beard J.D. Prospective observational study to evaluate NOTSS (Non-Technical Skills for Surgeons) for assessing trainees’ non-technical performance in the operating theatre. Br J Surg. 2011;98(7):1010–1020. doi: 10.1002/bjs.7478. [DOI] [PubMed] [Google Scholar]
- 27.The Non-Technical Skills for Surgeons (NOTSS) Structuring observation, feedback and rating of surgeons'’ behaviours in the operating theatre . 2019. System handbook v2.0: Royal College of Surgeons of Edinburgh; version 2.0. [Google Scholar]
- 28.Sterne J.A.C., Savovic J., Page M.J., Elbers R.G., Blencowe N.S., Boutron I., et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 29.Ahlborg L., Hedman L., Nisell H., Felländer-Tsai L., Enochsson L. Simulator training and non-technical factors improve laparoscopic performance among OBGYN trainees. Acta Obstet Gynecol Scand. 2013;92(10):1194–1201. doi: 10.1111/aogs.12218. [DOI] [PubMed] [Google Scholar]
- 30.Akdemir A., Sendağ F., Oztekin M.K. Laparoscopic virtual reality simulator and box trainer in gynecology. Int J Gynaecol Obstet. 2014;125(2):181–185. doi: 10.1016/j.ijgo.2013.10.018. [DOI] [PubMed] [Google Scholar]
- 31.Araujo S.E.A., Delaney C.P., Seid V.E., Imperiale A.R., Bertoncini A.B., Nahas S.C., et al. Short-duration virtual reality simulation training positively impacts performance during laparoscopic colectomy in animal model: results of a single-blinded randomized trial - VR warm-up for laparoscopic colectomy. Surg Endosc. 2014;28(9):2547–2554. doi: 10.1007/s00464-014-3500-3. [DOI] [PubMed] [Google Scholar]
- 32.Borahay M.A., Haver M.C., Eastham B., Patel P.R., Kilic G.S. Modular comparison of laparoscopic and robotic simulation platforms in residency training: a randomized trial. J Minim Invasive Gynecol. 2013;20(6):871–879. doi: 10.1016/j.jmig.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 33.Brown K., Mosley N., Tierney J. Battle of the bots: a comparison of the standard da Vinci and the da Vinci surgical skills simulator in surgical skills acquisition. J Robot Surg. 2017;11(2):159–162. doi: 10.1007/s11701-016-0636-2. [DOI] [PubMed] [Google Scholar]
- 34.Camp C.L., Krych A.J., Stuart M.J., Regnier T.D., Mills K.M., Turner N.S. Improving resident performance in knee arthroscopy: a prospective value assessment of simulators and cadaveric skills laboratories. J Bone Joint Surg Am. 2016;98(3):220–225. doi: 10.2106/JBJS.O.00440. [DOI] [PubMed] [Google Scholar]
- 35.Cannon W.D., Garrett W.E., Jr., Hunter R.E., Sweeney H.J., Eckhoff D.G., Nic, et al. Improving residency training in arthroscopic knee surgery with use of a virtual-reality simulator. A randomized blinded study. J Bone Joint Surg Am. 2014;96(21):1798–1806. doi: 10.2106/JBJS.N.00058. [DOI] [PubMed] [Google Scholar]
- 36.Daly M.K., Gonzalez E., Siracuse-Lee D., Legutko P.A. Efficacy of surgical simulator training versus traditional wet-lab training on operating room performance of ophthalmology residents during the capsulorhexis in cataract surgery. J Cataract Refract Surg. 2013;39(11):1734–1741. doi: 10.1016/j.jcrs.2013.05.044. [DOI] [PubMed] [Google Scholar]
- 37.Dickerson P., Grande S., Evans D., Levine B., Coe M. Utilizing intraprocedural interactive video capture with Google glass for immediate postprocedural resident coaching. J Surg Educ. 2019;76(3):607–619. doi: 10.1016/j.jsurg.2018.10.002. [DOI] [PubMed] [Google Scholar]
- 38.Fried M.P., Sadoughi B., Gibber M.J., Jacobs J.B., Lebowitz R.A., Ross D.A., et al. From virtual reality to the operating room: the endoscopic sinus surgery simulator experiment. Otolaryngol Head Neck Surg. 2010;142(2):202–207. doi: 10.1016/j.otohns.2009.11.023. [DOI] [PubMed] [Google Scholar]
- 39.Garfjeld Roberts P., Alvand A., Gallieri M., Hargrove C., Rees J. Objectively assessing intraoperative arthroscopic skills performance and the transfer of simulation training in knee arthroscopy: a randomized controlled trial. Arthroscopy. 2019;35(4):1197–1209. doi: 10.1016/j.arthro.2018.11.035. [e1] [DOI] [PubMed] [Google Scholar]
- 40.Graafland M., Bemelman W.A., Schijven M.P. Game-based training improves the surgeon’s situational awareness in the operation room: a randomized controlled trial. Surg Endosc. 2017;31(10):4093–4101. doi: 10.1007/s00464-017-5456-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Hauschild J., Rivera J.C., Johnson A.E., Burns T.C., Roach C.J. Shoulder arthroscopy simulator training improves surgical procedure performance: a controlled laboratory study. Orthop J Sports Med. 2021;9(5) doi: 10.1177/23259671211003873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hooper J., Tsiridis E., Feng J.E., Schwarzkopf R., Waren D., Long W.J., Poultsides L., Macaulay W., NYU Virtual Reality Consortium Virtual reality simulation facilitates resident training in total hip arthroplasty: a randomized controlled trial. J Arthroplasty. 2019;34(10):2278–2283. doi: 10.1016/j.arth.2019.04.002. Epub 2019 Apr 8. PMID: 31056442. [DOI] [PubMed] [Google Scholar]
- 43.Hou Y., Shi J., Lin Y., Chen H., Yuan W. Virtual surgery simulation versus traditional approaches in training of residents in cervical pedicle screw placement. Arch Orthop Trauma Surg. 2018;138(6):777–782. doi: 10.1007/s00402-018-2906-0. [DOI] [PubMed] [Google Scholar]
- 44.Huri G., Gulsen M.R., Karmis E.B., Karaguven D. Cadaver versus simulator based arthroscopic training in shoulder surgery. Turk J Med Sci. 2021;51(3):1179–1190. doi: 10.3906/sag-2011-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Jensen K., Ringsted C., Hansen H.J., Petersen R.H., Konge L. Simulation-based training for thoracoscopic lobectomy: a randomized controlled trial: virtual-reality versus black-box simulation. Surg Endosc. 2014;28(6):1821–1829. doi: 10.1007/s00464-013-3392-7. [DOI] [PubMed] [Google Scholar]
- 46.Kantar R.S., Alfonso A.R., Ramly E.P., Cohen O., Rifkin W.J., Maliha S.G., et al. Knowledge and skills acquisition by plastic surgery residents through digital simulation training: a prospective, randomized, blinded trial. Plast Reconstr Surg. 2020;145(1) doi: 10.1097/PRS.0000000000006375. [DOI] [PubMed] [Google Scholar]
- 47.Korets R., Mues A.C., Graversen J.A., Gupta M., Benson M.C., Cooper K.L., et al. Validating the use of the mimic dV-trainer for robotic surgery skill acquisition among urology residents. Urology. 2011;78(6):1326–1330. doi: 10.1016/j.urology.2011.07.1426. [DOI] [PubMed] [Google Scholar]
- 48.Korndorffer J.R., Jr., Bellows C.F., Tekian A., Harris I.B., Downing S.M. Effective home laparoscopic simulation training: a preliminary evaluation of an improved training paradigm. Am J Surg. 2012;203(1):1–7. doi: 10.1016/j.amjsurg.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 49.Kun Y., Hubert J., Bin L., Huan W.X. Self-debriefing model based on an integrated video-capture system: an efficient solution to skill degradation. J Surg Educ. 2019;76(2):362–369. doi: 10.1016/j.jsurg.2018.08.017. [DOI] [PubMed] [Google Scholar]
- 50.Logishetty K., Rudran B., Cobb J.P. Virtual reality training improves trainee performance in total hip arthroplasty: a randomized controlled trial. Bone Joint J. 2019;101(12):1585–1592. doi: 10.1302/0301-620X.101B12.BJJ-2019-0643.R1. [DOI] [PubMed] [Google Scholar]
- 51.Lohre R., Bois A.J., Athwal G.S., Goel D.P., Canadian Shoulder and Elbow Society (CSES) Improved complex skill acquisition by immersive virtual reality training: a randomized controlled trial. J Bone Joint Surg Am. 2020;102(6):e26. doi: 10.2106/JBJS.19.00982. PMID: 31972694. [DOI] [PubMed] [Google Scholar]
- 52.Orzech N., Palter V.N., Reznick R.K., Aggarwal R., Grantcharov T.P. A comparison of 2 ex vivo training curricula for advanced laparoscopic skills: a randomized controlled trial. Ann Surg. 2012;255(5):833–839. doi: 10.1097/SLA.0b013e31824aca09. [DOI] [PubMed] [Google Scholar]
- 53.Palter V.N., Grantcharov T.P. Individualized deliberate practice on a virtual reality simulator improves technical performance of surgical novices in the operating room: a randomized controlled trial. Ann Surg. 2014;259(3):443–448. doi: 10.1097/SLA.0000000000000254. [DOI] [PubMed] [Google Scholar]
- 54.Sloth S.B., Jensen R.D., Seyer-Hansen M., Christensen M.K., De Win G. Remote training in laparoscopy: a randomized trial comparing home-based self-regulated training to centralized instructor-regulated training. Surg Endosc. 2022;36(2):1444–1455. doi: 10.1007/s00464-021-08429-7. Epub 2021 Mar 19. PMID: 33742271; PMCID: PMC7978167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Valdis M., Chu M.W.A., Schlachta C., Kiaii B. Evaluation of robotic cardiac surgery simulation training: a randomized controlled trial. J Thoracic Cardiovasc Surg. 2016;151(6) doi: 10.1016/j.jtcvs.2016.02.016. [DOI] [PubMed] [Google Scholar]
- 56.van Det M.J., Meijerink W.J., Hoff C., Middel L.J., Koopal S.A., Pierie J.P. The learning effect of intraoperative video-enhanced surgical procedure training. Surg Endosc. 2011;25(7):2261–2267. doi: 10.1007/s00464-010-1545-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Varras M., Loukas C., Nikiteas N., Varra V.K., Varra F.N., Georgiou E. Comparison of laparoscopic surgical skills acquired on a virtual reality simulator and a box trainer: an analysis for obstetrics-gynecology residents. Clin Exp Obstet Gynecol. 2020;47(5):755. [Google Scholar]
- 58.Waterman B.R., Martin K.D., Cameron K.L., Owens B.D., Belmont P.J., Jr. Simulation training improves surgical proficiency and safety during diagnostic shoulder arthroscopy performed by residents. Orthopedics. 2016;39(3) doi: 10.3928/01477447-20160427-02. [DOI] [PubMed] [Google Scholar]
- 59.Yiasemidou M., de Siqueira J., Tomlinson J., Glassman D., Stock S., Gough M. “Take-home” box trainers are an effective alternative to virtual reality simulators. J Surg Res. 2017;213:69–74. doi: 10.1016/j.jss.2017.02.038. [DOI] [PubMed] [Google Scholar]
- 60.Sharifzadeh N., Tabesh H., Kharrazi H., Tara F., Kiani F., Rasoulian Kasrineh M., et al. Play and learn for surgeons: a serious game to educate medical residents in uterine artery ligation surgery. Games Health J. 2021;10(4):220–227. doi: 10.1089/g4h.2020.0220. [DOI] [PubMed] [Google Scholar]
- 61.McKinney B., Dbeis A., Lamb A., Frousiakis P., Sweet S. Virtual reality training in Unicompartmental knee arthroplasty: a randomized. Blinded Trial J Surg Educ. 2022;79(6):1526–1535. doi: 10.1016/j.jsurg.2022.06.008. [DOI] [PubMed] [Google Scholar]
- 62.Michael D., Chen S. Thomson Course Technology; Boston, MA: 2006. Serious games: games that educate, train, and inform. [Google Scholar]
- 63.Bokkerink G.M.J., Joosten M., Leijte E., Verhoeven B.H., de Blaauw I., Botden S. Take-home laparoscopy simulators in pediatric surgery: is more expensive better? J Laparoendosc Adv Surg Tech A. 2021;31(1):117–123. doi: 10.1089/lap.2020.0533. [DOI] [PubMed] [Google Scholar]
- 64.Aggarwal R., Grantcharov T.P., Darzi A. Framework for systematic training and assessment of technical skills. J Am Coll Surg. 2007;204(4):697–705. doi: 10.1016/j.jamcollsurg.2007.01.016. [DOI] [PubMed] [Google Scholar]
- 65.Adams B.J., Margaron F., Kaplan B.J. Comparing video games and laparoscopic simulators in the development of laparoscopic skills in surgical residents. J Surg Educ. 2012;69(6):714–717. doi: 10.1016/j.jsurg.2012.06.006. [DOI] [PubMed] [Google Scholar]
- 66.Fecso A.B., Kuzulugil S.S., Babaoglu C., Bener A.B., Grantcharov T.P. Relationship between intraoperative non-technical performance and technical events in bariatric surgery. Br J Surg. 2018;105(8):1044–1050. doi: 10.1002/bjs.10811. [DOI] [PubMed] [Google Scholar]
- 67.Johnson A.P., Aggarwal R. Assessment of non-technical skills: why aren’t we there yet? BMJ Qual Saf. 2019;28(8):606–608. doi: 10.1136/bmjqs-2018-008712. [DOI] [PubMed] [Google Scholar]
- 68.Zhang C., Zhang C., Grandits T., Harenstam K.P., Hauge J.B., Meijer S. A systematic literature review of simulation models for non-technical skill training in healthcare logistics. Adv Simul (Lond) 2018;3:15. doi: 10.1186/s41077-018-0072-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Putnam L.R., Pham D.H., Ostovar-Kermani T.G., Alawadi Z.M., Etchegaray J.M., Ottosen M.J., et al. How should surgical residents be educated about patient safety: a pilot randomized controlled trial. J Surg Educ. 2016;73(4):660–667. doi: 10.1016/j.jsurg.2016.02.011. [DOI] [PubMed] [Google Scholar]
- 70.Kassam A., Cowan M., Donnon T. An objective structured clinical exam to measure intrinsic CanMEDS roles. Med Educ Online. 2016;21:31085. doi: 10.3402/meo.v21.31085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Roberts G., Beiko D., Touma N., Siemens D.R. Are we getting through? A national survey on the CanMEDS communicator role in urology residency. Can Urol Assoc J. 2013;7(11−12):E781–E782. [PMC free article] [PubMed] [Google Scholar]
- 72.Barsom EZ, Duijm RD, Dusseljee-Peute LWP, Landman-van der Boom EB, van Lieshout EJ, Jaspers MW, et al. Cardiopulmonary resuscitation training for high school students using an immersive 360-degree virtual reality environment. Br J Educ Technol. n/a(n/a).
- 73.Crawford S.B., Monks S.M., Wells R.N. Virtual reality as an interview technique in evaluation of emergency medicine applicants. AEM Educ Train. 2018;2(4):328–333. doi: 10.1002/aet2.10113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.van Dalen A.S.H.M., Jansen M., van Haperen M., van Dieren S., Buskens C.J., Nieveen van Dijkum E.J.M., Bemelman W.A., Grantcharov T.P., Schijven M.P. Implementing structured team debriefing using a Black Box in the operating room: surveying team satisfaction. Surg Endosc. 2021;35(3):1406–1419. doi: 10.1007/s00464-020-07526-3. Epub 2020 Apr 6. PMID: 32253558; PMCID: PMC7886753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Byrnes Y.M., Luu N.N., Frost A.S., Chao T.N., Brody R.M., Cannady S.B., Rajasekaran K., Shanti R.M., Newman J.G. Evaluation of an interactive virtual surgical rotation during the COVID-19 pandemic. World J Otorhinolaryngol Head Neck Surg. 2021;8(4):302–307. doi: 10.1016/j.wjorl.2021.04.001. Epub ahead of print. PMID: 33936857; PMCID: PMC8064875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Peddle M., Bearman M., McKenna L., Nestel D. “Getting it wrong to get it right”: faculty perspectives of learning non-technical skills via virtual patient interactions. Nurse Educ Today. 2020;88:104381. doi: 10.1016/j.nedt.2020.104381. [DOI] [PubMed] [Google Scholar]
- 77.Winzer A., Jansky M. Digital lesson to convey the CanMEDS roles in general medicine using problem-based learning (PBL) and peer teaching. GMS J Med Educ. 2020;37(7) doi: 10.3205/zma001357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ward T.M., Mascagni P., Ban Y., Rosman G., Padoy N., Meireles O., et al. Computer vision in surgery. Surgery. 2021;169(5):1253–1256. doi: 10.1016/j.surg.2020.10.039. [DOI] [PubMed] [Google Scholar]
- 79.Faulkner H., Regehr G., Martin J., Reznick R. Validation of an objective structured assessment of technical skill for surgical residents. Acad Med. 1996;71(12):1363–1365. doi: 10.1097/00001888-199612000-00023. [DOI] [PubMed] [Google Scholar]
- 80.Martin J.A., Regehr G., Reznick R., MacRae H., Murnaghan J., Hutchison C., et al. Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg. 1997;84(2):273–278. doi: 10.1046/j.1365-2168.1997.02502.x. [DOI] [PubMed] [Google Scholar]
- 81.Guerlain S., Adams R.B., Turrentine F.B., Shin T., Guo H., Collins S.R., et al. Assessing team performance in the operating room: development and use of a “black-box” recorder and other tools for the intraoperative environment. J Am Coll Surg. 2005;200(1):29–37. doi: 10.1016/j.jamcollsurg.2004.08.029. [DOI] [PubMed] [Google Scholar]
- 82.Frederiksen J.G., Sorensen S.M.D., Konge L., Svendsen M.B.S., Nobel-Jorgensen M., Bjerrum F., et al. Cognitive load and performance in immersive virtual reality versus conventional virtual reality simulation training of laparoscopic surgery: a randomized trial. Surg Endosc. 2020;34(3):1244–1252. doi: 10.1007/s00464-019-06887-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary figures