Abstract
Motor neurone disease/amyotrophic lateral sclerosis (ALS) is a progressive neurodegenerative disorder with no known cure, where death is usually secondary to progressive respiratory failure. Assisting people with ALS through their disease journey is complex and supported by clinics that provide comprehensive multidisciplinary care (MDC).
This review aims to apply both a respiratory and a complexity lens to the key roles and areas of practice within the MDC model in ALS. Models of noninvasive ventilation care, and considerations in the provision of palliative therapy, respiratory support, and speech and language therapy are discussed. The impact on people living with ALS of both inequitable funding models and the complexity of clinical care decisions are illustrated using case vignettes. Considerations of the impact of emerging antisense and gene modifying therapies on MDC challenges are also highlighted.
The review seeks to illustrate how MDC members contribute to collective decision-making in ALS, how the sum of the parts is greater than any individual care component or health professional, and that the MDC per se adds value to the person living with ALS. Through this approach we hope to support clinicians to navigate the space between what are minimum, guideline-driven, standards of care and what excellent, person-centred ALS care that fully embraces complexity could be.
Educational aims
To highlight the complexities surrounding respiratory care in ALS.
To alert clinicians to the risk that complexity of ALS care may modify the effectiveness of any specific, evidence-based therapy for ALS.
To describe the importance of person-centred care and shared decision-making in optimising care in ALS.
Tweetable abstract
Complexity is inherent in the care of a person living with ALS. Respiratory considerations and individual care components intertwine. Optimum management requires a person-centred, multidisciplinary, shared decision-making approach. https://bit.ly/44BufSP
Introduction
Motor neurone disease/amyotrophic lateral sclerosis (ALS) is a progressive neurodegenerative disorder with no known cure, where death is usually secondary to progressive respiratory weakness and failure. While disease progression is highly variable between individuals and across clinical phenotypes, comprehensive multidisciplinary care (MDC) is recommended in contemporary patient information and clinical practice recommendations [1, 2]. MDC is delivered in a centralised clinic that coordinates care across multiple specialties; typically including neurology, speech and language, physiotherapy, respiratory, social work, nursing, palliative, and community care/service delivery expertise, to comprehensively assess and collectively provide treatment to ALS patients and their families. Similarly, patient advocacy organisations, whether integrated into a MDC team or not, play a central role in supporting families through their ALS journey.
In 2015, Rooney et al. [3] provided clear evidence of a survival benefit from MDC versus community-based care supported by an ALS specialist care worker. The authors compared ALS care in the Republic of Ireland (centralised MDC) and Northern Ireland (devolved community-based care) using population-based ALS registries with full case ascertainment. The MDC per se improved the opportunity for patient access to a broad suite of therapies and services for the problems they were experiencing. However, the approximate 8-month survival advantage in those attending the centralised Irish MDC was not attributable to the provision of any single intervention or medication. The authors speculated that the MDC improved survival because the complex decision making inherent in MDC enriched the overall care plan for each individual. As such, the ALS MDC can be conceptualised as a complex healthcare intervention, rather than a linearly associated, collection of component care-elements that are each considered and delivered separately [4].
While MDC is a recommended standard of care in all contemporary ALS care guidelines [1, 5–7], not all ALS care model comparisons have demonstrated survival benefits. A Southern Italian, population-based comparison for example, failed to show any survival advantage of MDC versus general neurological clinic care [8]. However, very few patients underwent noninvasive ventilation (NIV) (only 2.5% uptake in both the MDC and general neurology) and percutaneous endoscopic gastrostomy (PEG) (6% in MDC and 2.5% in general neurology) compared with that shown previously [3], and the interventions were accessed late in the disease course. A more recent systematic review and meta-analysis has confirmed that patients who attended MDC experience an approximate 4.6-month survival benefit [9].
Complexity in healthcare has been characterised as “a dynamic and constantly emerging set of processes and objects that not only interact with each other, but come to be defined by those interactions” [4]. In the context of respiratory care of people with ALS in MDC, this complexity may be expressed as the decision to insert a gastrostomy and start NIV during the same hospital admission because, for example, the patient is from a rural area and has a primary carer who works. In this hypothetical (but familiar to those who work with ALS) clinical example, the NIV initiation timing was driven by an urgent need for safe feeding in the face of rapidly declining bulbar function and associated dysphagia, coupled with the complexity of distant location and carer availability. While the patient was keen to try NIV, they were asymptomatic at NIV initiation, received no subjective benefit from the NIV, and subsequently found adherence with therapy difficult. In this hypothetical case the person with ALS received little benefit from NIV despite the person being interested in the treatment and NIV having strong evidence of efficacy [10], because additional complexity resulted in NIV being introduced to them “too early” in the disease.
ALS care guidelines have been produced from Canada [5], the European Federation of Neurological Societies [6], the National Institute for Health and Care Excellence in the UK [1], and MND New Zealand [7]. Recent publications have listed the component elements of both a respiratory neuromuscular clinic and the impact of respiratory, enteral feeding and other support in ALS [2, 11–13]. Furthermore, the Quality Standards Committee of the American Academy of Neurology have published practice parameters to guide clinicians [14, 15]. Given the availability of these comprehensive care guidelines, the aim of this Breathe review is not to replicate these, but to apply both a respiratory and a complexity lens to the key roles and areas of practice within the MDC model in ALS. The review highlights areas of clinical care where multiple members of the MDC team contribute discrete knowledge to the collective decision-making process. Through this approach we hope to support clinicians to navigate the space between the minimum standards of care according to the guidelines, and what excellent care that fully embraces complexity and the needs of each individual attending the MDC might look like.
The diagnostic odyssey of ALS
Making the diagnosis
Early in the disease the diagnosis of ALS may be unclear, but as the disease evolves the clinical features of ALS become clearer; it moves through possible or probable to definite [16]. The neurologist's primary purpose is to make a sound diagnosis, based on the history and signs, having excluded other pathologies through appropriate investigations. Median life expectancy in ALS is 20–36 months from the onset of symptoms [17]. Studies from higher-income countries suggest that, on average, 12 months or more are spent in the diagnostic process [18]. In Ireland, where there is a well-established ALS clinic, patients waited on average 19.1 months from symptom onset for their first appointment at their MDC and spent 5.2 months under investigation by the neurologist before receiving their ALS diagnosis [19].
Patients often have insidious symptoms for weeks or months before seeing their general practitioner. Early symptoms of ALS may not be specifically neurological (e.g. fatigue, weight loss, dyspnoea), and may result in referral to non-neurological specialists or allied health disciplines for symptoms that are later found to have been hallmarks of early ALS. The onset of weakness (usually focal) is the accepted point of disease onset for clinical trials, but clearly the underlying pathology precedes this manifestation. Patterns of focal onset of weakness can be misinterpreted as more common conditions (e.g. focal neuropathies, spinal spondylosis, stroke) and/or these conditions may be comorbid in this patient population [20, 21].
These delays in diagnosis eat into the time left for patients and families to come to terms with the disease and postpones their access to the MDC [3, 22, 23]. Uncommon diseases like ALS need better public awareness if the general community and primary healthcare services are to be more alert to the early symptoms of ALS. The neurologist, hampered by the inherent uncertainty in diagnosing early ALS without sensitive and specific biomarkers, may recommend a period of observation or referral for a second opinion. Perhaps a better approach is to adopt a “working diagnosis” of ALS when clinical suspicion is high, and to give the patient the option of running both clinical surveillance and getting on with care planning and management in parallel. The literature emphasises that late initiation of NIV is associated with worse efficacy and outcomes [24]. The “working diagnosis” approach facilitates timely respiratory referral so that the process of discussing if and when to start NIV can begin. Since many patients are referred to multidisciplinary ALS clinics with possible or probable ALS, the neurologist on the team provides that important second opinion and maintains diagnostic surveillance. Data from ALS registries suggests that while diagnostic accuracy in ALS is high, around 7% of cases are subsequently re-diagnosed [25].
Giving the diagnosis
Much has already been written about the patient and family experiences of how and when the diagnosis of ALS is given, and the views of neurologists, who generally feel that this is the most difficult diagnosis to deliver [26, 27]. Best practice is characterised by ensuring there is time and an environment free of interruptions to deliver the diagnosis, that the patient has a support person with them, and that information is given in an empathic manner, at a pace that the patient can control. Doctors are encouraged to check in with the patient about their understanding and whether they wish to receive more information. An early follow-up appointment should be offered and scheduled.
The neurologist within the multidisciplinary team
Even when the diagnosis is sensitively delivered, the narrative of this disease, its hallmarks of uncertain aetiology, potential for genetic transmission, usually short and always fatal prognosis, and minimal disease-modifying treatment, are shocking. The neurologist is able to guide patients and families through the challenges and fear of informing themselves about ALS [28], helping them navigate the misinformation on the internet and to identify areas of priority for each individual based on their philosophy and the imperatives of likely patterns of disease progression [29]. The mainstay of therapy is MDC with a focus on quality of life, symptom management, improving survival where desired and psychosocial support for patients and families [1, 5]. This is ideally delivered by an integrated team through shared decision-making and a person-centred focus [30–32]. Medical care is typically provided by a neurologist, but palliative care physician, rehabilitation specialist or geriatrician medical care has been reported [33]. Working within such a team requires all team members to acquire additional skills; some are cross-disciplinary. For example, the neurologist learns palliative care skills and has an understanding of respiratory care in ALS; the palliative care physician acquires knowledge about neurological phenotypes and expertise in withdrawing ventilatory support at the end of life. Other skills have evolved to manage the complexities of ALS itself, such as a team-based approach to managing secretions where the evidence base is poor. Effective teams reflect on what needs improvement and are innovative [34].
NIV and models of care for the delivery of NIV
Supporting breathing overnight with NIV is an effective treatment to increase survival in ALS. A 2006 single-site, randomised controlled trial of NIV versus no-NIV demonstrated a modest overall survival benefit [35]. At least five single-site cohorts have also associated NIV use with increased survival in ALS [36–40], including a 20-year study from Australia, which demonstrated that NIV slows respiratory decline and improves survival by a median of 13 months [36]. This is at least four times more survival time than the 2–3 months from our best medication (riluzole [41]), and ∼140% increase on the overall median survival.
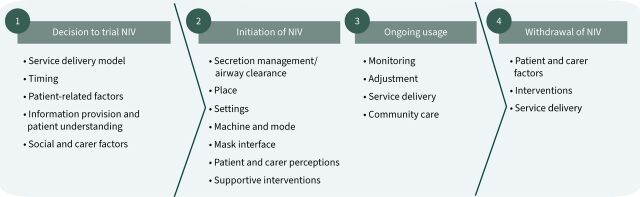
Recent articles have highlighted the challenges in providing excellent respiratory care for ALS in the USA [42]. While some of the identified issues are specific to the US healthcare system, the gaps in clinical research and structured, specific health professional training, a paucity of well-trained mentors, and little clarity on ventilation management beyond initiation are arguably universal complexities in ALS care. A recent narrative and thematic synthesis of the NIV in ALS pathway, coupled with a conceptual pathway, resulted in a process model that spans four stages: 1) the decision to trial, 2) initiation, 3) ongoing usage, and 4) withdrawal of NIV (figure 1) [24]. As is typically the case for complex adaptive systems in healthcare, the underlying evidence regarding NIV in ALS synthesised by Baxter et al. [24] was too heterogeneous for meta-analysis; instead, the authors presented a summary of factors associated with “optimal NIV” (table 1). This summary provides helpful pointers for respiratory care professionals, but these considerations could equally apply to many of the interventions provided by the MDC team, for example, timing and provision of gastrostomy, voice banking or discussion of voluntary assisted dying.
FIGURE 1.
Noninvasive ventilation (NIV) pathway model. Reproduced and modified from [24] with permission.
TABLE 1.
Summary of factors associated with optimal noninvasive ventilation (NIV) at different stages of the NIV pathway
| Stage | Optimising factors |
| Decision to trial NIV | Specialised units Joint respiratory palliative clinics Respiratory therapist / physiotherapist / nurse / scientist Recognition of limitations of symptom report to evaluate need Consideration of a suite of tests to assess respiratory insufficiency Early initiation Timely, ongoing decision-making Recognition that decision-making should be individualised Ensuring decision-making is active patient choice/patients are in control Emphasis on impact on quality of life rather than survival Ensure information provided is sufficient, consider need for education session Recognise potential for differing patient and family perceptions regarding the use of NIV, patient focus on present, family wish to plan for future Patients may require information at different times to carers Consider support systems required, reassurance regarding impact/burden on self and family |
| Initiation of NIV | Address excess secretions prior to initiation Supplementary use of assisted cough device Consider location of initiation: patients prefer home and this is less costly but varying evidence regarding success There is evidence regarding positive outcomes from outpatient rather than inpatient initiation Importance of optimising mask fitting, variety of interfaces, combine with mouthpiece interface for high usage Explore use of humidification Consider machine modes Recognise the importance of optimising settings Provide enhanced care for patients with bulbar symptoms |
| Ongoing NIV usage | Ensure regular monitoring of adequacy of ventilation Recognise the importance of analysing ventilator data Provide readjustment of pressure settings as required Consider telemonitoring; there is evidence that telemonitoring enables patient involvement, reduces time and cost |
| Withdrawal of NIV | Regularly review and re-discuss end of life wishes as part of the process Recognise the individual variation in decision-making Recognise that professionals find withdrawal challenging Provide opportunities for early discussion and holistic evaluation Consider use of medication to reduce symptoms, but provide support where professionals find this ethically challenging |
Reproduced and modified from [24] with permission.
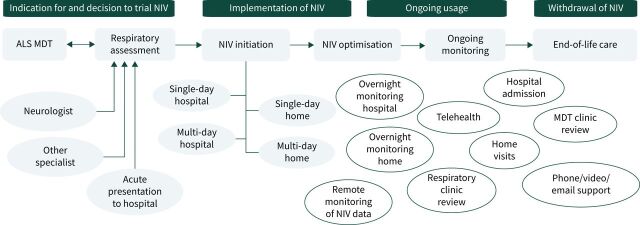
The initial referral for respiratory assessment and consideration of NIV typically comes from the specialist, neurology-led MDC clinics. However, several other pathways for referral may occur through private neurologists and respiratory physicians, or acute presentations to the emergency department (with or without a pre-existing diagnosis of ALS) (figure 2). Many MDC clinics have respiratory clinicians (doctors, physiotherapists, nurses) attending to facilitate regular review of patients with ALS, and/or to refer patients to a specialist respiratory service typically located at a major public hospital within the catchment of the referring MDC. Examples of the models of care that may be associated with stages of the NIV pathway are illustrated in figure 2. Criteria for timing of referral for NIV are broadly similar across guidelines, and guidelines similarly broadly recommend that respiratory assessments occur every 2–3 months.
FIGURE 2.
Examples of the models of care that may be associated with stages of the noninvasive ventilation (NIV) pathway. This figure illustrates the multiple entry points and models of care for respiratory assessment, NIV initiation/acclimatisation, optimisation, monitoring, and end-of-life care. ALS: amyotrophic lateral sclerosis; MDT: multidisciplinary team.
Individuals who are suitable for elective NIV commencement may attend a scheduled inpatient multi-day admission, attend an ambulatory day-admission outpatient visit or be set-up in their own home. The availability of these options for initiation are dependent on each respiratory service's model of care and the complexity of the patient's needs. While there is no consensus on the optimal place of NIV initiation, studies have demonstrated that outpatient initiation is as effective as inpatient initiation with reduced waiting times and improved management [43, 44] and similarly, that initiation of NIV at home is as effective as outpatient initiation with reduced carer burden [45, 46].
NIV initiation should be performed by a specialist respiratory health professional. The initial acclimatisation should be performed while the person is awake, with regular treatment commencing at night. Although optimal ventilator type, mode and settings are unclear, these and the choice of interface should be adjusted according to patient need, comfort and efficacy [47]. Therapy can be increased gradually depending on symptoms and comfort with the ultimate aim of achieving NIV use of >4 h per night [40]. Although current guidelines recommend monitoring every 2–3 months [1, 5–7], more regular monitoring in the days and weeks following initiation to identify issues and implement appropriate adjustments may promote adherence and effective ventilation [47]. The use of polysomnography to optimise NIV may have utility in improving patient–ventilator synchrony and adherence [48]; however, simple measurements of oximetry and evaluations of ventilator-recorded data may be sufficient [49].
Adding to the complexity of ALS care is the presence of a frontotemporal syndrome, which is found in 30–50% of ALS patients, with 10% reaching the diagnostic criteria for frontotemporal dementia [50, 51]. These cognitive and/or behavioural impairments are associated with a more rapid progression, poorer prognosis, and reduced survival [51]. Although limited, the available evidence has shown cognitive impairment is linked to reduced rates of acceptance and initiation of NIV and gastrostomy [52, 53], poorer adherence [54] and lower referral rates for these healthcare interventions [55].
The complex interplay of speech, communication, swallow, cough, nutritional support, hypermetabolism and respiratory care
Problems with speech, swallowing, airway protection and airway clearance commonly intertwine in people living with ALS (PlwALS). The coordination of more than 100 laryngeal, orofacial and respiratory muscles is required during speech production and swallowing [51]. Safe swallowing requires swallow and respiratory central pattern generators in the brainstem to interact, safeguarding the lower airway against aspiration as bolus material moves through the pharynx into the oesophagus [56]. Similarly, during respiration, pharyngeal, laryngeal and respiratory muscles act together to maintain patency of the upper airway and control airflow throughout the respiratory cycle, with upper airway activity preceding phrenic motor neurone output [57].
Speech and swallow
Deterioration in speech is rated as the most overwhelming aspect of ALS by PlwALS, superseding the loss of mobility, swallowing difficulties, and the awareness of a poor long-term prognosis [58]. In some cases, voice changes are the first symptom that prompts medical attention and diagnosis [59]. Up to 93% of individuals with bulbar disease experience dysarthria [59], with upper and lower motor neurone involvement leading to a mixed dysarthria of flaccid and spastic features over the course of disease progression [60].
Speech and respiration are tightly coupled: decreased phonatory function (e.g. hypo- or hyper-adduction of the vocal folds), insufficient breath support due to weak respiratory muscles, and/or decreased respiratory/phonatory control (difficulty coordinating speaking and breathing) all have adverse effects on speech production in ALS [61]. Initial changes typically include alterations to vocal quality, breathiness, roughness, hoarseness, strain and reduced loudness [62–67]. Weakening of the respiratory musculature in ALS is associated with frequent inspiration during speech, presenting clinically as longer and more frequent pause durations [68].
The current evidence base is limited in relation to the effectiveness of speech treatment in ALS. Historically, speech treatments aimed at increasing strength and mobility of the motor speech apparatus have been contraindicated. When natural speech becomes unintelligible, communication alternatives should be considered. Message banking or voice banking (a method of creating a synthetic copy of an individual's natural voice that can be used with speech generating devices) may offer options to maintain communication participation for PlwALS. However, banking needs to be completed prior to speech deterioration so that this technology can be integrated within augmentative and alternative communication devices once speech becomes unintelligible. If banking does not occur early in the disease process, it becomes unviable as a management strategy. The case vignette in table 2 illustrates how personal choices about the primacy of communication may take precedence over other treatment options in ALS. Please note that names of all case vignettes have been changed to protect the privacy of individuals.
TABLE 2.
Speech, communication and voice banking
| Case study 1: Jane, a 55-year-old female, diagnosed with spinal onset ALS 12 months ago; both PEG and NIV were previously declined |
| • Jane lives with her adult child in an apartment accessible by stairs (no wheelchair access). • Current level of function: severe upper and lower limb impairment, transfers via hoist, largely bed-bound, reports a decline in respiration with significant difficulty breathing (needs to be at an incline during the day and night). Jane is dependent on her child for activities of daily living including but not limited to: toileting, feeding, postural adjustments, and pressure care. Caring for Jane is having a notable impact on her child's psychosocial wellbeing (e.g. withdrawn, struggling to provide appropriate care, missing appointments). • Jane uses an eye-gaze system with banked voice to communicate; however, she can produce vocalisations. Voice banking was completed 6 months ago when she had a very mild flaccid dysarthria. • Initially, dysarthria was characterised by lingual weakness, reduced range and speed of lingual movement, reduced loudness, and mildly reduced sentence level intelligibility. At that time, over-articulation and increased loudness were successfully implemented as compensatory strategies to enhance functional communication. With disease progression, speaking became effortful and unintelligible to familiar communication partners, requiring the implementation of AAC (i.e. eye-gaze device with banked voice). Jane rates this technology as one of the most important interventions she has used during her disease course, and she remains determined to access and utilise it. |
PEG: percutaneous endoscopic gastrostomy; NIV: noninvasive ventilation; AAC: augmentative and alternative communication. Note that names of all case vignettes have been changed to protect the privacy of individuals.
Cough
Andersen et al. [69] recently published a detailed review of the complex laryngeal and respiratory coordination during a cough. Briefly, during the inspiratory phase, the laryngeal abductor muscles open the vocal cords and the diaphragm contracts, to inhale a large volume of air. During the compressive phase, the laryngeal adductors close the vocal cords and the expiratory muscles and diaphragm contract, to build intrathoracic pressure. The expiratory phase of a cough is marked by rapid vocal cord abduction in conjunction with contraction of the expiratory muscles, resulting in a short (30–50 ms) burst of supramaximal expiratory airflow [69]. Compared with healthy participants, PlwALS often have a prolonged inspiratory phase, reduced inspiratory and expiratory flow rates and slower cough “spikes” [70]. Many PlwALS may, over the course of the disease, benefit from techniques that improve cough effectiveness.
Recommended cough augmentation techniques include manual assisted cough (MAC), lung volume recruitment (LVR), also known as “breath-stacking”, or mechanical insufflation–exsufflation [1, 5, 15, 71–74]. Guidelines recommend techniques such as a MAC or LVR if PlwALS report difficulty clearing airway secretions [1, 5], however in clinical practice, the decision to implement cough augmentation techniques is often influenced by a broader assessment, including patient or carer report of ability to cough and clear secretions; volume and consistency of secretions; effort, fatigue or distress related to airway clearance; and incidence of respiratory tract infections or hospital admissions. Escalation to a mechanical insufflation–exsufflation device (MI-E), also known as a “cough assist machine”, may be appropriate if other techniques are not effective, if peak cough flow falls below 270 L·min−1, or during an acute respiratory tract infection [1, 5, 15]. However, titration of MI-E is not straightforward, especially in ALS. Collapse of the upper airway during both exsufflation [75, 76] and insufflation [76] has been observed in PlwALS, and individual customisation of all settings (i.e. not only pressure) can minimise this unwanted glottic closure [77].
The impact of introducing cough augmentation strategies into someone's daily routine requires thoughtful discussion with the PlwALS and their carer. A MAC may be difficult to perform if a gastrostomy is in situ, and typically requires external assistance (although the technique can be modified to self-cough [78]). PlwALS may lack the upper limb function to be able to perform LVR or MI-E independently and are likely to require physical assistance from a carer. Whilst manual techniques are low cost and readily accessible (e.g. approximate cost of LVR AUD 40), mechanical devices are considerably more expensive (approximately AUD 10 000) and access may be limited in some healthcare systems. Positive pressure therapy is not without risk, and cases of pneumothorax have been reported with LVR or MI-E [79–81]. Moreover, there are few prospective studies examining the longer-term benefit of performing cough augmentation on a regular basis, and therefore little published evidence that these techniques prevent respiratory tract infections or modify disease progression. Contrary to this state-of-science, many clinicians who are involved in the care of PlwALS recall cases where individuals attribute daily respiratory therapy to preventing hospital admissions or prolonging their life. This question of whether the benefit of the therapies outweighs the burden of using the therapies is illustrated in table 3.
TABLE 3.
Is the burden of respiratory therapy worth the benefit for the person living with ALS?
| Case study 2 | Case study 3 |
| Robert is a 75-year-old male, with limb onset ALS that was diagnosed 3 years ago. Referred to respiratory physiotherapist for assessment and consideration of strategies for airway clearance. | Ed, a 63-year-old male, with limb onset ALS that was diagnosed 2.5 years ago. No significant past medical history. |
|
Assessment • Conducted via telehealth, due to reduced mobility and difficulty attending clinic. • Lives at home with his wife (Matilda), who is his main carer. No external carers. • No purposeful upper limb movement; requires assistance for all PADLs. • Speech starting to slur and softer volume; saliva pools in back of mouth. • Difficulty swallowing liquids more than solids. Eating all food consistencies and has declined gastrostomy. • Denies symptoms of sleep disordered breathing and is open to trialling NIV for symptom relief when he feels the need. • Wakes with phlegm in back of throat. Difficult to clear: “is a noisy affair”. • Weak cough. • Current smoker (140 pack-years). • OSA (non-adherent with CPAP), BMI 35 kg·m−2. |
Assessment • Lives at home with wife (Sally), who continues to work part-time. NDIS participant. Paid in-home carers daily; funded hours are adequate. • No purposeful upper or lower limb movement; fully dependent for all PADLs. • Soft voice; uses voice amplifier. • Gastrostomy inserted ∼12 months ago. Most nutritional and hydration intake via PEG; small amount of oral intake for pleasure/QoL with acknowledged risk. • No pre-existing respiratory issues, but prior to ALS diagnosis, 1–2 chest infections a year that would take him >4 weeks to recover and be associated with sputum. • Recurrent chest infections since diagnosis (two hospital admissions in past 2 months). • On NIV for the past 12 months. Current usage is nocturnal, plus two daytime periods of 1–2 h. Total usage is 14 h per day. • Usually productive of thick clear sputum in mid-lower respiratory tract. Sputum can turn yellow. Weak cough and difficult to clear, but more effective clearance immediately after NIV session. • Reports feeling short of breath by the end of the day. • RFTs (4 months ago): FVC 3.07 L (67% predicted), SNIP 52 cmH2O (52%), MIP 50 cmH2O (49%), MEP 58 cmH2O (42%). |
|
Treatment • Discussed possible therapy options for improving airway clearance, including strategies to help loosen phlegm (bisolvon, nebulised saline, modifying diet to prevent aspiration), MAC, LVR and MI-E. • Robert keen to try bisolvon and nebulised saline. Reluctant to modify his diet or try thickeners, for him this would affect his QoL. • MAC and LVR would both require physical assistance from his wife, a petite 69-year-old woman, and as such deemed not able to be performed safely. Moreover, Matilda is already finding his care requirements to be at the upper limit of what she can continue to provide. They are about to commence in-home paid carers ∼2 h per day to assist. • Robert felt that MI-E was “not worth the bother”, as it would require a face-to-face appointment to titrate settings and provide carer education. Moreover, he did not feel comfortable with the possibility that he may become reliant on a machine to help him cough and did not think he would tolerate having a mask held onto his face (given past experience with CPAP and current lack of hand function). As Robert is over the age of 65 years, he is not eligible for NDIS funding and an application for ongoing rental cost for a MI-E device would need to be made to the local ALS association. Following a discussion of the potential benefits and the practicalities of MI-E, Robert expressed that his current routine for clearing phlegm “was manageable – and I don't want any heroics”. |
Initial treatment • Recommended to increase daytime NIV use (with humidification). Commenced on bisolvon and non-pharmacological strategies to reduce secretion thickness (pineapple juice, less dairy). Initiated LVR (regular use and as required to augment cough). Review after 1 month • After initial benefit with LVR, now feels exercises are too tiring/require too much active effort. • Using NIV ∼18 h per day. • RFTs: FVC 0.76 L (17%), SNIP 10 cmH2O (10%), MIP 10 cmH2O (10%), MEP 25 cmH2O (18%). • Commenced MI-E with three different programmes targeting: volume recruitment, airway clearance, cough augmentation. • Provided with escalation plan to increase MI-E use when experiencing the first signs of “chest infection” at home. Progress • Telehealth review 2 weeks after starting MI-E: clearing sputum in the morning easily, less coughing during the day and improved vocal loudness. • Ed's respiratory function declined quickly, and within 2 months he required NIV 24 h per day. • Ed continued living at home with his family for an additional 12 months, fully NIV dependent and with MI-E. Episodes of sputum plugging were mostly managed at home with MI-E, and Ed and Sally attributed the MI-E device with preventing at least three hospital admissions, and prolonging his life. |
ALS: motor neurone disease/amyotrophic lateral sclerosis; PADLs: personal activities of daily living; PEG: percutaneous endoscopic gastrostomy; QoL: quality of life; NIV: noninvasive ventilation; OSA: obstructive sleep apnoea; CPAP: continuous positive airway pressure; BMI: body mass index; MAC: manual assisted cough; LVR: lung volume recruitment; MI-E: mechanical insufflation–exsufflation; FVC: forced vital capacity; MIP: maximum inspiratory pressure; MEP: maximum expiratory pressure; NDIS: National Disability Insurance Scheme; RFTs: respiratory function tests; SNIP: sniff nasal inspiratory pressure. Note that names of all case vignettes have been changed to protect the privacy of individuals.
Secretion management
Secretion issues are reported by 40–60% PlwALS [82–85], and can be very difficult to manage, with approximately half of patients not optimally treated [84, 85]. An ineffective swallow and cough contribute to not being able to swallow or expectorate saliva, mucus or sputum effectively, and left untreated, excess secretions may contribute to poor tolerance of NIV [47, 86], and may increase the risk of aspiration pneumonia [87]. Differentiating contributing factors, the origin and consistency of secretions is recommended to provide optimal secretion management in PlwALS [84]. Clinically, secretions can be separated into: those from the nasal sinuses or nasopharynx (e.g. rhinosinusitis); saliva pooling in the oral cavity related to poor swallowing; thicker, stringy mucus in the oropharynx; or lower respiratory tract sputum. Whilst published ALS care guidelines and resources feature many secretion management options [88], the evidence base supporting their use is poor. A recent Cochrane review identified four secretion management randomised control trials in PlwALS, none of which included non-medical management [89].
Hypermetabolism and percutaneous endoscopic gastrostomy
Hypermetabolism is identified by having a resting energy expenditure that exceeds predicted resting energy requirements. Muscle mass accounts for 20–30% of resting energy requirements and is a major determinant of resting energy expenditure [90]. Therefore, observation of hypermetabolism in ALS [91–105] is paradoxical, as decreases in muscle mass in patients with ALS should contribute to decreases in resting energy expenditure. The impact of hypermetabolism in ALS is poorly understood. Hypermetabolism is proposed to contribute to weight loss, however, not all hypermetabolic patients with ALS experience weight loss [96, 97, 103]. Thus, hypermetabolism is suggested to only compound weight loss if patients experience deficits in appetite and/or impaired capacity to access food [93]. Indeed, weight loss, and more specifically, loss of fat mass suggesting negative energy balance is more prevalent in patients reporting loss of appetite [106]. Accordingly, hypermetabolism, independent of weight loss, has been shown to be a risk factor for faster disease progression and earlier death in ALS [97]. As measurement of metabolism is specialised, challenging and provides limited additional benefit, a practical approach to hypermetabolism in ALS is the regular monitoring of body weight and early referral to individualised dietary support where appropriate.
The complex interplay of how to manage speech and communication difficulties, ineffective cough, hypermetabolism, excess or difficult to manage oral and respiratory secretions, maintenance of nutritional support and effective NIV all come together in clinical decisions about emplacement of a PEG. PEG is a common intervention to ensure PlwALS have their nutrition and hydration needs met while maintaining a healthy weight [107] with the goal of prolonging survival [6]. Clinical management guidelines in ALS suggest PEG insertion should occur before forced vital capacity (FVC) falls below 50% of predicted normal value [6], as FVC of <50% predicted is associated with reduced survival post-PEG insertion [107]. However, there are several factors impacting the timely acceptance and use of PEG tube feeding. Reluctance to give up oral feeding, poor understanding of the benefits, and negative perceptions of gastrostomy have been identified by PlwALS and their informal carers as factors in the decision-making process [108]. Evaluation of quality of life (improved versus reduced), desire to prolong life, and acceptance of ALS and its progression also influence whether to have a PEG inserted or not [109]. Further, timing of PEG insertion is an example of where an effective MDC may anticipate future needs and therefore challenge those patients who prefer to live in the present. Accepting the wisdom of early gastrostomy insertion due to declining respiratory function, despite a preserved, normal swallow may retain the option for a PlwALS to prolong survival using ventilatory and nutritional support in the future.
Inequity in access and provision of care, due to discriminatory funding models: a complex challenge
The MDC for ALS may have variable levels of integration across primary (community), secondary and tertiary care. Ackrivo [42] has highlighted how funding models may impact on care in the USA, but many countries experience similarly complex funding-driven care gaps and inequities. “Different funding models create different financial incentives, which in turn lead to different services being offered and accessed. Quite simply, funding models can impact access to health care, and therefore health outcomes, in a substantial way.” [110].
In Australia for example, despite a strong public health system, there are age-related inequities in funding, meaning access to crucial respiratory equipment, care and support for PlwALS can vary substantially within the same country. Briefly, if you are diagnosed with ALS aged younger than 65 years, you are eligible for non-means-tested, federally funded National Disability Insurance Scheme (NDIS) support and equipment. This funding is not linked to the state-funded health system and thus the specialist clinical care is separated from the equipment provision. If you are older than 65 years and living in the community with ALS, you are only eligible for Commonwealth Home Support and MyAgedCare packages, which better cater for complex needs, but are means tested, capped in total available number and targeted to ageing not disability. Goods, Equipment and Assistive Technology funds are linked to each package amount, meaning equipment purchases can compromise care and support allocation. Additionally, PlwALS who move into residential aged care do not receive aged care packages if age 65 years and over, but if under 65 years they can still access the NDIS and have allied health professionals provide assessments and treatments. None of these schemes incorporate funding for “collaborative efforts” to bridge the inevitable gaps in eligibility and service provision and to provide person-centred care [111]. An illustration of how these funding inequities affect the lives of two Australian PlwALS is provided in table 4.
TABLE 4.
How inequity in care funding may impact noninvasive ventilation (NIV) provision: an example based on two people living with ALS in New South Wales, Australia
| Case study 4: lives with ALS in the community, age 55 years | Case study 5: lives with ALS in residential aged care, age 84 years |
| • Applies and receives a comprehensive NDIS plan to meet disability needs. | • Is not eligible for funding under the aged care system. |
| • Referred by a neurologist and assessed by a respiratory physician in the health system. | • Referred by a neurologist and assessed by a respiratory physician in the health system. |
| • Recommended to use NIV. | • Recommended to use NIV. |
| • Receives NDIS funding for disability health-related support to hire/purchase NIV devices, replacement masks and tubing. | • Funding to hire/purchase NIV through EnableNSW estimated to take many months: family decide to independently fund the purchase of NIV. |
| • Initiation of NIV occurs in hospital system. | • Initiation of NIV occurs in hospital system. |
| • No routine follow-up at home by hospital system, only seen at clinic (3-monthly reviews). | • No support or follow-up provided to PlwALS or nursing home staff from health system. PlwALS using NIV sporadically. |
| • Followed up by NDIS-funded physiotherapist in the home to ensure compliance and management. Regular physiotherapist follow-up funded by NDIS ensured correct mask fitting, and provided ongoing advice as condition deteriorated. | • Attended regional ALS MDC clinic. The MDC clinic has no capacity for in-person support in aged care setting. Information sent to residential care home, general practitioner and respiratory specialist informing them of poor NIV usage and encouraging greater use. |
ALS: motor neurone disease/amyotrophic lateral sclerosis; NDIS: National Disability Insurance Scheme; PlwALS: person living with ALS; EnableNSW: New South Wales state-based equipment provision scheme; MDC: multidisciplinary care.
Palliative care
Palliative care should be introduced at an early stage in PlwALS and be centred around needs rather than prognosis [112]. Palliative care provides a holistic approach to care for people with a serious illness [113], through careful enquiry of a person's physical, social and spiritual concerns. It also encompasses a patient's family and includes bereavement care [114]. An ability to document an advanced care plan [115], to explore how and where the PlwALS would like to be cared for and by whom, are essential aspects of a palliative approach to care. As with consideration of NIV [24], early referral to palliative care is recommended by specialist neurological societies and guidelines [1], and there is good evidence that early referral improves quality of life, can reduce symptom burden, minimises unwanted care at the end-of-life, and is cost effective [116–118]. The inclusion of palliative care as part of a multidisciplinary team caring for PlwALS is recommended [3, 21], and an illustration provided in table 5.
TABLE 5.
Palliative care: a story told through the eyes of a palliative care physician
| Case study 6 |
| Bill was a previously fit 70-year-old engineer, who lived at home with his wife of 40 years, Eileen. He had played rugby, still maintained fitness at the local gym, tinkered in his shed and flew his flight simulator at home. Bill's initial symptoms of ALS were subtle: a loss of dexterity with his tools in the shed and the joystick on his flight simulator. It took several months for a formal label of ALS to be provided. By this time, speech and swallow changes were emerging, along with a reduction in exercise intensity, but he still enjoyed the gym and good-natured banter with his friends. • On first review in the ALS clinic he was seen by the palliative care physician. He was adamant: “no treatment”, no riluzole, no PEG, no NIV. These proclamations were accepted, supported and explored without judgement. Discussions around goals of care were had; stories of travel and sport were shared. • Time passed. A visiting Portuguese clinician was his undoing: “It has always been on my wish list…I guess I will never get there”. Bill listened intently to our visiting clinician, her accent and the vivid descriptions of her country. • Bill's ALSFRS-R score [119] was falling; swallowing was becoming more difficult, weight loss was ensuing, his sleep was disturbed and he was no longer able to lie flat in bed without experiencing breathlessness. His goals of care were reviewed; things he was looking forward to were discussed and the activities he enjoyed encouraged. “Can you tell me about the PEG, Doc?” Sure. The discussion included concerns for respiratory function and a general anaesthetic, which resulted in an agreement to explore a sleep study with a view to commencing NIV. Both (previously unwanted) interventions occurred and were accepted with grace, an increase in weight and energy, and an abatement of the morning headaches. Life was back on track, still with clear limits of care in place. • Over the next several months, Bill's ability to care for himself faltered. He became unsteady on his feet, his speech became difficult to understand, the saliva excess was troubling despite medications trying to counter this and still enable a moist clean mouth. A delicate balance. • Just prior to Christmas during a planned ALS clinic review, he asked me “How many Temazepam do I have to take in order to kill myself?” An appropriate silence followed, my Registrar holding her breath. No time for a glib answer about his swallow, a sensitive conversation exploring his distress was required. He was in tears (exacerbated by his pseudo-bulbar affect) [120]. Checking in with his wife, it was the first she had heard of his thoughts and concerns, I was able to ensure there were no active plans for suicide. We discussed Christmas with the family, agreed for our community palliative care nurse to visit at home and to catch up just after Christmas. • Regular contact was made. I met Bill and his family at their home with one of our community palliative care nurses. Ongoing neck and shoulder pain owing to muscle weakness was causing significant distress. He did not enjoy the constipation caused by a Buprenorphine patch and could not be swayed to consider alternative aperients. Was this a degree of rigidity associated with frontotemporal dementia, or a justified fear of severe constipation in a man who was struggling to swallow, had reduced mobility, was short of breath with any effort and had minimal strength to sit upright? A variety of neck supports and collars failed to help but a combination of liquid paracetamol and non-steroidal anti-inflammatory drugs was effective. • The relentless loss of muscle strength resulted in progressive weakness, increased dependence, more time spent in bed, an inability to engage in family activities or go to the gym, and almost complete anarthria; this rapidly evolved over a 3-week period following Christmas. NIV use was increasing, and he asked how long it would take to die if he stopped his PEG feeds, which were his primary source of fluid and nutrition. He was not depressed. He was sad at leaving his family, he mourned the loss of ability to enjoy his sailing, and there was a cellar of red wine he would never get to enjoy. He did not want to die at home; he was concerned for his wife and family. Despite his marked weight loss, this former rugby player was still a large man, both physically and spiritually, and care needs at home were becoming harder for his family and carers. Bill asked to be admitted to the hospice for end-of-life care when the time came. The following plan was agreed: daily community nurse visits were arranged; he stopped his PEG feeds; he used NIV for comfort; and continued his analgesia regime. There was a steady stream of visitors. As Voluntary Assisted Dying was not legislated at this time, we discussed withdrawal of NIV with PST support [121] as an inpatient in the hospice. Our team checked in each day with Bill, his family, and carers, to ensure timely admission when a bed was available. • Bill was admitted to the hospice and spent a few days acquainting himself with the facility and the staff. He felt safe, secure and comfortable. Bill appointed the day to commence PST; his family were present, he bid his final farewells, thanked Eileen and staff for his care. Following a loading dose of midazolam and morphine, an infusion was maintained to ensure he was not rousable and remained comfortable, and NIV was removed. Bill died peacefully with his family present several hours after the removal of the NIV. His family assisted with after death care. As PST is an extraordinary event, routine debriefing sessions for the staff were held. The community palliative care team and family general practitioner ensured bereavement follow-up care were undertaken. |
ALS: motor neurone disease/amyotrophic lateral sclerosis; PEG: percutaneous endoscopic gastrostomy; NIV: noninvasive ventilation; ALSFRS-R: ALS Functional Rating Scale Revised; PST: palliative sedation therapy. Note that names of all case vignettes have been changed to protect the privacy of individuals.
ALS results in multiple losses and progressive deterioration [112], and a gentle exploration of the existential concerns that PlwALS may have is critical to spiritual care. Issues such as role, personhood, dignity, meaning and hope all add to the care of the person and their family. Understanding what and who are important to the individual helps to provide person directed care. For PlwALS, physical issues managed within palliative care may include pain, breathing, saliva management and bowel function. Pain can arise from pressure points, immobility, muscle cramps and spasticity, joint contractures and stiffness [122]. Attention to positioning, equipment, passive range of movement exercise and analgesia (ranging from paracetamol, non-steroidal anti-inflammatory drugs or opioids) may be required; the latter adding to the potential for constipation as a side-effect. Supportive feeding via a gastrostomy feeding tube or ventilatory support can provide symptom benefit, but only if these interventions are important to the individual. These issues always need to be reviewed and revisited, as goals and hopes change over time. ALS progresses with ongoing relentless loss, an accumulated myriad of symptoms, reduced mobility, increased NIV requirement [13, 121] and increased dependence for all care. Closer attention to end-of-life care needs should be sensitively addressed in a timely manner to anticipate what care may be required, including withdrawal of ventilation [123] and cessation of artificial feeding.
Future therapies will further increase complexity of care in ALS
Genotype-driven therapy trials, i.e. antisense oligonucleotide (ASO) therapies for specific pathogenic variant carriers, as well as increased understanding of the incidence of pathogenic variants in people with familial and sporadic disease, have led to the emergence of genetic counselling and testing as part of the MDC of PlwALS. Recent recommendations suggest all PlwALS should be offered diagnostic genetic testing [124, 125], and since April 2021, access to genetic counselling and testing is considered a fundamental right of PlwALS [126].
ASO therapies use ASOs to target mRNA and are emerging as a treatment option for several neurodegenerative diseases. One ASO therapy, nusinersen, has been approved on the pharmaceutical benefits scheme in Australia for use in spinal muscular atrophy, a mainly childhood-onset ALS [127]. Nusinersen prolonged life and improved motor function in infants with spinal muscular atrophy compared with those in the control group [128]. Some of the first children who were enrolled in the nusinersen trials are now on the cusp of teenagerhood and, like HIV/AIDS, this previously fatal disorder is gradually being transformed into a chronic disease. Perhaps like HIV/AIDS we need to prepare for a near future where we have an increasingly prevalent population of people living for longer with ALS, with further increases in complexity of care. Living with ALS for longer will continue to mandate the need for effective MDC teams that work collaboratively to enhance care.
Conclusion
Each PlwALS has a different personal journey, because each PlwALS has their own care preferences and ALS is characterised by heterogeneity in genotypes, phenotypes, symptomology and rate of change. While specific areas of practice such as the provision of riluzole and NIV have robust evidence of efficacy, the literature regarding when is the best time in an individual's ALS journey to deliver that therapy, relative to other combinations of therapies, is typically silent. These are the clinical care dilemmas that are best served by an effective and collaborative MDC. While clinical trials of novel ALS therapies will always be vital, we would suggest that an important scientific challenge in ALS care is to incorporate the complexity of PlwALS’ preferences and current best practice supportive care into evaluations of new therapeutics. Comprehensive, prospective collection of what interventions are delivered, to which person, at what point in their life with ALS are needed. This information will allow us to move beyond unidimensional clinical trials to better personalise each PlwALS' journey.
Key points
Multidisciplinary care in amyotrophic lateral sclerosis is a complex healthcare intervention.
Members of the multidisciplinary care team contribute discrete knowledge to the collective decision-making process, to assist people with amyotrophic lateral sclerosis through their disease journey within a person-centred model.
Interactions between individual care elements are complex: progressive respiratory impairment impacts other components of multidisciplinary care in amyotrophic lateral sclerosis and vice versa.
Self-evaluation questions
- If a person with ALS states that they do not want to consider using NIV at their first MDC appointment, clinicians should:
- Convince the patient to try NIV as there is strong evidence it is effective at improving quality of life and survival.
- Never mention NIV again as the patient doesn't want to use it.
- Provide care and support based on the patient's current wishes but remain open to revisiting NIV if the patient's needs and goals of care change over time.
- Refer the patient for NIV initiation if their respiratory function declines.
True or false: There is no benefit to patients being referred to an MDC clinic until a definitive diagnosis of ALS is made.
- Which of these statements is/are true:
- Because there is limited published evidence of cough augmentation techniques preventing respiratory infections, these therapies are not recommended for ALS patients.
- The impact of introducing cough augmentation strategies into someone's daily routine requires thoughtful discussion with the person living with ALS and their carer.
- Positive pressure therapy is safe and effective for all ALS patients.
- Recommended cough augmentation techniques for ALS include manual assisted cough, lung volume recruitment (LVR, or “breath-stacking”) or mechanical insufflation–exsufflation.
Suggested answers
c.
False.
b and d.
Footnotes
Conflict of interest: D.J. Berlowitz received no financial support for this work and reports no financial or personal conflicts of interest connected or unconnected with this work. D.J. Berlowitz has previously received competitive grant funding from Motor Neurone Disease Research Australia and the Medical Research Future Fund for unconnected work. S. Mathers received no financial support for this work and reports no financial or personal conflicts of interest connected or unconnected with this work. S. Mathers has previously received competitive grant funding from Motor Neurone Disease Research Australia, Fight MND and NHMRC for unconnected work. K. Hutchinson received no financial support for this work and reports no financial or personal conflicts of interest connected or unconnected with this work. A. Hogden received no financial support for this work and reports no financial or personal conflicts of interest connected or unconnected with this work. K.A. Carey received no financial support for this work and reports no financial or personal conflicts of interest connected or unconnected with this work. M. Graco received no financial support for this work and reports no financial or personal conflicts of interest connected or unconnected with this work. M. Graco has previously received competitive grant funding from Motor Neurone Disease Research Australia (MND Research Post-Doctoral Fellowship). B-M. Whelan received no financial support for this work and reports no financial or personal conflicts of interest connected or unconnected with this work. B-M. Whelan has previously received competitive grant funding from Motor Neurone Disease Research Australia for unconnected work (project grant funding). S. Charania received no financial support for this work and reports no financial or personal conflicts of interest connected or unconnected with this work. S. Charania has previously received a competitive scholarship from The Prince Charles Hospital for unconnected work (PhD funding in the area of Motor Neurone Disease). F. Steyn received no financial support for this work and reports no financial or personal conflicts of interest connected or unconnected with this work. F. Steyn has previously received competitive grant funding for unconnected work (project grant funding). This includes industry-funding for preclinical testing of compounds for the treatment of ALS. P. Allcroft received no financial support for this work and reports no financial or personal conflicts of interest connected or unconnected with this work. A. Crook received no financial support for this work and reports no financial or personal conflicts of interest connected or unconnected with this work. A. Crook has previously received competitive grant funding from Motor Neurone Disease Research Australia and the University of Technology Sydney for unconnected work (project funding and funding towards conference attendance). N.L. Sheers received no financial support for this work and reports no financial or personal conflicts of interest connected or unconnected with this work. N.L. Sheers has previously received competitive grant funding from Motor Neurone Disease Research Australia for unconnected work (project grant funding and funding towards conference attendance).
References
- 1.National Institute for Health and Care Excellence . Motor neurone disease: assessment and management. NICE guideline NG42. Date last updated: 23 July 2019. https://www.nice.org.uk/guidance/ng42 [PubMed]
- 2.Rimmer KP, Kaminska M, Nonoyama M, et al. Home mechanical ventilation for patients with amyotrophic lateral sclerosis: a Canadian Thoracic Society clinical practice guideline. Can J Respir Crit Care Sleep Med 2019; 3: 9–27. [Google Scholar]
- 3.Rooney J, Byrne S, Heverin M, et al. A multidisciplinary clinic approach improves survival in ALS: a comparative study of ALS in Ireland and Northern Ireland. J Neurol Neurosurg Psychiatry 2015; 86: 496–501. doi: 10.1136/jnnp-2014-309601 [DOI] [PubMed] [Google Scholar]
- 4.Greenhalgh T, Papoutsi C. Studying complexity in health services research: desperately seeking an overdue paradigm shift. BMC Med 2018; 16: 95. doi: 10.1186/s12916-018-1089-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shoesmith C, Abrahao A, Benstead T, et al. Canadian best practice recommendations for the management of amyotrophic lateral sclerosis. CMAJ 2020; 192: E1453–E1468. doi: 10.1503/cmaj.191721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The EFNS Task Force on Diagnosis and Management of Amyotrophic Lateral Sclerosis , Andersen PM, Abrahams S, et al. EFNS guidelines on the clinical management of amyotrophic lateral sclerosis (MALS) – revised report of an EFNS task force. Eur J Neurol 2012; 19: 360–375. Doi: 10.1111/j.1468-1331.2011.03501.x [DOI] [PubMed] [Google Scholar]
- 7.MND New Zealand . New Zealand Best Practice Recommendations for the Care of People with Motor Neurone Disease. Auckland, MND New Zealand, 2022. https://mnd.org.nz/wp-content/uploads/2022/11/NZ-Best-Practice-Recommendations-For-The-Care-Of-People-With-MND-issue-1-November-2022-FINAL.pdf [Google Scholar]
- 8.Zoccolella S, Beghi E, Palagano G, et al. ALS multidisciplinary clinic and survival: results from a population-based study in Southern Italy. J Neurol 2007; 254: 1107–1112. doi: 10.1007/s00415-006-0401-y [DOI] [PubMed] [Google Scholar]
- 9.de Almeida FEO, do Carmo Santana AK, de Carvalho FO. Multidisciplinary care in amyotrophic lateral sclerosis: a systematic review and meta-analysis. Neurol Sci 2021; 42: 911–923. doi: 10.1007/s10072-020-05011-2 [DOI] [PubMed] [Google Scholar]
- 10.Berlowitz DJ, Sheers N. Not only about the drugs: improved survival with noninvasive ventilation in amyotrophic lateral sclerosis. Ann Am Thorac Soc 2021; 18: 419–420. doi: 10.1513/AnnalsATS.202011-1404ED [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shah NM, Murphy PB, Kaltsakas G. The adult multidisciplinary respiratory neuromuscular clinic. Breathe 2020; 16: 200121. doi: 10.1183/20734735.0121-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Institute for Health and Clinical Excellence (NICE) . Motor neurone disease: the use of non-invasive ventilation in the management of motor neurone disease. London, National Institute for Health and Clinical Excellence (NICE), 2010. [PubMed] [Google Scholar]
- 13.Dorst J, Ludolph AC. Non-invasive ventilation in amyotrophic lateral sclerosis. Ther Adv Neurol Disord 2019; 12: 1756286419857040. doi: 10.1177/1756286419857040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Miller RG, Jackson CE, Kasarskis EJ, et al. Practice parameter update: the care of the patient with amyotrophic lateral sclerosis: multidisciplinary care, symptom management, and cognitive/behavioral impairment (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2009; 73: 1227–1233. doi: 10.1212/WNL.0b013e3181bc01a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Miller RG, Jackson CE, Kasarskis EJ, et al. Practice parameter update: the care of the patient with amyotrophic lateral sclerosis: drug, nutritional, and respiratory therapies (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 2009; 73: 1218–1226. doi: 10.1212/WNL.0b013e3181bc0141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van Es MA, Hardiman O, Chio A, et al. Amyotrophic lateral sclerosis. Lancet 2017; 390: 2084–2098. doi: 10.1016/S0140-6736(17)31287-4 [DOI] [PubMed] [Google Scholar]
- 17.Chiò A, Logroscino G, Hardiman O, et al. Prognostic factors in ALS: a critical review. Amyotroph Lateral Scler 2009; 10: 310–323. doi: 10.3109/17482960802566824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mitchell JD, Callagher P, Gardham J, et al. Timelines in the diagnostic evaluation of people with suspected amyotrophic lateral sclerosis (ALS)/motor neuron disease (MND) – a 20-year review: can we do better? Amyotroph Lateral Scler 2010; 11: 537–541. doi: 10.3109/17482968.2010.495158 [DOI] [PubMed] [Google Scholar]
- 19.Galvin M, Madden C, Maguire S, et al. Patient journey to a specialist amyotrophic lateral sclerosis multidisciplinary clinic: an exploratory study. BMC Health Serv Res 2015; 15: 571. doi: 10.1186/s12913-015-1229-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hardiman O, van den Berg LH, Kiernan MC. Clinical diagnosis and management of amyotrophic lateral sclerosis. Nat Rev Neurol 2011; 7: 639–649. doi: 10.1038/nrneurol.2011.153 [DOI] [PubMed] [Google Scholar]
- 21.Dharmadasa T, Henderson RD, Talman PS, et al. Motor neurone disease: progress and challenges. Med J Aust 2017; 206: 357–362. doi: 10.5694/mja16.01063 [DOI] [PubMed] [Google Scholar]
- 22.Traynor BJ, Alexander M, Corr B, et al. Effect of a multidisciplinary amyotrophic lateral sclerosis (ALS) clinic on ALS survival: a population based study, 1996–2000. J Neurol Neurosurg Psychiatry 2003; 74: 1258–1261. doi: 10.1136/jnnp.74.9.1258 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Van Den Berg JP, Kalmijn S, Veldink JH, et al. Multidisciplinary ALS care improves quality of life in patients with ALS. Neurology 2005; 65: 1264–1267. doi: 10.1212/01.wnl.0000180717.29273.12 [DOI] [PubMed] [Google Scholar]
- 24.Baxter SK, Johnson M, Clowes M, et al. Optimizing the noninvasive ventilation pathway for patients with amyotrophic lateral sclerosis/motor neuron disease: a systematic review. Amyotroph Lateral Scler Frontotemporal Degener 2019; 20: 461–472. doi: 10.1080/21678421.2019.1627372 [DOI] [PubMed] [Google Scholar]
- 25.Logroscino G, Traynor BJ, Hardiman O, et al. Descriptive epidemiology of amyotrophic lateral sclerosis: new evidence and unsolved issues. J Neurol Neurosurg Psychiatry 2008; 79: 6–11. doi: 10.1136/jnnp.2006.104828 [DOI] [PubMed] [Google Scholar]
- 26.Aoun SM, Breen LJ, Howting D, et al. Receiving the news of a diagnosis of motor neuron disease: what does it take to make it better? Amyotroph Lateral Scler Frontotemporal Degener 2016; 17: 168–178. doi: 10.3109/21678421.2015.1111907 [DOI] [PubMed] [Google Scholar]
- 27.Schellenberg KL, Schofield SJ, Fang S, et al. Breaking bad news in amyotrophic lateral sclerosis: the need for medical education. Amyotroph Lateral Scler Frontotemporal Degener 2014; 15: 47–54. doi: 10.3109/21678421.2013.843711 [DOI] [PubMed] [Google Scholar]
- 28.van Eenennaam RM, Koppenol LS, Kruithof WJ, et al. Discussing personalized prognosis empowers patients with amyotrophic lateral sclerosis to regain control over their future: a qualitative study. Brain Sci 2021; 11: 1597. doi: 10.3390/brainsci11121597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Talman P, Thi D, Vucic S, et al. Identification and outcomes of clinical phenotypes in amyotrophic lateral sclerosis/motor neuron disease: Australian National Motor Neuron Disease observational cohort. BMJ Open 2016; 6: e012054. doi: 10.1136/bmjopen-2016-012054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Paynter C, Cruice M, Mathers S, et al. Communication and cognitive impairments and health care decision making in MND: a narrative review. J Eval Clin Pract 2019; 25: 1182–1192. doi: 10.1111/jep.13219 [DOI] [PubMed] [Google Scholar]
- 31.Hogden A, Greenfield D, Nugus P, et al. Engaging in patient decision-making in multidisciplinary care for amyotrophic lateral sclerosis: the views of health professionals. Patient Prefer Adher 2012; 2012: 691–701. doi: 10.2147/PPA.S36759 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Hogden A, Greenfield D, Nugus P, et al. What influences patient decision-making in amyotrophic lateral sclerosis multidisciplinary care? A study of patient perspectives. Patient Prefer Adher 2012; 6: 829–838. doi: 10.2147/PPA.S37851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brennan F, Gardiner MD, Narasimhan M. The neuropalliative multidisciplinary team – members and their roles. In: Miyasaki JM, Kluger BM, eds. Neuropalliative Care, Part 1, Volume 190. Handbook of Clinical Neurology. Amsterdam, Elsevier Health Sciences, 2022; pp. 33–59. [DOI] [PubMed] [Google Scholar]
- 34.West MA, Markiewicz L. Effective team working in health care. In: Ferlie E, Montgomery K, Pedersen AR, eds. The Oxford Handbook of Health Care Management. Oxford, Oxford University Press, 2016; pp. 231–252. [Google Scholar]
- 35.Bourke SC, Tomlinson M, Williams TL, et al. Effects of non-invasive ventilation on survival and quality of life in patients with amyotrophic lateral sclerosis: a randomised controlled trial. Lancet Neurol 2006; 5: 140–147. doi: 10.1016/S1474-4422(05)70326-4 [DOI] [PubMed] [Google Scholar]
- 36.Berlowitz DJ, Howard ME, Fiore JF Jr, et al. Identifying who will benefit from non-invasive ventilation in amyotrophic lateral sclerosis/motor neurone disease in a clinical cohort. J Neurol Neurosurg Psychiatry 2016; 87: 280–286. doi: 10.1136/jnnp-2014-310055 [DOI] [PubMed] [Google Scholar]
- 37.Kleopa KA, Sherman M, Neal B, et al. Bipap improves survival and rate of pulmonary function decline in patients with ALS. J Neurol Sci 1999; 164: 82–88. doi: 10.1016/S0022-510X(99)00045-3 [DOI] [PubMed] [Google Scholar]
- 38.Aboussouan LS, Khan SU, Meeker DP, et al. Effect of noninvasive positive-pressure ventilation on survival in amyotrophic lateral sclerosis. Ann Intern Med 1997; 127: 450–453. doi: 10.7326/0003-4819-127-6-199709150-00006 [DOI] [PubMed] [Google Scholar]
- 39.Lo Coco D, Marchese S, Pesco MC, et al. Noninvasive positive-pressure ventilation in ALS: predictors of tolerance and survival. Neurology 2006; 67: 761–765. doi: 10.1212/01.wnl.0000227785.73714.64 [DOI] [PubMed] [Google Scholar]
- 40.Ackrivo J, Hsu JY, Hansen-Flaschen J, et al. Noninvasive ventilation use is associated with better survival in amyotrophic lateral sclerosis. Ann Am Thorac Soc 2021; 18: 486–494. doi: 10.1513/AnnalsATS.202002-169OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Miller RG, Mitchell JD, Moore DH. Riluzole for amyotrophic lateral sclerosis (ALS)/motor neuron disease (MND). Cochrane Database Syst Rev 2012; 3: CD001447. doi: 10.1002/14651858.CD001447.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ackrivo J. Pulmonary care for ALS: progress, gaps, and paths forward. Muscle Nerve 2023; 67: 341–353. doi: 10.1002/mus.27779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Sheers N, Berlowitz DJ, Rautela L, et al. Improved survival with an ambulatory model of non-invasive ventilation implementation in motor neuron disease. Amyotroph Lateral Scler Frontotemporal Degener 2014; 15: 180–184. doi: 10.3109/21678421.2014.881376 [DOI] [PubMed] [Google Scholar]
- 44.Bertella E, Banfi P, Paneroni M, et al. Early initiation of night-time NIV in an outpatient setting: a randomized non-inferiority study in ALS patients. Eur J Phys Rehabil Med 2017; 53: 892–899. doi: 10.23736/S1973-9087.17.04511-7 [DOI] [PubMed] [Google Scholar]
- 45.Nixon I, Popkiewicz F, Banerjee S, et al. Using a joint approach to non-invasive ventilation in motor neurone disease. Eur J Palliat Care 2015; 22: 182–184. [Google Scholar]
- 46.Volpato E, Ptacinsky L, Lax A, et al. Home-based adaptation to night-time non-invasive ventilation in patients with amyotrophic lateral sclerosis: a randomized controlled trial. J Clin Med 2022; 11: 3178. doi: 10.3390/jcm11113178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.O'Brien D, Stavroulakis T, Baxter S, et al. The optimisation of noninvasive ventilation in amyotrophic lateral sclerosis: a systematic review. Eur Respir J 2019; 54: 1900261. doi: 10.1183/13993003.00261-2019 [DOI] [PubMed] [Google Scholar]
- 48.Hannan LM, Rautela L, Berlowitz DJ, et al. Randomised controlled trial of polysomnographic titration of noninvasive ventilation. Eur Respir J 2019; 53: 1802118. doi: 10.1183/13993003.02118-2018. [DOI] [PubMed] [Google Scholar]
- 49.Janssens J-P, Borel J-C, Pépin J-L. Nocturnal monitoring of home non-invasive ventilation: the contribution of simple tools such as pulse oximetry, capnography, built-in ventilator software and autonomic markers of sleep fragmentation. Thorax 2011; 66: 438–445. doi: 10.1136/thx.2010.139782 [DOI] [PubMed] [Google Scholar]
- 50.Goldstein LH, Abrahams S. Changes in cognition and behaviour in amyotrophic lateral sclerosis: nature of impairment and implications for assessment. Lancet Neurol 2013; 12: 368–380. doi: 10.1016/S1474-4422(13)70026-7 [DOI] [PubMed] [Google Scholar]
- 51.Huynh W, Ahmed R, Mahoney CJ, et al. The impact of cognitive and behavioral impairment in amyotrophic lateral sclerosis. Expert Rev Neurother 2020; 20: 281–293. doi: 10.1080/14737175.2020.1727740 [DOI] [PubMed] [Google Scholar]
- 52.Govaarts R, Beeldman E, Kampelmacher MJ, et al. The frontotemporal syndrome of ALS is associated with poor survival. J Neurol 2016; 263: 2476–2483. doi: 10.1007/s00415-016-8290-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Martin NH, Landau S, Janssen A, et al. Psychological as well as illness factors influence acceptance of non-invasive ventilation (NIV) and gastrostomy in amyotrophic lateral sclerosis (ALS): a prospective population study. Amyotroph Lateral Scler Frontotemporal Degener 2014; 15: 376–387. doi: 10.3109/21678421.2014.886700 [DOI] [PubMed] [Google Scholar]
- 54.Olney RK, Murphy J, Forshew D, et al. The effects of executive and behavioral dysfunction on the course of ALS. Neurology 2005; 65: 1774–1777. doi: 10.1212/01.wnl.0000188759.87240.8b [DOI] [PubMed] [Google Scholar]
- 55.Tilanus TBM, Groothuis JT, Ten Broek-Pastoor JMC, et al. Respiratory assessment of ALS patients: a nationwide survey of current Dutch practice. J Neuromuscul Dis 2018; 5: 431–438. doi: 10.3233/JND-180302 [DOI] [PubMed] [Google Scholar]
- 56.Horton KK, Segers LS, Nuding SC, et al. Central respiration and mechanical ventilation in the gating of swallow with breathing. Front Physiol 2018; 9: 785. doi: 10.3389/fphys.2018.00785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pierce RJ, Worsnop CJ. Upper airway function and dysfunction in respiration. Clin Exp Pharmacol 1999; 26: 1–10. doi: 10.1046/j.1440-1681.1999.02988.x [DOI] [PubMed] [Google Scholar]
- 58.Hecht M, Hillemacher T, Grasel E, et al. Subjective experience and coping in ALS. Amyotroph Lateral Scler Other Motor Neuron Disord 2002; 3: 225–231. doi: 10.1080/146608202760839009 [DOI] [PubMed] [Google Scholar]
- 59.Chen A, Garrett CG. Otolaryngologic presentations of amyotrophic lateralsclerosis. Otolaryngol Head Neck Surg 2005; 132: 500–504. doi: 10.1016/j.otohns.2004.09.092 [DOI] [PubMed] [Google Scholar]
- 60.Tomik B, Guiloff RJ. Dysarthria in amyotrophic lateral sclerosis: a review. Amyotroph Lateral Scler 2010; 11: 4–15. doi: 10.3109/17482960802379004 [DOI] [PubMed] [Google Scholar]
- 61.Spencer KA, Yorkston KM, Duffy JR. Behavioral management of respiratory/phonatory dysfunction from dysarthria: a flowchart for guidance in clinical decision making. J Med Speech Lang Pathol 2003; 11: xxxix–lxi. [Google Scholar]
- 62.Robert D, Pouget J, Giovanni A, et al. Quantitative voice analysis in the assessment of bulbar involvement in amyotrophic lateral sclerosis. Acta Otolaryngol 1999; 119: 724–731. doi: 10.1080/00016489950180702 [DOI] [PubMed] [Google Scholar]
- 63.Strand EA, Ramig LO, Yorkston KM, et al. Differential phonatory characteristics of four women with amyotrophic lateral sclerosis. J Voice 1994; 8: 327–339. doi: 10.1016/S0892-1997(05)80281-4 [DOI] [PubMed] [Google Scholar]
- 64.McGuirt WF, Blalock D. The otolaryngologist's role in the diagnosis and treatment of amyotrophic lateral sclerosis. Laryngoscope 1980; 90: 1496–1501. doi: 10.1288/00005537-198012000-00016 [DOI] [PubMed] [Google Scholar]
- 65.Roth CR, Glaze LE, Goding GS Jr, et al. Spasmodic dysphonia symptoms as initial presentation of amyotrophic lateral sclerosis. J Voice 1996; 10: 362–367. doi: 10.1016/S0892-1997(96)80028-2 [DOI] [PubMed] [Google Scholar]
- 66.Watts CR, Vanryckeghem M. Laryngeal dysfunction in amyotrophic lateral sclerosis: a review and case report. BMC Ear Nose Throat Disord 2001; 1: 1. doi: 10.1186/1472-6815-1-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Tomik J, Wiatr M, Składzień J, et al. The evaluation of abnormal voice qualities in patients with amyotrophic lateral sclerosis. Neurodegener Dis 2015; 15: 225–232. doi: 10.1159/000381956 [DOI] [PubMed] [Google Scholar]
- 68.Green JR, Beukelman DR, Ball LJ. Algorithmic estimation of pauses in extended speech samples of dysarthric and typical speech. J Med Speech Lang Pathol 2004; 12: 149–154. [PMC free article] [PubMed] [Google Scholar]
- 69.Andersen TM, Hov B, Halvorsen T, et al. Upper airway assessment and responses during mechanically assisted cough. Respir Care 2021; 66: 1196–1213. doi: 10.4187/respcare.08960 [DOI] [PubMed] [Google Scholar]
- 70.Tabor-Gray L, Vasilopoulos T, Plowman EK. Differences in voluntary and reflexive cough strength in individuals with amyotrophic lateral sclerosis and healthy adults. Muscle Nerve 2020; 62: 597–600. doi: 10.1002/mus.27040 [DOI] [PubMed] [Google Scholar]
- 71.Chatwin M, Toussaint M, Gonçalves MR, et al. Airway clearance techniques in neuromuscular disorders: a state of the art review. Respir Med 2018; 136: 98–110. doi: 10.1016/j.rmed.2018.01.012 [DOI] [PubMed] [Google Scholar]
- 72.Toussaint M, Chatwin M, Gonzales J, et al. 228th ENMC International Workshop: Airway clearance techniques in neuromuscular disorders; Naarden, The Netherlands, 3–5 March, 2017. Neuromuscul Disord 2018; 28: 289–298. doi: 10.1016/j.nmd.2017.10.008 [DOI] [PubMed] [Google Scholar]
- 73.Sheers N, Howard ME, Berlowitz DJ. Respiratory adjuncts to NIV in neuromuscular disease. Respirology 2019; 24: 512–520. doi: 10.1111/resp.13431 [DOI] [PubMed] [Google Scholar]
- 74.Morrow B, Argent A, Zampoli M, et al. Cough augmentation techniques for people with chronic neuromuscular disorders. Cochrane Database Syst Rev 2021; 4: CD013170. doi: 10.1002/14651858.CD013170.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Sancho J, Servera E, Diaz J, et al. Efficacy of mechanical insufflation-exsufflation in medically stable patients with amyotrophic lateral sclerosis. Chest 2004; 125: 1400–1405. doi: 10.1378/chest.125.4.1400 [DOI] [PubMed] [Google Scholar]
- 76.Andersen T, Sandnes A, Brekka AK, et al. Laryngeal response patterns influence the efficacy of mechanical assisted cough in amyotrophic lateral sclerosis. Thorax 2017; 72: 221. doi: 10.1136/thoraxjnl-2015-207555 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Andersen TM, Sandnes A, Fondenes O, et al. Laryngeal responses to mechanically assisted cough in progressing amyotrophic lateral sclerosis. Respir Care 2018; 63: 538–549. doi: 10.4187/respcare.05924 [DOI] [PubMed] [Google Scholar]
- 78.CANVENT . Patient Info: Manually Assisted Cough (MAC). Date last updated: 2016. www.ohri.ca/nivam/documents/MAC%20Patient%20info%20V1.2-1.pdf
- 79.McDonald LA, Berlowitz DJ, Howard ME, et al. Pneumothorax in neuromuscular disease associated with lung volume recruitment and mechanical insufflation-exsufflation. Respirol Case Rep 2019; 7: e00447. doi: 10.1002/rcr2.447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Suri P, Burns SP, Bach JR. Pneumothorax associated with mechanical insufflation–exsufflation and related factors. Am J Phys Med Rehabil 2008; 87: 951–955. doi: 10.1097/PHM.0b013e31817c181e [DOI] [PubMed] [Google Scholar]
- 81.Westermann EJA, Jans M, Gaytant MA, et al. Pneumothorax as a complication of lung volume recruitment. J Bras Pneumol 2013; 39: 382–386. doi: 10.1590/S1806-37132013000300017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Hadjikoutis S, Wiles CM, Eccles R. Coughing and choking in motor neuron disease. J Neurol Neurosurg Psychiatry 2000; 68: 601–604. doi: 10.1136/jnnp.68.5.601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.McGeachan AJ, McDermott CJ. Management of oral secretions in neurological disease. Pract Neurol 2017; 17: 96–103. doi: 10.1136/practneurol-2016-001515 [DOI] [PubMed] [Google Scholar]
- 84.Hobson EV, McGeachan A, Al-Chalabi A, et al. Management of sialorrhoea in motor neuron disease: a survey of current UK practice. Amyotroph Lateral Scler Frontotemporal Degener 2013; 14: 521–527. doi: 10.3109/21678421.2013.790452 [DOI] [PubMed] [Google Scholar]
- 85.Bradley WG, Anderson F, Bromberg M, et al. Current management of ALS. Neurology 2001; 57: 500. doi: 10.1212/WNL.57.3.500 [DOI] [PubMed] [Google Scholar]
- 86.Vandenberghe N, Vallet AE, Petitjean T, et al. Absence of airway secretion accumulation predicts tolerance of noninvasive ventilation in subjects with amyotrophic lateral sclerosis. Respir Care 2013; 58: 1424–1432. doi: 10.4187/respcare.02103 [DOI] [PubMed] [Google Scholar]
- 87.Kurian KM, Forbes RB, Colville S, et al. Cause of death and clinical grading criteria in a cohort of amyotrophic lateral sclerosis cases undergoing autopsy from the Scottish Motor Neurone Disease Register. J Neurol Neurosurg Psychiatry 2009; 80: 84–87. doi: 10.1136/jnnp.2008.149708 [DOI] [PubMed] [Google Scholar]
- 88.Motor Neurone Disease Association . Managing saliva problems in motor neurone disease. Date last updated: March 2023. https://www.mndassociation.org/sites/default/files/2023-03/P3%20Managing%20saliva%20problems.pdf
- 89.James E, Ellis C, Brassington R, et al. Treatment for sialorrhea (excessive saliva) in people with motor neuron disease/amyotrophic lateral sclerosis. Cochrane Database Syst Rev 2022; 5: CD006981. doi: 10.1002/14651858.CD006981.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Zurlo F, Larson K, Bogardus C, et al. Skeletal muscle metabolism is a major determinant of resting energy expenditure. J Clin Invest 1990; 86: 1423–1427. doi: 10.1172/JCI114857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Desport JC, Preux PM, Magy L, et al. Factors correlated with hypermetabolism in patients with amyotrophic lateral sclerosis. Am J Clin Nutr 2001; 74: 328–334. doi: 10.1093/ajcn/74.3.328 [DOI] [PubMed] [Google Scholar]
- 92.Desport JC, Torny F, Lacoste M, et al. Hypermetabolism in ALS: correlations with clinical and paraclinical parameters. Neurodegener Dis 2005; 2: 202–207. doi: 10.1159/000089626 [DOI] [PubMed] [Google Scholar]
- 93.Bouteloup C, Desport JC, Clavelou P, et al. Hypermetabolism in ALS patients: an early and persistent phenomenon. J Neurol 2009; 256: 1236–1242. doi: 10.1007/s00415-009-5100-z [DOI] [PubMed] [Google Scholar]
- 94.Funalot B, Desport JC, Sturtz F, et al. High metabolic level in patients with familial amyotrophic lateral sclerosis. Amyotroph Lateral Scler 2009; 10: 113–117. doi: 10.1080/17482960802295192 [DOI] [PubMed] [Google Scholar]
- 95.Vaisman N, Lusaus M, Nefussy B, et al. Do patients with amyotrophic lateral sclerosis (ALS) have increased energy needs? J Neurol Sci 2009; 279: 26–29. doi: 10.1016/j.jns.2008.12.027 [DOI] [PubMed] [Google Scholar]
- 96.Jesus P, Fayemendy P, Nicol M, et al. Hypermetabolism is a deleterious prognostic factor in patients with amyotrophic lateral sclerosis. Eur J Neurol 2018; 25: 97–104. doi: 10.1111/ene.13468 [DOI] [PubMed] [Google Scholar]
- 97.Steyn FJ, Ioannides ZA, van Eijk RPA, et al. Hypermetabolism in ALS is associated with greater functional decline and shorter survival. J Neurol Neurosurg Psychiatry 2018; 89: 1016–1023. doi: 10.1136/jnnp-2017-317887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Jesus P, Fayemendy P, Marin B, et al. Increased resting energy expenditure compared with predictive theoretical equations in amyotrophic lateral sclerosis. Nutrition 2020; 77: 110805. doi: 10.1016/j.nut.2020.110805 [DOI] [PubMed] [Google Scholar]
- 99.Ngo ST, Restuadi R, McCrae AF, et al. Progression and survival of patients with motor neuron disease relative to their fecal microbiota. Amyotroph Lateral Scler Frontotemporal Degener 2020; 21: 549–562. doi: 10.1080/21678421.2020.1772825 [DOI] [PubMed] [Google Scholar]
- 100.Fayemendy P, Marin B, Labrunie A, et al. Hypermetabolism is a reality in amyotrophic lateral sclerosis compared to healthy subjects. J Neurol Sci 2021; 420: 117257. doi: 10.1016/j.jns.2020.117257 [DOI] [PubMed] [Google Scholar]
- 101.Nakamura R, Kurihara M, Ogawa N, et al. Prognostic prediction by hypermetabolism varies depending on the nutritional status in early amyotrophic lateral sclerosis. Sci Rep 2021; 11: 17943. doi: 10.1038/s41598-021-97196-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Cattaneo M, Jesus P, Lizio A, et al. The hypometabolic state: a good predictor of a better prognosis in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry 2022; 93: 41–47. doi: 10.1136/jnnp-2021-326184 [DOI] [PubMed] [Google Scholar]
- 103.Chang J, Shaw TB, Holdom CJ, et al. Lower hypothalamic volume with lower body mass index is associated with shorter survival in patients with amyotrophic lateral sclerosis. Eur J Neurol 2023; 30: 57–68. doi: 10.1111/ene.15589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.He J, Fu J, Zhao W, et al. Hypermetabolism associated with worse prognosis of amyotrophic lateral sclerosis. J Neurol 2022; 269: 1447–1455. doi: 10.1007/s00415-021-10716-1 [DOI] [PubMed] [Google Scholar]
- 105.Nakamura R, Kurihara M, Ogawa N, et al. Investigation of the prognostic predictive value of serum lipid profiles in amyotrophic lateral sclerosis: roles of sex and hypermetabolism. Sci Rep 2022; 12: 1826. doi: 10.1038/s41598-022-05714-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Ngo ST, van Eijk RPA, Chachay V, et al. Loss of appetite is associated with a loss of weight and fat mass in patients with amyotrophic lateral sclerosis. Amyotroph Lateral Scler Frontotemporal Degener 2019; 20: 497–505. doi: 10.1080/21678421.2019.1621346 [DOI] [PubMed] [Google Scholar]
- 107.Bond L, Ganguly P, Khamankar N, et al. A comprehensive examination of percutaneous endoscopic gastrostomy and its association with amyotrophic lateral sclerosis patient outcomes. Brain Sci 2019; 9: 223. doi: 10.3390/brainsci9090223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Stavroulakis T, Walsh T, Shaw PJ, et al. Gastrostomy use in motor neurone disease (MND): a review, meta-analysis and survey of current practice. Amyotroph Lateral Scler Frontotemporal Degener 2013; 14: 96–104. doi: 10.3109/17482968.2012.723722 [DOI] [PubMed] [Google Scholar]
- 109.Martin NH, Lawrence V, Murray J, et al. Decision making about gastrostomy and noninvasive ventilation in amyotrophic lateral sclerosis. Qual Health Res 2016; 26: 1366–1381. doi: 10.1177/1049732315583661 [DOI] [PubMed] [Google Scholar]
- 110.Schroeder L, Cutler H. Changing invisible landscapes – financial reform of health and care systems: ten issues to consider. Int J Integr Care 2021; 21: 21. doi: 10.5334/ijic.6461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Green C, Malbon E, Carey G, et al. Competition and collaboration between service providers in the NDIS. Sydney, Centre for Social Impact, UNSW Sydney, 2018. https://www.csi.edu.au/research/competition-and-collaboration-between-service-providers-in-the-ndis/ [Google Scholar]
- 112.Oliver D, de Visser M, Voltz R. Editorial: palliative care in neurology. Front Neurol 2019; 10: 1370. doi: 10.3389/fneur.2019.01370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Fahrner-Scott K, Zapata C, O'Riordan DL, et al. Embedded palliative care for amyotrophic lateral sclerosis: a pilot program and lessons learned. Neurol Clin Pract 2022; 12: 68–75. doi: 10.1212/CPJ.0000000000001124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Aoun SM, Cafarella PA, Rumbold B, et al. Who cares for the bereaved? A national survey of family caregivers of people with motor neurone disease. Amyotroph Lateral Scler Frontotemporal Degener 2021; 22: 12–22. doi: 10.1080/21678421.2020.1813780 [DOI] [PubMed] [Google Scholar]
- 115.Seeber AA, Pols AJ, Hijdra A, et al. Advance care planning in progressive neurological diseases: lessons from ALS. BMC Palliat Care 2019; 18: 50. doi: 10.1186/s12904-019-0433-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med 2010; 363: 733. doi: 10.1056/NEJMoa1000678 [DOI] [PubMed] [Google Scholar]
- 117.Sahlen KG, Boman K, Brannstrom M. A cost-effectiveness study of person-centered integrated heart failure and palliative home care: based on a randomized controlled trial. Palliat Med 2016; 30: 296–302. doi: 10.1177/0269216315618544 [DOI] [PubMed] [Google Scholar]
- 118.Hoerger M, Perry LM, Greer JA, et al. Defining the elements of early palliative care that are associated with patient-reported outcomes and the delivery of end-of-life care. J Clin Oncol 2018; 36: 1096–1102. doi: 10.1200/JCO.2017.75.6676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Cedarbaum JM, Stambler N, Malta E, et al. The ALSFRS-R: a revised ALS functional rating scale that incorporates assessments of respiratory function. J Neurol Sci 1999; 169: 13–21. doi: 10.1016/S0022-510X(99)00210-5 [DOI] [PubMed] [Google Scholar]
- 120.Thakore NJ, Pioro EP. Laughter, crying and sadness in ALS. J Neurol Neurosurg Psychiatry 2017; 88: 825–831. doi: 10.1136/jnnp-2017-315622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Faull C, Rowe Haynes C, Oliver D. Issues for palliative medicine doctors surrounding the withdrawal of non-invasive ventilation at the request of a patient with motor neurone disease: a scoping study. BMJ Support Palliat Care 2014; 4: 43–49. doi: 10.1136/bmjspcare-2013-000470 [DOI] [PubMed] [Google Scholar]
- 122.Stephens HE, Lehman E, Raheja D, et al. Pain in amyotrophic lateral sclerosis: patient and physician perspectives and practices. Amyotroph Lateral Scler Frontotemporal Degener 2015; 17: 21–29. doi: 10.3109/21678421.2015.1074701 [DOI] [PubMed] [Google Scholar]
- 123.Phelps K, Regen E, Oliver D, et al. Withdrawal of ventilation at the patient's request in MND: a retrospective exploration of the ethical and legal issues that have arisen for doctors in the UK. BMJ Support Palliat Care 2017; 7: 189–196. doi: 10.1136/bmjspcare-2014-000826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Roggenbuck J, Fong JC. Genetic testing for amyotrophic lateral sclerosis and frontotemporal dementia: impact on clinical management. Clin Lab Med 2020; 40: 271–287. doi: 10.1016/j.cll.2020.05.002 [DOI] [PubMed] [Google Scholar]
- 125.Turner MR, Al-Chalabi A, Chio A, et al. Genetic screening in sporadic ALS and FTD. J Neurol Neurosurg Psychiatry 2017; 88: 1042–1044. doi: 10.1136/jnnp-2017-315995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.International Alliance of ALS/MND Associations . Fundamental rights for people living with ALS/MND. Date last updated: October 2022. www.als-mnd.org/support-for-pals-cals/pals-and-cals-rights/
- 127.Australian Prescriber . Nusinersen. Aust Prescr 2019; 42: 75–76. doi: 10.18773/austprescr.2019.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Finkel RS, Mercuri E, Darras BT, et al. Nusinersen versus sham control in infantile-onset spinal muscular atrophy. N Engl J Med 2017; 377: 1723–1732. doi: 10.1056/NEJMoa1702752 [DOI] [PubMed] [Google Scholar]