Abstract
Background:
Although systemic inequities, broadly defined, are associated with health disparities in adults, there is a dearth of research linking contextual measures of exclusionary policies or prejudicial attitudes to health impairments in children, particularly among Latino populations. In this study, we examined a composite measure of systemic inequities in relation to the co-occurrence of multiple health problems in Latino children in the U.S.
Methods:
Participants included 17,855 Latino children ages 3 to 17 years from the National Survey of Children’s Health (2016–2020). We measured state-level systemic inequities using a factor score that combined an index of exclusionary state policies towards immigrants and aggregated survey data on prejudicial attitudes towards immigrants and Latino individuals. Caregivers reported on three categories of child health problems: common health difficulties in the past year, current chronic physical health conditions, and current mental health conditions. For each category, we constructed a variable reflecting zero, one, or two or more conditions.
Results:
In models adjusted for sociodemographic covariates, interpersonal discrimination, and state-level income inequality, systemic inequities were associated with 1.13 times the odds of a chronic physical health condition (95% confidence interval (CI): 1.02, 1.25) and 1.24 times the odds of two or more mental health conditions (95% CI: 1.06, 1.45).
Conclusions:
Latino children residing in states with higher levels of systemic inequity are more likely to experience mental health or chronic physical health conditions relative to those in states with lower levels of systemic inequity.
Table of Contents Summary:
Systemic inequities, assessed at the state-level, are associated with physical and mental health conditions among Latino children.
Introduction
Latino/Latina/Hispanic children (referred to as “Latino children” herein) comprise approximately one-quarter of all children under the age of 18 in the U.S.1 Latino children fare worse than non-Latino White children (referred to as “White children” herein) across several common health conditions, including respiratory illnesses,2, 3 overweight and obesity,4, 5 insufficient sleep,6–8 and heightened levels of inflammation.9 Systemic inequities related to structural or cultural racism, discrimination, xenophobia, and stigma (referred to as “systemic inequities” herein) limit access to power and resources for members of marginalized or stigmatized groups10–16 and may contribute to these disparities.17, 18 Such inequities can take many forms, including pervasive prejudicial attitudes and rhetoric directed toward racial or ethnic minorities, exclusionary laws designed to exclude individuals from various activities within society (e.g., related to education, health care, etc.), and criminalizing immigration policies.13
Consistent with research on the effects of discrimination on health in adults,10, 19 most research on child health has focused on individual experiences of discrimination,20 despite repeated calls to assess systemic or structural influences.10, 21–25 Moreover, the majority of studies that have examined state-level measures of systemic inequities (e.g., anti-immigrant policies) in relation to Latino health have focused on adults26–28 or perinatal outcomes,29–33 with less known about children and youth. Prior studies have shown that harsh immigrant policies are associated with poor mental health26 and reduced use of preventive health care and public assistance among Latino adults,34, 35 as well as food insecurity among Latino immigrant families.33, 36 Furthermore, restrictive immigration laws,30, 32 sociopolitical events with relevance to immigration policies (e.g., the 2016 U.S. election),37, 38 and enforcement actions39 have each been linked to adverse birth outcomes among children born to Latina mothers. Although research on state-level systemic inequities and child and adolescent health outcomes is sparse, recent evidence found that Latino adolescents in states with greater systemic inequities (measured via a composite index of state immigration policies and aggregate social attitudes towards immigrant and Latino populations) had smaller hippocampal volumes, a brain region associated with chronic stress exposure.40 This work is complemented by research on adolescent responses to immigration actions,41, 42 including a study documenting elevated worry and behavioral withdrawal among Latino adolescents with vulnerable versus more secure family immigrant statuses.41
Building on this nascent literature, the present study examined associations between state-level, systemic inequities and the number of reported health problems in Latino children. Co-occurrence of problems is an understudied aspect of child health,43–46 with potential implications for costs and quality of life for parents and children, health and earnings across the life course, as well as approaches to prevention. Systemic inequities may affect a broad range of children’s health conditions—and the clustering of conditions—via chronic stress and associated disruptions to the child’s stress-response system,47, 48 or through the deprivation of resources needed to support healthy development (e.g., lack of access to safe and secure neighborhoods and schools or affordable, nourishing food).49 These postulated pathways of chronic stress and deprivation of resources suggest potential shared mechanisms for mental and physical health problems among children.
Based on prior studies,26–28, 40 we hypothesized that greater systemic inequities would be associated with increased reported health problems among Latino children. We include both U.S.-born and foreign-born Latino children in our study based on: (a) quantitative research showing that restrictive immigration policies are associated with poor mental health among Latino adults26 and birth outcomes32 regardless of personal immigration history, and (b) qualitative research demonstrating few differences between US-born and foreign-born Latino adults in perceptions of vulnerability or psychological distress related to immigration enforcement activities.50 These findings are likely due to several factors, including that 40 percent of Latino adults live in households with mixed immigration status,51 thus making immigration-related policies salient to a large portion of Latino families.
Methods
Sample
We used data from 17,855 Latino children from the National Survey of Children’s Health (NSCH) (2016–2020), a cross-sectional, nationally representative, weighted probability sample of non-institutionalized children from birth through age 17. Each year, randomly selected households across the U.S. are mailed an invitation to complete a household screener and child-level questionnaire via a secured website or on paper. The paper and web instruments are available in both English and Spanish, and additional language support is available via telephone. Parents or guardians familiar with the child’s health and medical care are the respondents. After completing the screener, a single child from each home is randomly selected as the focal child. Details on design, administration, and completion rates are available at https://www.childhealthdata.org/learn-about-the-nsch/NSCH. Our analytic sample included children ages 3 years of age and older given the health outcomes on which we focus. Children from Washington, DC—notably, considered to be a “sanctuary city”52—were excluded from our analytic sample because data needed to construct the state-level systemic inequities score were unavailable.
Measures
Child health.
We assessed the number of problems within and across three distinct dimensions of child health, following Jackson and colleagues’ approach with the 2016 NSCH.53 Caregiver respondents reported on: (a) health difficulties in the past twelve months (six items: eating or swallowing because of a health condition; digesting food, including stomach or intestinal problems, constipation, or diarrhea; repeated or chronic physical pain, including headaches or other back and body pain; toothaches; bleeding gums; and decayed teeth or cavities); (b) provider-diagnosed, current, chronic physical conditions (six items: allergies; asthma; blood disorders; diabetes; heart condition; and arthritis); and (c) provider-diagnosed, current mental health conditions (four items: depression; Attention-Deficit/Hyperactivity Disorder (ADHD); anxiety problems; and behavioral or conduct problems). We examined the extent of problems within each health dimension by constructing a three-level variable to reflect zero, one, or two or more. We also created a four-level variable to indicate the co-occurrence of problems across dimensions (i.e., no health problems and problems within one, two, or all three dimensions). These outcomes are designed to indicate the pervasiveness of problems within and across multiple dimensions of mental and physical health, for both chronic and temporary conditions.53 As a secondary analysis, we examined outcomes individually as well.
Systemic inequities.
We operationalized systemic inequities via a factor score developed using data-driven methods and used in prior research.40 We included measures of aggregated public attitudes and social policies—and refer to them together as “systemic”—as both policies and attitudes reflect the broader macro-social context, are highly correlated,54 and are consistent with conceptual frameworks from minority stress theory and stigma research.55, 56
The factor score was based on three measures. First, a state-level summary index reflecting restrictiveness or supportiveness of state policies (related to health services, private sector employment, business licensing, rental housing access, higher education access, driver’s license access, immigration policy enforcement, non-English language use, identification requirements, and discrimination prohibition) towards immigrants as of 2016, with a positive point awarded for each of the items, and a negative point awarded if the state explicitly prohibited the item.57 Second, we used survey responses from the American National Election Study (ANES) to a “feelings thermometers” (i.e., a measurement technique where participants report their feelings towards a target on a scale ranging from 0 (extremely cold or negative feelings) to 100 (extremely warm or positive feelings)) reflecting attitudes towards Latino individuals (pooled, 1996 to 2016). Third, we used survey responses from the ANES on a “feelings thermometer” reflecting attitudes towards immigrants (pooled, 2004 to 2016). Responses on the ANES feelings thermometers were standardized for all respondents and then aggregated at the state-level. All three components were reverse scored so that higher ratings represented higher levels of structural inequity.
For the ANES feeling thermometer measures, survey years were pooled to maximize the number of respondents per state and to minimize measurement error; this approach is supported by research showing the stability of states relative to each other in terms of their residents’ attitudes towards marginalized groups (e.g., racial minorities and women) over 30 years.58, 59 We included attitudes and policies related to immigration for this measure, despite the fact that only a third of Latino individuals in the U.S. are foreign-born,60 because of the mixed status of many Latino households51 and because non-Latino individuals in the U.S. often conflate immigrant identity with Latino identity.61 See Appendix 2 for a table describing the component measures.
The model-based factor score was constructed for each state using exploratory factor analysis, with all three measures coded with higher values reflecting higher levels of systemic inequity. We have displayed the distribution of factor scores across states (see Figure 1). Appendix 3 presents the scores for each state. The continuous factor score ranged from −1.75 to +1.76, representing the state’s relative standing on the latent factor of systemic inequities for Latino children, with higher values reflecting higher levels of systemic inequity.
Figure 1.
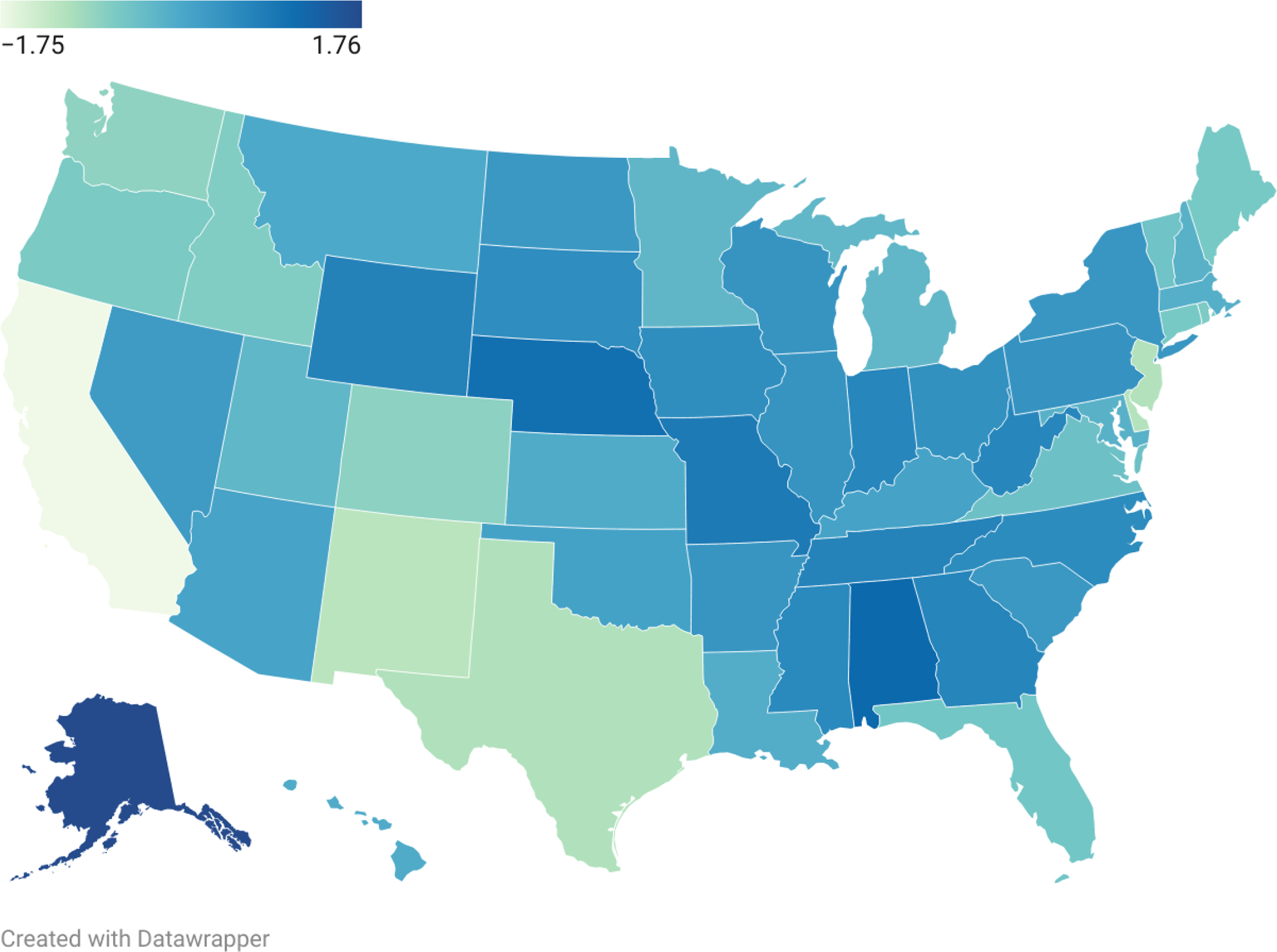
Distribution of systemic inequities for Latino populations across the United States
Note: Darker shade reflects higher values of the state-level systemic inequity score.
Covariates.
Caregivers reported on children’s ethnicity. We selected covariates to be consistent with prior research53 and constructed both minimally and fully adjusted models recognizing that some of the covariates could be on the causal pathway. Our basic set of covariates included child’s age and sex, survey year, family immigration history, mother’s age at child’s birth, and state-level Gini Index, to control for other macro-level characteristics related to income inequality (see Table 1 for variable categories). Our extended set of covariates additionally included highest education level in household, income-to-needs ratio (using the multiple imputed values provided by Census), caregiver report that the child ever resided in an unsafe neighborhood, health insurance status, caregiver self-rated health index (i.e., sum of single-item self-reports of physical and mental health), an index reflecting number of social services received (i.e., cash assistance, Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), Supplemental Nutrition Assistance Program (SNAP), and free or reduced-price school lunch), and caregiver report of the child’s personal experience of racism.
Table 1.
Descriptive characteristics of the sample (n=17,855)
| % | (S.E.) | |
|---|---|---|
|
|
||
| Child sex (male) | 50.90 | (0.83) |
| Age cohort | ||
| 3–5 years | 18.84 | (0.66) |
| 6–11 years | 40.38 | (0.83) |
| 12–17 years | 40.77 | (0.81) |
| No health insurance | 10.56 | (0.56) |
| Household income-to-needs ratio | ||
| Less than FPL | 29.50 | (0.91) |
| 100 – 399% FPL | 45.66 | (0.87) |
| ≥ 400% FPL | 24.84 | (0.72) |
| Highest household education | ||
| Less than high school | 23.74 | (0.83) |
| High school | 26.93 | (0.74) |
| More than high school | 49.33 | (0.83) |
| Family Structure | ||
| Two adults, married | 58.35 | (0.84) |
| Two adults, unmarried | 13.19 | (0.61) |
| Single parent | 22.71 | (0.69) |
| Grandparent or Other | 5.75 | (0.43) |
| Family Immigration History | ||
| Child or parent born out of US | 54.30 | (0.83) |
| Child born in US, parent data missing | 8.46 | (0.53) |
| Parent and child born in US | 37.24 | (0.78) |
| Count of social services received | ||
| 0 | 39.25 | (0.80) |
| 1 | 31.46 | (0.81) |
| 2 | 19.03 | (0.75) |
| 3 | 8.68 | (0.52) |
| 4 | 1.58 | (0.23) |
| Caregiver health index | ||
| Excellent (score=2–3) | 36.42 | (0.81) |
| Good (score=4–6) | 55.23 | (0.84) |
| Fair/poor (score=7–10) | 8.35 | (0.46) |
| Parent-report, unsafe neighborhood | 7.74 | (0.45) |
| Parent reported unfair treatment of child due to race or ethnicity | 5.66 | (0.34) |
Analysis
First, we display the social, demographic, and health characteristics for each group. Second, we used generalized estimating equations (GEE)62 and multinomial logistic regression to estimate the relative risk of exhibiting a single health problem and multiple problems within each of the three health dimensions, and across health dimensions, using systemic inequities as the independent variable. We selected multinomial regression because we conceptualized the co-occurrence of more than one condition as a discrete, qualitative outcome, rather than a count (consistent with prior research using a similar set of outcomes53). This approach accounts for the complex sample design and for correlations among children who reside in the same state. We present odds ratios, 95% confidence intervals (CIs), and p-values from Wald’s tests, which describe the significance of the association between the exposure and multi-category outcome, collectively (i.e., both categories against zero).63 As sensitivity analyses, we examined each health outcome individually and tested for effect modification by sex.
Descriptive statistics and models were generated using SUDAAN 11.0.3, and we weighted the results to represent non-institutionalized U.S. children. To handle missing data, analyses used six imputed data sets. The results using the imputed data are nearly identical to those using complete case data.
Results
Demographic characteristics.
Nearly one-third of children (29.50%) lived in households below the federal poverty level, and over one in ten (10.56%) did not have health insurance (see Table 1). Slightly over half of the children (54.30%) were either born outside of the U.S. or had a parent born outside the U.S. Table 2 presents the distributions for number of problems within and across three distinct dimensions of child health. See Appendix 1 for prevalence of each specific health outcome.
Table 2.
Health characteristics of the sample (n=17,855)
| % | (S.E.) | |
|---|---|---|
|
|
||
| Health difficulties | ||
| 0 | 70.76 | (0.77) |
| 1 | 19.76 | (0.69) |
| 2+ | 9.48 | (0.48) |
| Chronic physical health conditions | ||
| 0 | 78.22 | (0.64) |
| 1 | 16.86 | (0.58) |
| 2+ | 4.92 | (0.32) |
| Mental health conditions | ||
| 0 | 86.42 | (0.52) |
| 1 | 7.73 | (0.44) |
| 2+ | 5.85 | (0.32) |
| # of health dimensions with 1+ condition | ||
| 0 | 52.89 | (0.83) |
| 1 | 32.42 | (0.79) |
| 2 | 11.89 | (0.51) |
| 3 | 2.80 | (0.23) |
Note: Health difficulties (past 12 months) include problems (1) eating or swallowing; (2) digesting food, including stomach/intestinal problems; (3) repeated or chronic physical pain; (4) toothaches; (5) bleeding gums; and (6) cavities. Chronic health problems (current) include caregiver report of health care provider’s diagnosis of: (1) allergies; (2) asthma; (3) blood disorder; (4) diabetes; (5) heart condition; and (6) arthritis. Mental health disorders (current) include health care provider or educator report of (1) depression; (2) Attention Deficit Hyperactivity Disorder; (3) anxiety problems; and (4) behavioral or conduct problems. Number of health dimensions with 1+ condition is a count of the health outcome categories in which a child had one or more health conditions (range: 0 to 3).
Systemic inequities and number of health outcomes.
The multinomial models to estimate odds ratios for each health dimension, and across dimensions, were similar when adjusting for a basic set of covariates and when additionally adjusting for a more comprehensive set of social and demographic covariates (see Appendix 4 for values from the basic and fully-adjusted models). Figure 2 displays the odds ratios from the fully-adjusted models only.
Figure 2.

Adjusted odds ratios to display the relationship between state-level systemic inequities and health problems among Latino children (n=17,855) 3–17 years of age
Notes: Models are adjusted for child’s age, sex, personal experience of racism, survey year, household income, highest education in household, family immigration history, social service use index, mother’s age at child’s birth, neighborhood safety, insurance status, caregiver health, family structure, and state income inequality. See Appendix 4 for numeric values corresponding to estimates presented in the figure and Wald p-values.
In minimally adjusted models, systemic inequities were significantly associated with the number of chronic physical health conditions and number of mental health problems. Specifically, a one-unit increase in systemic inequities was associated increased odds of one (adjusted odds ratio (AOR)=1.13, 95% confidence interval (CI): 1.02, 1.25) or two or more (AOR=1.20, 95% CI: 1.00, 1.45) chronic physical health conditions, and two or more mental health conditions (AOR=1.27, 95% CI: 1.09, 1.48) (see Appendix 4). In models that additionally adjusted for demographic characteristics that could be on the causal pathway, systemic inequities were significantly associated with increased odds of having a chronic physical health condition (AOR=1.13, 95% CI: 1.02, 1.25) and increased odds of having two or more mental health conditions (AOR=1.24, 95% CI: 1.06, 1.45). No associations were evident for the outcome of health difficulties in the past 12 months. Although an increasing relationship between systemic inequities and the number of health dimensions with one or more health problems was suggested by the point estimates, with AORs increasing in magnitude as the number of dimensions with 1+ health problems increased, associations were not significant at p<.05.
In sensitivity analyses, we disaggregated our health categories to further examine the results (see Table 3): in fully-adjusted models, anxiety problems (AOR=1.24, 95% CI: 1.06, 1.46), ADHD (AOR: 1.20, 95%: 1.03, 1.40), and allergies (AOR=1.15, 95% CI: 1.04, 1.27) were each associated with systemic inequities at the p<.05 threshold. Finally, we did not find evidence for effect modification based on child’s sex (p-values>0.05) across the four primary outcomes.
Table 3.
Adjusted odds ratios to describe the relationship between the systemic inequities score and each outcome among Latino children, ages 3 to 17 years
| Systemic Inequities | ||
|---|---|---|
| AOR | 95% CI | |
| Health difficulties, past 12 months | ||
| Eating or swallowing problems | 1.18 | (0.84, 1.65) |
| Digesting food, including stomach or intestinal problems | 1.04 | (0.90, 1.20) |
| Chronic or repeated physical pain | 0.96 | (0.83, 1.11) |
| Toothaches | 1.01 | (0.83, 1.23) |
| Bleeding gums | 0.98 | (0.79, 1.23) |
| Decayed teeth or cavities | 0.93 | (0.82, 1.04) |
| Any dental problem | 0.92 | (0.82, 1.03) |
| Chronic health conditions | ||
| Allergies | 1.15 | (1.04, 1.27) |
| Asthma | 1.11 | (0.97, 1.28) |
| Mental health conditions | ||
| Depression | 1.05 | (0.82, 1.35) |
| Anxiety problems | 1.24 | (1.06, 1.46) |
| ADHD | 1.20 | (1.03, 1.40) |
| Behavioral or conduct problems | 1.14 | (0.96, 1.35) |
Notes: AOR = Adjusted odds ratios. All models are adjusted for child’s age, sex, survey year, household income, highest education in household, family immigration history, social service use index, mother’s age at child’s birth, neighborhood safety, insurance status, caregiver health, family structure, personal experience of racism, and state income inequality. We did not examine uncommon chronic physical health conditions as separate outcomes (i.e., blood disorders, diabetes, heart conditions, arthritis) due to data limitations resulting from the low prevalence for these conditions.
Discussion
This study examined whether Latino children who reside in states with higher levels of systemic inequities experience a greater co-occurrence of health problems relative to children who live in states with lower levels of inequity. We used nationally representative data from the NSCH linked to a state-level measure of systemic inequities, generated from aggregated public opinion data about Latino groups and immigrant populations as well as both exclusionary and inclusive policies towards immigrants.
As hypothesized based on prior research,26–28, 32, 64, 65 systemic inequities were associated with a greater co-occurrence of mental health conditions and the occurrence of chronic physical health conditions among Latino children, even after adjusting for a broad set of child and family characteristics and individual experiences of discrimination. Of note, while the observed associations are small in magnitude, research suggests that small effects can be meaningful when scaled across populations, as is the case in our measure of structural inequalities.66, 67 For both chronic physical and mental health conditions, we observed a graded relationship where the estimated associations were larger as the number of health conditions increased. This pattern is consistent with conceptualizations of systemic inequities as a broad, generalizable, risk factor.
Our results reinforce and build on prior studies of personally-experienced racism and child health,20, 68–70 as well as restrictive immigration policies and adult26–28 and perinatal health,29, 30, 33, 39 in several ways. First, we use a recent, large nationally representative sample of children, which improves the generalizability of our results and the ability to study variation in systemic inequities across states. Second, drawing on evidence that immigration policies and anti-immigrant sentiment are interconnected,54 our measure of systemic inequities combines both aggregated social attitudes and policies, thereby improving construct validity. Third, our analyses consider the co-occurrence of health problems, an understudied aspect of child development that has relevance for health equity research,43 which has rarely been studied in relation to structural contexts in childhood.
There are also limitations to consider in interpreting these study results. First, state-level analyses of systemic inequities are appropriate given the many important legislative activities at that level, but they offer a conservative test because more proximal environments are likely to exert stronger associations. Thus, more localized aspects of place-based inequities and protective factors that influence child health and development should be studied,71–73 as there is often substantial heterogeneity within states in terms of social climates surrounding Latino populations (e.g., differential enforcement of immigration policies). Also related to our exposure measure, the index of state policies reflects policies in place in 2016,57 and our measures of prejudicial attitudes pool across many years, up to 2016. Although our approach is supported by research showing stability in the rank ordering of state-level attitudes towards marginalized groups,58, 59 future studies might benefit from examining time-varying measures of systemic inequities. We also recognize that, despite the aforementioned strengths of using a factor score, one of the limitations of this approach is that there is not a direct interpretation of a one-unit change in this continuous measure because it combines interrelated components of systemic inequities.
Second, the NSCH has several limitations, such as reliance on caregiver report of provider-diagnosed mental health conditions; given the disparities in specialized mental health services for Latino children,74, 75 these outcomes are likely to be underestimates. Related, the survey was administered via mail and online, which could exclude families without permanent mailing addresses or reliable internet access, which represent some of the highest risk populations. Furthermore, our analysis is not inclusive of all relevant child outcomes (e.g., we could not include provider-diagnosed overweight or obesity since it was not asked in 2016 and 2017); and, our ability to explore potential within-group interactions by country of origin, age, geography, duration of time in the United States among the subset of children born outside of the US, and other child and family characteristics (e.g., interpersonal experiences of racism) was limited by insufficient sample sizes. We also were unable to account for how long a child lived in a state at the time of the survey, which could introduce measurement error, and our cross-sectional design prohibits causal inferences and examination of both unique and shared mechanisms, all of which represent important areas for future investigation. Finally, while interpreting these results it is important to keep in mind that odds ratios are overestimates of risk for common outcomes (i.e., >10 percent76).
Implications
Childhood health provides a foundation for well-being across the life course, including promotion of school attendance and performance,77–79 reducing risk for substance abuse,80, 81 and positive health and socioeconomic attainment in adulthood.82–84 Accordingly, our results and related studies have implications for a wide range of health-promoting policies, particularly in the face of persistent structural inequities related to racism, xenophobia, and punitive approaches to immigration. Policy statements from the American Academy of Pediatrics and other reports have called on pediatricians to play a more active role in educating the public about the adverse effects of systemic racism experienced by children of color and immigrant families.17, 85–88 This study underscores the importance of addressing the health impacts of state laws as well as the effects of public attitudes that perpetuate racist and/or anti-immigrant sentiments, all of which influence access to opportunities and resources that promote healthy development.89 Previous research has demonstrated that inclusive immigrant policies can be protective for educational attainment,90, 91 labor market outcomes,92 and other measures of socioeconomic wellbeing,93 which directly influence the resources available to minoritized children. Although studies of the potential benefits of inclusive immigrant policies for child health outcomes are limited, one quasi-experimental study of children whose mothers received protection from deportation via the United States’ Deferred Action for Childhood Arrivals program (i.e., determined based on their birth date) reported 50 percent fewer diagnoses of anxiety and adjustment disorders compared to children who did not receive this protection.94 Further investigation is needed to identify policies, administrative practices, and localized programs that are most effective in advancing health equity. In addition, pediatricians working with Latino children and children in immigrant families should be cognizant of major changes to immigrant-related policies or highly visible discriminatory events and can advocate for strategies to minimize structural or cultural racism, including the removal of exclusionary policies.
Conclusion
This study begins to address significant gaps in the empirical literature on the harmful consequences of discriminatory policies and prejudicial social contexts on children’s health. Beyond the need for a strong pediatric voice in educating policymakers and the general public about this threat to child wellbeing, a deeper understanding of the causal mechanisms that explain these findings is essential for moving beyond documenting the consequences of structural inequities and towards accelerating the development of more effective strategies to prevent, reduce, and/or mitigate their harmful effects.
What’s Known on This Subject
Prior studies have documented that systemic inequities, including harsh immigrant policies, are associated with poor mental health among Latino adults and adverse birth outcomes for Latino infants. Few studies have examined state-level measures of systemic inequities and children’s health.
What This Study Adds
Systemic inequities—including exclusionary state policies and prejudicial attitudes—are associated with the occurrence of multiple physical and mental health conditions among Latino children over and above individual and family characteristics, highlighting the importance of considering macro-level social determinants of child health.
What’s Known on This Subject
Systemic inequities, including harsh immigration policies, are associated with poor mental health among Latino adults and adverse birth outcomes for Latino infants. Yet, few studies have examined associations between state-level measures of systemic inequities and children’s health.
What This Study Adds
Systemic inequities—including exclusionary state policies and prejudicial attitudes—are associated with the occurrence of physical and mental health conditions among Latino children over and above individual and family characteristics, highlighting the importance of considering macro-level social determinants of child health.
Source(s) of Support:
This work was supported by an award from the Foster Family Funds to the Center on the Developing Child at Harvard University.
Role of Funder/Sponsor:
The funder/sponsor did not participate in the work.
Abbreviations:
- NSCH
National Survey of Children’s Health
- ADHD
attention deficit hyperactivity activity disorder
- ANES
American National Election Study
- OR
odds ratio
Appendix 1.
Specific health outcomes in children (n=17,855)
| % | (S.E.) | |
|---|---|---|
|
|
||
| Health difficulties, past 12 months | ||
| Eating or swallowing problems | 1.41 | (0.18) |
| Digesting food, including stomach or intestinal problems | 8.74 | (0.45) |
| Chronic or repeated physical pain | 8.63 | (0.46) |
| Toothaches | 4.75 | (0.36) |
| Bleeding gums | 3.11 | (0.28) |
| Decayed teeth or cavities | 15.53 | (0.63) |
| Any dental problem | 18.28 | (0.67) |
| Current chronic health conditions | ||
| Allergies | 16.93 | (0.57) |
| Asthma | 8.46 | (0.44) |
| Blood disorders | 0.21 | (0.07) |
| Diabetes | 0.26 | (0.05) |
| Heart conditions | 0.94 | (0.11) |
| Arthritis | 0.12 | (0.02) |
| Current mental health conditions | ||
| Depression | 2.93 | (0.24) |
| Anxiety problems | 6.53 | (0.35) |
| ADHD | 6.75 | (0.37) |
| Behavioral or conduct problems | 6.03 | (0.35) |
Appendix 2.
Structural inequity related to Latino ethnicity
| Component | Source | Year(s) of data |
|---|---|---|
|
| ||
| Illegal immigrants feelings thermometer1 | American National Election Survey | 2004, 2008, 2012, 2016 |
| Hispanics feelings thermometer1 | American National Election Survey | 1996, 2000, 2002, 2004, 2008, 2012, 2016 |
| Index for the following 10 policies: Access to health services for immigrants; cooperation by state or local law enforcement with federal immigration enforcement; use of non-English language; immigrant employment in a broad segment of the private sector; restricts immigrant access to a broad class of business licenses; access to rental housing for immigrants; prohibits discrimination based on citizenship or immigration status; provides identification to access relevant services or opportunities; access to higher education for immigrants; access to driver’s licenses for immigrants2 | Wake Forest Immigration Law Coding Project | 2016 |
Note: All components were reverse scored so that higher ratings represented higher levels of structural inequity.
A “feelings thermometer” is a visual analog scale; respondents are asked to rank their views of the subject on a scale from “cold,” which indicates cold or negative feelings, to “hot” which indicates warm, or positive feelings, scored on a range from 0 to 100. National scores were standardized and then aggregated at the state-level.
Score was computed by awarding a positive point for the presence of a given item; a negative point was awarded if there was a law to explicitly prohibit the item.
Appendix 3.
Systemic inequity factor score for each state
| Alabama | 1.192609415 |
| Alaska | 1.762166823 |
| Arizona | 0.09262617 |
| Arkansas | 0.362811591 |
| California | −1.746000735 |
| Colorado | −0.764800338 |
| Connecticut | −0.594610506 |
| Delaware | −1.131580132 |
| Florida | −0.534851602 |
| Georgia | 0.674533941 |
| Hawaii | −0.053595288 |
| Idaho | −0.68201278 |
| Illinois | 0.379332559 |
| Indiana | 0.647283447 |
| Iowa | 0.489941806 |
| Kansas | −0.052408919 |
| Kentucky | 0.103890173 |
| Louisiana | −0.090151361 |
| Maine | −0.594149601 |
| Maryland | −0.160155081 |
| Massachusetts | −0.122937467 |
| Michigan | −0.277416171 |
| Minnesota | −0.253823636 |
| Mississippi | 0.585269372 |
| Missouri | 0.881863619 |
| Montana | −0.002640792 |
| Nebraska | 1.069464245 |
| Nevada | 0.247743259 |
| New Hampshire | −0.160049548 |
| New jersey | −1.1168013 |
| New Mexico | −1.196954002 |
| New York | 0.340094743 |
| North Carolina | 0.54052828 |
| North Dakota | 0.312859548 |
| Ohio | 0.446518179 |
| Oklahoma | 0.127157003 |
| Oregon | −0.624085962 |
| Pennsylvania | 0.39290517 |
| Rhode island | −0.637706676 |
| South Carolina | 0.316076419 |
| South Dakota | 0.509147968 |
| Tennessee | 0.698644606 |
| Texas | −1.111367825 |
| Utah | −0.264389678 |
| Vermont | −0.492881888 |
| Virginia | −0.454053702 |
| Washington | −0.797251392 |
| West Virginia | 0.638810582 |
| Wisconsin | 0.383011156 |
| Wyoming | 0.721386309 |
Note: Darker shade reflects higher values of the state-level systemic inequity score
Appendix 4.
Multinomial models estimating associations between systemic inequities and health problems in Latino children (n=17,855) ages 3 – 17 years
| Model 1 | Model 2 | |||
|---|---|---|---|---|
| AOR | (95% CI) | AOR | (95% CI) | |
| Health difficulties | ||||
| 0 | 1.00 | 1.00 | ||
| 1 | 0.95 | (0.85, 1.06) | 0.94 | (0.84, 1.05) |
| 2+ | 1.00 | (0.88, 1.15) | 0.99 | (0.86, 1.13) |
| Wald p-value | 0.67 | 0.55 | ||
| Chronic physical health conditions | ||||
| 0 | 1.00 | 1.00 | ||
| 1 | 1.13 | (1.02, 1.25) | 1.13 | (1.02, 1.24) |
| 2+ | 1.20 | (1.00, 1.45) | 1.20 | (0.99, 1.44) |
| Wald p-value | 0.02 | 0.02 | ||
| Mental health conditions | ||||
| 0 | 1.00 | 1.00 | ||
| 1 | 1.08 | (0.92, 1.26) | 1.07 | (0.92, 1.24) |
| 2+ | 1.27 | (1.09, 1.48) | 1.24 | (1.06, 1.45) |
| Wald p-value | 0.01 | 0.03 | ||
| # of health dimensions with 1+ condition | ||||
| 0 | 1.00 | 1.00 | ||
| 1 | 1.04 | (0.95, 1.14) | 1.04 | (0.95, 1.13) |
| 2 | 1.12 | (0.98, 1.28) | 1.11 | (0.98, 1.27) |
| 3 | 1.19 | (0.97, 1.47) | 1.15 | (0.93, 1.42) |
| Wald p-value | 0.18 | 0.32 | ||
Notes: AOR=adjusted odds ratios. Model 1 is adjusted for child’s age, sex, survey year, family immigration history, mother’s age at child’s birth, and state income inequality. Model 2 is adjusted for covariates in Model 1, in addition to personal experience of racism, household income, highest education in household, social service use index, neighborhood safety, insurance status, caregiver health index, family structure, and state income inequality. OR=odds ratio; CI=confidence interval. Values for Model 2 correspond to the values presented in Figure 2.
Footnotes
Conflicts of Interest Disclosure: The authors have no conflicts of interest to disclose.
References
- 1.Child Trends. Racial and ethnic composition of the child population. 2018:2019. [Google Scholar]
- 2.Urquhart A, Clarke P. US racial/ethnic disparities in childhood asthma emergent health care use: National Health Interview Survey, 2013–2015. J Asthma. 2020;57(5):510–520. [DOI] [PubMed] [Google Scholar]
- 3.United States Environmental Protection Agency. America’s Children and the Environment 2019. [Google Scholar]
- 4.Weaver RG, Brazendale K, Hunt E, Sarzynski MA, Beets MW, White K. Disparities in childhood overweight and obesity by income in the United States: an epidemiological examination using three nationally representative datasets. International Journal of Obesity. 2019;43(6):1210–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Skinner AC, Ravanbakht SN, Skelton JA, Perrin EM, Armstrong SC. Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics. 2018;141(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Guglielmo D, Gazmararian JA, Chung J, Rogers AE, Hale L. Racial/ethnic sleep disparities in US school-aged children and adolescents: a review of the literature. Sleep Health. 2018;4(1):68–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ash T, Davison KK, Haneuse S, Horan C, Kitos N, Redline S, et al. Emergence of racial/ethnic differences in infant sleep duration in the first six months of life. Sleep Medicine: X. 2019;1:100003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith JP, Hardy ST, Hale LE, Gazmararian JA. Racial disparities and sleep among preschool aged children: a systematic review. Racial disparities and sleep among preschool aged children: a systematic review. Sleep Health. 2019;5(1):49–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmeer KK, Tarrence J. Racial-ethnic Disparities in Inflammation: Evidence of Weathering in Childhood? J Health Soc Behav. 2018;59(3):411–428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. The Lancet. 2017;389(10077):1453–1463. [DOI] [PubMed] [Google Scholar]
- 11.Williams DR, Whitfield KE. Racism and health. Closing the Gap: Improving the Health of Minority Elders in the New Millennium. 2004. [Google Scholar]
- 12.Hatzenbuehler ML. Structural stigma and health. The Oxford handbook of stigma, discrimination, and health. 2017:1–28. [Google Scholar]
- 13.Hatzenbuehler ML, Link BG. Introduction to the special issue on structural stigma and health. Social Science & Medicine. 2014. [DOI] [PubMed] [Google Scholar]
- 14.Lukachko A, Hatzenbuehler ML, Keyes KM. Structural racism and myocardial infarction in the United States. Social Science & Medicine. 2014;103:42–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.HPA Hardeman R. R., Chantarat T, Davis BA, Brown TH Improving The Measurement Of Structural Racism To Achieve Antiracist Health Policy. Health Affairs. 2022;41(2):179–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Braveman P. A. AE, Proctor D, Kauh T, and Holm N Systemic And Structural Racism: Definitions, Examples, Health Damages, And Approaches To Dismantling. Health Affairs. 2022;41(2):171–178. [DOI] [PubMed] [Google Scholar]
- 17.Trent M, Dooley DG, Dougé J. The Impact of Racism on Child and Adolescent Health. Pediatrics. 2019;144(2):e20191765. [DOI] [PubMed] [Google Scholar]
- 18.Malawa Z, Gaarde J, Spellen S. Racism as a root cause approach: A new framework. Pediatrics. 2021;147(1). [DOI] [PubMed] [Google Scholar]
- 19.Williams DR, Lawrence JA, Davis BA. Racism and health: evidence and needed research. Annual review of public health. 2019;40:105–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cave L, Cooper MN, Zubrick SR, Shepherd CC. Racial discrimination and child and adolescent health in longitudinal studies: a systematic review. Social science & medicine. 2020;250:112864. [DOI] [PubMed] [Google Scholar]
- 21.Alson JG, Robinson WR, Pittman L, Doll KM. Incorporating Measures of Structural Racism into Population Studies of Reproductive Health in the United States: A Narrative Review. Health Equity. 2021;5(1):49–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Groos M, Wallace M, Hardeman R, Theall KP. Measuring inequity: a systematic review of methods used to quantify structural racism. Journal of Health Disparities Research and Practice. 2018;11(2):13. [Google Scholar]
- 23.Hardy LJ, Getrich CM, Quezada JC, Guay A, Michalowski RJ, Henley E. A Call for Further Research on the Impact of State-Level Immigration Policies on Public Health. Am J Public Health. 2012;102(7):1250–1253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Trawalter S, Bart-Plange D-J, Hoffman KM. A socioecological psychology of racism: making structures and history more visible. Current opinion in psychology. 2020;32:47–51. [DOI] [PubMed] [Google Scholar]
- 25.Neblett EW Jr. Racism and health: Challenges and future directions in behavioral and psychological research. Cultural Diversity and Ethnic Minority Psychology. 2019;25(1):12. [DOI] [PubMed] [Google Scholar]
- 26.Hatzenbuehler ML, Prins SJ, Flake M, Philbin M, Frazer MS, Hagen D, et al. Immigration policies and mental health morbidity among Latinos: A state-level analysis. Social science & medicine. 2017;174:169–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Philbin MM, Flake M, Hatzenbuehler ML, Hirsch JS. State-level immigration and immigrant-focused policies as drivers of Latino health disparities in the United States. Social Science & Medicine. 2018;199:29–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Vernice NA, Pereira NM, Wang A, Demetres M, Adams LV. The adverse health effects of punitive immigrant policies in the United States: A systematic review. PLoS One. 2020;15(12):e0244054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sudhinaraset M, Woofter R, Young M-EDT, Landrian A, Vilda D, Wallace SP. Analysis of State-Level Immigrant Policies and Preterm Births by Race/Ethnicity Among Women Born in the US and Women Born Outside the US. JAMA Network Open. 2021;4(4):e214482–e214482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Torche F, Sirois C. Restrictive immigration law and birth outcomes of immigrant women. American journal of epidemiology. 2019;188(1):24–33. [DOI] [PubMed] [Google Scholar]
- 31.Wallace M, Crear-Perry J, Richardson L, Tarver M, Theall K. Separate and unequal: Structural racism and infant mortality in the US. Health & place. 2017;45:140–144. [DOI] [PubMed] [Google Scholar]
- 32.Stanhope KK, Hogue CR, Suglia SF, Leon JS, Kramer MR. Restrictive sub-federal immigration policy climates and very preterm birth risk among US-born and foreign-born Hispanic mothers in the United States, 2005–2016. Health & Place. 2019;60:102209. [DOI] [PubMed] [Google Scholar]
- 33.Crookes DM, Stanhope KK, Kim YJ, Lummus E, Suglia SF. Federal, State, and Local Immigrant-Related Policies and Child Health Outcomes: a Systematic Review. J Racial Ethn Health Disparities. 2021:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.White K, Blackburn J, Manzella B, Welty E, Menachemi N. Changes in use of county public health services following implementation of Alabama’s immigration law. Journal of health care for the poor and underserved. 2014;25(4):1844–1852. [DOI] [PubMed] [Google Scholar]
- 35.Toomey RB, Umaña-Taylor AJ, Williams DR, Harvey-Mendoza E, Jahromi LB, Updegraff KA. Impact of Arizona’s SB 1070 immigration law on utilization of health care and public assistance among Mexican-origin adolescent mothers and their mother figures. Am J Public Health. 2014;104 Suppl 1(Suppl 1):S28–S34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Potochnick S, Chen J-H, Perreira K. Local-level immigration enforcement and food insecurity risk among Hispanic immigrant families with children: National-level evidence. Journal of Immigrant and Minority Health. 2017;19(5):1042–1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Krieger N, Huynh M, Li W, Waterman PD, Van Wye G. Severe sociopolitical stressors and preterm births in New York City: 1 September 2015 to 31 August 2017. J Epidemiol Community Health. 2018;72(12):1147–1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gemmill A, Catalano R, Casey JA, Karasek D, Alcalá HE, Elser H, et al. Association of preterm births among US latina women with the 2016 presidential election. JAMA network open. 2019;2(7):e197084–e197084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Novak NL, Geronimus AT, Martinez-Cardoso AM. Change in birth outcomes among infants born to Latina mothers after a major immigration raid. Int J Epidemiol. 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hatzenbuehler ML, Weissman DG, McKetta S, Lattanner MR, Ford JV, Barch DM, & McLaughlin KA Smaller hippocampal volume among Black and Latinx youth living in high-stigma contexts. Journal of the American Academy of Child and Adolescent Psychiatry. 2022;6(61):809–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Roche KM, White RMB, Rivera MI, Safa MD, Newman D, Falusi O. Recent immigration actions and news and the adjustment of U.S. Latino/a adolescents. Cultur Divers Ethnic Minor Psychol. 2021;27(3):447–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Eskenazi B, Fahey CA, Kogut K, Gunier R, Torres J, Gonzales NA, et al. Association of Perceived Immigration Policy Vulnerability With Mental and Physical Health Among US-Born Latino Adolescents in California. JAMA Pediatrics. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shadmi E Multimorbidity and equity in health. BioMed Central; 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cornish RP, Boyd A, Van Staa T, Salisbury C, Macleod J. Socio-economic position and childhood multimorbidity: a study using linkage between the Avon Longitudinal study of parents and children and the general practice research database. International journal for equity in health. 2013;12(1):1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Russell J, Grant CC, Morton SM. Multimorbidity in early childhood and socioeconomic disadvantage: findings from a large New Zealand child cohort. Academic pediatrics. 2020;20(5):619–627. [DOI] [PubMed] [Google Scholar]
- 46.Bright MA, Thompson LA. Association of Adverse Childhood Experiences with Co-occurring Health Conditions in Early Childhood. J Dev Behav Pediatr. 2018;39(1):37–45. [DOI] [PubMed] [Google Scholar]
- 47.Shonkoff JP, Slopen N, Williams DR. Early childhood adversity, toxic stress, and the impacts of racism on the foundations of health. Annual Review of Public Health. 2021;42:115–134. [DOI] [PubMed] [Google Scholar]
- 48.Boyce WT, Sokolowski MB, Robinson GE. Genes and environments, development and time. Proceedings of the National Academy of Sciences. 2020;117(38):23235–23241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Acevedo-Garcia D, Noelke C, McArdle N, Sofer N, Hardy EF, Weiner M, et al. Racial And Ethnic Inequities In Children’s Neighborhoods: Evidence From The New Child Opportunity Index 2.0. Health Affairs. 2020;39(10):1693–1701. [DOI] [PubMed] [Google Scholar]
- 50.Quiroga SS, Medina DM, Glick J. In the Belly of the Beast: Effects of Anti-Immigration Policy on Latino Community Members. American Behavioral Scientist. 2014. [Google Scholar]
- 51.Gonzalez D, Karpman M, Kenney GM, Zuckerman S. Hispanic adults in families with noncitizens disproportionately feel the economic fallout from COVID-19. Washington, DC: Urban Institute. 2020. [Google Scholar]
- 52.Vaughan JM, Griffith B. Map: Sanctuary Cities, Counties, and States. https://cis.org/Map-Sanctuary-Cities-Counties-and-States. Published 2023. Accessed 3/16/2023. [Google Scholar]
- 53.Jackson DB, Posick C, Vaughn MG. New evidence of the nexus between neighborhood violence, perceptions of danger, and child health. Health Affairs. 2019;38(5):746–754. [DOI] [PubMed] [Google Scholar]
- 54.Flores RD. Do anti-immigrant laws shape public sentiment? A study of Arizona’s SB 1070 using Twitter data. American Journal of Sociology. 2017;123(2):333–384. [Google Scholar]
- 55.Meyer IH. Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychol Bull. 2003;129(5):674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Link BG, Phelan JC. Conceptualizing Stigma. Annual Review of Sociology. 2001;27:363–385. [Google Scholar]
- 57.Rhodes SD, Mann-Jackson L, Song EY, Wolfson M, Filindra A, Hall M. Laws and Policies Related to the Health of US Immigrants: A Policy Scan. Health Behav Policy Rev. 2020;7(4):314–324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.McKetta S, Hatzenbuehler ML, Pratt C, Bates L, Link BG, Keyes KM. Does social selection explain the association between state-level racial animus and racial disparities in self-rated health in the United States? Annals of epidemiology. 2017;27(8):485–492. e486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Charles KK, Guryan J, Pan J. The effects of sexism on American women: The role of norms vs. discrimination: National Bureau of Economic Research; 2018. [Google Scholar]
- 60.Batalova JH M; Levesque C Frequently Requested Statistics on Immigrants and Immigration in the United States. https://www.migrationpolicy.org/article/frequently-requested-statistics-immigrants-and-immigration-united-states-2020. Published 2021. Accessed 8/11, 2021.
- 61.Browne I, Tatum K, Gonzalez B. Presumed Mexican Until Proven Otherwise: Identity Work and Intersectional Typicality among Middle-Class Dominican and Mexican Immigrants. Social Problems. 2020;68(1):80–99. [Google Scholar]
- 62.Hanley JA, Negassa A, Edwardes MDd, Forrester JE. Statistical analysis of correlated data using generalized estimating equations: an orientation. American journal of epidemiology. 2003;157(4):364–375. [DOI] [PubMed] [Google Scholar]
- 63.Kwak C, Clayton-Matthews A. Multinomial logistic regression. Nursing research. 2002;51(6):404–410. [DOI] [PubMed] [Google Scholar]
- 64.Vargas ED, Sanchez GR, Juárez M. Fear by Association: Perceptions of Anti-Immigrant Policy and Health Outcomes. Journal of Health Politics, Policy and Law. 2017;42(3):459–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Vargas ED, Ybarra VD. U.S. Citizen Children of Undocumented Parents: The Link Between State Immigration Policy and the Health of Latino Children. J Immigr Minor Health. 2017;19(4):913–920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rose G Sick individuals and sick populations. International Journal of Epidemiology. 1985;14(1):32. [DOI] [PubMed] [Google Scholar]
- 67.Greenwald AG, Banaji MR, Nosek BA. Statistically small effects of the Implicit Association Test can have societally large effects. 2015. [DOI] [PubMed] [Google Scholar]
- 68.Anderson AT, Luartz L, Heard-Garris N, Widaman K, Chung PJ. The detrimental influence of racial discrimination on child health in the United States. Journal of the National Medical Association. 2020;112(4):411–422. [DOI] [PubMed] [Google Scholar]
- 69.Priest N, Paradies Y, Trenerry B, Truong M, Karlsen S, Kelly Y. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Social Science & Medicine. 2013;95:115–127. [DOI] [PubMed] [Google Scholar]
- 70.Bennett M, Roche KM, Huebner DM, Lambert SF. School discrimination and changes in Latinx adolescents’ internalizing and externalizing symptoms. Journal of youth and adolescence. 2020;49(10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Sewell AA. Political economies of acute childhood illnesses: measuring structural racism as mesolevel mortgage market risks. Ethnicity & Disease. 2021;31(Suppl):319–332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Aris IM, Rifas-Shiman SL, Jimenez MP, Li LJ, Hivert MF, Oken E, et al. Neighborhood Child Opportunity Index and Adolescent Cardiometabolic Risk. Pediatrics. 2021;147(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Krager MK, Puls HT, Bettenhausen JL, Hall M, Thurm C, Plencner LM, et al. The Child Opportunity Index 2.0 and Hospitalizations for Ambulatory Care Sensitive Conditions. Pediatrics. 2021:e2020032755. [DOI] [PubMed] [Google Scholar]
- 74.Merikangas KR, J-p He, Burstein M, Swendsen J, Avenevoli S, Case B, et al. Service utilization for lifetime mental disorders in US adolescents: results of the National Comorbidity Survey–Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50(1):32–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Shi Y, Guevara LRH, Dykhoff HJ, Sangaralingham LR, Phelan S, Zaccariello MJ, et al. Racial disparities in diagnosis of attention-deficit/hyperactivity disorder in a US national birth cohort. JAMA network open. 2021;4(3):e210321–e210321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.McNutt L-A, Wu C, Xue X, Hafner JP. Estimating the relative risk in cohort studies and clinical trials of common outcomes. American journal of epidemiology. 2003;157(10):940–943. [DOI] [PubMed] [Google Scholar]
- 77.Currie J, Stabile M. Child mental health and human capital accumulation: the case of ADHD. Journal of health economics. 2006;25(6):1094–1118. [DOI] [PubMed] [Google Scholar]
- 78.Mikkonen J, Moustgaard H, Remes H, Martikainen P. The Population Impact of Childhood Health Conditions on Dropout from Upper-Secondary Education. The Journal of Pediatrics. 2018;196:283–290.e284. [DOI] [PubMed] [Google Scholar]
- 79.Allison MA, Attisha E, HEALTH COS. The Link Between School Attendance and Good Health. Pediatrics. 2019;143(2):e20183648. [DOI] [PubMed] [Google Scholar]
- 80.Charach A, Yeung E, Climans T, Lillie E. Childhood Attention-Deficit/Hyperactivity Disorder and Future Substance Use Disorders: Comparative Meta-Analyses. Journal of the American Academy of Child & Adolescent Psychiatry. 2011;50(1):9–21. [DOI] [PubMed] [Google Scholar]
- 81.Copeland WE, Alaie I, Jonsson U, Shanahan L. Associations of childhood and adolescent depression with adult psychiatric and functional outcomes. Journal of the American Academy of Child & Adolescent Psychiatry. 2021;60(5):604–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Smith JP. The impact of childhood health on adult labor market outcomes. The review of economics and statistics. 2009;91(3):478–489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Currie J Child health as human capital. Health Economics. 2020;29(4):452–463. [DOI] [PubMed] [Google Scholar]
- 84.Braveman P, Barclay C. Health disparities beginning in childhood: a life-course perspective. Pediatrics. 2009;124 Suppl 3:S163–175. [DOI] [PubMed] [Google Scholar]
- 85.Linton JM, Nagda J, Falusi OO. Advocating for Immigration Policies that Promote Children’s Health. Pediatr Clin North Am. 2019;66(3):619–640. [DOI] [PubMed] [Google Scholar]
- 86.Boyce WT, Levitt P, Martinez FD, McEwen BS, Shonkoff JP. Genes, environments, and time: the biology of adversity and resilience. Pediatrics. 2021;1047(2). [DOI] [PubMed] [Google Scholar]
- 87.Heard-Garris N, Cale M, Camaj L, Hamati M, Dominguez T. Transmitting Trauma: A systematic review of vicarious racism and child health. Social Science & Medicine. 2017. [DOI] [PubMed] [Google Scholar]
- 88.Shonkoff J, Boyce WT, Bush N, Gunnar M, Hensch TK, Levitt P, Meaney M, Nelson C, Slopen N, Williams D, Silveira P. Translating the biology of adversity and resilience into new measures for pediatric practice. Pediatrics. 2022;In press. [DOI] [PubMed] [Google Scholar]
- 89.Perreira KM, Pedroza JM. Policies of exclusion: Implications for the health of immigrants and their children. Annual review of public health. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Potochnick S How states can reduce the dropout rate for undocumented immigrant youth: The effects of in-state resident tuition policies. Social Science Research. 2014;45:18–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Kaushal N In-state tuition for the undocumented: Education effects on Mexican young adults. Journal of Policy Analysis and Management. 2008;27(4):771–792. [Google Scholar]
- 92.Orrenius PM, Zavodny M. The impact of E-Verify mandates on labor market outcomes. Southern Economic Journal. 2015;81(4):947–959. [Google Scholar]
- 93.M-E De Trinidad Young, León-Pérez G, Wells CR, Wallace SP. More Inclusive States, Less Poverty Among Immigrants? An Examination of Poverty, Citizenship Stratification, and State Immigrant Policies. Population Research and Policy Review. 2018;37(2):205–228. [Google Scholar]
- 94.Hainmueller J, Lawrence D, Martén L, Black B, Figueroa L, Hotard M, et al. Protecting unauthorized immigrant mothers improves their children’s mental health. Science. 2017;357(6355):1041–1044. [DOI] [PMC free article] [PubMed] [Google Scholar]


