Abstract
Traumatic brain injury (TBI) is a major global health concern. Due to the increase in TBI incidence and the aging population, an increasing number of patients with TBI are taking antithrombotic agents for their underlying disease. When TBI occurs in patients with these diseases, there is a conflict between the disease, which requires an antithrombotic effect, and the neurosurgeon, who must minimize intracranial hemorrhage. Nevertheless, there are no clear guidelines for the reversal or resumption of antithrombotic agents when TBI occurs in patients taking antithrombotic agents. In this review article, we intend to classify antithrombotic agents and provide information on them. We also share previous studies on the reversal and resumption of antithrombotic agents in patients with TBI to help neurosurgeons in this dilemma.
Keywords: Traumatic brain injury, Antithrombotic agents, Anticoagulants, Antiplatelet agents
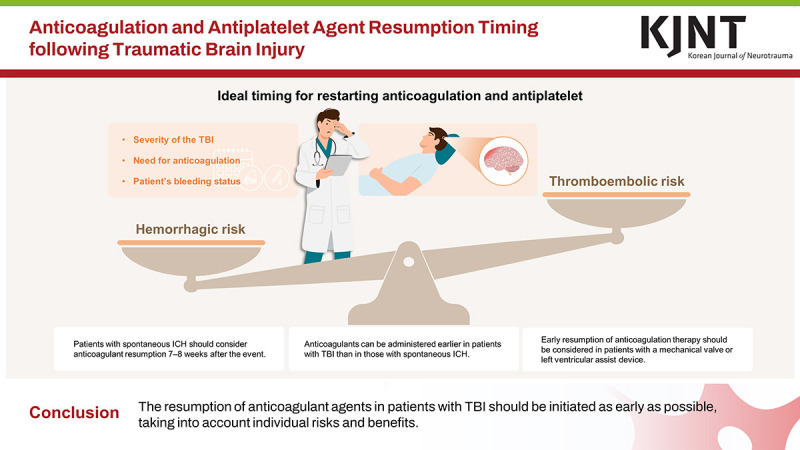
GRAPHICAL ABSTRACT
INTRODUCTION
Traumatic brain injury (TBI) is a major global health concern. TBI is a leading cause of mortality and disability and causes significant socioeconomic problems.19,37) Due to the increase in TBI incidence and the aging of the population, an increasing number of patients with TBI are taking antithrombotic agents for their underlying disease. Ischemic cerebrovascular disease, cardiovascular disease, and thromboembolic events are common causes for taking antithrombotic agents.24,26,29) When TBI occurs in patients with these diseases, there is a conflict between the diseases, which require an antithrombotic effect, and the neurosurgeon, who has to minimize intracranial hemorrhage. Nevertheless, there are no clear guidelines for the reversal or resumption of antithrombotic agents when TBI occurs in patients taking antithrombotic agents.
When TBI occurs in a patient taking an antithrombotic agent, there is a consensus that antithrombotic agents should be immediately discontinued and antidotes should be used. However, no guidelines or consensus have been established regarding the timing of antiplatelet and anticoagulant therapies. Therefore, through this review article, we aim to provide useful information to help patients with TBI and neurosurgeons who are experiencing dilemmas in making wise decisions.
CLASSIFICATION OF ANTITHROMBOTIC AGENTS
Antithrombotic agents are used to prevent and treat thrombosis. Antithrombotic agents are divided into three classes based on their mechanisms of action: antiplatelet drugs, anticoagulant agents, and fibrinolytic agents.
Antiplatelet drugs inhibit platelet activation and aggregation, important steps in blood clot formation. Antiplatelet agents can reduce the risk of thrombosis by preventing platelets from sticking together and forming clumps. The antiplatelet agents included aspirin, clopidogrel, prasugrel, and ticagrelor.
Anticoagulants activate antithrombin and accelerate the rate at which antithrombin inhibits clotting enzymes, particularly thrombin and factor Xa. Anticoagulants can help reduce the risk of thrombosis by slowing down or stopping the blood clotting process. Parenteral anticoagulants include heparin, low-molecular-weight heparin (LMWH), and fondaparinux. Currently available oral anticoagulants include vitamin K antagonists (warfarin) and direct oral anticoagulants such as dabigatran, rivaroxaban, apixaban, and edoxaban.
Fibrinolytic agents, including streptokinase, acylated plasminogen streptokinase activator complex (anistreplase), urokinase, and recombinant tissue-type plasminogen activator, also known as alteplase or activase, directly dissolve the existing thrombi. These agents are the preferred therapeutic regimens for the acute treatment of thrombosis in selected patients. Therefore, patients with TBI encountered in the emergency room rarely use these agents.11,28,38)
REVERSAL OF ANTITHROMBOTIC AGENTS
Antiplatelet drugs
To date, there are no clear guidelines for antithrombotic agent reversal when TBI occurs in patients taking antithrombotic agents. Instead, we can refer to the 2022 Guideline for the Management of Patients with Spontaneous Intracerebral Hemorrhage (ICH) from the American Heart Association/American Stroke Association (AHA/ASA).13) According to the guideline, platelet transfusion might be considered to reduce postoperative bleeding and mortality in patients with aspirin who require surgical intervention for ICH.18) However, in patients who do not require surgical intervention, platelet transfusions are potentially harmful and should not be administered.3) The effects of desmopressin on preventing hematoma expansion and prognosis are unclear.10,22,34)
Anticoagulants
According to the 2022 AHA/ASA guideline, in patients with anticoagulant-associated spontaneous ICH, anticoagulation should be discontinued immediately, and rapid reversal of anticoagulation should be performed as soon as possible.14)
For patients taking warfarin with an International Normalized Ratio (INR) ≥2.0, coagulation factor replacement is recommended to achieve rapid INR correction and prevent hematoma expansion. As a coagulation factor replacement, the four-factor prothrombin complex concentrate may be superior to the fresh-frozen plasma.36) Even in patients with an INR of 1.3 to 1.9, it may be reasonable to use prothrombin complex concentrate to achieve rapid correction of the INR and prevent hematoma expansion.9,14) In all patients taking warfarin, intravenous vitamin K should be administered directly after coagulation factor replacement to prevent a subsequent increase in INR.9,23,39)
In patients taking direct factor Xa inhibitors (rivaroxaban, apixaban, and edoxaban), andexanet alfa is reasonable to reverse the anticoagulant effect.7,8) In patients taking direct thrombin inhibitors (dabigatran), idarucizumab is reasonable to reverse the anticoagulant effect.31)
In patients receiving unfractionated heparin, intravenous protamine can reverse the anticoagulant effects. However, a previous study reported that protamine only partially reversed the anticoagulant effect in patients administered LMWH.35)
Anticoagulants and their reversal agents are summarized in TABLE 1.
TABLE 1. Antithrombotic agents and its reversal agents.
| Drug | Reversal agent | Dose | |
|---|---|---|---|
| Antiplatelet drugs | Aspirin, clopidogrel, cilostizol | Platelet | >3×109 platelet/L 1 U |
| Parenteral anticoagulants | Heparin | Protamine | 1 mg IV per 100 U of heparin over last 4 hours (maximum 50 mg) |
| Enoxaparin | Protamine | 1 mg IV per 1 mg of LMWH (maximum 50 mg) | |
| Oral anticoagulants | Warfarin | Vitamin K | 1–2 mg IV or PO 2.5–10 mg q 12 hours |
| FFP | Administer until corrected | ||
| PCC | 25 U/kg IV for INR 2–4, 35 U/kg IV for INR 4–6, 50 U/kg IV for INR >6 | ||
| Rivaroxaban | PCC | 50 IU/kg IV | |
| Andexanet alfa | 400–800 mg IV bolus, 480–960 mg infusion | ||
| Apixaban | PCC | 50 IU/kg IV | |
| Andexanet alfa | 400 mg IV bolus, 480 mg infusion | ||
| Edoxaban | PCC | 50 IU/kg IV | |
| Andexanet alfa | 800 mg IV bolus, 960 mg infusion | ||
| Dabigatran | Idarucizumab | 5g IV bolus |
FFP: fresh-frozen plasma, PCC: prothrombin complex concentrate, INR: international normalized rat.
RESUMPTION OF ANTITHROMBOTIC AGENTS
When TBI occurs in patients taking antithrombotic agents, the medication should be discontinued to prevent hematoma expansion. However, the optimal timing for initiating anticoagulation or antiplatelet therapy (APT) after TBI remains controversial. When anticoagulation should be restarted, several factors should be considered, including the severity of the TBI, the patient’s bleeding status, and the need for anticoagulation. Therefore, the attending physician must determine the timing of anticoagulant resumption by balancing the risk of hemorrhage recurrence that may occur with anticoagulant resumption with the benefit of preventing thromboembolic events, which is a difficult decision. We introduce several papers that may help neurosurgeons determine the timing of anticoagulant resumption (TABLE 2).
TABLE 2. Studies on resumption timing for anticoagulation or antiplatelet therapy.
| Study population | Suggested resumption timing | Authors | Year | |
|---|---|---|---|---|
| Parenteral anticoagulants (heparin or enoxaparin) | Traumatic intracerebral hemorrhage | Within 7 days of injury | Chipman et al.5) | 2020 |
| Traumatic intracerebral hemorrhage | 13 days after the injury. | Byrnes et al.4) | 2012 | |
| Oral anticoagulants (warfarin, rivaroxaban, apixaban, edoxaban, dabigatran) | Spontaneous intracranial hemorrhage | 10–30 weeks after hemorrhage | Majeed et al.20) | 2010 |
| Spontaneous intracranial hemorrhage | 6–8 weeks after hemorrhage | Moon et al.23) | 2022 | |
| Anticoagulant or antiplatelet | Spontaneous intracerebral hemorrhage | 7–8 weeks after hemorrhage | Pennlert et al.30) | 2017 |
| Traumatic brain injury | 7–9.5 days after injury | Puckett et al.32) | 2018 | |
| Traumatic subdural hemorrhage | Anticoagulant: 30 days after injury | Naylor et al.25) | 2021 | |
| Antiplatelet: 16 days after injury. |
Several large studies have reported the ideal timing for restarting warfarin after an intracranial hemorrhage. Majeed et al.20) conducted a retrospective multicenter cohort study to determine the optimal timing for anticoagulation resumption after warfarin-related intracranial hemorrhage. Among 234 patients with warfarin-associated intracranial hemorrhage, 177 who survived after 1 week were included in the study. The faster warfarin was restarted, the higher the hazard ratio for recurrent ICH. The slower the warfarin restart time, the higher the hazard ratio for ischemic stroke. Based on the combined risk, the authors argued that the optimal period of warfarin resumption was between 10 and 30 weeks after the initial ICH.20)
More recently, Pennlert et al.30) published a study of 2,619 ICH patients with ICH fibrillation who survived for more than 1 year. The authors found that anticoagulant resumption was associated with a reduced risk of vascular death and nonfatal stroke in high-risk patients, with no significantly increased risk of severe hemorrhage. They argued that anticoagulant treatment should be initiated 7–8 weeks after ICH, considering the risks and benefits.30)
However, since the two papers mentioned above included only spontaneous ICH in their study, the optimal timing they claim cannot be applied to patients with TBI. According to previous reports, anticoagulant resumption appears to be less strongly associated with ICH recurrence in patients with hemorrhagic stroke than in those with traumatic ICH. Nielsen et al.27) found that anticoagulant resumption was associated with ICH recurrence in patients with hemorrhagic stroke (adjusted hazard ratio [aHR], 1.31; 95% confidence intervals [CIs], 0.68–2.50), but no association was found between anticoagulant resumption and ICH recurrence in patients with traumatic ICH (aHR, 0.45; 95% CI, 0.26–0.76).27)
In the aforementioned studies, patients with traumatic ICH resumed anticoagulants earlier than 7–8 weeks, supporting their safety. Chipman et al.5) reported a retrospective, single-center study of 50 patients with traumatic ICH concomitant with pulmonary emboli. There was no significant difference in ICH expansion between patients who started anticoagulation therapy within 7 days of injury and those who started anticoagulation 7 days after injury. None of the patients required neurosurgical intervention due to ICH expansion.5)
Byrnes et al.4) reported on 42 patients with traumatic ICH who subsequently developed thrombotic complications. Twenty-six patients underwent therapeutic anticoagulation, an average of 13 days after the injury was started. ICH remained stable in almost all patients (25 of 26), and one patient had slightly increased bleeding, but no neurosurgical intervention was required.4)
In a multicenter prospective observational study, the EAST ACT-TBI Multicenter Study Group found that the early initiation of anticoagulants had a significant effect on the progression of traumatic brain injury. A total of 168 patients with TBI who received anticoagulation therapy before injury were classified into TBI progression and stable groups after the resumption of anticoagulation. The progression group restarted anticoagulation therapy significantly earlier than the stable group (4.5 days vs. 11.0 days, p=0.015).21)
Albrecht et al.2) reported a retrospective analysis of 10,782 patients with traumatic brain injuries who had received warfarin in the month before the injury. Warfarin resumption was associated with a decreased risk of thrombotic events (relative risk [RR], 0.77; 95% CI, 0.67–0.88) and an increased risk of hemorrhagic events (RR, 1.51; 95% CI, 1.29–1.78). The authors argued that there was a net benefit because warfarin resumption decreased the combined risk of hemorrhagic or ischemic stroke. (RR, 0.83; 95% CI, 0.72–0.96).2)
Nielsen et al.27) reported a study investigating the prognosis associated with the resumption of warfarin treatment in 1,325 hemorrhagic stroke patients with atrial fibrillation, and 1,090 traumatic ICH patients with atrial fibrillation. In patients with traumatic ICH, resumption of warfarin therapy is associated with a lower rate of ischemic stroke or systemic embolism. The resumption of therapy was associated with a significantly lower ICH recurrence rate. Of course, the finding that warfarin resumption lowers ICH recurrence is due to the failure to remove all confounding variables. However, warfarin resumption did not significantly increase ICH recurrence despite confounding.27)
In summary, the resumption of anticoagulant agents in patients with TBI should be initiated as early as possible, taking into account individual risks and benefits. Although there are reports that IVC filter insertion reduces the incidence and mortality of pulmonary embolism, its effectiveness remains controversial, and no significant effect has been demonstrated in deep vein thrombosis. Therefore, after the risk of hemorrhage is resolved, pharmacological prophylaxis should be actively considered.12,15,17,33)
In particular, early resumption of anticoagulation therapy should be considered in patients with a high risk of thromboembolic events due to a mechanical valve or left ventricular assist device.6,16,32)
According to previous studies, antiplatelet agents tend to resume earlier than anticoagulants in patients with intracranial hemorrhage. The effects of antiplatelet therapy after stroke due to intracerebral hemorrhage (REstart or STop Antithrombotics Randomized Trial, RESART), the first randomized controlled trial to ensure the safety of resumption of antiplatelet agents, compared 268 patients with ICH who restarted APT with 269 patients who avoided APT. They reported no difference in the recurrence rate of ICH or the incidence of major hemorrhagic events between the two groups. They argued that the benefits outweighed the risks of resuming APT. However, the optimal resumption timing was not presented in this study.1)
Puckett et al.32) reported a retrospective study to determine the optimal timing of the resumption of anticoagulation/antiplatelet therapy in 256 patients with TBI. They claimed that adverse events were minimized when therapy was restarted 7–9.5 days after injury.32)
Naylor et al.25) conducted a retrospective, single-center study of 456 patients with traumatic subdural hemorrhage. In this study, anticoagulation therapy was restarted on average 30 days after injury, and APT was restarted on average 16 days after injury. There was no significant difference in the evacuation rate owing to hematoma expansion between the resumption and control groups.25)
CONCLUSION
According to the AMA/ASA, patients with spontaneous ICH should consider anticoagulant resumption 7–8 weeks after the event. Considering the etiology of TBI, anticoagulants can be administered earlier in patients with TBI than in those with spontaneous ICH. After confirming that the hematoma has stabilized through a follow-up brain CT, anticoagulant treatment should be resumed, considering the individual risks and benefits.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
References
- 1.RESTART Collaboration. Effects of antiplatelet therapy after stroke due to intracerebral haemorrhage (RESTART): a randomised, open-label trial. Lancet. 2019;393:2613–2623. doi: 10.1016/S0140-6736(19)30840-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Albrecht JS, Liu X, Baumgarten M, Langenberg P, Rattinger GB, Smith GS, et al. Benefits and risks of anticoagulation resumption following traumatic brain injury. JAMA Intern Med. 2014;174:1244–1251. doi: 10.1001/jamainternmed.2014.2534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Baharoglu MI, Cordonnier C, Al-Shahi Salman R, de Gans K, Koopman MM, Brand A, et al. Platelet transfusion versus standard care after acute stroke due to spontaneous cerebral haemorrhage associated with antiplatelet therapy (PATCH): a randomised, open-label, phase 3 trial. Lancet. 2016;387:2605–2613. doi: 10.1016/S0140-6736(16)30392-0. [DOI] [PubMed] [Google Scholar]
- 4.Byrnes MC, Irwin E, Roach R, James M, Horst PK, Reicks P. Therapeutic anticoagulation can be safely accomplished in selected patients with traumatic intracranial hemorrhage. World J Emerg Surg. 2012;7:25. doi: 10.1186/1749-7922-7-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chipman AM, Radowsky J, Vesselinov R, Chow D, Schwartzbauer G, Tesoriero R, et al. Therapeutic anticoagulation in patients with traumatic brain injuries and pulmonary emboli. J Trauma Acute Care Surg. 2020;89:529–535. doi: 10.1097/TA.0000000000002805. [DOI] [PubMed] [Google Scholar]
- 6.Cho SM, Moazami N, Katz S, Starling R, Frontera JA. Reversal and resumption of antithrombotic therapy in lvad-associated intracranial hemorrhage. Ann Thorac Surg. 2019;108:52–58. doi: 10.1016/j.athoracsur.2019.01.016. [DOI] [PubMed] [Google Scholar]
- 7.Connolly SJ, Crowther M, Eikelboom JW, Gibson CM, Curnutte JT, Lawrence JH, et al. Full study report of andexanet alfa for bleeding associated with factor Xa inhibitors. N Engl J Med. 2019;380:1326–1335. doi: 10.1056/NEJMoa1814051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Demchuk AM, Yue P, Zotova E, Nakamya J, Xu L, Milling TJ, Jr, et al. Hemostatic efficacy and anti-FXa (factor Xa) reversal with andexanet alfa in intracranial hemorrhage: ANNEXA-4 substudy. Stroke. 2021;52:2096–2105. doi: 10.1161/STROKEAHA.120.030565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dentali F, Ageno W, Crowther M. Treatment of coumarin-associated coagulopathy: a systematic review and proposed treatment algorithms. J Thromb Haemost. 2006;4:1853–1863. doi: 10.1111/j.1538-7836.2006.01986.x. [DOI] [PubMed] [Google Scholar]
- 10.Feldman EA, Meola G, Zyck S, Miller CD, Krishnamurthy S, Cwikla GM, et al. Retrospective assessment of desmopressin effectiveness and safety in patients with antiplatelet-associated intracranial hemorrhage. Crit Care Med. 2019;47:1759–1765. doi: 10.1097/CCM.0000000000004021. [DOI] [PubMed] [Google Scholar]
- 11.Giakoumettis D, Vrachatis DA, Panagopoulos D, Loukina A, Tsitsinakis G, Apostolopoulou K, et al. Antithrombotics in intracerebral hemorrhage in the era of novel agents and antidotes: a review. J Popul Ther Clin Pharmacol. 2020;27:e1–ee18. doi: 10.15586/jptcp.v27i2.660. [DOI] [PubMed] [Google Scholar]
- 12.Gorman PH, Qadri SF, Rao-Patel A. Prophylactic inferior vena cava (IVC) filter placement may increase the relative risk of deep venous thrombosis after acute spinal cord injury. J Trauma. 2009;66:707–712. doi: 10.1097/TA.0b013e318188beba. [DOI] [PubMed] [Google Scholar]
- 13.Greenberg SM, Ziai WC, Cordonnier C, Dowlatshahi D, Francis B, Goldstein JN, et al. 2022 guideline for the management of patients with spontaneous intracerebral hemorrhage: a guideline from the American Heart Association/American Stroke Association. Stroke. 2022;53:e282–e361. doi: 10.1161/STR.0000000000000407. [DOI] [PubMed] [Google Scholar]
- 14.Hanger HC, Geddes JA, Wilkinson TJ, Lee M, Baker AE. Warfarin-related intracerebral haemorrhage: better outcomes when reversal includes prothrombin complex concentrates. Intern Med J. 2013;43:308–316. doi: 10.1111/imj.12034. [DOI] [PubMed] [Google Scholar]
- 15.Haut ER, Garcia LJ, Shihab HM, Brotman DJ, Stevens KA, Sharma R, et al. The effectiveness of prophylactic inferior vena cava filters in trauma patients: a systematic review and meta-analysis. JAMA Surg. 2014;149:194–202. doi: 10.1001/jamasurg.2013.3970. [DOI] [PubMed] [Google Scholar]
- 16.Kuramatsu JB, Sembill JA, Gerner ST, Sprügel MI, Hagen M, Roeder SS, et al. Management of therapeutic anticoagulation in patients with intracerebral haemorrhage and mechanical heart valves. Eur Heart J. 2018;39:1709–1723. doi: 10.1093/eurheartj/ehy056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ley EJ, Brown CV, Moore EE, Sava JA, Peck K, Ciesla DJ, et al. Updated guidelines to reduce venous thromboembolism in trauma patients: A Western Trauma Association critical decisions algorithm. J Trauma Acute Care Surg. 2020;89:971–981. doi: 10.1097/TA.0000000000002830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li X, Sun Z, Zhao W, Zhang J, Chen J, Li Y, et al. Effect of acetylsalicylic acid usage and platelet transfusion on postoperative hemorrhage and activities of daily living in patients with acute intracerebral hemorrhage. J Neurosurg. 2013;118:94–103. doi: 10.3171/2012.9.JNS112286. [DOI] [PubMed] [Google Scholar]
- 19.Maas AI, Stocchetti N, Bullock R. Moderate and severe traumatic brain injury in adults. Lancet Neurol. 2008;7:728–741. doi: 10.1016/S1474-4422(08)70164-9. [DOI] [PubMed] [Google Scholar]
- 20.Majeed A, Kim YK, Roberts RS, Holmström M, Schulman S. Optimal timing of resumption of warfarin after intracranial hemorrhage. Stroke. 2010;41:2860–2866. doi: 10.1161/STROKEAHA.110.593087. [DOI] [PubMed] [Google Scholar]
- 21.Matsushima K, Leichtle SW, Wild J, Young K, Chang G, Demetriades D, et al. Anticoagulation therapy in patients with traumatic brain injury: an Eastern Association for the Surgery of Trauma multicenter prospective study. Surgery. 2021;169:470–476. doi: 10.1016/j.surg.2020.07.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mengel A, Stefanou MI, Hadaschik KA, Wolf M, Stadler V, Poli K, et al. Early administration of desmopressin and platelet transfusion for reducing hematoma expansion in patients with acute antiplatelet therapy associated intracerebral hemorrhage. Crit Care Med. 2020;48:1009–1017. doi: 10.1097/CCM.0000000000004348. [DOI] [PubMed] [Google Scholar]
- 23.Moon JY, Bae GH, Jung J, Shin DH. Restarting anticoagulant therapy after intracranial hemorrhage in patients with atrial fibrillation: a nationwide retrospective cohort study. Int J Cardiol Heart Vasc. 2022;40:101037. doi: 10.1016/j.ijcha.2022.101037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics--2015 update: a report from the American Heart Association. Circulation. 2015;131:e29–ee322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 25.Naylor RM, Dodin RE, Henry KA, De La Peña NM, Jarvis TL, Labott JR, et al. Timing of restarting anticoagulation and antiplatelet therapies after traumatic subdural hematoma-a single institution experience. World Neurosurg. 2021;150:e203–e208. doi: 10.1016/j.wneu.2021.02.135. [DOI] [PubMed] [Google Scholar]
- 26.Ng IC, Barnes C, Biswas S, Wright D, Dagal A. When is it safe to resume anticoagulation in traumatic brain injury? Curr Opin Anaesthesiol. 2022;35:166–171. doi: 10.1097/ACO.0000000000001117. [DOI] [PubMed] [Google Scholar]
- 27.Nielsen PB, Larsen TB, Skjøth F, Lip GY. Outcomes associated with resuming warfarin treatment after hemorrhagic stroke or traumatic intracranial hemorrhage in patients with atrial fibrillation. JAMA Intern Med. 2017;177:563–570. doi: 10.1001/jamainternmed.2016.9369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nimjee SM, Crofton AR, Oh N, Kirsch W, Haglund MM, Grant GA. Youmans and winn neurological surgery. ed 8. Philadelphia, PA: Elsevier; 2022. Chapter 18: coagulation for the neurosurgeon. [Google Scholar]
- 29.Ovbiagele B, Goldstein LB, Higashida RT, Howard VJ, Johnston SC, Khavjou OA, et al. Forecasting the future of stroke in the United States: a policy statement from the American Heart Association and American Stroke Association. Stroke. 2013;44:2361–2375. doi: 10.1161/STR.0b013e31829734f2. [DOI] [PubMed] [Google Scholar]
- 30.Pennlert J, Overholser R, Asplund K, Carlberg B, Van Rompaye B, Wiklund PG, et al. Optimal timing of anticoagulant treatment after intracerebral hemorrhage in patients with atrial fibrillation. Stroke. 2017;48:314–320. doi: 10.1161/STROKEAHA.116.014643. [DOI] [PubMed] [Google Scholar]
- 31.Pollack CV, Jr, Reilly PA, van Ryn J, Eikelboom JW, Glund S, Bernstein RA, et al. Idarucizumab for dabigatran reversal - full cohort analysis. N Engl J Med. 2017;377:431–441. doi: 10.1056/NEJMoa1707278. [DOI] [PubMed] [Google Scholar]
- 32.Puckett Y, Zhang K, Blasingame J, Lorenzana J, Parameswaran S, Brooks Md Facs SE, et al. Safest time to resume oral anticoagulation in patients with traumatic brain injury. Cureus. 2018;10:e2920. doi: 10.7759/cureus.2920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rajasekhar A, Lottenberg L, Lottenberg R, Feezor RJ, Armen SB, Liu H, et al. A pilot study on the randomization of inferior vena cava filter placement for venous thromboembolism prophylaxis in high-risk trauma patients. J Trauma. 2011;71:323–328. doi: 10.1097/TA.0b013e318226ece1. [DOI] [PubMed] [Google Scholar]
- 34.Schmidt KJ, Sager B, Zachariah J, Raad BF, James EG, Fletcher JJ. Cohort analysis of desmopressin effect on hematoma expansion in patients with spontaneous intracerebral hemorrhage and documented pre-ictus antiplatelet use. J Clin Neurosci. 2019;66:33–37. doi: 10.1016/j.jocn.2019.05.032. [DOI] [PubMed] [Google Scholar]
- 35.Schulman S, Bijsterveld NR. Anticoagulants and their reversal. Transfus Med Rev. 2007;21:37–48. doi: 10.1016/j.tmrv.2006.08.002. [DOI] [PubMed] [Google Scholar]
- 36.Steiner T, Poli S, Griebe M, Hüsing J, Hajda J, Freiberger A, et al. Fresh frozen plasma versus prothrombin complex concentrate in patients with intracranial haemorrhage related to vitamin K antagonists (INCH): a randomised trial. Lancet Neurol. 2016;15:566–573. doi: 10.1016/S1474-4422(16)00110-1. [DOI] [PubMed] [Google Scholar]
- 37.Thurman DJ, Alverson C, Dunn KA, Guerrero J, Sniezek JE. Traumatic brain injury in the United States: a public health perspective. J Head Trauma Rehabil. 1999;14:602–615. doi: 10.1097/00001199-199912000-00009. [DOI] [PubMed] [Google Scholar]
- 38.Weitz JI. In: Harrison's principles of internal medicine. ed 20. Jameson JL, Fauci AS, Kasper DL, Hauser SL, Longo DL, Loscalzo J, editors. New York, NY: McGraw-Hill Education; 2018. Antiplatelet, anticoagulant, and fibrinolytic drugs. [Google Scholar]
- 39.Yasaka M, Sakata T, Minematsu K, Naritomi H. Correction of INR by prothrombin complex concentrate and vitamin K in patients with warfarin related hemorrhagic complication. Thromb Res. 2002;108:25–30. doi: 10.1016/s0049-3848(02)00402-4. [DOI] [PubMed] [Google Scholar]


