Abstract
The dietary supplements industry disproportionately markets potentially harmful products promising weight loss, cleansing/detoxing, and boosted energy and immunity to women. The COVID-19 pandemic heightened consumer concerns around health and body weight, which may have increased women’s risks of using supplements, particularly if they had a higher weight and experienced weight discrimination. This study aimed to estimate inequities in prevalence and change in use of weight-loss, cleanse/detox, immunity, and energy supplements in the first year of the pandemic and to assess the extent to which the relationship between weight and supplement use differs across discrimination experiences. We drew upon longitudinal data from cisgender women in the U.S. COVID-19 Pandemic Substudy of the Nurses’ Health Study II and 3 and Growing Up Today Study cohorts, collected over 5 waves from April/May 2020 to April 2021 (N=51,814). Modified Poisson generalized estimating equation models, adjusted for age, cohort, race/ethnicity, wave, and Census region, estimated the relative excess risk due to interaction (RERI) between weight status and weight discrimination on prevalence of supplement use. Weight status categories were derived from body mass index (BMI), and weight discrimination was assessed using the attributions item of the Everyday Discrimination Scale. Baseline prevalence of supplement use was 2.7% for weight-loss, 3.3% for cleanse/detox, 4.2% for energy, and 22.6% for immune. Respondents with BMIs of 25–29.9 kg/m2 and 30–34.9 kg/m2 who experienced weight discrimination had RERI values of 0.89 (95% CI 0.14, 1.65) and 1.00 (95% CI 0.25, 1.75) for weight-loss and 0.57 (95% CI 0.13, 1.02) and 0.60 (95% CI 0.19, 1.01) for immune supplements, respectively, indicating this group had excess risk of use compared to lower BMI respondents who experienced no weight discrimination. The findings demonstrate the disproportionate impact of weight discrimination on use of potentially harmful supplements among cisgender women with higher weights during the pandemic.
Keywords: Dietary Supplements, Weight-Based Discrimination, COVID-19, Women’s Health
1. Introduction
The dietary supplements market in the U.S. is vast and quickly growing, estimated to be worth $66 billion USD by 2024 (Grebow, 2021). Dietary supplements with claims related to weight loss, boosting immunity, boosting energy, or cleansing or “detoxing” make up a notable share of the market. Since the passage of the Dietary Supplement Health and Education Act (DSHEA) of 1994, which classified supplements in a way that would not require screening or proof of efficacy prior to sale, the manufacturers of dietary supplements have faced few federal regulations (Cassileth et al., 2009; Pomeranz et al., 2015; Sissung et al., 2021). Given minimal federal oversight, the producers of supplements purporting weight loss, boosted immunity or energy, or cleansing/detoxing benefits often make deceptive claims (Cassileth et al., 2009; Wharton et al., 2020), and such products have been found to include prohibited pharmaceuticals, anabolic steroids, and toxic chemicals (Marcus, 2016; Mathews, 2018; Tucker et al., 2018; Yen & Ewald, 2012). The use of these types of dietary supplements has also been linked to serious health consequences, including adverse cardiovascular events, liver disease, and death (Geller et al., 2015; Or et al., 2019; Vanderperren et al., 2005; Yen & Ewald, 2012).
There are also known disparities in the use of dietary supplements, as several studies have found that the use of some dietary supplements (i.e., weight-loss, cleanse/detox supplements) is disproportionately higher among girls and women, individuals in low-income households, individuals with higher weights, and minoritized racial/ethnic populations (Austin et al., 2017; Pillitteri et al., 2008; Vitagliano et al., 2022). Importantly, disparities in the use of potentially harmful supplements are likely driven by structural factors, including the systemic targeting of traditionally marginalized communities. For example, manufacturers of weight-loss and cleanse/detox supplements have faced federal charges in the U.S. for explicit and deceptive targeting of Latine communities (Wilkes, 2019), demonstrating practices of systemic targeting of marginalized communities by industry. Further, the labelling and marketing of products includes claims that are unfounded and may mislead consumers with lower levels of health or nutrition literacy (Hua et al., 2021; Wang et al., 2023) as well as those with higher weights who may have a desire to modify their body weight and/or shape (Pillitteri et al., 2008; Wharton et al., 2020). Since body ideals in the U.S. are highly gendered and women face disproportionate pressures to ascribe to a thinner body ideal (Murnen & Smolak, 2015), it is unsurprising that the research literature consistently demonstrates that women consume dietary supplements, and especially weight-loss supplements, more often than men (Blanck et al., 2007; Pillitteri et al., 2008; Wang et al., 2023). Energy supplements, which often contain stimulants, may even be used to aide in weight loss and metabolism boosting attempts among women trying to lose weight (Blanck et al., 2007; Jeffers et al., 2013).
The novel coronavirus disease (COVID-19) pandemic has led to an increase in consumer concerns surrounding weight gain and disease spread (Adams et al., 2020; Hamulka et al., 2020), both of which are suspected to have contributed to an increase in the U.S. dietary supplements market. In 2020, industry publications reported drastic single-year increases in sales; in April 2020, during the earliest wave of the pandemic, the industry reported a 44% increase in sales compared to the same period in 2019 (Lordan, 2021). This is of concern given the potential harms of under-regulated dietary supplements, especially among individuals who may have heightened pandemic-related fears about their health and safety. One recent study found that, among adults living in the U.S. during the first year of the pandemic, experiencing financial precarity, food insecurity, and/or psychological distress was associated with an increased risk of using weight-loss, cleanse/detox, energy, and immune supplements (Austin et al., 2023), which may be linked to stress and coping pathways and/or barriers to health care access. Given the widespread media attention on pandemic-related weight gain and demonstrated increases in potentially harmful supplement use among vulnerable populations, it is possible that weight stigma and discrimination could also be exacerbating supplement use.
1.1. Weight stigma, discrimination, and dietary supplements use.
Weight stigma encompasses “the social rejection and devaluation that accrues to those who do not comply with prevailing social norms of adequate body weight and shape” (Tomiyama et al., 2018). Although weight stigma can be targeted to people of a range of body sizes, it is most often directed towards people with higher weights. Weight discrimination, driven by pervasive weight stigma, captures experiences of discrimination attributable to one’s weight. Experiencing weight discrimination is associated with a wide range of negative mental and physical health consequences, including increased allostatic load, metabolic dysregulation, engagement in unhealthy dietary and physical activity behaviors, poor mental health outcomes, and mortality (Sutin et al., 2016; Sutin et al., 2015; Vadiveloo & Mattei, 2017; Zhu et al., 2022). Weight discrimination is a social-structural determinant of health and health inequities, as it also affects access to resources and opportunities through biased subjective grading in schools (MacCann & Roberts, 2013), lower college admissions (Burmeister et al., 2013), and poorer employment-related outcomes such as fewer promotions and lower wages and salaries (Puhl et al., 2008; Vanhove & Gordon, 2014). Experiences of weight discrimination differ at various intersections of identity, including gender, race, ethnicity, and socioeconomic status (Ciciurkaite & Perry, 2017; Himmelstein et al., 2017), and much of the research has identified the ways in which women face greater weight discrimination than men (Puhl et al., 2008).
Weight stigma and discrimination are highly gendered, as girls and women face substantial pressures to attain and maintain a thin body ideal (Calogero et al., 2016). Hegemonic gender roles and norms, rooted in patriarchal ideologies, reinforce the notion that femininity is aligned with having a thin body and/or the act of pursuing a thin body (Piran, 2010; Siegel & Calogero, 2019); as such, cisgender girls and women face particular and immense pressures from social and mass media and broader cultural norms to attain and maintain a low body weight. Building on Goffman’s seminal work on stigma (Goffman, 1963), scholars have further delineated the ways in which weight stigma is tied into and motivated by neoliberal, capitalist norms that promote individual responsibility and consumerism as avenues to and lose weight and “pass” as a smaller-bodied person (Monaghan, 2016), thereby reducing the likelihood of experiencing further weight stigma and discrimination. As such, hegemonic gender norms may lead cisgender women who experience weight discrimination to engage in consumerist actions, such as purchasing supplements that deceptively promote passing through promised weight loss. The social consequences of having a higher weight (e.g., reduced wages) are substantially gendered (Fikkan & Rothblum, 2012), which likely also contributes to increased risk of weight-loss oriented behaviors among women.
The association between experiencing weight discrimination and eating disorder pathology, including unhealthy weight-related behaviors such as the use of diet pills, is well-documented (Himmelstein et al., 2018; Mason et al., 2021). Prior to the onset of the COVID-19 pandemic, individuals with higher weights had an increased risk of weight-loss supplement use (Blanck et al., 2007), and perceived weight discrimination was a motivator for higher-weight individuals to avoid medical care and perhaps seek out alternative forms of perceived health-promoting behaviors, such as the use of dietary supplements. Thus, there is a possibility that the COVID-19 pandemic may have exacerbated pre-existing experiences of weight-related discrimination among higher-weight adults, placing them at an elevated risk of potentially harmful supplement use.
The Health Stigma and Discrimination Framework (Stangl et al., 2019) builds upon the work of Goffman (1963) and authors to conceptualize “the broader social, cultural, political and economic forces that structure stigma,” rather than stigma as a byproduct of actions from one person or group to another. The Framework may be used to conceptualize how the intersecting effects of structural systems of power/oppression (e.g., racism, sexism, classism) are compounded by health-specific stigmas, such as weight discrimination, and how this may lead to a disproportionate risk of using potentially harmful supplements among cisgender women with higher weights during the pandemic specifically. The Framework details how the process of stigmatization unfolds and manifests in discriminatory outcomes for individuals that translate into health impacts. For example, drivers such as fear of COVID-19 infection and self-blame for weight gain during the pandemic may interact with facilitating cultural factors (e.g., social norms and beliefs around higher weights) to result in stigma marking (i.e., the process through which stigma is applied to certain people or groups), whereby health-related weight stigma intersects with other stigmas, such as sexism. This may manifest in experiences of weight discrimination, which can lead to inequities in health outcomes, such as an increased risk of potentially harmful supplement use. As such, the compounding pressures of weight discrimination and sexism may have exacerbated supplement use risk during the unique context of the pandemic.
1.2. Weight stigma and discrimination during the COVID-19 pandemic
With increasing concerns about the transmission and health consequences of COVID-19, there has also been an influx of scientific studies linking higher weights with an increased risk of COVID-19 mortality (de Macêdo et al., 2022; Puhl et al., 2020). Research on the increased risk of COVID-19 mortality among higher-weight individuals has informed mainstream messaging from prominent public health organizations globally, including the U.S. Centers for Disease Control and Prevention and the World Health Organization, which have identified a high body mass index (BMI) as a “risk factor” for COVID-19 severity and mortality (Kompaniyets et al., 2021; World Health Organization, 2020). However, evidence suggests that weight stigma and discrimination may hinder higher-weight individuals from seeking medical care and lead to worse health outcomes (Alberga et al., 2019). Indeed, weight stigma and discrimination have been well-documented in medical settings and may partially explain increased risks of certain medical conditions, such as gynecological cancers (Aldrich & Hackley, 2010), among higher-weight individuals. The public health “war on obesity” has also resulted in the promotion of weight-stigmatizing messaging that may further exacerbate experiences of weight discrimination in the general population (Hunger et al., 2020).
Emerging research suggests that widespread shelter-in-place orders, pandemic-related policies, and the disruption of normal daily routines during the first year of the pandemic exacerbated fear of gaining weight, contributing to disordered weight control behaviors and symptoms of eating disorders (Meyer et al., 2020; Puhl et al., 2020; Rodgers et al., 2020; Termorshuizen et al., 2020). This effect may be intensified among individuals with higher weights, as pre-pandemic experiences of weight discrimination have been shown to result in greater risks of depression, stress, eating as a coping strategy, and binge eating during the pandemic (Puhl et al., 2020). Negative and pervasive media depictions of weight gain during the pandemic (Prohaska, 2023) may have aggravated stigma marking (Stangl et al., 2019) and subsequent experiences of weight discrimination and health-related concerns, particularly among people with higher weights, and driven them to seek additional pathways to regulate their weight (via weight-loss or cleanse/detox supplements) or improve their overall health (via energy and immune-boosting supplements).
1.3. Purpose of the current study
Despite the evidence of harmful ingredients in dietary supplements, increasing sales of supplements since the onset of the pandemic, and the potential vulnerability of higher-weight individuals, to our knowledge, no studies have investigated usage of supplements during the COVID-19 pandemic and elevated risks among people experiencing weight discrimination. The aims of this study were: (1) to estimate weight status-related inequities in prevalence of use and change in use of potentially harmful supplements (i.e., weight-loss, cleanse/detox, immunity, and energy supplements) over time in the first year of the COVID-19 pandemic among cisgender women and (2) to evaluate the extent to which the relationship between body size (i.e., weight status) and dietary supplement use differs across weight-related discrimination experiences.
2. Methods
2.1. Sample Composition
Data were drawn from the COVID-19 Substudy (Rich-Edwards et al., 2021), launched in April/May 2020 within the U.S.-based prospective Nurses’ Health Study II (NHSII), Nurses’ Health Study 3 (NHS3), and Growing Up Today Study (GUTS) cohorts. Eligible participants (n=109,662) from the three cohorts (i.e., those currently enrolled with an email on record) were invited to complete the COVID-19 baseline survey and received reminders after 3 and 10 days. Participants (n=58,612) living in the U.S. completed the baseline survey. Participants were included in the present analyses if they provided data on use of dietary supplements on some or all the five waves of data collection from April/May 2020 to April 2021 in which dietary supplement use was assessed. Eligible participants were excluded if they were missing all information on supplement use at every wave (n=422) or were living outside of the U.S. (n=820) and/or missing any information on weight/height, gender identity, race/ethnicity, age, geographic region, mental health status, unemployment status, healthcare worker status, and COVID-19 infections (n=6,434). We focused our analysis on cisgender women (n=51,814), as this was the only gender group with sufficient sample size to obtain precise group-specific estimates in the cohort. The overall study was approved by the Brigham and Women’s Hospital Institutional Review Board (IRB) and the current analyses by the Boston Children’s Hospital IRB.
2.2. Measures
The primary predictor of interest was weight-related discrimination (binary variable: yes/no; see Supplementary Material). The six-item Everyday Discrimination Scale (Williams et al., 1997) queries participants about different experiences of lifetime discrimination (e.g., treated with less courtesy and respect than other people, threatened or harassed). To assess weight-related discrimination specifically, those who reported any level of discrimination were asked to indicate attributions for their experiences (e.g., race, gender, etc.); those who selected “weight” were designated as experiencing lifetime weight-related discrimination and those who did not select “weight” or reported no discrimination in the measure were coded as not experiencing weight discrimination. The Everyday Discrimination Scale was administered at wave 4 of the COVID-19 Substudy, which occurred an average 2.9 months after wave 1/baseline; however, given that the items ask about lifetime experiences with discrimination, we treated this measure as time invariant over the course of the study period and analyzed responses in relation to all five waves of the outcomes.
Weight status was evaluated using BMI (kg/m2). BMI was calculated from self-reported adult height and most recently self-reported weight in pounds prior to the pandemic (which occurred in 2019 for most participants). BMI was included as either a continuous or a categorical variable (hereafter referred to as “weight status” and categorized in six groupings (<25 kg/m2; 25–29.9 kg/m2; 30–34.9 kg/m2; 35–39.9 kg/m2; 40–44.9 kg/m2; >45 kg/m2). Although BMI does not capture the full complexity of experiencing life in a larger body, nor weight perception (Carter et al., 2022), we used it as a proxy to assess the varying degrees of weight discrimination experienced by individuals of different body sizes. We recognize critiques of how the use of BMI as an indicator or correlate of health status may reinforce weight stigma (Hunger et al., 2020) and use it as a measure solely to classify participants’ body sizes in the context of experiencing weight discrimination.
The outcomes of interest, self-reported use of dietary supplements, were assessed at all five waves (see Supplementary Material). We considered two outcome operationalizations. Prevalent use included any reported use at a given wave of cleanse/detox, weight-loss, energy boosting, and/or immune boosting supplements, regardless of whether the use was initiated pre- or post-pandemic onset. New onset use was defined as the first reported instance of use among those who did not report using supplements pre-pandemic; here, participants were censored after their first report of use.
Finally, potential confounders of the relationship between weight discrimination and supplement use were included in the analyses, including race/ethnicity (categorical: non-Hispanic Asian, non-Hispanic Black/African American, Hispanic/Latina, non-Hispanic White, other/unlisted), age (continuous), cohort (categorical: NHSII, NHS3, GUTS), survey wave (categorical), and Census region (categorical: Midwest, Northeast, South, West).
2.3. Statistical Analyses
We modelled the relative risks (RR) and 95% confidence intervals (CI) of the associations between each operationalization of BMI (i.e., continuous and categorical) and prevalent and new onset use for each type of dietary supplement. RR estimates were derived from modified Poisson generalized estimating equation (GEE) models that adjusted for age, cohort, race/ethnicity, study wave, and geographic region. We fit modified Poisson rather than logistic GEE models to estimate RRs because some of our outcomes were common (i.e., prevalence >5%) (Zou & Donner, 2013). Finally, we evaluated whether experiencing weight discrimination moderated associations between weight status and prevalent and new supplement use for each supplement type by including weight status-by-weight discrimination interaction terms and calculating the relative excess risk due to interaction (RERI). RERI is a type of additive-scale moderation that is recommended for identifying factors that contribute to health inequities (Ward et al., 2019) and quantifies the extent to which the risk of an outcome among a doubly exposed group differs from what would be expected, where the expected risk is given by the sum of the effects associated with each of the two exposures. In this study, the doubly exposed group is individuals with higher weights who also experience weight discrimination.
Participants who skipped one or multiple waves were treated as missing for that wave but not excluded from all analyses. We used inverse probability weighting (IPW) to address potential selection biases due to loss-to-follow-up and/or item non-response. Given the prevalence of attrition across the study period (May 2020 19.3%, June 2020 23.8%, July 2020 25.4%, October 2020 27.8%, January 2021 25.0%, April 2021 17.2%), we used IPW to re-weight the data such that they reflected the cohort composition at baseline with respect to demographics and other key factors. Our approach followed the methods outlined by Fewell et al. (2004) for implementing IPW in the context of repeated-measures data. Briefly, we built a set of weights that predicted censoring due to loss-to-follow-up or item non-response at each study wave (for prevalent use models) or the cumulative probability of remaining uncensored over time (for new onset use models), conditional on age, race/ethnicity, region of residence, healthcare worker status, COVID-19 infection and related symptomology, unemployment, and mental health status. We then incorporated these weights into our longitudinal models, such that we fit weighted GEE models that produced estimates interpretable as the associations that would have been observed had there been no loss-to-follow-up or item non-response across the study period, assuming no omitted-variable bias in our models predicting censoring.
3. Results
The characteristics of the analytic sample of cisgender women are presented in Table 1. The sample varied in age (M=57.8 years, SD=12.9) and was mostly non-Hispanic White (93.5%). At baseline, prevalent use (i.e., any reported use regardless of whether use was initiated pre- or post-pandemic onset) for each type of supplement was 2.7% for weight-loss, 3.3% for cleanse/detox, 4.2% for energy, and 22.6% for immune supplements. New onset use of supplements at baseline (i.e., current use among those with no pre-pandemic use) was 0.5–0.6% for each of weight-loss, cleanse/detox, and energy supplements and 6.5% for immune supplements. Nearly one-tenth of participants reported experiencing weight discrimination (7.8%). Experiencing weight discrimination was positively associated with continuous BMI (data not shown, RR=1.11, 95% CI 1.11, 1.12, p <0.05), where each additional BMI unit was associated with 11% higher risk of experiencing weight discrimination. Table 2 presents the proportion of participants reporting prevalent and new onset dietary supplement use by weight status at baseline.
Table 1.
Sociodemographic characteristics, prevalence of weight discrimination, and prevalence of weight-loss, cleanse/detox, energy, and immune supplement use among cisgender women in the COVID-19 Pandemic Sub-Study at baseline (April/May 2020) (N=51,814)
| Characteristic | Analytic Sample |
|---|---|
| Age in years, M (SD) | 57.8 (12.9) |
| Cohort, n (%) | |
| Nurses’ Health Study 2 | 37,058 (71.5) |
| Nurses’ Health Study 3 | 11,188 (21.6) |
| Growing Up Today Study | 3,568 (6.9) |
| Race/ethnicity, n (%) | |
| Non-Hispanic Asian | 642 (1.2) |
| Non-Hispanic Black | 565 (1.1) |
| Hispanic/Latine | 979 (1.9) |
| Non-Hispanic White | 48,460 (93.5) |
| Other/unlisted | 1,168 (2.3) |
| Geographic region, n (%) | |
| Midwest | 15,399 (29.7) |
| Northeast | 14,027 (27.1) |
| South | 12,244 (23.6) |
| West | 10,144 (19.6) |
| Body mass index, M (SD) | 27.3 (6.3) |
| Weight status | |
| <25 kg/m2 | 22,673 (43.8) |
| 25–29.9 kg/m2 | 15,015 (29.0) |
| 30–34.9 kg/m2 | 7,951 (15.3) |
| 35–39.9 kg/m2 | 3,748 (7.2) |
| 40–44.9 kg/m2 | 1,540 (3.0) |
| ≥45 kg/m2 | 887 (1.7) |
| Weight discrimination, n (%) | |
| Yes | 4,044 (7.8) |
| No | 35,283 (68.1) |
| Missing | 12,487 (24.1) |
| Prevalent dietary supplement use, n (%) | |
| Weight-loss supplements | 1,411 (2.7) |
| Cleanse/detox supplements | 1,692 (3.3) |
| Energy supplements | 2,197 (4.2) |
| Immune supplements | 11,725 (22.6) |
| New onset dietary supplement use, n (%) | |
| Weight-loss supplements | 246 (0.5) |
| Cleanse/detox supplements | 274 (0.5) |
| Energy supplements | 306 (0.6) |
| Immune supplements | 3,389 (6.5) |
Note: M = mean, SD = standard deviation. Percentages may not sum to 100% due to rounding. Prevalent use is defined as use at baseline, regardless of whether use was initiated pre- or post-pandemic onset. New onset use is defined as first reported instance of use among those who did not report using supplements pre-pandemic.
Table 2.
Proportion of cisgender women participants reporting dietary supplement use by weight status in the COVID-19 Pandemic Sub-Study at baseline (April/May 2020) (N=51,814)
| Prevalent use | ||||
|---|---|---|---|---|
| Weight-loss | Cleanse/detox | Energy | Immune | |
| Weight status | % | % | % | % |
| <25 kg/m2 | 1.5 | 3.3 | 3.7 | 22.7 |
| 25–29.9 kg/m2 | 3.2 | 3.4 | 4.5 | 22.9 |
| 30–34.9 kg/m2 | 3.9 | 3.4 | 4.5 | 22.3 |
| 35–39.9 kg/m2 | 4.2 | 2.7 | 5.1 | 21.9 |
| 40–44.9 kg/m2 | 5.0 | 2.4 | 5.0 | 22.5 |
| ≥45 kg/m2 | 5.5 | 2.9 | 5.7 | 22.1 |
| New onset use | ||||
| Weight-loss | Cleanse/detox | Energy | Immune | |
| Weight status | % | % | % | % |
| <25 kg/m2 | 0.3 | 0.4 | 0.5 | 7.9 |
| 25–29.9 kg/m2 | 0.6 | 0.5 | 0.7 | 7.2 |
| 30–34.9 kg/m2 | 0.6 | 0.5 | 0.6 | 6.9 |
| 35–39.9 kg/m2 | 0.6 | 0.3 | 0.5 | 6.3 |
| 40–44.9 kg/m2 | 0.2 | 0.2 | 0.3 | 7.8 |
| ≥45 kg/m2 | 0.9 | 0.1 | 1.2 | 5.2 |
Note: Percentages may not sum to 100% due to rounding. Prevalent use is defined as use at baseline, regardless of whether use was initiated pre- or post-pandemic onset. New onset use is defined as first reported instance of use among those who did not report using supplements pre-pandemic.
Table 3 displays the results of the model that estimated inequities in prevalent and new onset weight-loss, cleanse/detox, energy, and immune supplement use by BMI and weight status. There were statistically significant positive associations between continuous BMI and prevalent use of weight-loss (RR = 1.05, 95% CI 1.05, 1.06) and energy (RR = 1.02, 95% CI 1.01, 1.02) supplements. Compared to participants with weight status less than 25 kg/m2, participants with higher weight statuses were statistically significantly more likely to report prevalent use of these supplement types. Having a higher BMI pre-pandemic was statistically significantly positively associated with new onset use of weight-loss (RR = 1.04, 95% CI 1.04, 1.05) and energy (RR = 1.02, 95% CI 1.01, 1.03) supplements (Table 3). Compared to participants with a BMI < 25 kg/m2, participants with a BMI between 30–34.9 kg/m2 and 40–44.9 kg/m2 had elevated risks of new onset use of cleanse/detox supplements during the first year of the pandemic (Table 3). In Table 4, we present the results of models estimating associations between weight discrimination and prevalent and new onset use of each of the supplement types. Weight-related discrimination was statistically significantly associated with prevalent use of weight-loss (RR = 1.72, 95% CI 1.54, 1.92), energy (RR = 1.25, 95% CI 1.13, 1.39), and immune (RR = 1.08, 95% CI 1.03, 1.13) supplements, as well as new onset use.
Table 3.
Associations between BMI, weight status, and dietary supplement use in the COVID- 19 Pandemic Sub-Study across the study period (April/May 2020–April 2021) among cisgender women (N=51,814)
| Prevalent use | ||||
|---|---|---|---|---|
| Weight-loss | Cleanse/detox | Energy | Immune | |
| RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| BMI (kg/m2) | 1.05 (1.05, 1.06) | 1.00 (0.99, 1.00) | 1.02 (1.01, 1.02) | 1.00 (1.00, 1.00) |
| Weight status (ref: <25 kg/m2) | ||||
| 25–29.9 kg/m2 | 1.97 (1.79, 2.16) | 1.00 (0.93, 1.09) | 1.29 (1.20, 1.39) | 1.04 (1.00, 1.07) |
| 30–34.9 kg/m2 | 2.57 (2.32, 2.85) | 1.01 (0.91, 1.12) | 1.28 (1.17, 1.40) | 1.01 (0.97, 1.05) |
| 35–39.9 kg/m2 | 2.75 (2.41, 3.12) | 0.85 (0.74, 0.98) | 1.43 (1.28, 1.60) | 1.03 (0.98, 1.09) |
| 40–44.9 kg/m2 | 3.23 (2.73, 3.81) | 1.02 (0.84, 1.24) | 1.52 (1.29, 1.77) | 1.07 (0.99, 1.15) |
| ≥45 kg/m2 | 3.14 (2.54, 3.88) | 1.02 (0.79, 1.31) | 1.34 (1.09, 1.66) | 1.01 (0.91, 1.12) |
| New onset use | ||||
| Weight-loss | Cleanse/detox | Energy | Immune | |
| RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| BMI (kg/m2) | 1.04 (1.04, 1.05) | 1.01 (1.00, 1.02) | 1.02 (1.01, 1.03) | 1.01 (1.00, 1.01) |
| Weight status (ref: <25 kg/m2) | ||||
| 25–29.9 kg/m2 | 1.70 (1.49, 1.94) | 1.18 (1.05, 1.33) | 1.29 (1.15, 1.44) | 1.05 (1.00, 1.11) |
| 30–34.9 kg/m2 | 2.19 (1.89, 2.53) | 1.19 (1.02, 1.38) | 1.42 (1.24, 1.63) | 1.06 (0.99, 1.12) |
| 35–39.9 kg/m2 | 2.06 (1.69, 2.50) | 1.10 (0.89, 1.35) | 1.40 (1.16, 1.68) | 1.08 (0.99, 1.17) |
| 40–44.9 kg/m2 | 2.63 (2.05, 3.37) | 1.45 (1.11, 1.90) | 1.35 (1.03, 1.77) | 1.16 (1.03, 1.31) |
| ≥45 kg/m2 | 2.83 (2.08, 3.84) | 1.23 (0.84, 1.80) | 1.73 (1.27, 2.35) | 1.03 (0.87, 1.20) |
Note: RR = risk ratio, CI = confidence interval, BMI = body mass index. Estimates are derived from modified Poisson GEE models adjusted for age, cohort, race/ethnicity, and geographic region of residence and are weighted to account for loss-to-follow-up. Separate models were conducted with BMI as a continuous variable and weight status groups.
Table 4.
Associations between weight-related discrimination and dietary supplement use in the COVID-19 Pandemic Sub-Study across the study period (April/May 2020–April 2021) among cisgender women (N=51,814)
| Prevalent use | ||||
|---|---|---|---|---|
| Weight-loss | Cleanse/detox | Energy | Immune | |
| RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Weight-related discrimination | 1.72 (1.54, 1.92) | 1.08 (0.96, 1.22) | 1.25 (1.13, 1.39) | 1.08 (1.03, 1.13) |
| New onset use | ||||
| Weight-loss | Cleanse/detox | Energy | Immune | |
| RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Weight-related discrimination | 1.59 (1.36, 1.85) | 1.07 (0.90, 1.27) | 1.25 (1.08, 1.45) | 1.14 (1.06, 1.22) |
Note: RR = risk ratio, CI = confidence interval. Estimates are derived from modified Poisson GEE models adjusted for age, cohort, race/ethnicity, and geographic region of residence and are weighted to account for loss-to-follow-up.
Results of the models estimating the associations between weight status and prevalent use of dietary supplements, by supplement type, with moderation by weight discrimination are presented in Table 5. The RERI quantifying whether experiencing weight discrimination moderated associations between weight status and prevalent weight-loss and energy supplement was statistically significantly elevated for participants in the 25–29.9 kg/m2 and 30–34.9 kg/m2 weight status ranges (Table 5), indicating that participants in these ranges had excess risk of using weight-loss and energy supplements compared to participants with lower weight status who experienced no weight discrimination. Additional sensitivity analyses were conducted in which all participants with a BMI ≥35 were combined into a single group; the RERI quantifying the moderating effect of weight discrimination on prevalence weight-loss and energy supplement use was not significant (data not shown). Weight discrimination did not significantly moderate the association between weight status and new onset supplement use for any type of supplement (data not shown). To further illustrate the relationship between supplement use and weight discrimination, in Figure 1, we provide an example diagram of the association between new onset weight-loss supplement use and BMI with effect measure modification by weight discrimination. Participants with a BMI less than 40 kg/m2 who reported experiencing weight discrimination had a slightly elevated risk of new onset weight-loss supplement use during the first year of the pandemic, while the trend is reversed among participants with a BMI above 40 kg/m2.
Table 5.
Associations between weight status and prevalent weight-loss, cleanse/detox, energy, and immune supplement use with effect measure modification by weight-related discrimination in the COVID-19 Pandemic Sub-Study across the study period (April 2020–April 2021), among cisgender women (N=51,814)
| Dietary supplement type | ||||
|---|---|---|---|---|
| Weight-loss | Cleanse/detox | Energy | Immune | |
| RR (95% CI) | RR (95% CI) | RR (95% CI) | RR (95% CI) | |
| Cisgender women | ||||
| BMI <25 vs. 25–29.9 kg/m2 | ||||
| BMI <25, no discrimination | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| BMI <25, discrimination | 0.83 (0.47, 1.19) | 1.12 (0.79,1.45) | 0.85 (0.58,1.12) | 0.97 (0.84,1.10) |
| BMI 25–29.9, no discrimination | 1.88 (1.66, 2.09) | 0.98 (0.88,1.08) | 1.22 (1.11,1.33) | 1.03 (0.99,1.07) |
| BMI 25–29.9, discrimination | 2.60 (1.92, 3.28) | 1.38 (1.02,1.74) | 1.64 (1.28,2.00) | 1.11 (0.99,1.23) |
| RERI | 0.89 (0.14, 1.65) | 0.28 (−0.20,0.76) | 0.57 (0.13,1.02) | 0.11 (−0.07,0.28) |
| BMI <25 vs. 30–34.9 kg/m2 | ||||
| BMI <25, no discrimination | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| BMI <25, discrimination | 0.84 (0.47,1.21) | 1.11 (0.78,1.44) | 0.85 (0.58,1.12) | 0.97 (0.84,1.03) |
| BMI 30–34.9, no discrimination | 2.43 (2.11,2.75) | 1.00 (0.87,1.13) | 1.14 (1.01,1.27) | 0.98 (0.93,1.10) |
| BMI 30–34.9, discrimination | 3.28 (2.61,3.94) | 0.92 (0.70,1.15) | 1.59 (1.28,1.90) | 1.06 (0.96,1.15) |
| RERI | 1.00 (0.25,1.75) | −0.19 (−0.60,0.22) | 0.60 (0.19,1.01) | 0.11 (−0.05,0.27) |
| BMI <25 vs. 35–39.9 kg/m2 | ||||
| BMI <25, no discrimination | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| BMI <25, discrimination | 0.84 (0.47,1.21) | 1.12 (0.79,1.45) | 0.86 (0.58,1.13) | 0.97 (0.85,1.10) |
| BMI 35–39.9, no discrimination | 2.89 (2.37,3.42) | 0.82 (0.66,0.98) | 1.43 (1.21,1.66) | 0.99 (0.92,1.07) |
| BMI 35–39.9, discrimination | 2.98 (2.32,3.63) | 0.94 (0.69,1.18) | 1.39 (1.10,1.67) | 1.14 (1.03,1.24) |
| RERI | 0.24 (−0.60,1.09) | 0.00 (−0.43,0.43) | 0.10 (−0.33,0.54) | 0.17 (−0.01,0.35) |
| BMI <25 vs. 40–44.9 kg/m2 | ||||
| BMI <25, no discrimination | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| BMI <25, discrimination | 0.84 (0.47,1.21) | 1.12 (0.79,1.45) | 0.86 (0.59,1.14) | 0.98 (0.85,1.11) |
| BMI 40–44.9, no discrimination | 3.15 (2.33,3.96) | 0.98 (0.69,1.26) | 1.31 (0.96,1.66) | 0.99 (0.87,1.11) |
| BMI 40–44.9, discrimination | 3.46 (2.52,4.40) | 1.11 (0.74,1.49) | 1.59 (1.17,2.01) | 1.18 (1.03,1.33) |
| RERI | 0.47 (−0.76,1.70) | 0.01 (−0.56,0.58) | 0.42 (−0.18,1.01) | 0.21 (−0.00,0.44) |
| BMI <25 vs. >45 kg/m2 | ||||
| BMI <25, no discrimination | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) | 1.00 (referent) |
| BMI <25, discrimination | 0.84 (0.48,1.21) | 1.12 (0.79,1.45) | 1.48 (0.97,1.14) | 0.97 (0.84,1.10) |
| BMI >45, no discrimination | 3.02 (1.90,4.13) | 1.17 (0.71,1.64) | 0.86 (0.97,1.99) | 1.06 (0.87,1.25) |
| BMI >45, discrimination | 3.28 (2.20,4.35) | 1.11 (0.70,1.52) | 1.24 (0.83,1.65) | 1.07 (0.91,1.22) |
| RERI | 0.42 (−1.13,1.96) | −0.81 (−0.88,0.51) | −0.10 (−0.80,0.60) | 0.03 (−0.24,0.30) |
Note: RR = risk ratio, CI = confidence interval, BMI = body mass index, RERI = relative excess risk due to interaction. Estimates are derived from modified Poisson GEE models adjusted for age, cohort, gender identity (overall models only), race/ethnicity, and geographic region of residence and are weighted to account for loss-to-follow-up.
Figure 1.
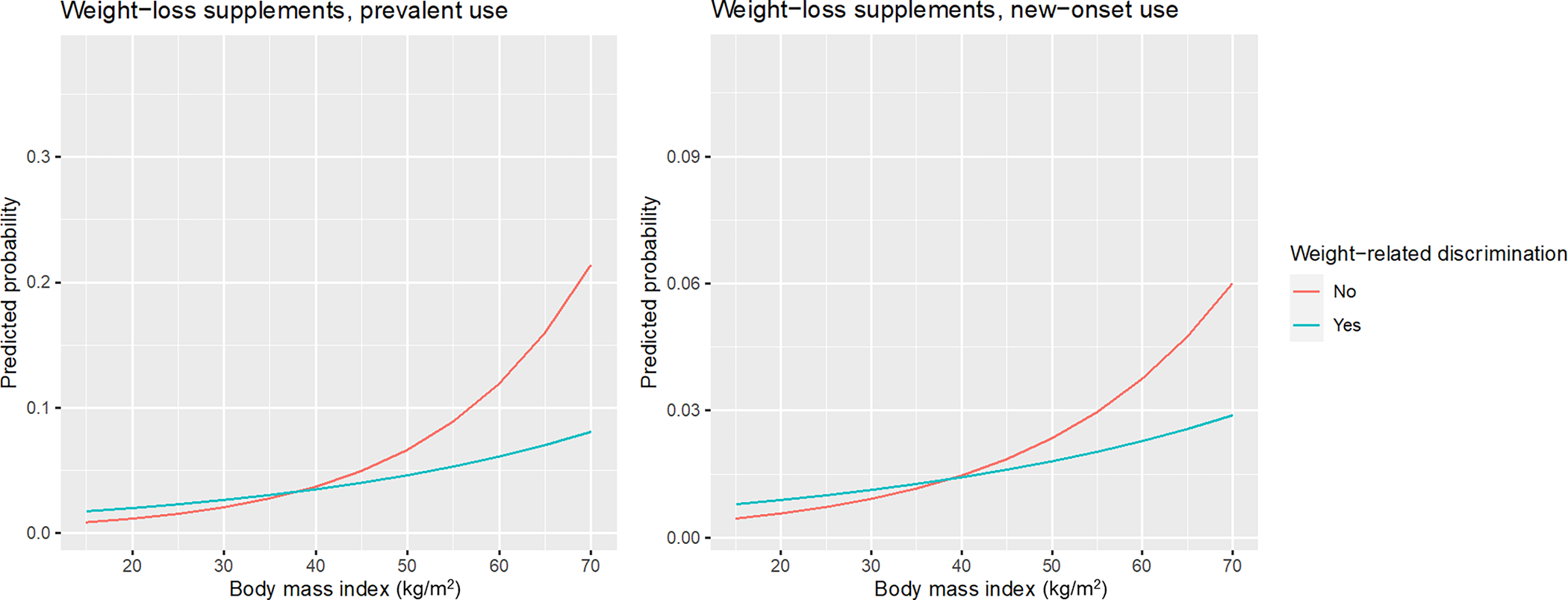
Predicted probability of prevalent and new onset weight-loss supplement use by body mass index (kg/m2) with effect measure modification by weight-related discrimination in the COVID-19 Pandemic Sub-Study across the study period (April/May 2020–April 2021), among cisgender women (N=51,814).
4. Discussion
In a cohort of over 50,000 cisgender women in the U.S., we found that higher weight status and experiencing weight discrimination, independently, were associated with prevalent and new onset use of weight-loss and energy supplements during the COVID-19 pandemic. Additionally, weight discrimination moderated associations between weight status and prevalent weight-loss and energy supplement use for women in the 25–29.9 kg/m2 and 30–34.9 kg/m2 weight status ranges, indicating that weight discrimination operates differently across weight status groups and is disproportionately harmful for those living in larger bodies. This is the first known study to examine use of potentially harmful dietary supplements and associations with weight discrimination during the COVID-19 pandemic and highlights the elevated health risks that people with higher weights may face as a result of greater societal weight stigma and ensuing discrimination, as well as exposure to deceptive and potentially dangerous dietary supplements.
Amidst increasing concerns among the general population about health and losing or maintaining weight during the pandemic (de Macêdo et al., 2022), the dietary supplements industry experienced a notable increase in sales (Grebow, 2021). Given the industry’s history of deceptive marketing tactics to exploit consumers’ health- and weight-related fears (Hua et al., 2021; Wilkes, 2019), which were likely elevated during the first year of the pandemic, it is unsurprising that we found associations between experiencing weight discrimination and the use of weight-loss, immune, and energy supplements, the latter of which may promoted for use to “rev up” metabolism (Blanck et al., 2007; Jeffers et al., 2013). However, the RERI indicating synergistic effects of weight status and weight discrimination on prevalent use of weight-loss and energy supplements was significantly elevated in this sample of cisgender women in only the lower end of the high weight status ranges (i.e., 25–29.9 kg/m2 and 30–34.9 kg/m2) and not among women with a BMI of 35 and higher. This was verified by sensitivity analyses, which identified that the RERI was not significant even when all women with a BMI of 35 and higher were combined into a single category. The ceiling effect of this additive interaction is visualized in Figure 1. At baseline, there is a seemingly linear positive relationship between weight status and prevalent use of weight-loss and energy supplements (Table 2), whereby prevalence of use is slightly higher among each increasing weight status group.
The Health Stigma and Discrimination Framework (Stangl et al., 2019) may be used to conceptualize how weight-related stigma manifests in such a way that discriminatory experiences may not have prompted increased risk of supplement use during the pandemic among cisgender women in the highest weight status ranges in this study. Indeed, experiencing weight discrimination was more common for individuals with larger bodies pre-pandemic (Puhl et al., 2008), and this relationship was likely upheld during the first year of the pandemic. However, it is possible that stigma marking and subsequent experiences of discrimination for cisgender women with higher weights was more severe for women who had previously not experienced as much weight stigma, lending to an increased risk of using supplements that they assumed might lend to weight loss at a time when weight stigma was especially salient (de Macêdo et al., 2022; Puhl et al., 2020). Alternatively, weight stigma and discrimination may be so ubiquitous for cisgender women with a BMI above 35 that there is not much nuance in the effects of discrimination on their use of weight-loss and energy supplements during the pandemic. It is also noteworthy that the RERI values for new onset use were not significant, which may indicate that the weight stigmatizing context of the pandemic did not in fact promote new use of supplements, but rather led to more persistent use among those who were already using weight-loss and energy supplements.
This study’s findings should be interpreted considering several limitations. First, the study sample is not representative of the U.S. population, as participants of the COVID-19 Substudy were drawn from NHSII, NHS3, and GUTS cohorts, which consists of respondents who were nurses or the children of nurses at the time of enrollment. Subsequently, the analytic sample of this study was majority non-Hispanic White and from a middle or higher socioeconomic background than the general population, limiting the generalizability. Given the compounding effects of varying stigmas (Stangl et al., 2019), such as racism, and known disparities in supplement use between white and racially/ethnically minoritized people (Pillitteri et al., 2008; Tsai et al., 2009) as well as greater financial burden of supplement use on low-income households in the U.S. (Austin et al., 2017), the findings may have underestimated the risk of use of potentially harmful supplements and its association with weight discrimination. Further, considering this study’s focus on cisgender women, the findings are not generalizable to cisgender men or transgender and gender diverse communities. The use of self-reported height and weight to determine BMI and weight status may have led to misclassification of participants, as the proportion of cisgender women participants in the 40–44.9 kg/m2 and ≥45 kg/m2 weight status ranges (4.7%) is noticeably lower than that of more generalizable samples (e.g., 11.4% in (Stierman et al., 2021). The primary exposure variable of lifetime weight discrimination was measured at only one wave and may not reflect the dynamism of weight discrimination experiences during the pandemic as well as how changes in discrimination may be associated with new onset use of supplements. Finally, sample attrition may have resulted in selection bias if participants who were most vulnerable and likely to experience weight discrimination and/or use supplements did not complete the latter surveys; however, this bias may have been ameliorated by the use of IPW in all statistical models.
The passage of DSHEA in 1994 codified a legal framework for the dietary supplements market that would not require pre-screening for safety nor efficacy of products (Sissung et al., 2021), placing vulnerable consumers at greater risk of experiencing the myriad of negative health consequences associated with adulteration and contamination of these products (Marcus, 2016; Mathews, 2018; Tucker et al., 2018; Yen & Ewald, 2012). Given the ways in which multiple stigmas, such as sexism and weight stigma, intersect and manifest in greater experiences of discrimination (Stangl et al., 2019), the lack of adequate industry oversight by government and known targeting of product advertising to women and individuals trying to lose weight places higher-weight cisgender women at elevated risks of using potentially harmful supplements. There is an urgent need for public health and government intervention against the dietary supplements industry and its inequitable impacts on marginalized populations, such as increased regulation of gendered supplement marketing, as well as policy efforts to reduce weight-based discrimination.
Supplementary Material
Highlights.
Disproportionate use of potentially harmful dietary supplements is well-documented
We assessed the influence of weight discrimination on supplement use among women
High weight women reporting weight discrimination have excess risk of supplement use
Excess risk was specific to potentially harmful weight-loss and immune supplements
Experiencing weight discrimination influenced supplement use during the pandemic
Funding:
This work was supported by the National Institutes of Health, Nation Heart, Lung and Blood Institute (NHLBI)/Office on Dietary Supplements (ODS) administrative supplement to parent grant NIH U01 HL145386; the Centers for Disease Control and Prevention and the National Institute for Occupational Safety and Health (75D30120P08255); the National Institutes of Health (U01HL145386, R24ES028521, U01CA176726, R01CA67262, R01HD057368); the Canadian Institutes of Health Research, Institute of Population and Public Health (co-author AR: MFE-171217); the National Institute on Minority Health and Health Disparities (co-author AB: 1F32MD017452-01); the National Institute of Environmental Health Sciences (co-author JH: P30 ES000002); and the Maternal and Child Health Bureau, Health Resources and Services Administration (co-author SBA: T76MC00001).
Footnotes
Declarations of Interest: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adams KK, Baker WL, & Sobieraj DM (2020). Myth busters: Dietary supplements and COVID-19. Annals of Pharmacotherapy, 54(8), 820–826. 10.1177/1060028020928052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alberga AS, Edache IY, Forhan M, & Russell-Mayhew S (2019). Weight bias and health care utilization: A scoping review. Primary Health Care Research & Development, 20, e116, Article e116. 10.1017/S1463423619000227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aldrich T, & Hackley B (2010). The impact of obesity on gynecologic cancer screening: An integrative literature review. Journal of Midwifery & Women’s Health, 55(4), 344–356. 10.1016/j.jmwh.2009.10.001 [DOI] [PubMed] [Google Scholar]
- Austin SB, Beccia AL, Raffoul A, Jackson DA, Sarda V, Hart JE, Chavarro JE, & Rich-Edwards J (2023). Financial precarity, food insecurity, and psychological distress prospectively linked with use of potentially dangerous dietary supplements during the pandemic in the US. Frontiers in Public Health, 11. 10.3389/fpubh.2023.1120942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Austin SB, Yu K, Liu SH, Dong F, & Tefft N (2017). Household expenditures on dietary supplements sold for weight loss, muscle building, and sexual function: Disproportionate burden by gender and income. Preventive Medicine Reports, 6, 236–241. 10.1016/j.pmedr.2017.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanck HM, Serdula MK, Gillespie C, Galuska DA, Sharpe PA, Conway JM, Khan LK, & Ainsworth BE (2007). Use of nonprescription dietary supplements for weight loss is common among Americans. Journal of the American Dietetic Association, 107(3), 441–447. 10.1016/j.jada.2006.12.009 [DOI] [PubMed] [Google Scholar]
- Burmeister JM, Kiefner AE, Carels RA, & Musher-Eizenman DR (2013). Weight bias in graduate school admissions. Obesity, 21(5), 918–920. 10.1002/oby.20171 [DOI] [PubMed] [Google Scholar]
- Calogero RM, Tylka TL, & Mensinger JL (2016). Scientific weightism: A view of mainstream weight stigma research through a feminist lens. In Roberts T-A, Curtin N, Duncan LE, & Cortina LM (Eds.), Feminist Perspectives on Building a Better Psychological Science of Gender (pp. 9–28). [Google Scholar]
- Carter A, Hoang N, Gilbert P, & Kirby JN (2022). Body weight perception outweighs body weight when predicting shame, criticism, depression and anxiety for lower BMI range and higher BMI range adults. J Health Psychol, 27(10), 2276–2290. 10.1177/13591053211027641 [DOI] [PubMed] [Google Scholar]
- Cassileth BR, Heitzer M, & Wesa K (2009). The public health impact of herbs and nutritional supplements. Pharmaceutical Biology, 47(8), 761–767. 10.1080/13880200902991581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ciciurkaite G, & Perry BL (2017). Body weight, perceived weight stigma and mental health among women at the intersection of race/ethnicity and socioeconomic status: Insights from the modified labelling approach. Sociology of Health and Illness, 40(1), 18–37. 10.1111/1467-9566.12619 [DOI] [PubMed] [Google Scholar]
- de Macêdo PFC, Nepomuceno CMM, dos Santos NS, Queiroz V. A. d. O., Pereira EM, Leal L. d. C., Santos L. A. d. S., Nascimento LF, Martins PC, & de Santana MLP (2022). Weight stigma in the COVID-19 pandemic: a scoping review. Journal of Eating Disorders, 10(1), 1–15. 10.1186/S40337-022-00563-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fewell Z, Hernán MA, Wolfe F, Tilling K, Choi H, & Sterne JAC (2004). Controlling for time-dependent confounding using marginal structural models. The Stata Journal, 4(4), 402–420. [DOI] [Google Scholar]
- Fikkan JL, & Rothblum ED (2012). Is fat a feminist issue? Exploring the gendered nature of weight bias. Sex Roles, 66(9–10), 575–592. 10.1007/s11199-011-0022-5 [DOI] [Google Scholar]
- Geller AI, Shehab N, Weidle NJ, Lovegrove MC, Wolpert BJ, Timbo BB, Mozersky RP, & Budnitz DS (2015). Emergency department visits for adverse events related to dietary supplements. New England Journal of Medicine, 373(16), 1531–1540. 10.1056/NEJMSA1504267/SUPPL_FILE/NEJMSA1504267_DISCLOSURES.PDF [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goffman E (1963). Stigma: Notes on the Management of Spoiled Identity. Simon & Schuster. [Google Scholar]
- Grebow J (2021). Dietary supplement sales success post-COVID: How can industry keep the momentum going after the pandemic? Retrieved April 3 from https://www.nutritionaloutlook.com/view/dietary-supplement-sales-success-post-covid-how-can-industry-keep-the-momentum-going-after-the-pandemic
- Hamulka J, Jeruszka-Bielak M, Górnicka M, Drywień ME, & Zielinska-Pukos MA (2020). Dietary supplements during COVID-19 outbreak. Results of Google Trends analysis supported by PLifeCOVID-19 online studies. Nutrients, 13(1), 54–54. 10.3390/nu13010054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Himmelstein MS, Puhl RM, & Quinn DM (2017). Intersectionality: An understudied framework for addressing weight stigma. American Journal of Preventive Medicine, 53(4), 421–431. 10.1016/j.amepre.2017.04.003 [DOI] [PubMed] [Google Scholar]
- Himmelstein MS, Puhl RM, & Quinn DM (2018). Weight stigma and health: The mediating role of coping responses. Health Psychology, 37(2), 139–147. 10.1037/hea0000575 [DOI] [PubMed] [Google Scholar]
- Hua SV, Granger B, Bauer K, & Roberto CA (2021). A content analysis of marketing on the packages of dietary supplements for weight loss and muscle building. Preventive Medicine Reports, 23, 101504. 10.1016/j.pmedr.2021.101504 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunger JM, Smith JP, & Tomiyama AJ (2020). An evidence-based rationale for adopting weight-inclusive health policy. Social Issues and Policy Review, 14(1), 73–107. 10.1111/sipr.12062 [DOI] [Google Scholar]
- Jeffers A, Benotsch EG, & Koester S (2013). Misuse of prescription stimulants for weight loss, psychosocial variables, and eating disordered behaviors. Appetite, 65, 8–13. 10.1016/j.appet.2013.01.008 [DOI] [PubMed] [Google Scholar]
- Kompaniyets L, Goodman AB, Belay B, Freedman DS, Sucosky MS, Lange SJ, Gundlapalli AV, Boehmer TK, & Blanck HM (2021). Body mass index and risk for COVID-19-related hospitalization, intensive care unit admission, invasive mechanical ventilation, and death - United States, March-December 2020. Morbidity and Mortality Weekly Report, 70(10), 355–361. 10.15585/mmwr.mm7010e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lordan R (2021). Dietary supplements and nutraceuticals market growth during the coronavirus pandemic - Implications for consumers and regulatory oversight. PharmaNutrition, 18, 100282. 10.1016/j.phanu.2021.100282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCann C, & Roberts RD (2013). Just as smart but not as successful: Obese students obtain lower school grades but equivalent test scores to nonobese students. International Journal of Obesity, 37(1), 40–46. 10.1038/ijo.2012.47 [DOI] [PubMed] [Google Scholar]
- Marcus DM (2016). Dietary supplements: What’s in a name? What’s in the bottle? Drug Testing and Analysis, 8(3–4), 410–412. 10.1002/DTA.1855 [DOI] [PubMed] [Google Scholar]
- Mason TB, Mozdzierz P, Wang S, & Smith KE (2021). Discrimination and eating disorder psychopathology: A meta-analysis. Behavior Therapy, 52(2), 406–417. 10.1016/j.beth.2020.05.003 [DOI] [PubMed] [Google Scholar]
- Mathews NM (2018). Prohibited contaminants in dietary supplements. Sports Health: A Multidisciplinary Approach, 10(1), 19–30. 10.1177/1941738117727736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meyer J, McDowell C, Lansing J, Brower C, Smith L, Tully M, & Herring M (2020). Changes in physical activity and sedentary behavior in response to covid-19 and their associations with mental health in 3052 us adults. International Journal of Environmental Research and Public Health, 17(18), 1–13. 10.3390/ijerph17186469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monaghan LF (2016). Re-framing weight-related stigma: From spoiled identity to macro-social structures. Social Theory & Health, 15(2), 1–24. 10.1057/s41285-016-0022-1 [DOI] [Google Scholar]
- Murnen SK, & Smolak L (2015). Gender and eating disorders. In The Wiley Handbook of Eating Disorders (pp. 352–366). 10.1002/9781118574089.ch27 [DOI] [Google Scholar]
- Or F, Kim Y, Simms J, & Austin SB (2019). Taking stock of dietary supplements’ harmful effects on children, adolescents, and young adults. Journal of Adolescent Health, 65(4), 455–461. 10.1016/j.jadohealth.2019.03.005 [DOI] [PubMed] [Google Scholar]
- Pillitteri JL, Shiffman S, Rohay JM, Harkins AM, Burton SL, & Wadden TA (2008). Use of dietary supplements for weight loss in the United States: results of a national survey. Obesity, 16(4), 790–796. 10.1038/oby.2007.136 [DOI] [PubMed] [Google Scholar]
- Piran N (2010). A feminist perspective on risk factor research and on the prevention of eating disorders. Eating Disorders, 18(3), 183–198. 10.1080/10640261003719435 [DOI] [PubMed] [Google Scholar]
- Pomeranz JL, Barbosa G, Killian C, & Austin SB (2015). The dangerous mix of adolescents and dietary supplements for weight loss and muscle building: Legal strategies for state action. J Public Health Manag Pract, 21(5), 496–503. 10.1097/phh.0000000000000142 [DOI] [PubMed] [Google Scholar]
- Prohaska A (2023). “Help curb the hunger pangs”: News media frames of weight loss during the COVID-19 lockdown. Critical Public Health, 33(3), 332–342. 10.1080/09581596.2022.2104155 [DOI] [Google Scholar]
- Puhl RM, Andreyeva T, & Brownell KD (2008). Perceptions of weight discrimination: Prevalence and comparison to race and gender discrimination in America. International Journal of Obesity, 32(6), 992–1000. 10.1038/ijo.2008.22 [DOI] [PubMed] [Google Scholar]
- Puhl RM, Lessard LM, Larson N, Eisenberg ME, & Neumark-Stzainer D (2020). Weight stigma as a predictor of distress and maladaptive eating behaviors during COVID-19: Longitudinal findings from the eat study. Annals of Behavioral Medicine, 54(10), 738–746. 10.1093/ABM/KAAA077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rich-Edwards JW, Ding M, Rocheleau CM, Boiano JM, Kang JH, Becene I, Nguyen LH, Chan AT, Hart JE, Chavarro JE, & Lawson CC (2021). American frontline healthcare personnel’s access to and use of personal protective equipment early in the COVID-19 pandemic. J Occup Environ Med, 63(11), 913–920. 10.1097/jom.0000000000002308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodgers RF, Lombardo C, Cerolini S, Franko DL, Omori M, Fuller-Tyszkiewicz M, Linardon J, Courtet P, & Guillaume S (2020). The impact of the COVID-19 pandemic on eating disorder risk and symptoms. International Journal of Eating Disorders, 53(7), 1166–1170. 10.1002/eat.23318 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel JA, & Calogero RM (2019). Conformity to feminine norms and self-objectification in self-identified feminist and non-feminist women. Body Image, 28, 115–118. 10.1016/j.bodyim.2019.01.005 [DOI] [PubMed] [Google Scholar]
- Sissung TM, Cordes LM, & Figg WD (2021). The Dietary Supplement Health And Education Act: Are we healthier and better informed after 27 years? The Lancet Oncology, 22(7), 915–916. 10.1016/S1470-2045(21)00084-X [DOI] [PubMed] [Google Scholar]
- Stangl AL, Earnshaw VA, Logie CH, van Brakel W, Simbayi C, L., Barré I, & Dovidio JF (2019). The Health Stigma and Discrimination Framework: A global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Medicine, 17(1), 31. 10.1186/s12916-019-1271-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stierman B, Afful J, Carroll MD, Chen T-C, Davy O, Fink S, Fryar CD, Gu Q, Hales CM, Hughes JP, Ostchega Y, Storandt RJ, & Akinbami LJ (2021). National Health and Nutrition Examination Survey 2017–March 2020 prepandemic data files —Development of files and prevalence estimates for selected health outcomes [Journal Issue]. National Health Statistics Reports(158). https://stacks.cdc.gov/view/cdc/106273 [Google Scholar]
- Sutin AR, Stephan Y, Grzywacz JG, Robinson E, Daly M, & Terracciano A (2016). Perceived weight discrimination, changes in health, and daily stressors. Obesity, 24(10), 2202–2209. 10.1002/oby.21598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutin AR, Stephan Y, & Terracciano A (2015). Weight discrimination and risk of mortality. Psychol Sci, 26(11), 1803–1811. 10.1177/0956797615601103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Termorshuizen JD, Watson HJ, Thornton LM, Borg S, Flatt RE, MacDermod CM, Harper LE, van Furth EF, Peat CM, & Bulik CM (2020). Early impact of COVID-19 on individuals with self-reported eating disorders: A survey of ~1,000 individuals in the United States and the Netherlands. International Journal of Eating Disorders, 53(11), 1780–1790. 10.1002/eat.23353 [DOI] [PubMed] [Google Scholar]
- Tomiyama AJ, Carr D, Granberg EM, Major B, Robinson E, Sutin AR, & Brewis A (2018). How and why weight stigma drives the obesity ‘epidemic’ and harms health. BMC Medicine, 16(1), 123–123. 10.1186/s12916-018-1116-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AG, Wadden TA, Pillitteri JL, Sembower MA, Gerlach KK, Kyle TK, & Burroughs VJ (2009). Disparities by ethnicity and socioeconomic status in the use of weight loss treatments. Journal of the National Medical Association, 101(1), 62–70. http://www.ncbi.nlm.nih.gov/pubmed/19245074 [DOI] [PubMed] [Google Scholar]
- Tucker J, Fischer T, Upjohn L, Mazzera D, & Kumar M (2018). Unapproved pharmaceutical ingredients included in dietary supplements associated with US Food and Drug Administration warnings. JAMA Network Open, 1(6), e183337–e183337. 10.1001/JAMANETWORKOPEN.2018.3337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vadiveloo M, & Mattei J (2017). Perceived weight discrimination and 10-year risk of allostatic load among US adults. Annals of Behavioral Medicine, 51(1), 94–104. 10.1007/s12160-016-9831-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vanderperren B, Rizzo M, Angenot L, Haufroid V, Jadoul M, & Hantson P (2005). Acute liver failure with renal impairment related to the abuse of senna anthraquinone glycosides. Annals of Pharmacotherapy, 39(7–8), 1353–1357. 10.1345/aph.1E670 [DOI] [PubMed] [Google Scholar]
- Vanhove A, & Gordon RA (2014). Weight discrimination in the workplace: A meta-analytic examination of the relationship between weight and work-related outcomes. Journal of Applied Social Psychology, 44(1), 12–22. 10.1111/jasp.12193 [DOI] [Google Scholar]
- Vitagliano JA, Beccia A, Mattei J, Cory H, & Austin SB (2022). Disproportionate use of over-the-counter diet pills among Latinx youth and increased use over time among Latinx females: Results of US national study. Journal of Adolescent Health, 70(6), 993–996. 10.1016/J.JADOHEALTH.2022.01.126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Neilson LC, & Ji S (2023). Why and how do consumers use dietary supplements? A systematic review and thematic analysis. Health Promotion International, 38(1). 10.1093/heapro/daac197 [DOI] [PubMed] [Google Scholar]
- Ward JB, Gartner DR, Keyes KM, Fliss MD, McClure ES, & Robinson WR (2019). How do we assess a racial disparity in health? Distribution, interaction, and interpretation in epidemiological studies. Ann Epidemiol, 29, 1–7. 10.1016/j.annepidem.2018.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wharton S, Bonder R, Jeffery A, & Christensen RAG (2020). The safety and effectiveness of commonly-marketed natural supplements for weight loss in populations with obesity: A critical review of the literature from 2006 to 2016. Critical Reviews in Food Science and Nutrition, 60(10), 1614–1630. 10.1080/10408398.2019.1584873 [DOI] [PubMed] [Google Scholar]
- Wilkes B (2019, August 19, 2016). Hispanic purchasing power won’t be ignored, ask Herbalife. Retrieved April 3, 2023 from https://thehill.com/blogs/pundits-blog/civil-rights/291996-hispanic-purchasing-power-wont-be-ignored-ask-herbalife/ [Google Scholar]
- Williams DR, Yan Y, Jackson JS, & Anderson NB (1997). Racial differences in physical and mental health. Journal of Health Psychology, 2(3), 335–351. 10.1177/135910539700200305 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2020). COVID-19 and NCD risk factors. https://www.who.int/docs/default-source/ncds/un-interagency-task-force-on-ncds/uniatf-policy-brief-ncds-and-covid-030920-poster.pdf
- Yen M, & Ewald MB (2012). Toxicity of weight loss agents. Journal of Medical Toxicology, 8(2), 145–152. 10.1007/S13181-012-0213-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu X, Smith RA, & Buteau E (2022). A meta-analysis of weight stigma and health behaviors. Stigma and Health, 7(1), 1–13. 10.1037/sah0000352 [DOI] [Google Scholar]
- Zou GY, & Donner A (2013). Extension of the modified Poisson regression model to prospective studies with correlated binary data. Statistical Methods in Medical Research, 22(6), 661–670. 10.1177/0962280211427759 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


