Abstract
Purpose:
To evaluate the accuracy of intraocular lens (IOL) power prediction of the formulas available on the American Society of Cataract and Refractive Surgery (ASCRS) post-refractive calculator in eyes with prior radial keratotomy (RK) for myopia.
Methods:
This retrospective study included 25 eyes of 18 patients whose status was post-RK for treatment of myopia, which had undergone cataract extraction with IOL implantation. Prediction error was calculated as the difference between implanted IOL power and predicted power by various formulae available on ASCRS post-refractive calculator. The formulas compared were Humphrey Atlas method, IOLMaster/Lenstar method, Barrett True-K no-history formula, ASCRS Average power, and ASCRS Maximum power on ASCRS post-refractive calculator.
Results:
Median absolute errors were the least for Barrett True-K and ASCRS Maximum power, that is, 0.56 (0.25, 1.04) and 0.56 (0.25, 1.06) D, respectively, and that of Atlas method was 1.60 (0.85, 2.28) D. Median arithmetic errors were positive for Atlas, Barrett True-K, ASCRS Average (0.86 [−0.17, 1.61], 0.14 [−0.22 to 0.54], and 0.23 [−0.054, 0.76] D, respectively) and negative for IOLMaster/Lenstar method and ASCRS Maximum power (−0.02 [−0.46 to 0.38] and − 0.48 [−1.06 to − 0.22] D, respectively). Multiple comparison analysis of Friedman’s test revealed that Atlas formula was significantly different from IOLMaster/Lenstar, Barrett True-K, and ASCRS Maximum power; ASCRS Maximum power was significantly different from all others (P < 0.00001).
Conclusion:
In post-RK eyes, Barrett True-K no-history formula and ASCRS Maximum power given by the ASCRS calculator were more accurate than other available formulas, with ASCRS Maximum leading to more myopic outcomes when compared to others.
Keywords: American Society of Cataract and Refractive Surgery, cataract, intraocular lens calculator, radial keratotomy
Radial keratotomy (RK) was the most common refractive procedure in the late 1970s to 1980s.[1] In this procedure, four to 32 incisions are made to flatten the central cornea for correction of myopia, depending upon the amount of refractive error. An estimated 1.2 million individuals underwent the RK procedure between 1980 and 1990, and most of them are likely to eventually present with visually significant cataracts.[1]
Intraocular lens (IOL) power calculation after prior RK is widely known to lead to errors in IOL power estimation and postoperative hyperopic outcomes.[2,3,4,5,6] One of the major factors leading to errors was an error in estimated lens position (ELP) prediction in these eyes.[7] Various studies have shown accuracy in IOL power calculation in these eyes with the advent of specially developed regression formulas and with corneal powers obtained from different corneal topographers like Orbscan,[8] Pentacam,[9] and Atlas.[1]
The American Society of Cataract and Refractive Surgery (ASCRS) has provided a calculator online (www.iolcalc.ascrs.org), which incorporates different formulas for the calculation of IOL powers in eyes with prior RK and is shown to provide favorable results as reported by many studies.[10,11,12,13,14] Optical coherence tomography (OCT)-based IOL calculation formula and Barrett True-K formula are the most recent additions in the updated version 4.7, 2015 of the ASCRS calculator. In eyes with prior RK, though the existing formulas on the ASCRS calculator can predict IOL powers for emmetropia, further improvements in the methods of corneal power measurement and IOL power calculation are required for these eyes as reported by several studies.[15,16]
In this study, we aim to compare the accuracy of various IOL calculation formulae available on the ASCRS post-refractive surgery IOL calculator concerning IOL power prediction in eyes with prior RK.
Methods
Study design and setting
This retrospective study was undertaken in a tertiary eye care center after obtaining ethical clearance from the Institutional Review Board and adhering to the tenets of Declaration of Helsinki.
Study participants
Twenty-five eyes of 18 patients whose status was post-RK with subsequent cataract extraction and IOL implantation performed by five surgeons at a tertiary care center between January 2018 and October 2022 were included. We included all cases with uncomplicated refractive surgery who underwent cataract extraction or clear lens exchange between January 2018 and October 2022, with at least 1-month follow-up after cataract surgery. All cases with eventful cataract surgery, those requiring IOL explantation or exchange later, and those lost to follow-up at 1 month after surgery were excluded from our study.
Biometry and IOL power calculation
Optical biometry values were obtained from either Lenstar LS900 (Software EyeSuite i9.6.3.0; Haag Streit Diagnostics, Koniz, Switzerland) or IOLMaster 700 (version 1.07; Carl Zeiss Meditech, Jena, Germany). Keratometry values for 1–4 mm zones were obtained from the Holladay equivalent keratometry readings (EKR) report of Pentacam HR (version 1.22r05; Oculus Inc, Wetzlar, Germany). The RK module for prior RK available on ASCRS post-refractive IOL calculator (www.iolcalc.ascrs.org) was used to calculate IOL powers in these eyes. In the RK calculator of ASCRS, we used −1.00 D as the target refraction for eyes with eight RK incisions, −1.5 D for eyes with 12 RK incisions and for those with six RK cuts and two arcuate keratotomy (AK) incisions, and −2.00 D for eyes with 16 RK incisions.[17] The IOL power calculation methods compared in this study were Humphrey Atlas method, IOLMaster/Lenstar method, Barrett True-K formula, ASCRS Average power, and ASCRS Maximum power.
Surgical technique
Phacoemulsification was performed in all cases with a 2.8 temporal clear corneal incision using the Alcon Centurion phacoemulsification system (Alcon Laboratories, Fort Worth, TX, USA). IOLs implanted in the capsular bag were Tecnis ZCB00 (Johnson and Johnson), Tecnis Eyhance (Johnson and Johnson), Acrysof IQ (Alcon), Acriol EC, (Care Group,Vadodra, India).
Outcome measures
Postoperatively, data were obtained 1 month after surgery. Prediction error (PE) was calculated by subtracting the predicted IOL power given by each of the five formulas on the ASCRS calculator taken into consideration in this study from the implanted IOL power. A positive value of PE (predicted IOL power lesser than the power of the implanted IOL) would lead to a hyperopic outcome. Conversely, a negative value of PE would lead to a myopic outcome. Media Absolute Error (MedAE) was calculated for each formula by obtaining the absolute values of the arithmetic PE and then deriving the median of those values.
Statistical analysis
Statistical analysis was performed using MedCalc® Statistical Software version 20.112 (MedCalc Software Ltd, Ostend, Belgium; https://www.medcalc.org; 2022). All calculated values were medians with 95% confidence interval. The normality of data was checked using the Kolmogorov–Smirnov test and since the data was not normally distributed, a nonparametric Friedman’s test was used to compare PEs of different formulas on the post-RK module of ASCRS post-refractive calculator. Snellen’s visual acuity was converted to and presented as log of minimum angle of resolution (logMAR) acuity. Results calculated for each formula were as follows: median arithmetic IOL PE (with 95% confidence interval), median absolute IOL PE (with 95% confidence interval), MedAE (with 95% confidence interval [CI]), and refractive error within ±0.5, ±1.00, ±1.5, ±2.00, and ±2.50 D. Wilcoxon signed-rank test was used to analyze the level of significance between the preoperative and postoperative spherical equivalent (SE). A P value of less than 0.05 was considered statistically significant.
Results
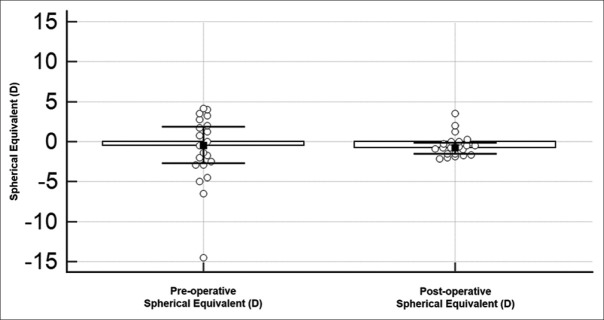
Twenty-five eyes of 18 patients were included in this study. Fourteen (56.00%) eyes were right eyes and 11 (44.00%) eyes were left eyes. The median age of the included patients was 51.00 (47.40, 54.60) years. There were 12 males (66.66%) and six females (33.33%). The median axial length was 26.58 (24.81, 27.75) mm. The median number of RK incisions was 8 (8.00, 14.60). Median IOL power implanted was +22.50 (20.15, 25.00) D [Table 1]. Among patients with prior RK, 12 eyes had eight RK incisions, two eyes had six RK and two AK incisions, four eyes had 12 RK incisions, and seven eyes had 16 RK incisions. The median preoperative logMAR uncorrected visual acuity (UCVA) and best-corrected visual acuity (BCVA) were 0.6 (0.48, 0.99) and 0.3 (0.30, 0.40), respectively, and the median postoperative UCVA and BCVA were 0.30 (0.30, 0.48) and 0.1 (0.00, 0.18), respectively. The median difference between preoperative and postoperative SE was 0.38 D (−1.56 to 1.94), but it was not statistically significant (P value: 0.87) [Fig. 1].
Table 1.
Demographics of patients
| n=25 eyes | Median (95% CI) | Range |
|---|---|---|
| Age at cataract surgery (years) | 51.00 (47.40, 54.60) | 29–79 |
| Pre-cataract surgery SE (D) | −0.50 (−2.67, 1.86) | -14.50 to 4.13 |
| Post-cataract surgery SE (D) | −0.63 (−1.08, −0.29) | -2.13 to 3.5 |
| Axial length (mm) | 26.58 (24.81, 27.75) | 23.84–31.95 |
| Implanted IOL power (D) | 22.50 (20.15, 25.00) | 6.5–29 |
| Number of RK incisions | 8 (8.00, 14.60) | 8–16 |
CI=Confidence interval, IOL=Intraocular lens, RK=Radial keratotomy, SE=Spherical equivalent
Figure 1.
Wilcoxon ranked-sum test for preoperative and postoperative spherical equivalent
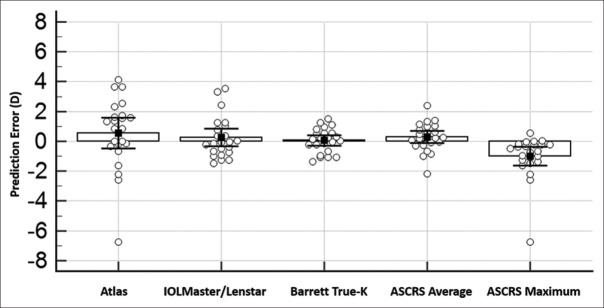
IOL PE was calculated for each formula for all included 25 post-RK eyes [Fig. 2]. MedAE for Barrett True-K and ASCRS Maximum power were the lowest, that is, 0.56 (0.25, 1.04) and 0.56 (0.25, 1.06) D, respectively, when compared to Atlas, IOLMaster/Lenstar, and ASCRS Average, that is, 1.6 (0.85, 2.28), 0.75 (0.37, 1.21), and 0.63 (0.24, 1.00) D, respectively [Table 2]. Multiple comparison analysis of Friedman’s test revealed that the Atlas formula was significantly different from IOLMaster/Lenstar, Barrett True-K, and ASCRS Maximum power, the IOLMaster/Lenstar formula and the Barrett True-K were each significantly different from Atlas and ASCRS Maximum formulas, ASCRS Average formula was significantly different from ASCRS Maximum power, and ASCRS Maximum power was significantly different from all the others (P < 0.00001). Using the assumption that every 1.00 D of error in IOL power causes 0.7 D error in refractive error at the spectacle plane,[18] we calculated the percentage of eyes within IOL power PE of ±0.5, ±1.00, ±1.5, ±2.00, and ±2.50D [Table 3]. In the two eyes of the same patient with six RK and two AK incisions (cases 14 and 15), we targeted −1.50 D. In these eyes, the preoperative logMAR UCVA of the right eye was 0.9 and BCVA was 0.3, while the preoperative logMAR UCVA and BCVA of the left eye were 0.4 and 0.1, respectively. The postoperative logMAR UCVA and BCVA in the right eye were 0.3 and 0.1, and those in the left eye were 0.3 and 0.0, respectively. The preoperative and postoperative SE in the right eye were −2.00 and −0.63 D, respectively, and those in the left eye were 1.75 and −0.88, respectively. To the best of our knowledge, there are no studies assessing the impact of prior AK on IOL power calculation.
Figure 2.
Friedman’s test for analyzing IOL power prediction error for each formula. IOL = intraocular lens
Table 2.
IOL prediction error for each formula
| IOL prediction error (RK), (n=25) | ||||
|---|---|---|---|---|
|
| ||||
| Arithmetic median (D) | Arithmetic range (D) | Absolute median (D) | Absolute range (D) | |
| Atlas | 0.86 (−0.17, 1.61) | −6.73 to 4.13 | 1.6 (0.85, 2.28) | 0.00–6.73 |
| IOLMaster/Lenstar | −0.02 (−0.46, 0.38) | −1.49 to 3.54 | 0.75 (0.37, 1.21) | 0.02–3.54 |
| Barrett True-K | 0.14 (−0.22 to 0.54) | −1.35 to 1.72 | 0.56 (0.25, 1.04) | 0.03–1.72 |
| ASCRS Average power | 0.23 (−0.054, 0.76) | −2.18 to 2.38 | 0.63 (0.24, 1.00) | 0.02–2.38 |
| ASCRS Maximum power | −0.48 (−1.06, −0.22) | −6.73 to 0.56 | 0.56 (0.25, 1.06) | 0.00–6.73 |
ASCRS=American Society of Cataract and Refractive Surgery, IOL=Intraocular lens, RK=Radial keratotomy
Table 3.
Percentage of eyes within refractive prediction error of ±0.5, ±1.00, ±1.5, ±2.00, and±2.50 D for each method
| Status post-RK (n=25) | |||||
|---|---|---|---|---|---|
|
| |||||
| Percentage of eyes within refractive error of | |||||
| Formula | ±0.5 D | ±1.00 D | ±1.50 D | ±2.00 D | ±2.50 D |
| Atlas | 10.64% | 21.28% | 31.91% | 40.43% | 40.43% |
| IOLMaster/Lenstar | 48.00% | 84.00% | 88.00% | 92.00% | 100.00% |
| Barrett True-K | 56.00% | 92.00% | 100.00% | 100.00% | 100.00% |
| ASCRS Average | 56.00% | 92.00% | 92.00% | 100.00% | 100.00% |
| ASCRS Maximum | 52.00% | 80.00% | 88.00% | 96.00% | 96.00% |
ASCRS=American Society of Cataract and Refractive Surgery, IOL=Intraocular lens, RK=Radial keratotomy
Discussion
After RK, there is central corneal flattening which causes ELP to erroneously shift more posteriorly, leading to the selection of a lower IOL power and consequent postoperative hyperopia. ASCRS post-refractive calculator is freely available to use online and is easily accessible at www.iolcalc.ascrs.org.[19] It provides three separate calculators for prior RK, prior myopic Laser Assisted In Situ Keratomileusis/Photo Refractive Keratectomy (LASIK/PRK), and prior hyperopic-LASIK/PRK and facilitates the automated generation of a range of IOL powers using various methods incorporated in it, like topography-based methods, biometry-based methods, and Barrett True-K formula, and also generates an average of these IOL powers and the minimum and maximum IOL powers out of the ones calculated.[19] In this study, we evaluated the accuracy of IOL calculation formulas available on ASCRS post-refractive calculator.
Our results revealed that Barrett True-K formula was more accurate than the others on the calculator with respect to the arithmetic and absolute median PE within 95% CI and MedAE. Both Barrett True-K and ASCRS Maximum power showed the least MedAE, that is, 0.56 D (0.25, 1.04) and 0.56 (0.25, 1.06), respectively, when compared to other formulas.
In the present study, at 1 month after surgery, four eyes with eight RK incisions had no spherical error, three eyes had a hyperopic refractive error, and five eyes had a myopic error. Two eyes with 12 RK incisions had no spherical error and two eyes had a myopic error. Two eyes with 16 RK incisions had no spherical error and two eyes had hyperopic error, whereas three eyes had a myopic outcome. Both eyes with six RK incisions and two AK incisions had a myopic error. However, longer follow-ups are necessary to better assess outcomes in these eyes.
Hyperopic outcomes after RK have been related to delayed incisional healing in these eyes. Thus, many clinicians have proposed that the more the number of incisions in RK, the more the chances of hyperopic outcomes after surgery.[22]
Limitations of the present study include shorter follow-up and lack of stratification of the number of RK incisions. Corneal Analysis System (EyeSys Technologies) was not used in our evaluation before surgery in the RK module. Also, we were unable to use the central corneal power method due to the lack of required data for the same. Humphrey Atlas (Carl Zeiss Meditec, Dublin, CA, USA) was not used in our preoperative evaluation. In this study, we have used the Pentacam Holladay EKR map zone values for Atlas ring values due to nonavailability of the latter at the time the included patients were operated on. This method, however, has continued to provide close to accurate IOL power prediction and consequent favorable results. Another limitation is that surgeries in this study were performed by five surgeons, and the difference between their surgical techniques may lead to different outcomes. With regards to the two eyes with RK and AK for which target refraction was taken as −1.50 D, a larger number of samples with AK incisions may be required to better assess the impact of AK incisions with RK on IOL power calculations. Table 4 shows 3 different previous studies to compare with our current study.
Table 4.
Comparison with similar studies conducted previously
| Study | Inferences | Other relevant details of previous study | Comparison of present study |
|---|---|---|---|
| Demill et al. evaluated the use of ASCRS calculator in eyes with prior RK. Formulas evaluated were the Humphrey Atlas method, average central power method, and the average ASCRS power. In our study, we have not compared the average central power method | ASCRS Average best predicts the IOL power | They recommended adding +1.00 to +1.50 D to the final power to achieve emmetropic outcomes | We have chosen -1.00 and−2.00 D as target refraction in the RK calculator in corneas with eight RK incisions and 16 incisions, respectively, to achieve emmetropia.[1] Barrett True-K had the highest percentage of eyes within±0.5 D and the least MedAE, equal to that of ASCRS Maximum power compared to others[1] |
| Packer et al., in 2004, evaluated the efficacy of corneal topography in determining central corneal refractive power in IOL power calculations in eyes status post-incisional and thermal keratoplasties | They had 80% of outcomes within ±0.5 D with the average central power[20] | Eyes post-thermal keratoplasty were not included in this study | |
| Awwad et al. evaluated the efficacy of ACCP in IOL power prediction in status post-RK eyes | ACCP in 3-mm zone resulted in 87.5% of eyes being within ±0.5 D IOL prediction error | They used the same formula as the ASCRS calculator using measurements from the Topographic Modeling System (Tomey Corporation, Aichi, Japan)[21] | ACCP was not compared in the present study. Both Barrett True-K and ASCRS Average power had 56% of eyes within±0.50 D, but only Barrett True-K showed 100% of eyes within±1.50 D |
ACCP=Average central corneal power, ASCRS=American Society of Cataract and Refractive Surgery, IOL=Intraocular lens, RK=Radial keratotomy
ASCRS post-refractive calculator is a tool of great utility for the calculation of IOL power in eyes with prior RK. This study found that in post-RK eyes, Barrett True-K no-history formula and ASCRS Maximum power are more accurate, with the latter leading to more myopic outcomes compared to other formulas.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
This work was supported by Narayana Nethralaya Foundation. The funders had no role in the study design, data collection and analysis, decision to publish, or preparation of this abstract.
References
- 1.Demill DL, Hsu M, Moshirfar M. Evaluation of the American Society of Cataract and Refractive Surgery intraocular lens calculator for eyes with prior radial keratotomy. Clin Ophthalmol. 2011;5:1243–7. doi: 10.2147/OPTH.S24514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Koch DD, Liu JF, Hyde LL, Rock RL, Emery JM. Refractive complications of cataract surgery after radial keratotomy. Am J Ophthalmol. 1989;108:676–82. doi: 10.1016/0002-9394(89)90860-x. [DOI] [PubMed] [Google Scholar]
- 3.Hoffer KJ. Intraocular lens power calculation for eyes after refractive keratotomy. J Refract Surg. 1995;11:490–3. doi: 10.3928/1081-597X-19951101-17. [DOI] [PubMed] [Google Scholar]
- 4.Jt H. Consultations in refractive surgery: IOL calculations following radial keratotomy surgery. Refract Corneal Surg. 1989;5:203. [Google Scholar]
- 5.Seitz B, Langenbucher A, Nguyen NX, Kus MM, Küchle M. Underestimation of intraocular lens power for cataract surgery after myopic photorefractive keratectomy. Ophthalmology. 1999;106:693–702. doi: 10.1016/S0161-6420(99)90153-7. [DOI] [PubMed] [Google Scholar]
- 6.Odenthal MTP, Eggink CA, Melles G, Pameyer JH, Geerards AJM, Beekhuis WH. Clinical and theoretical results of intraocular lens power calculation for cataract surgery after photorefractive keratectomy for myopia. Arch Ophthalmol. 2002;120:431–8. doi: 10.1001/archopht.120.4.431. [DOI] [PubMed] [Google Scholar]
- 7.Shammas HJ, Shammas MC. No-history method of intraocular lens power calculation for cataract surgery after myopic laser in situ keratomileusis. J Cataract Refract Surg. 2007;33:31–6. doi: 10.1016/j.jcrs.2006.08.045. [DOI] [PubMed] [Google Scholar]
- 8.Arce CG, Soriano ES, Weisenthal RW, Hamilton SM, Rocha KM, Alzamora JB, et al. Calculation of intraocular lens power using Orbscan II quantitative area topography after corneal refractive surgery. J Refract Surg. 2009;25:1061–74. doi: 10.3928/1081597X-20091117-05. [DOI] [PubMed] [Google Scholar]
- 9.Potvin R, Hill W. New algorithm for post-radial keratotomy intraocular lens power calculations based on rotating Scheimpflug camera data. J Cataract Refract Surg. 2013;39:358–65. doi: 10.1016/j.jcrs.2012.09.019. [DOI] [PubMed] [Google Scholar]
- 10.Tang M, Li Y, Huang D. An Intraocular lens power calculation formula based on optical coherence tomography: A pilot study. J Refract Surg. 2010;26:430–7. doi: 10.3928/1081597X-20090710-02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang D, Tang M, Wang L, Zhang X, Armour RL, Gattey DM, et al. Optical coherence tomography–based corneal power measurement and intraocular lens power calculation following laser vision correction (An American Ophthalmological Society Thesis) Trans Am Ophthalmol Soc. 2013;111:34–45. [PMC free article] [PubMed] [Google Scholar]
- 12.Tang M, Wang L, Koch DD, Li Y, Huang D. Intraocular lens power calculation after previous myopic laser vision correction based on corneal power measured by Fourier-domain optical coherence tomography. J Cataract Refract Surg. 2012;38:589–94. doi: 10.1016/j.jcrs.2011.11.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang L, Tang M, Huang D, Weikert MP, Koch DD. Comparison of newer IOL power calculation methods for post-corneal refractive surgery eyes. Ophthalmology. 2015;122:2443–9. doi: 10.1016/j.ophtha.2015.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abulafia A, Hill WE, Koch DD, Wang L, Barrett GD. Accuracy of the Barrett True-K formula for intraocular lens power prediction after laser in situ keratomileusis or photorefractive keratectomy for myopia. J Cataract Refract Surg. 2016;42:363–9. doi: 10.1016/j.jcrs.2015.11.039. [DOI] [PubMed] [Google Scholar]
- 15.Leite de Pinho Tavares R, de Almeida Ferreira G, Ghanem VC, Ghanem RC. IOL Power calculation after radial keratotomy using the Haigis and Barrett True-K formulas. J Refract Surg. 2020;36:832–7. doi: 10.3928/1081597X-20200930-02. [DOI] [PubMed] [Google Scholar]
- 16.Ma JX, Tang M, Wang L, Weikert MP, Huang D, Koch DD. Comparison of newer IOL power calculation methods for eyes with previous radial keratotomy. Invest Ophthalmol Vis Sci. 2016;57:OCT162–8. doi: 10.1167/iovs.15-18948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dell S, Koch D, Mackool R, Masket S, Schultz M, Woodhams T. Assessing post-RK eyes. J Cataract Refract Surg Today. 2010 [Google Scholar]
- 18.American Academy of Ophthalmology. San Francisco, CA. Basic and clinical science course: Optics, refraction, and contact lenses. 1996–7;3:176. [Google Scholar]
- 19.American Society of Cataract and Refractive Surgery web site. [Last accessed on 2022 Nov 30]. Available from: http://wwwascrsorg .
- 20.Packer M, Brown LK, Hoffman RS, Fine IH. Intraocular lens power calculation after incisional and thermal keratorefractive surgery. J Cataract Refract Surg. 2004;30:1430–4. doi: 10.1016/j.jcrs.2004.02.075. [DOI] [PubMed] [Google Scholar]
- 21.Awwad ST, Dwarakanathan S, Bowman RW, Cavanagh HD, Verity SM, Mootha VV, et al. Intraocular lens power calculation after radial keratotomy: estimating the refractive corneal power. J Cataract Refract Surg. 2007;33:1045–50. doi: 10.1016/j.jcrs.2007.03.018. [DOI] [PubMed] [Google Scholar]
- 22.Analysis of intraocular lens power calculation in post-radial keratotomy eyes. [Last accessed on 2022 Nov 12]. Available from: https://pubmed.ncbi.nlm.nih.gov/12551669/ [DOI] [PubMed]