ABSTRACT
Introduction
Vertebrobasilar vascular pathology and upper cervical ligament instability may contraindicate the use of cervical manual therapy. We examined physical therapists’ documentation of screening for these conditions and hypothesized screening would be more common with specific risk factors and when using manual therapy.
Methods
This chart review included adults with neck pain presenting for outpatient physical therapy from 2015–2021. Exclusions were age<18 and history of cervical spine surgery. Demographics, vertebrobasilar and upper cervical ligament instability screening questions and examination tests, risk factors (i.e. hypertension, whiplash), and use of manual therapy were extracted.
Results
260 patients were included (mean age ± standard deviation 59.6 ± 16.2 years, 70.8% female). Physical therapists infrequently administered vertebrobasilar and upper cervical ligament instability tests (each<14%). Screening questions were generally more common (e.g. headache, visual disturbances; each>13%). There was no significant difference in any frequency of screening method given the presence of hypertension, whiplash, or use of manual therapy (p > .05 for each).
Conclusion
In the present study, physical therapists infrequently documented performance of vertebrobasilar or upper cervical ligament instability screening for adults with neck pain, even in the presence of risk factors or preceding manual therapy. Further research should corroborate these findings and explore reasons for use/avoidance of screening.
KEYWORDS: Vertebral Artery, Spinal manipulation, Physical examination, Medical history taking, Joint instability
Introduction
In the United States (US), patients with neck pain often present to physical therapists in the outpatient setting [1]. Accordingly, these providers must be prepared to encounter comorbid cervical vascular and ligamentous pathology that could contraindicate manual therapy treatment to the cervical spinal region [1,2]. For example, patients may have previously undiagnosed vascular disorders of the vertebrobasilar system (i.e. vertebral artery and posterior brain circulation) or upper cervical ligament instability. While recent clinical practice guidelines recommend administering screening questions for potential vertebrobasilar pathology or cervical ligament instability among patients with neck pain [1,2], specialized physical tests for these conditions are typically no longer recommended due to issues with reliability and accuracy [1–5]. However, little research has explored how frequently physical therapists administer such screening questions and tests for vertebrobasilar or cervical ligament pathology. Vertebral artery dissection, stroke, and posterior circulation insufficiency (transient hypoperfusion) are only a few of the disorders that fall under the category of vertebrobasilar pathology [2–4]. Several risk factors for these conditions have been described. For example, hypertension and smoking are relevant risk factors for insufficiency and stroke whereas trauma (e.g. whiplash) is a risk factor for vertebral artery dissection [2]. Vertebrobasilar pathology is relevant to physical therapists because it may initially manifest as neck pain and/or headache, so patients may present for physical therapy unaware that they have a vascular disorder [2,3]. Manual therapies like cervical joint mobilization or manipulation, or soft tissue therapies may be dangerous (i.e. contraindicated) in these patients, who should instead be referred for surgical consultation [2,6].
Upper cervical ligament instability is defined as a loss of structural integrity or pathologically increased mobility of the first and/or second cervical vertebrae [5]. Upper cervical instability typically arises following neck trauma, inflammatory arthritis, or in the context of certain congenital disorders, and may initially present as typical musculoskeletal neck pain [5]. As upper cervical ligament instability may increase the risk of vascular injury and myelopathy (i.e. spinal cord injury), cervical manual therapies are contraindicated in these patients [6]. Instead, such patients should be referred for surgical consultation.
Currently, clinical practice guidelines regarding neck pain from the Orthopaedic Section of the American Physical Therapy Association (2017) and International Federation of Orthopedic Manipulative Physical Therapists Incorporated (IFOMPT, 2022) recommend that physical therapists screen for cervical vascular pathology and ligamentous instability [1,2]. These guidelines note the value of documenting risk factors for vascular and ligamentous conditions (also referred to as ‘red flags’), and emphasize the importance of physical examination, including tests of neurological function such as a cranial nerve examination and motor, sensory and reflex tests [1,2]. While previous clinical practice guidelines recommended specific physical examination tests for vertebrobasilar pathology and upper cervical ligament instability, these tests have been found to have low reliability and accuracy [4,5] and thus have been left out of recent guidelines [1,2].
While survey studies have explored physical therapists reported use of vertebrobasilar and upper cervical ligament instability tests [7–9], we are not aware of any research that has examined physical therapists’ real-world use of screening for these conditions. An updated evaluation of physical therapists’ real-world practice patterns is required in light of the shifting paradigm that emphasizes screening via a detailed history of risk factors rather than specific physical examination tests [1,2].
Our study investigated the documented utilization of various screening techniques by physical therapists in context of the guidelines for physical therapists to screen for vertebrobasilar pathology and upper cervical instability in patients with neck pain. We hypothesized that any form of screening would be related to the presence of risk factors for these disorders (i.e. hypertension and whiplash) and administration of manual therapy. We also hypothesized that the frequency of any form of screening would be less than 50% in this population. The purpose of this study is to examine documentation utilization of various screening techniques by physical therapists when treating neck pain.
Methods
Study design
The current study was a retrospective chart review of patients who presented to outpatient physical therapists with neck pain between January 2015 and January 2021. The Institutional Review Board from the author’s institution approved the current retrospective chart review (IRB#20220545).
Setting and data source
De-identified data were retrieved from multiple outpatient physical therapy clinics within a single health care organization. Chart retrieval involved identifying patients who had (1) an International Classification of Diseases, 10th edition diagnosis code for cervicalgia (i.e. M54.2) appearing in the diagnosis or problem list, and (2) a physical therapy evaluation procedure code (i.e. 97161, 97162, or 97,163). Chart retrieval was done by the author’s institution’s Clinical Research Center in June 2022. Charts were retrieved at random and given to the authors who applied the inclusion and exclusion criteria. Patient data was stored on a secure browser using separate linking and data collection sheets. Patient charts from the entire course of physical therapy were hand-searched, from initial evaluation to final visit, to determine presence of vertebrobasilar and upper cervical instability screening questions and tests. All material in the patient charts relating to these items was recorded. As data extraction was performed by multiple authors, any possible disagreement was resolved by mutual discussion, then arbitrated by first author as needed.
Participants
Inclusion criteria were the diagnosis of neck pain and presenting to outpatient physical therapists for neck pain. Physical therapy included an initial evaluation and any potential subsequent treatment sessions. Exclusion criteria was history of cervical spine surgery and age less than 18 years.
Variables
Vertebrobasilar pathology tests were recorded as present when any tests describing a combination of sustained cervical extension and rotation, or any other test described for the vertebrobasilar system, were listed in the patient chart, regardless of if the findings were normal or abnormal. Synonyms and eponyms for vertebrobasilar pathology tests included: the cervical extension-rotation test, Wallenberg’s test, DeKleyn’s test, and Hautant’s test [4,10]. Acronyms or other terminology describing the vertebral artery test or vertebrobasilar insufficiency test (VA, VBI or VBAI test) were also considered as part of this variable. Testing with sonography or other forms of advanced imaging (i.e. angiography) were not considered vertebrobasilar pathology screening tests as part of this study as they are not routinely performed by physical therapists during examinations.
Manual tests for ligamentous instability of the upper cervical spine were also recorded, including the alar ligament test, transverse ligament (stress) test, and Sharp-Purser test, based on those commonly described in the literature [5]. No other manual tests for ligamentous instability were recorded during examination of the patient charts. These tests are different, but each involves a combination of carefully guided patient movement and simultaneous palpation of the neck [11]. Each test may variably alter patients’ symptoms, cause a click or clunk, or the practitioner may perceive increased motion [11]. Tests were recorded regardless of if the findings were normal or abnormal.
The presence of any screening questions about headache, dizziness (including vertigo, disequilibrium, lightheadedness), diplopia (i.e. double vision), blurry vision, were recorded, as these are common symptoms of vertebrobasilar pathology [1]. An additional category of ‘other signs of vascular pathology’ included any further screening questions that didn’t fit the specific items listed above. These included screening questions about unsteadiness/ataxia, dysphagia, nausea/vomiting, facial palsy, ptosis, loss of consciousness, drowsiness, and confusion [1]. Screening questions were recorded regardless of whether or not findings were present.
Other data items included patient demographics (age and sex). The patient age was recorded as the age at the initial evaluation for neck pain. The presence of risk factors noted in the patient history including hypertension and whiplash (i.e. cervical sprain/strain injury).
The use of cervical spinal manual therapy was also recorded as a variable. This included any manual traction, joint mobilization, thrust manipulation, or soft tissue therapy applied to the cervical spinal joints and/or musculature during treatment.
Study size
Prior to initiating the study, we conducted feasibility testing to ensure that there were enough patients that met inclusion criteria by testing the search query in the hospital system records (i.e. diagnosis and procedure codes and date range). An initial batch of 150 charts was retrieved to ensure that the query was sufficient before proceeding to the larger chart retrieval needed for study completion. A study size endpoint of 260 patients was reached by practicality after six months of screening a total of 1500 charts.
Statistical methods
Statistical analysis was performed using IBM SPSS Statistics for Windows, version 28.0 (IBM Corp., Armonk, NY, USA). Frequency statistics were used to describe the presence or absence of screening items. Chi square tests were used to compare the relationship between screening items, risk factors, and use of manual therapy with statistical significance set at p = .05.
Results
The current study included 260 patients (Figure 1) with a mean age (standard deviation, [SD]) of 59.6 (16.2) years with 70.8% (n = 184) patients being female and 29.2% (n = 76) patients being male. Ninety-four patients (36.2%) had a history of hypertension, and 26 (10%) had neck pain due to whiplash. Two hundred and twenty-eight patients (87.7%) received manual therapy.
Figure 1.
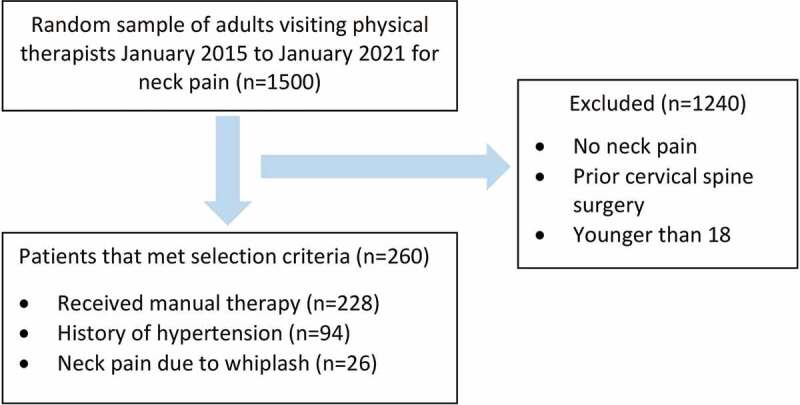
Flow diagram of patients (n=260) who met inclusion criteria from initial group of patients eligible for the study (n=1500). In the bottom box, the itemized list equals greater than 260 as certain patients fit more than one criterion.
In the documentation for the entire cohort of patients (n = 260), physical therapists screened for headache in 31.5% (n = 82), dizziness in 16.9% (n = 44), double vision in 13.5% (n = 35), blurry vision in 13.1% (n = 34), and for any other symptoms of vascular pathology in 15.4% of patients (n = 40). Physical therapists conducted vertebrobasilar testing in 6.5% of patients (n = 17), alar ligament testing in 5.8% (n = 15), transverse ligament testing in 6.5% (n = 17), Sharp-Purser testing in 34% (n = 34) (Figure 2).
Figure 2.
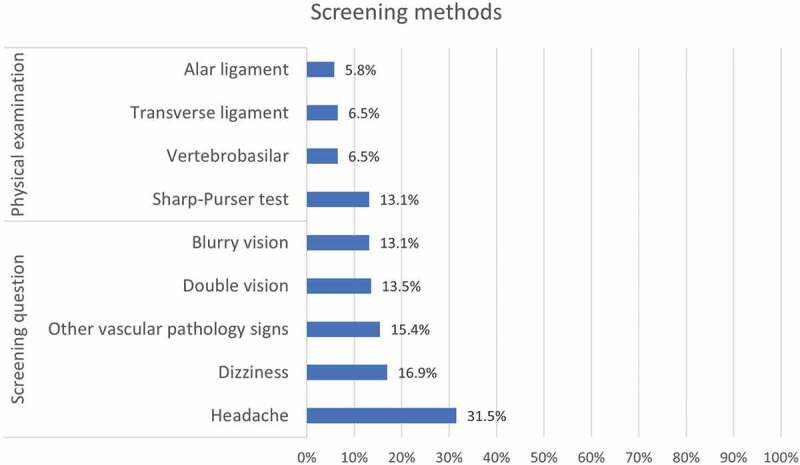
Frequency of screening methods for the entire cohort (n=260).
For patients with hypertension (n = 94), physical therapists screened for dizziness in 19.1% of patients (n = 18), double vision in 14.9% (n = 14), blurry vision in 13.8% (n = 13), headache in 24.5% (n = 23), and any other symptoms of cervical vascular pathology in 14.9% (n = 14). Physical therapists conducted vertebrobasilar testing in 7.4% of patients (n = 7), alar ligament testing in 4.3% (n = 4), transverse ligament testing in 6.4% (n = 6), and Sharp-Pursing testing in 12.8 (n = 12).
For patients with neck pain due to whiplash (n = 26), physical therapists screened for dizziness in 11.5% of patients (n = 3), double vision in 3.8% of patients (n = 1), blurry vision in 3.8% (n = 1), headache in 34.6% (n = 9), any other signs of cervical vascular pathology in 11.5% (n = 3). Physical therapists conducted vertebrobasilar testing in 3.8% of patients (n = 1), alar ligament testing in 11.5% (n = 3), transverse ligament testing in 7.7% (n = 2), and Sharp-Pursing testing in 19.2% (n = 5).
For patients who received manual therapy during treatment for neck pain (n = 228), physical therapists screened for headache in 31.6% of patients (n = 72), dizziness in 15.8% (n = 36), double vision in 12.7% (n = 29), blurry vision in 12.7% (n = 29), and any other signs of cervical vascular pathology in 14.0% (n = 32). Physical therapists performed vertebrobasilar testing in 6.6% of patients (n = 15), alar ligament testing in 5.7% (n = 13), transverse ligament testing in 6.6% (n = 15), and Sharp-Pursing testing in 13.2% (n = 30).
For comparing frequencies of upper cervical pathology screening methods based on the presence of a history of hypertension, neck pain due to whiplash, or use of manual therapy during treatment, there was no significant difference in frequency of screening for any item (p > .05 for each value, Table 1). However, physical therapists’ screening for headache among individuals with neck pain and underlying hypertension approached statistical significance (p = .065).
Table 1.
Relationship between a history of whiplash, hypertension, or receipt of manual therapy and physical therapists’ use of screening tests or questions. Results are presented as p-values, based on Chi square testing for each comparison. Alpha significance set at 0.05.
| Screening test or question | Whiplash (p-value) |
Hypertension (p-value) |
Manual Techniques (p-value) |
|---|---|---|---|
| Alar ligament test | .184 | .431 | .901 |
| Blurry Vision | .141 | .786 | .648 |
| Dizziness | .440 | .471 | .193 |
| Double Vision | .130 | .611 | .349 |
| Headache | .722 | .065 | .970 |
| Other symptoms of cervical vascular pathology | .567 | .869 | .107 |
| Sharp-Purser test | .327 | .911 | .918 |
| Transverse ligament test | .802 | .939 | .944 |
| Vertebrobasilar test | .558 | .656 | .944 |
Discussion
The present retrospective chart review is the first study to highlight physical therapists’ practical use of screening questions and physical tests for vertebrobasilar pathology and upper cervical instability by assessing documentation in clinical notes. In contrast to our hypothesis, we discovered that physical therapists’ use of screening was not influenced by a patient’s history of hypertension or whiplash, or by the use of manual therapy during care. The low rate of specialized physical examination tests for vertebrobasilar pathology and upper cervical ligament instability appears concordant with recent clinical practice guidelines which no longer recommend these tests [1–3]. The low rate of screening questions, on the other hand, contradicts clinical practice guidelines, which recommend thorough screening via history taking in patients with neck pain [1–3].
In 2014, a survey of musculoskeletal physiotherapists in the United Kingdom (n = 111) found a higher rate of screening questions for vertebrobasilar pathology than our current chart review [8]. In this prior study, most respondents (80%) reported always screening patients with neck pain by asking about dizziness, diplopia, drop attacks, dysphagia, and dysarthria, while 60% reported always asking patients about numbness, nystagmus, and nausea [8]. Additionally, 47% reported performing vertebrobasilar pathology tests before administering cervical mobilizations [8]. However, because this is a survey study, the previously reported percentage of screening may be increased due to participants’ recall bias or the desire to provide socially acceptable responses [8]. Therefore, the findings of our current chart review could show a comparatively lower rate of screening due to a difference in study design rather than actual rate of screening.
To our knowledge, little research has explored physical therapists’ use of upper cervical ligament instability tests among patients with neck pain. A survey of Australian physical therapists (n = 578) published in 2011 found that less than half of respondents indicated performing any of the upper cervical ligament instability tests [7]. Respondents also provided open-ended answers, suggesting that limitation in test validity, concern about exacerbating symptoms during testing, and a desire to only apply the tests in specific contexts explained the low use of these tests [7]. In contrast, more than half of respondents indicated they would conduct a cervical ligament instability test for a patient presenting with acute or chronic whiplash symptoms in a 2014 survey study of US physical therapists (n = 1,484) [9].
The results of the current study should also be interpreted in the context of a changing paradigm in screening for vertebrobasilar pathology. In 2007, testing for vertebrobasilar pathological positional instability were advised by all physical therapy organizations affiliated with IFOMPT, whereas tests for upper cervical ligament instability were advised by 36% of them [12]. With more recent evidence suggesting vertebrobasilar and upper cervical ligament instability tests are unreliable and have a low accuracy and pretest probability [4,5], and guidelines discouraging the use of such tests [1–3], it is possible that the percentage of physical therapists using these tests has decreased in a corresponding manner.
In the current study, screening questions for vertebrobasilar pathology and upper cervical ligament instability were more commonly administered (i.e.>13% for each) than specialized physical examination tests (i.e.<14% for each). However, given that the most recent clinical practice guidelines encourage using screening questions [1–3], we expected a higher rate of these items. In contrast to specialized physical tests, history taking has been described as the single most important factor for detecting symptoms of vertebrobasilar pathology [13]. In the present study, part of the reason for a lower rate of screening could have been because certain questions were divided into multiple categories, such as diplopia and blurred vision, rather than a single category of visual disturbance. However, the screening rate would still be poor, below 30%, even if the latter two categories were combined.
Screening for headache approached significance (p = .065) for individuals with hypertension. Given the relatively low sample size and low percentage of included patients with headache, we cannot rule out a significant relationship between screening for headache among individuals with cardiovascular risk factors such as hypertension. Such as finding, if statistically significant, would suggest that physical therapists are more likely to screen for risk factors in populations of patients with neck pain at risk for vertebrobasilar pathology.
Readers should note that, in spite of recent guidelines, some authors contend that specialized physical testing for vertebrobasilar pathology remains valuable and should be routinely performed [14]. This lack of agreement could explain why there were still some instances in the present study in which vertebrobasilar pathology tests were performed. Additionally, research regarding risk factors for vertebrobasilar pathology is continuously being updated [2]. It’s possible that clinicians’ usage of screening will vary as the body of knowledge on the subject changes or as more reliable assessment tests become available. Furthermore, it is unknown how much the literature and/or clinical practice guidelines influence clinician behaviors and future research could focus on determining the impact of clinical practice guidelines on clinician screening behaviors.
Limitations
First, as a retrospective chart review, this study is subject to documentation bias as information in patients’ charts may have been missing or incorrect. It is possible that some patients were screened, but this information was omitted from the chart. Several variables were not recorded that could affect the likelihood of conducting cervical screening, such as the presence or absence of rheumatoid arthritis or Ehler-Danlos syndrome. No sample size calculation was performed prior to initiation of the study. The current study did not examine use of general physical or neurological examination tests such as those for cranial nerves, reflexes, or Romberg balance testing. However, these tests are more broadly applied rather than specific to or to vertebrobasilar pathology or upper cervical instability [1,2]. We also did not examine if patients had undergone previous magnetic resonance imaging and/or angiography which could affect the likelihood a provider would conduct further specialized screening tests [11]. It is possible that the impact of direct access could change the frequency of cervical screening for physical therapists and this study is unable to sufficiently comment on this factor. We also did not record the number of unique physical therapists, or account for providers’ characteristics such as years in practice or additional certifications beyond a physical therapy degree which could have influenced the likelihood of screening. The frequency of screening questions and tests was lower than hypothesized, hindering the ability to detect statistical significance via Chi-squared testing. In addition, it was beyond the scope of our study to calculate the true and false positive or negative rate for identifying vertebrobasilar pathology or upper cervical instability. Our findings stem from a single US institution and may not be broadly generalizable. Depending on the country of practice or rural versus urban setting, physical therapists may encounter a different patient population or have a different role in the health care system. Furthermore, the follow-up on this study was not sufficient to determine if any deleterious effects occurred because lack of screening. Therefore, it is not known how the presence of absence of cervical vascular or ligamentous screening impacted patient outcomes.
Follow-up studies on this topic should include a larger sample size and should be conducted in a different region or health care setting. A broader sample of physical therapists could be examined using a survey, which could incorporate open-ended questions about why certain screening methods are used or avoided (e.g. reflective of evidence, limited time with patients, lack of training, etc.) which was beyond the scope of the current study to explore.
Conclusion
The present study found that US physical therapists in a single institution did not routinely administer screening questions or physical examination tests to detect vertebrobasilar pathology or upper cervical ligament instability as documented in their clinical notes. This finding was consistent regardless of the presence of risk factors (i.e. hypertension, whiplash) or physical therapists’ use of manual therapy. In order to compare these results to other groups and understand the causes of the absence of screening, more research is required.
Acknowledgements
The authors wish to thank our institution’s Clinical Research Center staff for their assistance in retrieving data for the present study.
Biographies
Anthony Baumann is a physical therapist for University Hospitals and a medical student at Northeast Ohio Medical University purusing orthopedic surgery.
Robert J. Trager is a chiropractor and researcher for University Hospitals.
Deven Curtis is a medical student at Northeast Ohio Medical University.
Mingda Chen is a medical student at Case Western Reserve University.
Keith Baldwin is an orthopedic surgery and physical therapist at Children’s Hospital of Philadelphia.
Funding Statement
The authors reported there is no funding associated with the work featured in this article.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
The data used in the present study are not publicly available as they may contain information that could compromise research participants’ privacy.
References
- [1].Blanpied PR, Gross AR, Elliott JM, et al. Neck pain: revision 2017: clinical practice guidelines linked to the international classification of functioning, disability and health from the orthopaedic section of the American physical therapy association. Journal of Orthopaedic & Sports Physical Therapy. 2017;47(7):A1–83. DOI: 10.2519/jospt.2017.0302 [DOI] [PubMed] [Google Scholar]
- [2].Rushton A, Carlesso LC, Flynn T, et al. Position statement: international framework for examination of the cervical region for potential of vascular pathologies of the neck prior to musculoskeletal intervention: international IFOMPT cervical Framework. Journal of Orthopaedic & Sports Physical Therapy. 2022;53(1):1–62. [DOI] [PubMed] [Google Scholar]
- [3].Rushton A, Rivett D, Carlesso L, et al. International framework for examination of the cervical region for potential of cervical arterial dysfunction prior to orthopaedic manual therapy intervention. Manual Ther. 2014;19(3):222–228. [DOI] [PubMed] [Google Scholar]
- [4].Hutting N, Kranenburg H, Kerry R.. Others: yes, we should abandon pre-treatment positional testing of the cervical spine. Musculoskeletal Sci Pract. 2020;49:102181. [DOI] [PubMed] [Google Scholar]
- [5].Hutting N, Scholten-Peeters GGM, Vijverman V, et al. Diagnostic accuracy of upper cervical spine instability tests: a systematic review. Phys Ther. 2013;93(12):1686–1695. [DOI] [PubMed] [Google Scholar]
- [6].Hutting N, Kerry R, Coppieters MW, et al. Considerations to improve the safety of cervical spine manual therapy. Musculoskelet Sci Pract. 2018;33:41–45. [DOI] [PubMed] [Google Scholar]
- [7].Osmotherly PG, Rivett DA. Knowledge and use of craniovertebral instability testing by Australian physiotherapists. Man Ther. 2011;16(4):357–363. [DOI] [PubMed] [Google Scholar]
- [8].Kennedy I, Caldwell K. A cross-sectional postal survey of musculoskeletal physiotherapists’ current practice of cervical pain assessment in relation to vertebrobasilar artery insufficiency, attitudes toward guidelines, and manual therapy practice. Int Musculoskelet Med. 2014;36(4):137–149. [Google Scholar]
- [9].Corkery MB, Edgar KL, Smith CE. A survey of physical therapists’ clinical practice patterns and adherence to clinical guidelines in the management of patients with whiplash associated disorders (WAD). J Man Manip Ther. 2014;22(2):75–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Myers BJ, Davey D, Cook CE. Factors associated with cervical arterial dysfunction: a survey of physical therapist educators in the United States. J Man Manip Ther. 2021;29(1):33–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Kaale BR, Krakenes J, Albrektsen G, et al. Clinical assessment techniques for detecting ligament and membrane injuries in the upper cervical spine region—a comparison with MRI results. Man Ther. 2008;13(5):397–403. [DOI] [PubMed] [Google Scholar]
- [12].Carlesso L, Rivett D. Manipulative practice in the cervical spine: a survey of IFOMPT member countries. J Man Manip Ther. 2011;19(2):66–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Chaibi A, Russell MB. A risk–benefit assessment strategy to exclude cervical artery dissection in spinal manual-therapy: a comprehensive review. Ann Med. 2019;51(2):118–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Thomas L, Treleaven J. Should we abandon positional testing for vertebrobasilar insufficiency? Musculoskelet Sci Pract. 2020;46:102095. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data used in the present study are not publicly available as they may contain information that could compromise research participants’ privacy.


