Abstract
Background:
Many pediatric heart transplant (HT) recipients reach adulthood and may be interested in family planning; there is little data regarding safety of pregnancy post HT and clinicians’ opinions differ. Pediatric HT clinicians are instrumental in early counseling. Thus, a better understanding of pediatric HT clinicians’ practices regarding family planning and how well aligned these practices are with adult transplant centers is essential.
Methods:
We conducted a confidential, web-based survey of pediatric HT clinicians in fall 2021. We summarized and compared answers using Fisher’s exact test.
Results:
The survey was sent to 53 United States-based HT directors and to the International Society for Heart and Lung Transplantation and Pediatric Heart Transplant Society list serves. There were 69 respondents. The majority (77%) of respondents felt pregnancy was feasible in selected or all female HT recipients. Ten respondents reported that their institution had an established policy regarding pregnancy post HT. A majority (77%) of HT clinicians would either use a shared care model or recommend transition to their adult institution if pregnancy occurred, though 74% of respondents were either unaware of their corresponding adult institution’s policy (62%) or had a counterpart adult program with a policy against pregnancy post HT (12%).
Conclusions:
While many providers feel pregnancy is feasible in pediatric HT recipients, there remains significant practice variation. Few pediatric programs have a policy regarding pregnancy post HT. Future efforts to provide consistent messaging between adult and pediatric HT programs regarding the feasibility and care of post HT pregnancy are warranted.
Introduction
Post-transplant survival for children and adolescents continues to improve.1 Many pediatric heart transplant (HT) recipients will reach adulthood and may be interested in family planning.2 There are hypothetical concerns that carrying a fetus may increase risk of rejection in solid organ transplant patients and there is limited data regarding safety of pregnancy.3 Due to this lack of data, clinicians caring for HT recipients differ in opinions regarding safety of pregnancy and recommended immunosuppression during pregnancy.4
DeFilippis et al. found that about one third of HT clinicians believed that pregnancy should be avoided in all female HT recipients and nearly half reported that their center had a formal policy regarding pregnancy post HT.3 To our knowledge, DeFilippis’ survey is the only published study regarding opinions surrounding pregnancy in HT recipients and primarily included adult HT clinicians; there are no surveys focused on pediatric HT clinicians. However, pediatric HT clinicians are instrumental in early counseling and teaching, as they care for many children and young adults in their early reproductive years. Thus, a better understanding of pediatric HT clinicians’ attitudes and practices regarding family planning and how well aligned these practices are with adult transplant centers is essential. The aim of this study was to describe current practices among pediatric HT clinicians and pediatric institutional policies regarding pregnancy post HT.
Methods
We conducted a confidential, voluntary, web-based survey of pediatric HT clinicians between September and November 2021. Survey questions can be found in the supplemental materials. The University of Utah and Primary Children’s Hospital Institutional Review Boards approved this study. This study complies with the ISHLT Ethics statement. United States-based pediatric HT directors were emailed with a link inviting them to participate in the survey with a subsequent reminder message weeks later. The survey link was then distributed via the International Society for Heart and Lung Transplantation (ISHLT) connect platform (375 members) and Pediatric Heart Transplant Society (PHTS) Basecamp platform (648 members). This distribution was followed by two reminder messages in the following weeks. Data were collected via Research Electronic Data Capture (REDCap). The questionnaire was developed and refined using expert review and adherence to best practices in survey question writing.5 All of the questions were mandatory and the majority of questions included a “prefer not to answer” option. We summarized the survey by the full cohort or by subset by count and percentage since all were categorical variables. Fisher’s exact test was used to compare clinician characteristics across recommendations to avoid posttransplant pregnancy. Statistical significance was assessed at the 0.05 level. Statistical analyses were implemented using R v. 4.1.2 (R Core Team, 2020).
Results
Respondent Characteristics
The survey was sent to as many as 1023 HT clinicians: 53 United States-based pediatric HT directors as well as to members of the ISHLT and PHTS list serves with 69 respondents. An overall response rate calculation was not performed given the likely but unknown extent of overlap between the two list serves, making it difficult to accurately capture the denominator of respondents.6 However, 30 of the self-identified transplant medical directors were US based, making the response rate 57% (30/53) among US based pediatric HT directors.
Nearly half of respondents (46%) identified themselves as a transplant medical director. The majority of respondents were pediatric cardiologists (77%) followed by pediatric transplant advance practice clinicians (nurse practitioners / physician assistants) (20%), surgeons (1%), and nurse or transplant coordinators (1%). Nearly one-half of the respondents were women (48%) and about one-half of the respondents have been in practice for greater than ten years (49%). The majority reported practicing in the United States (93%); followed by Canada (6%), and Austria (1%). There were respondents from at least 39 different pediatric transplant centers (37 US-based, as well as one center each from Canada and Austria) (Table 1). The number of pediatric HTs varied widely with respondents practicing at centers with the following annual pediatric HT volumes: 14% <5, 33% with 6-10; 28% with 11-15, and 23% >15.
Table 1: Demographics of pediatric HT respondents.
| Variable | All (N=69) |
Feasible for all or selected (N=52) |
Pregnancy should be avoided (N=11) |
Undecided/Preferred not to answer (N=6) |
P Value |
|---|---|---|---|---|---|
| Gender | |||||
| Female | 33 (48%) | 23(44.2%) | 6(54.5%) | 4(66.7%) | 0.60f |
| Male | 36 (52%) | 29 (55.8%) | 5 (45.5%) | 2 (33.3%) | |
| Years in practice | |||||
| 1-10 years | 35 (51%) | 23(44.2%) | 6(54.5%) | 6(100%) | 0.037f |
| 10+ years | 34 (49) | 29 (55.8%) | 5 (45.5%) | 0 (0%) | |
| Country | |||||
| Canada | 4 (6%) | 3(5.8%) | 0(0%) | 1(16.7%) | 0.56f |
| United States | 64 (93%) | 48(92.3%) | 11(100%) | 5(83.3%) | - |
| Other | 1 (1%) | 1(1.9%) | 0(0%) | 0(0%) | - |
| OPTN Region | |||||
| East Coast | 16 (25%) | 13(27.1%) | 2(18.2%) | 1(20%) | 0.98f |
| Midwest | 21 (33%) | 15(31.2%) | 4(36.4%) | 2(40%) | - |
| South | 11 (17%) | 7(14.6%) | 3(27.3%) | 1(20%) | - |
| West Coast | 11 (17%) | 9(18.8%) | 1(9.1%) | 1(20%) | - |
| Prefer not to answer | 5 (8%) | 4(8.3%) | 1(9.1%) | 0(0%) | - |
| Annual center HT volume | |||||
| 1-10 | 33 (49%) | 24(47.1%) | 6(54.5%) | 3(50%) | 0.92f |
| 10+ | 35 (51%) | 27 (52.9%) | 5 (45.5%) | 3(50%) | |
| # of pregnant HT recipients in past 5 years | |||||
| 0 | 43 (63%) | 30(58.8%) | 9(81.8%) | 4(66.7%) | 0.50f |
| 1-5 | 20 (29%) | 17(33.3%) | 2(18.2%) | 1(16.7%) | - |
| Unsure | 5 (7%) | 4(7.8%) | 0(0%) | 1(16.7%) | - |
Missing values: Annual center HT volume =1/0/0,
Experience and Counseling
The majority of respondents (87%) reported gynecologists or primary care clinicians serve as the primary prescribers of contraception for HT patients. Only 6% reported transplant clinicians typically prescribe contraception for their patients. Almost half (45%) recommended that female HT recipients specifically use two methods of contraception.
Notably, 59% of respondents had a HT recipient interested in becoming pregnant, though only 29% of the respondents reported that a HT recipient had become pregnant in their program within the past 5 years. About half (52%) of respondents reported that clinicians at their institution always or often provide information regarding pregnancy post transplantation to pediatric HT recipients or their families prior to transplantation. About one-third (36%) reported that they typically counsel female transplant recipients on the possibility that their partner may be the sole parent given the projected survival of HT recipients, while 10% preferred not to answer this question. Similarly, about one-third (32%) reported counseling male HT recipients that their partner may be the sole parent and 6% preferred not to answer this question.
Clinician Opinions regarding Pregnancy in HT Recipients
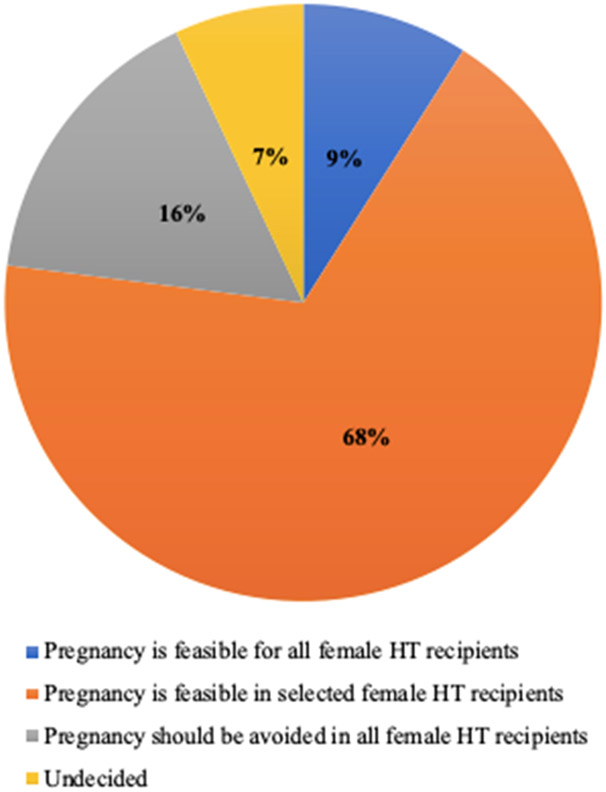
The majority of respondents felt pregnancy was feasible in selected or all female HT recipients (77%). Only 16% felt pregnancy should be avoided in all female HT recipients and 7% remained undecided regarding pregnancy post heart transplantation (Figure 1).
Figure 1:
Pediatric HT clinicians’ opinions regarding pregnancy post HT
We analyzed multiple factors including respondent years of practice, gender, country of practice, Organ Procurement and Transplantation Network (OPTN) region, transplant center volume, and recent experience with pregnant HT recipients to assess any association with respondents’ belief that pregnancy should be avoided in all HT recipients. The only factor that was associated with respondents’ beliefs was years of experience with more experienced practitioners more likely to support pregnancy (55.8% vs 44.2%; p=0.037, Table 1).
Of those who felt pregnancy was feasible, 23% recommended waiting one year, 33% recommended waiting two years, and 40% had no recommendations regarding the timing of pregnancy post transplantation. Within this same cohort, many conditions were considered contraindications to pregnancy (Table 2). Reduced left ventricular ejection fraction (72%), history of noncompliance (70%) and presence of cardiac allograft vasculopathy CAV2 or greater (56%) were the most commonly reported contraindications for attempting conception.
Table 2: Commonly reported contraindications to pregnancy in HT recipients.
The table below lists the percentages of respondents who reported that the conditions would be a contraindication to pregnancy after heart transplantation.
| % Providers (n=57) |
|
|---|---|
| History of any 2R rejection | 11% |
| History of 2R rejection within the past year | 53% |
| History of any 3R rejection | 19% |
| History of 3R rejection within the past year | 19% |
| History of AMR 1h or 1i within the past year | 28% |
| History of AMR 2 | 28% |
| History of AMR 2 in the past year | 51% |
| Reduced left ventricular ejection fraction | 72% |
| Presence of donor specific antibodies without evidence of AMR | 14% |
| presence of any cardiac allograft vasculopathy | 40% |
| Presence of cardiac allograft vasculopathy CAV2 or greater | 56% |
| History of noncompliance within the past year | 70% |
| History of peripartum cardiomyopathy pretransplant | 33% |
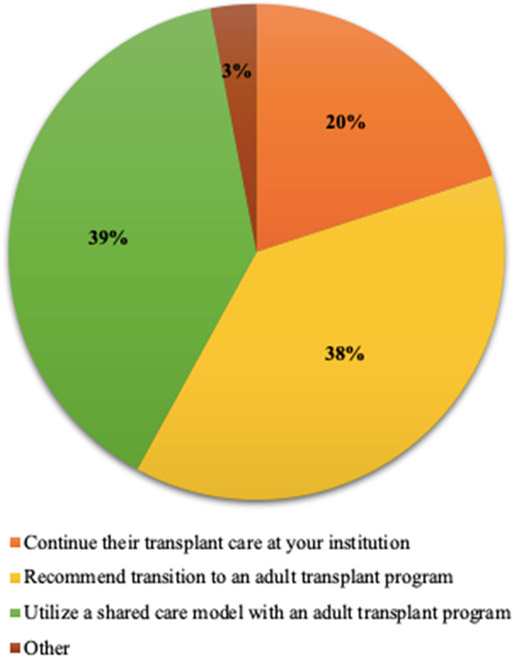
If a transplant recipient 15 years or older were to become pregnant, 38% of respondents would recommend transition to an adult transplant program and 39% would recommend utilizing a shared care model with an adult transplant program (Figure 2). Most respondents (55%) would defer the safety of breastfeeding to a gynecologist or maternal fetal medicine specialist, while 28% reported that it is safe for a HT recipient mother to breastfeed their baby.
Figure 2:
Pediatric HT clinician’s preference when caring for pregnant HT recipients
Institutional Policies regarding Pregnancy in HT Recipients
Only ten respondents (14%) reported that their institution had an established policy regarding pregnancy post HT. Of those ten, six reported the policy was best described as “pregnancy is feasible in selected HT recipients” and four reported the policy was best described as “pregnancy should be avoided in all female HT recipients.” Institutional pre-conception immunosuppression recommendations for the six programs with policies describing pregnancy as feasible varied. The majority of these programs did not have a specified recommended interval for performing echocardiograms (67%) in pregnant HT recipients, while one respondent reported an institutional recommendation of echocardiograms every 2 months and another every 3 months during pregnancy.
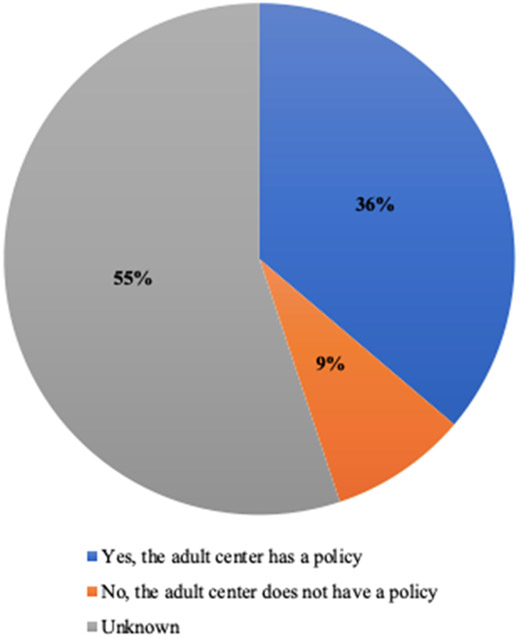
Figure 3 shows the breakdown of respondents’ knowledge about whether their corresponding adult HT program had an established policy regarding pregnancy post HT. The majority (55%) did not know if their adult center had a policy. 36% reported their corresponding adult center did have a policy regarding pregnancy and the remaining 9% reported their corresponding adult center did not have an established policy. Among the 25 respondents who noted that their corresponding adult program had an established policy, 48% reported the adult center policy as “pregnancy is feasible in selected or all female HT recipients” while 32% reported the adult center policy as “pregnancy should be avoided in all female HT recipients.” The remaining 20% were unfamiliar with the specifics of the adult center’s policy. Seven of these 25 respondents also had a pediatric center policy and reported concordance between the pediatric and adult centers’ policies.
Figure 3:
Pediatric HT clinicians’ familiarity with their adult center’s policy (n=69)
Discussion
We describe for the first time, pediatric HT clinicians’ perspectives on pregnancy. While the majority of respondents felt pregnancy was feasible for HT recipients, <30% have had a HT recipient become pregnant in the last 5 years, suggesting they may have limited experience shaping their opinions. Only 16% of pediatric HT clinicians believe pregnancy should be avoided in all female HT recipients compared to 30% reported in DeFilippis’ recent survey of adult HT clinicians.3 The reason for this discordance is not clear, but may reflect differences in clinical experience as adult HT clinicians reported more recent experience caring for pregnant HT recipients (60% vs. 29%). It may also be due to differences in patient age at the time of a HT. While the average age of pediatric HT patients is less than 11 years, the average age of adult recipients is over 50 years with less than a quarter of recipients women and only 11% between the age of 18-34.7 Adult institutions are more likely to have established institutional policies when compared to pediatric institutions (43% vs. 14%) and this may also contribute to clinicians’ opinion regarding pregnancy post HT.3 Notably, the majority (85%) of pediatric HT clinicians with at least ten years of experience believed that pregnancy was feasible for all or selected HT recipients. This may suggest that pediatric HT clinicians who have longitudinal knowledge about the overall health and well-being of pediatric HT recipients believe that the risk to benefit ratio is favorable for females who want to become pregnant after a HT. Alternatively, it may reflect less comfort with restricting patients’ autonomy related to an important decision with limited data.
The majority of caregivers have had a patient interested in becoming pregnant and 29% report a recipient in their program has become pregnant in the last five years; however, only 52% of respondents report regularly providing information regarding pregnancy post HT prior to undergoing transplant there are opportunities to increase counseling pre-HT in terms of contraception, feasibility of a successful pregnancy, and potential risks to both the fetus and the patient. About half of pregnancies among HT recipients in the Transplant Pregnancy Registry were not planned. 2 This highlights the importance of providing contraception counseling to all HT patients regardless of their age.
One of the most striking findings from our survey is that 77% of the pediatric clinicians surveyed would involve their adult colleagues if a pediatric patient became pregnant, yet 62% of pediatric transplant clinicians are not aware if their adult program has a policy or what that policy is and another 12% report their adult HT program recommending against pregnancy in all HT recipients. Our community recognizes the importance of aligned expectations during transition for HT care to improve outcomes8; yet there appears to be a significant knowledge and communication gap related to post HT pregnancy. As pregnancies will continue to occur in female HT patients, irrespective of institutional recommendations, it is important for pediatric HT centers to proactively communicate with their adult HT counterparts and have consistent messaging for their patients.
As with any voluntary survey, this survey may be subject to response bias. An accurate response rate was difficult to ascertain given the identity of respondents was anonymous and the overlap in the listservs, which were likely highly concordant, was unknown. Respondents were not required to report their institutional affiliation, so it is possible that multiple respondents from the same institution were reporting the same information. Nevertheless, the majority of respondents voluntarily reported their institution and OPTN region, and respondents came from at least 39 different institutions and represented all OPTN regions. There was also a robust response rate (57%) among pediatric transplant directors. While this study was limited by the challenges of self-report, which may not accurately reflect institutional practice, these findings contribute a unique perspective on clinician attitudes towards pregnancy.
Moving forward there is a need for further research on the outcomes of pregnancy post HT and for guidelines to guide clinical practice as well as conversations with patients. Participation in existing registries such as the Transplant Pregnancy Registry International will allow for more robust data and with more data regarding risks of pregnancy post HT, clinicians will likely feel more equipped and be more likely to counsel patients regarding feasibility and risks of a pregnancy. Guidelines should include recommendations for routine education about contraceptive options to prevent unplanned pregnancy and to provide appropriate guidance for pregnancy planning or care. The best method to provide contraceptive guidance is not yet clear, but has been prioritized as the initial project of the newly formed PHTS Quality improvement committee. Guidelines should also specify who would care for a pregnant pediatric HT patient whether it is a pediatric team, adult team, or shared care model. Ideally, pediatric and adult guidelines would be concordant. Programs should also consider the feasibility of forming a multidisciplinary team that could include pediatric and adult transplant cardiologists, cardio-obstetrics team with nursing, maternal-fetal medicine, neonatology, pediatric gynecology, anesthesiology, psychology, social work when discussing and managing these cases.9,10
Conclusion
While many pediatric clinicians feel pregnancy is feasible in female HT recipients, there remains significant practice variation and few pediatric transplant programs have a policy regarding pregnancy. Pediatric HT clinicians should discuss pregnancy post HT with their patients and should be familiar with their corresponding adult institutional policy to set expectations early. More research is needed regarding outcomes of pregnancy in post HT patients as well as best practices for care prior to conception and for prenatal care for pregnant HT recipients. Future efforts to create guidelines and provide consistent messaging between adult and corresponding pediatric HT programs is warranted.
Supplementary Material
Acknowledgements
This investigation was supported by the University of Utah Study Design and Biostatistics Center with funding in part from the National Center for Research Resources and the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant 8UL1TR000105 (formerly UL1RR025764) and Award Number UL1TR002538. This content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations:
- HT
Heart transplant
- ISHLT
International Society for Heart and Lung Transplantation
- PHTS
Pediatric Heart Transplant Society
- REDCap
Research Electronic Data Capture
Footnotes
Disclosures
The authors have no actual or potential conflicts of interest (financial, competitive, or otherwise) to disclose.
Contributor Information
Megan M. Collins, Department of Pediatrics, University of Utah, Salt Lake City, UT..
Zhining Ou, Department of Internal Medicine, Division of Epidemiology, University of Utah, Salt Lake City, UT..
Morgan M. Millar, Department of Internal Medicine, Division of Epidemiology, University of Utah, Salt Lake City, UT..
Michelle M. Kittleson, Department of Cardiology, Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles, CA..
Lindsay J. May, Department of Pediatrics, Division of Pediatric Cardiology, University of Utah, Salt Lake City, UT..
Michelle S. Ploutz, Department of Pediatrics, Division of Pediatric Cardiology, University of Utah, Salt Lake City, UT..
Kimberly M. Molina, Department of Pediatrics, Division of Pediatric Cardiology, University of Utah, Salt Lake City, UT..
Katherine G. Hayes, Department of Obstetrics & Gynecology, Division of Pediatric Gynecology, University of Utah, Salt Lake City, UT..
Ashwin K. Lal, Department of Pediatrics, Division of Pediatric Cardiology, University of Utah, Salt Lake City, UT..
References
- 1.Dipchand AI (2018). Current state of pediatric cardiac transplantation. Annals of cardiothoracic surgery, 7(1), 31–55. 10.21037/acs.2018.01.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Perch Michael, et al. “The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Thirty-Eighth Adult Lung Transplantation Report — 2021; Focus on Recipient Characteristics.” The Journal of Heart and Lung Transplantation, vol. 40, no. 10, 2021, pp. 1023–1072., 10.1016/j.healun.2021.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Punnoose Lynn R., et al. “Pregnancy Outcomes in Heart Transplant Recipients.” The Journal of Heart and Lung Transplantation, vol. 39, no. 5, 2020, pp. 473–480., 10.1016/j.healun.2020.02.005. [DOI] [PubMed] [Google Scholar]
- 4.DeFilippis Ersilia M., et al. “Practice Patterns Surrounding Pregnancy After Heart Transplantation.” Circulation: Heart Failure, 2020; 13(4):e006811. Doi: 10.1161/circheartfailure.119.006811. [DOI] [PubMed] [Google Scholar]
- 5.Dillman DA, Smyth JD, & Christian LM (2014). Internet, phone, mail, and mixed mode surveys: The tailored design method (4th ed.). John Wiley & Sons Inc. [Google Scholar]
- 6.The American Association for Public Opinion Research. 2016. Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. 9th edition. AAPOR. [Google Scholar]
- 7.“OPTN/SRTR 2019 Annual Data Report.” American Journal of Transplantation, vol. 21, no. S2, 2021, pp. 1–10., 10.1111/ajt.16497. [DOI] [Google Scholar]
- 8.Bell LE, Bartosh SM, Davis CL, Dobbels F, Al-Uzri A, Lotstein D, Reiss J, Dharnidharka VR. Adolescent Transition to Adult Care in Solid Organ Transplantation: a consensus conference report. Am J Transplant. 2008. Nov;8(11):2230–42. doi: 10.1111/j.1600-6143.2008.02415. [DOI] [PubMed] [Google Scholar]
- 9.DeFilippis Ersilia M., and Kittleson Michelle M.. “Pregnancy after Heart Transplantation: A Need for Updated Guidelines.” The Journal of Heart and Lung Transplantation, vol. 39, no. 10, 2020, p. 1159., 10.1016/j.healun.2020.06.029. [DOI] [PubMed] [Google Scholar]
- 10.Davis MB, et al. Team-Based Care of Women With Cardiovascular Disease From Pre-Conception Through Pregnancy and Postpartum: JACC Focus Seminar 1/5. Journal of the American College of Cardiology, 77(14), 1763–1777. 10.1016/j.jacc.2021.02.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.