Abstract
We provide an overview of the assessment and management of inducible laryngeal obstruction and breathing pattern disorder. We highlight the multidisciplinary team members involved and their essential roles within a complex breathlessness service. We discuss treatments initiated by physiotherapy and speech and language therapy, the importance of joint working, and discuss the high incidence of comorbidities and the association with other respiratory disorders.
Educational aims
Inducible laryngeal obstruction and breathing pattern disorder are common causes of breathlessness.
Inducible laryngeal obstruction is an inappropriate, transient, reversible narrowing of the laryngeal area that causes breathlessness and laryngeal symptoms.
Breathing pattern disorder is an alteration in the normal biomechanical patterns of breathing that results in intermittent or chronic symptoms, which may be respiratory and/or non-respiratory.
People with inducible laryngeal obstruction or breathing pattern disorder often have other comorbidities that will also need addressing.
Multidisciplinary assessment and treatment is essential for comprehensive workup and holistic care.
Timely assessment and diagnosis can prevent unnecessary medication use and hospital admissions and facilitate effective management of the condition using reassurance, advice, education, breathing retraining and vocal exercises.
Tweetable abstract
Inducible laryngeal obstruction and breathing pattern disorder are common causes of breathlessness. Multidisciplinary assessment can prevent unnecessary medication use, hospital admissions and facilitate effective management of these complex conditions. https://bit.ly/47tSYe1
Introduction
Respiratory symptoms such as dyspnoea, chest and throat tightness, cough, and noisy breathing are nonspecific, and clinical assessment and testing are required to make a diagnosis. Many patients have persistent symptoms either in the absence of an obvious cause or when the most obvious cause has been adequately treated. We use the term “complex breathlessness” to describe this presentation, as also defined in the ERS Monograph in 2022 [1]. Two leading causes of complex breathlessness are inducible laryngeal obstruction (ILO) and breathing pattern disorder (BPD). Over the years several terms have been used to describe these disorders, such as paradoxical fold motion and vocal cord dysfunction for ILO, and functional breathing disorder and dysfunctional breathing for BPD [2, 3]. Individuals with ILO and BPD present across a variety of healthcare settings with differing levels of morbidity [4] and can attract unnecessary medical treatment and increased healthcare utilisation [5]. Having access to a specialist multidisciplinary team (MDT) can reduce economic and healthcare burden by reducing general practitioner visits, hospitalisations and prescribing of unnecessary medications [6].
Inducible laryngeal obstruction
ILO describes an inappropriate, transient, reversible narrowing of the laryngeal aperture in response to an external trigger [7]. It generally occurs during inspiration and comes on suddenly with symptoms localised to the throat or upper chest [4, 7, 8]. It occurs at the glottic and/or supraglottic level [7], and patients report symptoms of dyspnoea, cough, throat tightness, chest tightness and dysphonia [9]. Symptoms are usually transient and follow exposure to specific laryngeal irritants [10], these include strong scents, temperature changes, airborne irritants, vocalisation, physical activity, and occupational factors [11, 12]. The pathophysiological link between triggers and ILO is not fully understood [3] and there may be various phenotypes of ILO demonstrating different symptom responses [13]. The true prevalence of ILO is unknown, but it is more common in females over a broad age range [4, 8].
Breathing pattern disorder
BPD describes an alteration in the normal pattern of breathing that can result in intermittent or chronic respiratory and non-respiratory symptoms in the absence, or in excess of, any organic respiratory disease [14–16]. The key symptom in BPD is dyspnoea; hyperventilation is also often associated with dizziness, chest tightness, frequent yawning, deep sighing and blurred vision [14, 17, 18]. The pathogenesis of BPD remains unclear, but is likely to be a combination of biomechanical and biochemical stimuli and psychopathological factors [19, 20]. The most widely recognised form of BPD is hyperventilation; however, this is just one type of BPD and individuals may display different phenotypes including thoracic dominant breathing, forced abdominal expiration, thoraco-abdominal asynchrony and end-expiratory breathing [14], which may coexist with each other. The prevalence of BPD is unknown due to the lack of a gold standard diagnosis, but like ILO it often coexists with other respiratory conditions and comorbidities.
Comorbidities
As symptoms of ILO and BPD are nonspecific, a careful approach to differential diagnosis is essential to ensure the correct management is given. Often patients with ILO/BPD are misdiagnosed with, or have coexisting, asthma [21, 22]. The prevalence of ILO in asthma ranges from 19% to 50% depending on the severity of asthma [5, 23]. The prevalence of BPD in asthma can be as high as 80% in non-severe asthma [24, 25], and 20–30% in severe asthma [26, 27]. Nasal disease is often found as an aggravating comorbidity in ILO and BPD, and treatment of nasal disease can improve both nasal breathing and ILO and BPD symptoms [21, 28]. Likewise, reflux is often described as an aggravating factor by patients and professionals [29–31]. ILO symptoms can occur following exposure to a substance and be misdiagnosed an allergic reaction [32], but without other features of anaphylaxis or angioedema [13, 32]. Depression and anxiety are significant comorbid factors for ILO and BPD [33] and are associated with worse health status, but they are also common with chronic breathlessness caused by other respiratory conditions [19]. It is important to rule out any organic cause for laryngeal symptoms or dyspnoea (e.g. vocal cord palsy, subglottic stenosis or diaphragmatic weakness). Visualising the upper airway to ensure there are no structural abnormalities is essential in the workup. If any structural abnormalities are identified patients are immediately referred to specialist ear, nose and throat (ENT) colleagues. Cardiac disease and neurological factors should also be ruled out in all cases of ILO and BPD.
Multidisciplinary teamworking
To assess complex breathlessness, patients should undergo an MDT assessment to explore all factors that could be contributing to their symptoms [34, 35]. Our tertiary clinic receives referrals from across the UK, and all new referrals are given a “one stop” assessment appointment where a full clinical history and initial investigations are completed. The time from initial referral and triage to one-stop assessment is typically 6 months. The team includes physicians, speech and language therapists (SLTs), respiratory physiotherapists, a clinical nurse specialist (CNS), clinical psychologist, pharmacist and MDT coordinator. Each team member has unique skills and expertise, providing a holistic assessment and treatment approach as shown in table 1.
TABLE 1.
Manchester Airways Service multidisciplinary team (MDT) members and roles
| MDT member | MDT role |
| Respiratory physician | Triage referrals |
| Diagnose, treat, and manage upper airway and other respiratory conditions | |
| Request and interpret additional respiratory tests (e.g. imaging and lung function, bronchoscopy) | |
| Prescribe or discontinue medication as appropriate | |
| Speech and language therapist | Provide expert assessment of upper airway dysfunction, contributing to differential diagnosis and non-pharmacological management |
| Provide a provocation laryngoscopy service | |
| Provide individualised therapy programmes to resolve upper airway symptoms to premorbid state or maximal potential | |
| Clinical nurse specialist | Provide specialist knowledge, skills and leadership in triage, diagnosis, and treatment |
| Manage patients in a nurse-led clinic independently, providing individualised care plans | |
| Provide non-medical prescribing; working in alignment with local and national nurse prescribing guidelines | |
| Liaise with the severe asthma service where appropriate | |
| Physiotherapist | Provide expert comprehensive assessment of suspected BPD |
| Develop individualised physiotherapy treatment programmes and self-management strategies, in collaboration with the patient and in response to patient need | |
| Improve symptoms and functional ability to maximal potential | |
| Clinical psychologist | Provide comprehensive assessment and formulation to show the psychological impact of respiratory disease |
| Enable patients in understanding the nature and implications of their respiratory condition | |
| Enable patients in developing therapy goals, addressing unrealistic expectations | |
| Enable patients to adapt to their respiratory condition, exploring ways to reduce the impact of their condition | |
| Build self-efficacy and coping abilities | |
| Address any fears, concerns or misunderstanding about their respiratory diagnosis | |
| Help patients to cope with the emotional triggers of breathing difficulties such as anxiety/depression | |
| Support the MDT in the treatment of patients presenting with complex difficulties by offering consultation, complex care planning and indirect formulation | |
| Pharmacist | Provide education on the role of inhaled medication |
| Provide training on correct inhaler technique | |
| Provide reassurance on the side-effects of medication | |
| Improve patient adherence to inhaled therapies | |
| Provide advice on reducing oral corticosteroids | |
| MDT coordinator | Support the MDT team in collating all information needed |
| Coordinate booking of all clinics | |
| Ensure effective communication across the patient pathway | |
| Attend MDT meetings: ensuring all correspondence and investigations are available; making notes and actioning any outcomes | |
| Work collaboratively with medical secretaries and operational delivery network leads to ensure appropriate management of patient information and coordination of patient pathways | |
| Dealing with patient telephone enquiries and promptly communicate to the team any urgent actions | |
| All team members | Participate in MDT meetings |
| Contribute to education and training | |
| Dissemination of respiratory updates through in-service training and supervision | |
| Hosting visits from external teams | |
| Support research |
BPD: breathing pattern disorder.
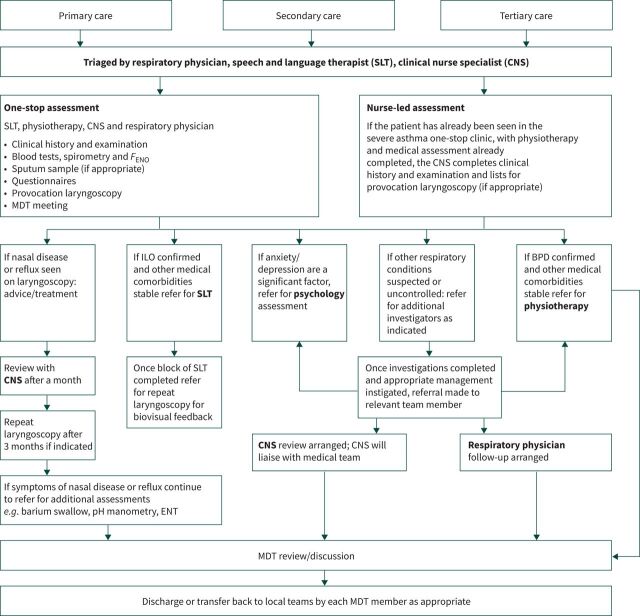
All patients are seen for an initial assessment by the MDT and are then either sent for further investigations, listed for pharmacological trials, referred for speech and language therapy and/or physiotherapy, or referred onto another service (see figure 1). We have close links with the regional severe asthma service and several members of the MDT work across both teams. We have a bimonthly complex cases MDT including respiratory, ENT, allergy and intensive care specialities. This allows teams to bring together the expertise and skills of different professionals to assess, plan and manage care jointly, and ensure a timely and effective service for patients.
FIGURE 1.
Manchester Airways Service referral pathway. FENO: exhaled nitric oxide fraction; MDT: multidisciplinary team; ILO: inducible laryngeal obstruction; ENT: ear, nose and throat.
Assessment and diagnosis
The diagnosis of ILO and/or BPD is not straightforward, and many patients present with symptoms that have been misinterpreted by both patients and clinicians for some time [9]. Often an incorrect diagnosis of severe asthma has led to escalating doses of inhaled and/or oral steroids, yet patients typically describe no clear benefit.
During a one-stop assessment patients will have tests such as spirometry, fractional exhaled nitric oxide (FENO), bloods, sputum induction (if appropriate and able to produce) and provocation laryngoscopy. The bloods requested will vary depending on previous investigations, but typically consist of routine haematology, biochemistry and an allergy screen. Patient-reported outcome questionnaires (see table 2) are completed during every one-stop assessment, to help understand issues and concerns that are specific to the patient. The questionnaire scores along with detailed case history and diagnostic tests help understand the patient's main symptom concerns and therapy priorities. During laryngoscopy, the structure and function of the larynx is assessed as well as any comorbidities such as nasal disease and reflux. More recently, alternative methods for diagnosing ILO have been described, such as dynamic computed tomography [42] or ultrasound of the larynx [43], but these are not currently widely used in clinical practice.
TABLE 2.
Upper airway questionnaires used in the one-stop assessment clinic
| Questionnaire | Target area | Summary |
| Vocal Cord Dysfunction Questionnaire (VCDQ) [10] | ILO | A 12-item questionnaire for symptom monitoring in ILO 5-point Likert scale (1–5) |
| Score range: 12–60 | ||
| Minimal clinically important change: 4 | ||
| Total Nasal Symptom Score (TNSS) [36] | Nasal disease | Adapted version: 3-item questionnaire |
| 4-point Likert scale (0–3) | ||
| Score range: 0–9 | ||
| Minimal clinically important change reported from: 0.28–3.6 | ||
| Asthma Control Questionnaire (ACQ) [37] | Asthma | Adapted version: ACQ-5 5-item questionnaire |
| 7-point Likert scale (0–6) | ||
| Mean score of all responses calculated; score range: 0–6 | ||
| A score below 1 interpreted as good control | ||
| Minimal clinically important change: 0.5 | ||
| Nijmegen questionnaire [24] | BPD | Validated for hyperventilation syndrome (Note: not known to be valid in all types of BPD) |
| 16-item questionnaire | ||
| 5-point Likert scale (0–4) | ||
| Scored out of 64 | ||
| Score over 23 suggestive of hyperventilation syndrome | ||
| Modified Medical Research Council (mMRC) scale [38] | Multidimensional breathlessness | Adapted scale |
| Used to assess the degree of baseline functional disability due to dyspnoea | ||
| 5-point scale (0–4) | ||
| Minimal clinically important change: 0.5 | ||
| GAD-7 [39] | Anxiety | Captured over the past 2 weeks |
| 7-item questionnaire | ||
| 4-point Likert scale (0–3) | ||
| Cut-offs of 5, 10 and 15 for mild, moderate and severe anxiety | ||
| Minimal clinical important change: 4 | ||
| PHQ-8 [40] | Depression | Captured over the past 2 weeks |
| 8-item questionnaire | ||
| 4-point Likert scale (0–3) | ||
| Cut-offs of 2, 5, 8 and 12 for normal, mild, moderate and severe depression | ||
| Minimal clinical important change: 3 | ||
| Dyspnoea-12 (D-12) [41] | Multidimensional breathlessness | 12-item questionnaire covering both physical and psychological dimensions. |
| 4-point likert scale (0–3) | ||
| Item scores are summed and can be divided into subscales reflecting physical and affective domains. | ||
| Minimal clinical important change 0.25 |
ILO: inducible laryngeal obstruction; BPD: breathing pattern disorder.
MDT roles
Respiratory physician
The role of the respiratory physician is to triage referrals for patients describing suggestive symptoms and ensure other respiratory and non-respiratory comorbidities are diagnosed and adequately treated. If it is felt that symptoms are due to uncontrolled comorbidity, treatment can be optimised or changed, and further investigations or referrals can be ordered where indicated. Common comorbidities include asthma, bronchiectasis, reflux and rhinitis, but because most patients have already undergone specialist assessment prior to referral, less common conditions, such as excessive dynamic airways collapse and neuromuscular disease, are uncovered relatively frequently. During laryngoscopy if it is felt reflux or nasal disease is a contributing factor and treatment is not optimised, appropriate medication can be prescribed, further investigations ordered, or onward referrals made to relevant specialities such as gastroenterology, allergy and ENT.
Owing to the transient nature of ILO symptoms, the consensus gold standard for diagnosis is laryngoscopy with provocation [27]. In our service, provocation laryngoscopy is performed with both the respiratory physician and SLT present. Patients are exposed to relevant irritants (such as aerosols, talking, laughing or exercise) whilst the laryngoscope is in place. Often this will provoke symptoms of ILO and/or BPD and so contribute to diagnosis and treatment planning.
Speech and language therapist
The most effective treatment for ILO is speech and language therapy, via laryngeal control therapy [9, 11, 44, 45]. SLTs have the skills to contribute across a patient's clinical journey, i.e. during assessment, differential diagnosis, management planning, treatment and discharge. They have the expertise to obtain an upper airway history, asking specifically about symptoms that are associated with ILO (dryness, tightness, globus pharyngeous, dysphonia and tickle) and play a key role in educating patients on managing upper airway conditions, using upper airway breathing techniques, vocal hygiene training, cough suppression strategies and psychoeducational counselling. Following laryngoscopy, patients can visualise their larynx via immediate video playback, and biovisual feedback is given pre- and post-therapy to aid understanding. Although the specialist SLTs do not manage dysphonia and dysphagia in our service, they do have the knowledge to ask about symptoms related to these conditions and refer on to specialist services if required. As laryngeal specialists they have experience of identifying any structural abnormalities in the upper airway and can make timely referrals to ENT if indicated. There are currently no well validated diagnostic measures for ILO, but several patient questionnaires have been developed and are used to assist in diagnosis and measure patient-reported outcomes, as shown in table 2.
Physiotherapist
The role of a specialist respiratory physiotherapist is integral to the assessment, diagnosis, and management of BPD. A management plan for BPD can be developed following comprehensive assessment alongside the MDT to ensure treatable traits or other contributing factors are identified and addressed [40]. Physiotherapy assessment includes subjective assessment, history of presenting condition including duration and any precipitating factors, and patient-reported symptoms including breathlessness and sputum burden. Review of triggers and easing factors and associated symptoms such as tetany, social history, exercise tolerance, past medical history and previous investigations are completed. Outcome measures may include questionnaires to understand patient-reported symptoms and aid evaluation of breathlessness [19] as shown in table 2. Assessment of the patient includes observation of breathlessness and breathing pattern, hands-on assessment including Manual Assessment of Respiratory Motion, and may include lung function testing [46, 47]. Alternatively, a validated measure such as the Breathing Pattern Assessment Tool can be used to score aspects of breathing pattern [35]. Assessment and management need to consider the biochemical, biomechanical and psychophysiological components of the patients breathing pattern [48]. Once identified management plans include collaborative working and understanding the problems from the patient's perspective, breathlessness management, education, lifestyle management that may have contributary factors to BPD, and an individualised breathing retraining programme (see table 3) [2, 9].
TABLE 3.
Therapy techniques for inducible laryngeal obstruction (ILO) and breathing pattern disorder (BPD)
| Diagnosis | Therapy provided |
| ILO | Breathing strategies (rescue breathing, diaphragmatic breathing, relaxed breathing) |
| Vocal hygiene advice and vocal exercises | |
| Laryngeal desensitisation | |
| Cough suppression | |
| Relaxation of head and neck extrinsic muscle tension | |
| Release of inappropriate upper airway constriction | |
| Posture control | |
| Education and differentiation with other respiratory conditions | |
| Discussion of contributory and maintaining factors | |
| Relaxation | |
| Psychoeducational counselling | |
| Biovisual feedback using laryngoscopy | |
| Controlling symptoms during provocation | |
| Reassurance | |
| BPD | Education on the pathophysiology of the disorder |
| Self-observation of the BPD and kinaesthetic feedback | |
| Breathing retraining (pursed lip breathing, nasal breathing, diaphragmatic breathing) | |
| Appropriate tidal volume | |
| Education of stress and tension in the body | |
| Posture control | |
| Breathing with movement and activity | |
| Breathing with speech | |
| Reassurance |
Clinical nurse specialist
The CNS role is a vital and fundamental part of the MDT to help form the correct diagnosis and deliver the right treatment for patients with ILO and other coexisting conditions. The CNS brings knowledge, skills and leadership as an expert in the diagnosis and treatment of respiratory disease. During the one-stop assessment the CNS obtains a full clinical history and performs clinical tests including chest auscultation, lung function and FENO measurements to gain an in-depth understanding of the patient's current condition. The CNS has extensive knowledge and expertise in respiratory care, and therefore, is well equipped for managing patients with ILO, BPD and other comorbidities such as asthma, allergic rhinitis or reflux disease, providing medication management and advice as a non-medical prescriber. Nasal symptoms are rarely at the forefront of treatment considerations in asthma and other complex breathing conditions, but our “one airway” approach (treating nasal disease in a timely and appropriate manner) means patients achieve effective symptom control and can perform the ILO and BPD breathing exercises as taught by SLT and physiotherapy.
A major part of the CNS role is education for non-specialist staff (e.g. in other departments) and patients, providing explanations and reassurance about ILO, asthma and other conditions and helping patients differentiate between the different conditions. The CNS works closely with the severe asthma service in coordinating individual patient care. The CNS is an autonomous practitioner and is able to independently manage a complex caseload and support the rest of the MDT.
Pharmacist
Pharmacists are uniquely placed to optimise clinical outcomes in patients with airway disease. Their role involves educating patients on their disease state and in particular the role of inhaled medications. An essential part of their role in asthma is in providing inhaler technique training and addressing any concerns patients have about potential side-effects of medications, which can improve adherence to therapy. The pharmacist undertakes medication reviews focussed on improving adherence, optimising current medication, and escalating patients to biologic therapies, where appropriate. An assessment of response to inhaled therapies can lead to identification of symptoms that are not asthma related and may be linked to ILO or BPD. Asking patients about the symptoms they have that lead to use of short-acting β-agonist (SABA) inhalers or oral corticosteroids, and whether these treatments effectively suppress symptoms, may highlight that those symptoms are due to other causes. Such patients will then be discussed at the combined severe asthma/airways MDT meeting and referred on for assessment for ILO or BPD.
When conducting annual assessments of patients on high-cost biologic therapies the pharmacist can identify patients who are still receiving courses of oral corticosteroids for symptoms potentially related to ILO or BPD. The aim of the biologics is to reduce patient exposure to harmful oral corticosteroids. Referring these patients for assessment and therapy from the airways service can help them define which of their symptoms are asthma related. This can lead to a reduction in oral corticosteroid courses and overuse of SABA (a major contributor to environmental impact of respiratory treatments).
Likewise, patients with a diagnosis of ILO or BPD can benefit from a pharmacist review of asthma therapies. ILO and BPD can be driven by uncontrolled asthma. Improving inhaler technique and adherence to inhaled therapies or, if appropriate, escalating patients to severe asthma biologic therapy, can improve asthma control. Treating uncontrolled inflammation in the airways can lead to reduced ILO and BPD episodes. Ensuring the patient is on an inhaler that they can take correctly also reduces the risk of laryngeal irritation, which may drive ILO symptoms. In our pharmacist-led clinic, we have used smart inhaler monitors to improve adherence to inhalers, with subsequent resolution of ILO symptoms.
Clinical psychologist
Psychology entails the assessment, formulation and intervention for psychological distress (e.g. depression and anxiety). Clinical psychology within physical healthcare is important since individuals living with a chronic illness are two to three times more likely to develop depression and anxiety than those who are physically healthy, and there is also some suggestion that the experience of depression and/or anxiety is likely to be more persistent due to the chronic, and often fluctuating nature of physical illness [49]. Within respiratory services, clinical psychologists can contribute to improved treatment adherence, quality of life, general adjustment, and the development of effective coping strategies. The contributions of clinical psychology are essential and well documented for such teams [50].
Living with ILO and/or BPD can be a stressful experience and affect mental health. It is important and helpful for clinicians to validate and normalise the different emotions patients can experience. Clinical psychologists can work on an individual level with patients, enabling them to understand the triggers for their distress, evaluate their ways of coping with it (sometimes ways of coping can be unhelpful and inadvertently perpetuate distress), and learn better coping strategies to reduce distress. This is important as emotional distress can both trigger ILO attacks and perpetuate BPD. Clinical psychologists can work effectively when embedded within the MDT, informing discussions about the complexities patients can present with, and guiding the MDT through formulation and the evidence base in their approach and management of such complexity in order to improve patient outcomes.
Joint working
Often members of the MDT will complete joint assessment and treatment sessions which can be extremely effective in managing these complex disorders. Patients may commonly have both ILO and BPD occurring together [51], in these cases joint management from physiotherapy and SLT is appropriate to ensure they know which technique to use depending on the symptoms they are experiencing. Patients typically undergo an average of three SLT and/or physiotherapy sessions. It can also be helpful for clinical psychologists to work alongside other disciplines (e.g. joint physiotherapy and clinical psychology clinics to address poor breathing patterns in part sustained by anxiety), which can be more efficient and accessible for patients, compared with individual interventions. Psychology sessions initially consist of three assessment sessions before a block of therapy is booked or patients are referred on to other services, i.e. local mental health services or more specialist services (e.g. for grief/ trauma therapy).
Evolution of the service
Our airways service has continually evolved to meet the needs of patients and referrers and offer improved treatments for ILO and BPD. It was initially set up in 2017 with a small team and has now expanded to accommodate 10 team members. The service receives ∼800 referrals a year with over half of these being diagnosed with ILO and/or BPD. Prior to 2017, patients with ILO had to be referred to external services to receive SLT and psychology provision. Once the service was established in Manchester the referral numbers grew quickly and changes had to be made to accommodate the growing numbers. The MDT clinics were established and triage/referral pathways giving clear guidance on appropriate patients to accept. Close relationships were built with the north-west MDT networks to allow discussion prior to referral and ensure appropriate timing and patient provision.
Training and leadership
Several of the MDT members in our service are leaders in the field of ILO, BPD and severe asthma, sitting on national and international committees and being involved in the writing of guidelines and policies including for the National Institute for Health and Care Excellence (NICE), British Thoracic Society (BTS), Royal College of Speech and Language Therapists (RCSLT), the Association of Chartered Physiotherapists in Respiratory Care (ACPRC) and the Association of Respiratory Nurse Specialists (ARNS).
We have close links with the University of Manchester and Manchester Metropolitan University and regularly host students from all MDT disciplines. Several MDT members teach on the undergraduate and masters level courses and provide regular training locally and externally to the range of MDT professions.
Challenges
The service we have built requires patients to attend for a full day case assessment. This approach does not suit all patients with complex breathlessness and adaption of some appointments are required to meet patient needs. Resources and staffing numbers are a challenge to implementing and continually improving our multidisciplinary service, especially as UK National Health Service services have been on block contracts for the past few years and there have been competing demands on the speciality area due to being involved in a global pandemic (coronavirus disease 2019), which caused increasing waiting times and restrictions on the service. However, improved patient-reported outcomes, reduced hospitalisations, reduced medication use and improved quality of life show the benefits of the airways service and MDT working, and support the continuous investment in this service.
Research
Manchester airways service is one of the centres for airways research in the UK and has several research projects ongoing, including collaborations with other respiratory centres in the north-west and regular publications in high impact journals. There are several features of ILO and BPD that we still do not fully understand (box 1) and we are hopeful that future research will help us understand these complex conditions further.
BOX 1 Future research questions in inducible laryngeal obstruction (ILO) and breathing pattern disorder (BPD)
• Randomised control trials for ILO and BPD to show the effectiveness of therapy.
• Refining diagnostic testing (computed tomography imaging/ultrasound of the larynx and diaphragm).
• Phenotyping ILO and BPD.
• Measuring the long-term impact of ILO and BPD from a patient and clinician perspective, particularly developing ILO and BPD specific patient-reported outcome measures.
Conclusion
We have described the multidisciplinary service we provide for patients with ILO and BPD, in which we provide individualised, patient centred treatment plans, addressing specific traits that are causing symptoms and impact. Further research is required on diagnosing and treating these complex conditions, especially more robust, prospective, randomised controlled trials on the efficacy of SLT and physiotherapy for ILO and BPD and those that capture the long-term impact of living with these conditions from a patient perspective. The success of the service is due to continued quality improvement, adaption to change and motivation to provide the best patient care. A multidisciplinary approach is integral to managing the complexity of ILO and BPD patients.
Acknowledgements
We would like to thank Charles Thomas Pantin, Claire Somerton, Lesley Moores and Jemma Haines for their support.
Footnotes
Conflict of interest: The authors declare that there are no conflicts of interest.
Support statement: S.J. Fowler is supported by the NIHR Manchester Biochemical Research Centre.
References
- 1.Hull J, Haines J, eds. Complex breathlessness (ERS Monograph). Sheffield, European Respiratory Society, 2022. DOI: 10.1183/2312508X.erm9722 [DOI] [Google Scholar]
- 2.Christopher KL, Wood RP, Eckert RC, et al. Vocal-cord dysfunction presenting as asthma. N Engl J Med 1983; 308: 1566–1570. doi: 10.1056/NEJM198306303082605 [DOI] [PubMed] [Google Scholar]
- 3.Vidotto L, de Carvalho C, Harvey A, et al. Dysfunctional breathing: what do we know? J Bras Pneumol 2019; 45: e20170347. doi: 10.1590/1806-3713/e20170347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haines J, Hull JH, Fowler SJ. Clinical presentation, assessment and management of inducible laryngeal obstruction. Curr Opin Otolaryngol Head Neck Surg 2018; 26: 174–179. doi: 10.1097/MOO.0000000000000452 [DOI] [PubMed] [Google Scholar]
- 5.Abdelwahab H, Aboelnass A, Ayman A, et al. Prevalence of inducible laryngeal obstruction among patients diagnosed as bronchial asthma. Adv Respir Med 2020; 88: 129–133. doi: 10.5603/ARM.2020.0087 [DOI] [PubMed] [Google Scholar]
- 6.Fukusho R, Ruanne L, Pyland D, et al. A multidisciplinary team clinic for vocal cord dysfunction reduced corticosteroid burst therapy. J Allergy Clin Immunol 2022; 10: 612–614. doi: 10.1016/j.jaip.2021.10.039 [DOI] [PubMed] [Google Scholar]
- 7.Halvorsen T, Walstead ES, Bucca C, et al. Inducible Laryngeal Obstruction: an official joint European Respiratory Society and European Laryngological Society statement. Eur Respir J 2017; 50: 1602221. doi: 10.1183/13993003.02221-2016 [DOI] [PubMed] [Google Scholar]
- 8.Petrov A. Vocal cord dysfunction: the spectrum across the ages. Immunol Allergy Clin North Am 2019; 29: 547–560. doi: 10.1016/j.iac.2019.07.008 [DOI] [PubMed] [Google Scholar]
- 9.Hull JH, Backer V, Gibson PG, et al. Laryngeal dysfunction: assessment and management for the clinician. Am J Respir Crit Care Med 2016; 194: 9–11. doi: 10.1164/rccm.201601-0149ED [DOI] [PubMed] [Google Scholar]
- 10.Fowler SJ, Thurston A, Chesworth B, et al. The VCDQ: a questionnaire for symptom monitoring in vocal cord dysfunction. Clin Exp Allergy 2015; 45: 1406–1411. doi: 10.1111/cea.12550 [DOI] [PubMed] [Google Scholar]
- 11.Marcinow AM, Thompson J, Forrest LA, et al. Irritant-induced paradoxical vocal fold motion disorder: diagnosis and management. Otolaryngol Head Neck Surg 2015; 153: 996–1000. doi: 10.1177/0194599815600144 [DOI] [PubMed] [Google Scholar]
- 12.Anderson JA. Work-associated irritable larynx syndrome. Curr Opin Allergy Clin Immunol 2015; 15: 150–155. doi: 10.1097/ACI.0000000000000144 [DOI] [PubMed] [Google Scholar]
- 13.Leong P, Phyland D, Koh J, et al. Middle airway obstruction: phenotyping vocal cord dysfunction or inducible laryngeal obstruction. Lancet 2022; 10: 3–5. doi: 10.1016/S2213-2600(21)00501-4 [DOI] [PubMed] [Google Scholar]
- 14.Boulding R, Stacey R, Niven R, et al. Dysfunctional breathing: a review of the literature and proposal for classification. Eur Respir Rev 2016; 25: 287–294. doi: 10.1183/16000617.0088-2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Folgering H. The pathophysiology of hyperventilation syndrome. Monaldi Arch Chest Dis 1999; 54: 365–372. [PubMed] [Google Scholar]
- 16.Gardner WN. The pathophysiology of hyperventilation disorders. Chest 1996; 109: 516–534. doi: 10.1378/chest.109.2.516 [DOI] [PubMed] [Google Scholar]
- 17.Hornsveld H, Garssen B. The low specificity of the Hyperventilation Provocation Test. J Psychosom Res 1996; 41: 435–449. doi: 10.1016/S0022-3999(96)00195-X [DOI] [PubMed] [Google Scholar]
- 18.Rafferty GF, Saisch SG, Gardner WN. Relation of hypercapnic symptoms to rate of fall of end tidal PCO2 in normal subjects. Respir Med 1992; 86: 335–340. doi: 10.1016/S0954-6111(06)80033-8 [DOI] [PubMed] [Google Scholar]
- 19.Courtney R. Breathing training for dysfunctional breathing in asthma: taking a multidimensional approach. ERJ Open Res 2017; 3: 00065-2017. doi: 10.1183/23120541.00065-2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Grillo L, Russell A-M, Shannon H, et al. Physiotherapy assessment of breathing pattern disorder: a qualitative evaluation. BMJ Open Respir Res 2023; 10: 1136. doi: 10.1136/bmjresp-2022-001395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vertigan A, Kapela S, Gibson P. Chronic cough in vocal cord dysfunction: description of a clinical entity. Respir Med 2020; 168: 105990. doi: 10.1016/j.rmed.2020.105990 [DOI] [PubMed] [Google Scholar]
- 22.Thomas M, McKinley RK, Freeman E, et al. The prevalence of dysfunctional breathing in adults in the community with and without asthma. Primary Care Respir J 2005; 14: 78–82. doi: 10.1016/j.pcrj.2004.10.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bardin P, Rangaswamy J, Yo S. Managing co-morbid conditions in severe asthma. Med J Aust 2018; 209: 11–17. doi: 10.5694/mja18.00196 [DOI] [PubMed] [Google Scholar]
- 24.Grammatopoulou EP, Skordilis EK, Georgoudis G, et al. Hyperventilation in asthma: a validation study of the Nijmegen Questionnaire – NQ. J Asthma 2014; 51: 839–846. doi: 10.3109/02770903.2014.922190 [DOI] [PubMed] [Google Scholar]
- 25.Martínez-Moragón E, Perpiñá M, Belloch A, et al. Prevalence of hyperventilation syndrome in patients treated for asthma in a pulmonology clinic. Arch Bronconeumol 2005; 41: 267–271. doi: 10.1016/s1579-2129(06)60221-8 [DOI] [PubMed] [Google Scholar]
- 26.Heaney LG, Robinson DS. Severe asthma treatment: need for characterising patients. Lancet 2005; 365: 974–976. doi: 10.1016/S0140-6736(05)71087-4 [DOI] [PubMed] [Google Scholar]
- 27.Radhakrishna N, Tay TR, Hore-Lacy F, et al. Validated questionnaires heighten detection of difficult asthma comorbidities. J Asthma 2017; 54: 294–299. doi: 10.1080/02770903.2016.1212369 [DOI] [PubMed] [Google Scholar]
- 28.Kenn K, Balkissoon. Vocal cord dysfunction: what do we know? Eur Respir J 2011; 37: 194–200. doi: 10.1183/09031936.00192809 [DOI] [PubMed] [Google Scholar]
- 29.Spyridoulias A, Lillie S, Vyas A, et al. Detecting laryngopharyngeal reflux in patients with upper airways symptoms: symptoms, signs, or salivary pepsin? Respir Med 2015; 109: 963–969. doi: 10.1016/j.rmed.2015.05.019 [DOI] [PubMed] [Google Scholar]
- 30.Woolnough K, Blakey J, Pargeter N, et al. Acid suppression does not reduce symptoms for vocal cord dysfunction, where gastroesophageal reflux is a known trigger. Respirology 2013; 18: 553–554. doi: 10.1111/resp.12058 [DOI] [PubMed] [Google Scholar]
- 31.Molyneux ID, Morice AH. Airway reflux, cough and respiratory disease. Ther Adv Chronic Dis 2011; 2: 237–248. doi: 10.1177/2040622311406464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tidmarsh B, Marinho S, Haines J, et al. Differentiating throat symptoms in inducible laryngeal obstruction from anaphylaxis – information for patients and health care professionals. J Allergy Clin Immunol 2022; 10: 645–646. doi: 10.1016/j.jaip.2021.11.008 [DOI] [PubMed] [Google Scholar]
- 33.Gregson DE, Campbell S, Lillie S, et al. Psychological comorbidity in vocal cord dysfunction. Thorax 2011; 66. doi: 10.1136/thoraxjnl-2011-201054c.206 [DOI] [Google Scholar]
- 34.Haines J, Chua S, Smith J, et al. Triggers of breathlessness in inducible laryngeal obstruction and asthma. Clin Exp Allergy 2020; 50: 1230–1237. doi: 10.1111/cea.13715 [DOI] [PubMed] [Google Scholar]
- 35.Todd S, Walstead ES, Grillo L, et al. Novel assessment tool to detect breathing pattern disorder in patients with refractory asthma. Respirology 2017; 23: 284–290. doi: 10.1111/resp.13173 [DOI] [PubMed] [Google Scholar]
- 36.Schatz M, Meltzer EO, Nathan R, et al. Psychometric validation of the rhinitis control assessment test: a brief patient – completed instrument for validating rhinitis symptoms. Annal Allergy Asthma Immunol 2010; 104: 118–124. doi: 10.1016/j.anai.2009.11.063 [DOI] [PubMed] [Google Scholar]
- 37.Juniper EF, Svensson K, Mork AC, et al. Measurement properties and interpretation of three shortened versions of the asthma control questionnaire. Respir Med 2005; 99: 553558. doi: 10.1016/j.rmed.2004.10.008 [DOI] [PubMed] [Google Scholar]
- 38.Bestall JC, Paul EA, Garrod R, et al. Usefulness of the Medical Research Council (MRC) dyspnea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax 1999; 54: 581–586. doi: 10.1136/thx.54.7.581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lowe B, Decker O, Muller S, et al. Validation and standardisation of the Generalised Anxiety Disorder Screener (GAD-7) in the general population. Med Care 2008; 46: 266–274. doi: 10.1097/MLR.0b013e318160d093 [DOI] [PubMed] [Google Scholar]
- 40.Brooke L, Fisher F, Benedetti A, et al. PHQ-8 scores and estimation of depression prevalence. Lancet Public Health 2021; 11: e793. doi: 10.1016/S2468-2667(21)00229-2 [DOI] [PubMed] [Google Scholar]
- 41.Williams MT, Lewthwaite H, Paquet C, et al. Dyspnea-12, and Multidimensional Dyspnea Profile: systematic review of use and properties. J Pain Symptom Manage 2021; 63: e75–e87. doi: 10.1016/j.jpainsymman.2021.06.023 [DOI] [PubMed] [Google Scholar]
- 42.Koh JH, Ruane LE, Phyland D, et al. Computed tomography imaging of the larynx for diagnosis of vocal cord dysfunction. NEJM Evid 2023; 2: EVIDoa2200183. doi: 10.1056/EVIDoa2200183 [DOI] [PubMed] [Google Scholar]
- 43.Wiltrakis SM, Gutierrez P. Use of POCUS in diagnosis of paradoxical vocal cord movement. Paediatr Emerg Care 2022; 38: e1085–e1086. doi: 10.1097/PEC.0000000000002662 [DOI] [PubMed] [Google Scholar]
- 44.Liyanagedara S, McLeod R, Elhassan H. Exercise induced laryngeal obstruction: a review of diagnosis and management. Eur Arch Otorhinolaryngol 2017; 274: 1781–1789. doi: 10.1007/s00405-016-4338-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lillie SF, Haines J, Vyas A, et al. Speech and language therapy by Skype™ for vocal cord dysfunction and chronic cough. Thorax 2014; 69: Suppl. 2, A126–A127. [Google Scholar]
- 46.Holmes LJ, Sheehan RL, Elsey L, et al. The Manchester multidisciplinary severe asthma day case assessment and its impact on patient care. Br J Hosp Med 2021; 2: 1–7. doi: 10.12968/hmed.2021.0142 [DOI] [PubMed] [Google Scholar]
- 47.Courtney R, van Dixhoorn J, Cohen M. Evaluation of breathing pattern: comparison of a Manual Assessment of Respiratory Motion (MARM) and respiratory induction plethysmography. Appl Psychophysiol Biofeedback 2008; 33: 91–100. doi: 10.1007/s10484-008-9052-3 [DOI] [PubMed] [Google Scholar]
- 48.Courtney R. A Multi-Dimensional Model of Dysfunctional Breathing and Integrative Breathing Therapy – Commentary on the functions of breathing and its dysfunctions and their relationship to breathing therapy. J Yoga Phys Ther 2016; 6: 257. doi: 10.4172/2157-7595.1000257 [DOI] [Google Scholar]
- 49.National Institute for Health and Care Excellence (NICE) . Depression in adults with a chronic physical health problem: recognition and management. Clinical guideline [CG91]. London, NICE, 2009. https://www.nice.org.uk/guidance/cg91 [PubMed] [Google Scholar]
- 50.NHS England . Specialised Respiratory Services (adult) – Severe Asthma. Date last updated: 25 May 2017. https://www.england.nhs.uk/wp-content/uploads/2017/04/specialised-respiratory-services-adult-severe-asthma.pdf
- 51.Selby J, Tidmarsh B, Bailey E, et al. Breathing pattern disorder is prevalent in patients with subjective symptoms of inducible laryngeal obstruction. Eur Respir J 2019; 54: Suppl. 63, PA4348. doi: 10.1183/13993003.congress-2019.PA4348 [DOI] [Google Scholar]