Abstract
The SENTRY Program was established in January 1997 to measure the predominant pathogens and antimicrobial resistance patterns of nosocomial and community-acquired infections over a broad network of sentinel hospitals in the United States (30 sites), Canada (8 sites), South America (10 sites), and Europe (24 sites). During the first 6-month study period (January to June 1997), a total of 5,058 bloodstream infections (BSI) were reported by North American SENTRY participants (4,119 from the United States and 939 from Canada). In both the United States and Canada, Staphylococcus aureus and Escherichia coli were the most common BSI isolates, followed by coagulase-negative staphylococci and enterococci. Klebsiella spp., Enterobacter spp., Pseudomonas aeruginosa, Streptococcus pneumoniae, and β-hemolytic streptococci were also among the 10 most frequently reported species in both the United States and Canada. Although the rank orders of pathogens in the United States and Canada were similar, distinct differences were noted in the antimicrobial susceptibilities of several pathogens. Overall, U.S. isolates were considerably more resistant than those from Canada. The differences in the proportions of oxacillin-resistant S. aureus isolates (26.2 versus 2.7% for U.S. and Canadian isolates, respectively), vancomycin-resistant enterococcal isolates (17.7 versus 0% for U.S. and Canadian isolates, respectively), and ceftazidime-resistant Enterobacter sp. isolates (30.6 versus 6.2% for U.S. and Canadian isolates, respectively) dramatically emphasize the relative lack of specific antimicrobial resistance genes (mecA, vanA, and vanB) in the Canadian microbial population. Among U.S. isolates, resistance to oxacillin among staphylococci, to vancomycin among enterococci, to penicillin among pneumococci, and to ceftazidime among Enterobacter spp. was observed in both nosocomial and community-acquired pathogens, although in almost every instance the proportion of resistant strains was higher among nosocomial isolates. Antimicrobial resistance continues to increase, and ongoing surveillance of microbial pathogens and resistance profiles is essential on national and international scales.
Bloodstream infections (BSI) due to bacterial and fungal pathogens affect over 200,000 individuals annually in the United States alone and are a tremendously important cause of morbidity and mortality worldwide (19, 20, 22). The attributable mortality of BSI is approximately 27% (19), and a recently published national vital statistics report has documented an increase in age-adjusted death rates due to septicemia from 4.2 per 100,000 in 1980 to 13.2 per 100,000 in 1992 (18).
The impact of specific etiologic agents on the outcome of BSI has been well documented and speaks to the need for a better understanding of the spectrum of pathogens causing both nosocomial and community-acquired BSI (19, 22). Detection of microorganisms in blood cultures is considered an indicator of disseminated infection and has been shown to be a valid marker for surveillance of BSI (16). In a recent prospective multicenter study of BSI, Weinstein et al. (22) noted substantial changes in the microbiology, epidemiology, and clinical and prognostic significance of positive blood cultures over a 20-year period. They found that Staphylococcus aureus and Escherichia coli continued to be the most common etiologic agents of BSI and noted important increases in BSI due to coagulase-negative staphylococci (CoNS), fungi, and Pseudomonas aeruginosa (community acquired). Importantly, they found that BSI due to fungi and Enterobacteriaceae other than E. coli were associated with a significantly increased risk of death. The rapid detection of positive blood cultures and reporting of antimicrobial susceptibility results were also useful in the care of patients (22).
One of the more alarming recent trends in infectious diseases has been the increasing frequency of antimicrobial resistance among microbial pathogens causing nosocomial and community-acquired infections (1, 9). Numerous classes of antimicrobial agents have become less effective as a result of the emergence of antimicrobial resistance, often as a result of the selective pressure of antimicrobial usage (2, 9). Among the more important emerging resistance problems are oxacillin resistance in staphylococci, penicillin resistance in streptococci, vancomycin resistance in enterococci (and eventually staphylococci), resistance to extended-spectrum cephalosporins and fluoroquinolones in the Enterobacteriaceae, and carbapenem resistance in P. aeruginosa (1, 9, 17).
These resistance trends and the clinical significance and changing spectrum of microbial pathogens argue strongly for a national program of antimicrobial resistance surveillance. Such a program will play a critical role in guiding physicians toward appropriate parenteral agents for use in the treatment of both community- and hospital-acquired BSI, as well as identifying changing patterns of etiologic agents and drug susceptibility. In this study we describe the frequencies of occurrence and antimicrobial susceptibility profiles of BSI isolates from 38 North American medical centers (30 in the United States and 8 in Canada) participating in the SENTRY antimicrobial resistance surveillance program. The SENTRY program is a longitudinal surveillance program designed to track antimicrobial resistance trends nationally and internationally over a 5- to 10-year period. The present study includes all BSI isolates in the United States and Canada from the initiation of the program (January 1997) through June 1997 (approximately 6 months).
MATERIALS AND METHODS
Study design.
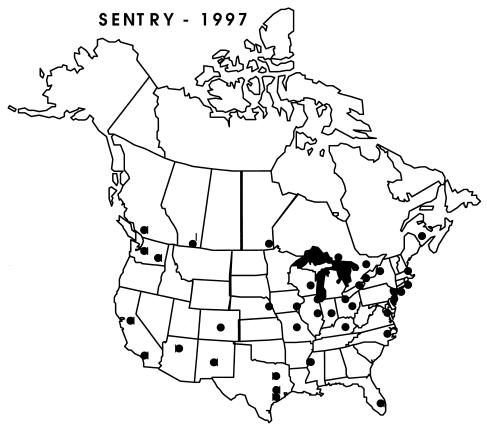
The SENTRY program was established to monitor the predominant pathogens and antimicrobial resistance patterns of nosocomial and community-acquired infections via a broad network of sentinel hospitals distributed equally by geographic location and size. The monitored infections include bacteremia and fungemia (objective A), outpatient respiratory infections due to fastidious organisms (Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis; objective B), pneumonia (objective C), wound infections (objective D), and urinary tract infections (objective E) in hospitalized patients. Participating institutions include 30 medical centers in the United States, 8 in Canada, 10 in South America, and 24 in Europe. The present report will focus on BSI isolates from North America (30 U.S. and 8 Canadian sites) (Fig. 1). The U.S. sites were located in 23 different states and represented institutions ranging in size from 250 to 4,000 beds (mean, 760 beds). The Canadian sites were located in seven provinces (Alberta, British Columbia, Manitoba, Nova Scotia, Ontario, Quebec, and Saskatchewan) and represented institutions ranging in size from 400 to 1,200 beds (mean, 726 beds).
FIG. 1.
Locations of North American participants in the SENTRY program.
Each participant hospital contributed results (organism identification, date of isolation, and antimicrobial susceptibility profile) on the first 20 consecutive blood culture isolates judged to be clinically significant by local criteria (separate patients) that were detected in each calendar month during the initial 6-month period, January 1997 through 30 June 1997. Each laboratory was encouraged to critically analyze CoNS in the context of their clinical significance. All isolates were saved on agar slants and sent on a weekly basis to the University of Iowa (Iowa City) for storage and for further characterization by reference identification and susceptibility testing methods.
Organism identification.
All blood culture isolates were identified at the participating institution by the routine methodology in use at each laboratory. Upon receipt at the University of Iowa, isolates were subcultured onto blood agar to ensure viability and purity. Confirmation of species identification was performed with Vitek (bioMerieux Vitek, St. Louis, Mo.) and API (bioMerieux) products or conventional methods as required (12). Isolates were frozen at −70°C until needed.
Susceptibility testing.
Antimicrobial susceptibility testing of isolates was performed by reference broth microdilution methods as described by the National Committee for Clinical Laboratory Standards (NCCLS) (13). Microdilution trays were purchased from MicroScan (Sacramento, Calif.) and Prepared Media Laboratories (Tualatin, Oreg.). Antimicrobial agents were obtained from the respective manufacturers and included ampicillin, oxacillin, penicillin, piperacillin, ticarcillin, amoxicillin-clavulanate, ticarcillin-clavulanate, piperacillin-tazobactam, cefazolin, cefuroxime, cefoxitin, ceftriaxone, ceftazidime, cefepime, aztreonam, imipenem, meropenem, amikacin, gentamicin, tobramycin, streptomycin, ciprofloxacin, ofloxacin, levofloxacin, sparfloxacin, gatifloxacin, trovafloxacin, erythromycin, clindamycin, quinupristin-dalfopristin, chloramphenicol, rifampin, tetracycline, teicoplanin, vancomycin, and trimethoprim-sulfamethoxazole. Quality control was performed by testing E. coli ATCC 25922, S. aureus ATCC 29213, P. aeruginosa ATCC 27853, S. pneumoniae ATCC 49619, and Enterococcus faecalis ATCC 29212. Interpretive criteria for each antimicrobial tested were those published by NCCLS (14).
RESULTS
Frequency of occurrence of bloodstream pathogens.
During the 6-month study period (January 1997 to June 1997) a total of 5,058 BSI were reported by SENTRY participants (4,119 from the United States and 939 from Canada). Table 1 lists the 20 most frequently isolated bacterial pathogens causing BSI in these hospitals. These 20 organisms and groups accounted for 97.8% of all BSI during this time period. In both the United States and Canada, S. aureus and E. coli were the most common BSI isolates, followed by CoNS and enterococci. These four organism groups accounted for approximately 64% of all BSI in the 38 North American sites. Klebsiella spp., S. pneumoniae, P. aeruginosa, Enterobacter spp., and beta-hemolytic streptococci were also among the 10 most frequently reported species at both U.S. and Canadian study sites.
TABLE 1.
Frequencies of occurrence of bacterial pathogens associated with BSI in participating medical centers in the United States and Canada (SENTRY antimicrobial surveillance program, 1997)
| Rank | Organismb | No. of isolates (%)a from:
|
||
|---|---|---|---|---|
| U.S. | Canada | Total | ||
| 1 | S. aureus | 969 (23.5) | 185 (19.7) | 1,154 (22.8) |
| 2 | E. coli | 769 (18.7) | 181 (19.3) | 950 (18.8) |
| 3 | CoNS | 533 (12.9) | 142 (15.1) | 675 (13.3) |
| 4 | Enterococcus spp. | 396 (9.6) | 78 (8.3) | 474 (9.4) |
| 5 | Klebsiella spp. | 311 (7.6) | 53 (5.6) | 364 (7.2) |
| 6 | S. pneumoniae | 209 (5.1) | 59 (6.3) | 268 (5.3) |
| 7 | P. aeruginosa | 189 (4.6) | 45 (4.8) | 234 (4.6) |
| 8 | Enterobacter spp. | 151 (3.7) | 34 (3.6) | 185 (3.7) |
| 9 | Beta-hemolytic streptococci | 151 (3.7) | 33 (3.5) | 184 (3.6) |
| 10 | P. mirabilis | 68 (1.7) | 9 (1.0) | 77 (1.5) |
| 11 | Viridans group streptococci | 36 (0.9) | 37 (3.9) | 73 (1.4) |
| 12 | Acinetobacter spp. | 57 (1.4) | 10 (1.1) | 67 (1.3) |
| 13 | Serratia spp. | 50 (1.2) | 12 (1.3) | 62 (1.2) |
| 14 | Citrobacter spp. | 37 (0.9) | 3 (0.3) | 40 (0.8) |
| 15 | S. maltophilia | 30 (0.7) | 10 (1.1) | 40 (0.8) |
| 16 | P. agglomerans | 20 (0.5) | 8 (0.9) | 28 (0.6) |
| 17 | Salmonella spp. | 18 (0.4) | 6 (0.6) | 24 (0.5) |
| 18 | Haemophilus spp. | 15 (0.3) | 4 (0.4) | 19 (0.4) |
| 19 | M. morganii | 11 (0.2) | 3 (0.3) | 14 (0.3) |
| 20 | Corynebacterium spp. | 10 (0.2) | 3 (0.3) | 13 (0.2) |
Percent of 5,058 isolates (4,119 U.S. and 939 Canadian isolates).
P. mirabilis, Proteus mirabilis; S. maltophilia, Stenotrophomonas maltophilia; P. agglomerans, Pantoea agglomerans; M. morganii, Morganella morganii.
Antimicrobial susceptibilities of gram-positive pathogens.
Tables 2 to 5 list MICs of 27 antimicrobial agents tested against the four most prevalent causes of gram-positive BSI (S. aureus, CoNS, enterococci, and S. pneumoniae) in the United States (Tables 2 and 3) and Canada (Tables 4 and 5). In both countries these species accounted for approximately 50% (51% in the United States and 49% in Canada) of all bacteremic episodes. For the staphylococci, considerable differences in the percentages of S. aureus isolates that were susceptible to oxacillin between the United States and Canada were observed. Only 73.8% of U.S. S. aureus BSI isolates were susceptible to oxacillin versus 97.3% of Canadian isolates (Tables 2 and 4). This difference in oxacillin susceptibility corresponds to similar differences in susceptibility to all β-lactam agents (Tables 2 and 4) and also to non-β-lactam antimicrobials (Tables 3 and 5). Canadian S. aureus BSI isolates were more susceptible to gentamicin (97.7 versus 86.3%), fluoroquinolones (97.7 to 98.3% versus 71.8 to 73.7%), macrolides (58.7 to 96.7% versus 35.9 to 76%), and trimethoprim-sulfamethoxazole (96.6 versus 89.2%). Notably, quinupristin-dalfopristin, teicoplanin, and vancomycin were uniformly active against all isolates of S. aureus in both the United States and Canada.
TABLE 2.
Activities and spectra of activity of the 10 β-lactam antimicrobial agents tested against the four most prevalent causes of gram-positive bacteremia in the United States (51% of all bacteremic episodes)
| Antimicrobial class and agent tested | Activitya againstb:
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
S. aureus (969)
|
CoNS (533)
|
Enterococcus (396)
|
S. pneumoniae (209)
|
|||||||||
| MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | |
| Penicillins | ||||||||||||
| Ampicillin-amoxicillin | ≤0.12–>16 | 8/>16 | 11.1 | ≤0.12–>16 | 8/>16 | 17.9 | ≤0.12–>16 | 1/>16 | 74.3 | ≤0.06–>8 | ≤0.06/2 | 84.4 |
| Oxacillin | ≤0.06–>8 | 0.5/>8 | 73.8 | ≤0.06–>8 | 8/>8 | 43.1 | ≤0.06–>8 | >8/>8 | —c | NTd | — | — |
| Penicillin | ≤0.015–>32 | 16/>32 | 10.2 | ≤0.015–>32 | 8/>32 | 13.4 | ≤0.015–>32 | 2/>32 | 72.5 | ≤0.08–>16 | 0.06/2 | 59.0 |
| Amoxicillin-clavulanate | ≤0.12–>16 | 1/>16 | 73.8e | ≤0.12–>16 | 2/16 | 43.1e | ≤0.12–>16 | 1/>16 | — | ≤0.6–>8 | ≤0.06/4 | 83.4 |
| Piperacillin-tazobactam | ≤0.5–>64 | 1/64 | 73.8e | ≤0.5–>64 | 2/64 | 43.1e | 1–>64 | 4/>64 | — | NT | — | — |
| Cephalosporins | ||||||||||||
| Cefazolin | ≤2–>16 | ≤2/>16 | — | ≤2–>16 | ≤2/>16 | — | ≤2–>16 | >16/>16 | — | NT | — | — |
| Cefuroxime | NT | — | — | NT | — | — | NT | — | — | ≤0.06–>8 | ≤0.06/4 | 79.5 |
| Cefotaxime-ceftriaxone | ≤0.25–>32 | 4/>32 | — | ≤0.25–>32 | 8/>32 | — | ≤0.25–>32 | >32/>32 | — | ≤0.008–8 | 0.03/1 | 86.8 |
| Cefepime | ≤0.12–>16 | 4/>16 | — | ≤0.12–>16 | 4/>16 | — | ≤0.12–>16 | >16/>16 | — | ≤0.06–4 | ≤0.06/1 | 83.4 |
| Other | ||||||||||||
| Imipenem | ≤0.06–>8 | 0.12/>8 | — | ≤0.06–>8 | 0.5/>8 | — | 0.06–>8 | 2/>8 | — | NT | — | — |
MIC50 and MIC90, MICs at which 50 and 90% of the isolates, respectively, were inhibited. The units for all MICs are micrograms per milliliter. % S, percent of isolates susceptible per NCCLS criteria (14).
Numbers in parentheses are numbers of isolates.
—, no interpretive criteria have been published by the NCCLS (14).
NT, not tested.
The spectra of activity for all β-lactams versus S. aureus and CoNS are predicted by the oxacillin result.
TABLE 5.
Activities and spectra of activity of 16 representatives of non-β-lactam drug classes tested against the four most prevalent causes of gram-positive bacteremia in Canada
| Antimicrobial class and agent tested | Activity againsta:
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
S. aureus (185)
|
CoNS (142)
|
Enterococcus (78)
|
S. pneumoniae (59)
|
|||||||||
| MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | |
| Aminoglycosides | ||||||||||||
| Gentamicin | ≤0.12–>16 | 0.5/1 | 97.7 | ≤0.12–>16 | 4/>16 | 50.8 | NTc | —f | — | NT | — | — |
| Gentamicin (HL)b | NT | — | — | NT | — | — | ≤500–>1,000 | >1,000/>1,000 | 48.0 | NT | — | — |
| Streptomicin (HL) | NT | — | — | NT | — | — | ≤1,000–>2,000 | ≤1,000/>2,000 | 50.7 | NT | — | — |
| Fluoroquinolones | ||||||||||||
| Ciprofloxacin | 0.06–>2 | 0.25/0.5 | 98.3 | ≤0.15–>2 | 0.25/>2 | 68.2 | 0.12–>2 | >2/>2 | 36.8 | 0.5–>2 | 1/2 | — |
| Levofloxacin | NT | — | — | NT | — | — | NT | — | — | ≤0.5–4 | 1/2 | 96.6 |
| Sparfloxacind | ≤0.25–>2 | ≤0.25/≤0.25 | 97.7 | ≤0.25–>2 | ≤0.25/>2 | 68.9 | ≤0.25–>2 | >2/>2 | — | ≤0.12–0.5 | 0.25/0.5 | — |
| Gatifloxacind | ≤0.03–>4 | 0.06/0.12 | — | ≤0.03–>4 | 0.12/4 | — | 0.06–>4 | >4/>4 | — | 0.12–0.5 | 0.5/0.5 | — |
| Trovafloxacind | ≤0.03–4 | ≤0.03/0.12 | — | ≤0.03–>4 | 0.12/>4 | — | ≤0.03–>4 | >4/>4 | — | 0.12–1 | 0.25/0.5 | 100 |
| MLSg | ||||||||||||
| Erythromycin | 0.25–>8 | 0.5/>8 | 58.7 | 0.12–>8 | >8/>8 | 26.5 | 0.12–>8 | >8/>8 | — | ≤0.25–>32 | ≤0.25/≤0.25 | 93.2e |
| Clindamycin | 0.12–>8 | 0.12/0.25 | 96.7 | ≤0.06–>8 | 0.25/>8 | 56.6 | 0.12–>8 | >8/>8 | — | ≤0.06–>8 | 0.12/0.12 | 98.3 |
| Quinupristin-dalfopristind (30:70) | 0.12–1 | 0.25/0.5 | — | ≤0.06–2 | 0.25/0.5 | — | 0.25–>8 | 4/>8 | — | 0.25–4 | 0.5/1 | — |
| Others | ||||||||||||
| Chloramphenicol | 1–>16 | 8/16 | 79.9 | ≤0.12–>16 | 8/>16 | 84.6 | 2–>16 | 8/>16 | 72.0 | ≤2–16 | ≤2/≤2 | 98.3 |
| Rifampin | ≤0.015–>2 | ≤0.015/≤0.015 | 99.5 | ≤0.015–>2 | ≤0.015/0.03 | 95.6 | ≤0.015–>2 | 2/>2 | — | ≤1 | ≤1/≤1 | 100 |
| Tetracycline | ≤4–>8 | ≤4/≤4 | 94.3 | ≤4–>8 | ≤4/>8 | 81.8 | ≤4–>8 | >8/>8 | 44.7 | ≤2–>16 | ≤2/4 | 89.8 |
| Teicoplanin | ≤0.12–8 | 0.25/1 | 100 | ≤0.12–>6 | 1/8 | 94.1 | ≤0.12–1 | 0.25/0.5 | 100 | NT | — | — |
| Vancomycin | 0.5–2 | 0.5/1 | 100 | 0.25–4 | 1/2 | 100 | 0.5–2 | 1/2 | 100 | 0.12–0.5 | 0.25/0.5 | 100 |
| Trimethoprim-sulfamethoxazole | ≤0.5–>1 | ≤0.5/≤0.5 | 96.6 | ≤0.5–>1 | ≤0.5/>1 | 56.1 | ≤0.5–>1 | >1/>1 | — | ≤0.25–>8 | ≤0.25/4 | 76.3 |
MIC50, MIC90, and % S are as defined for Table 2 (see footnote a). MIC units are micrograms per milliliter. Numbers in parentheses are numbers of isolates.
HL, high-level aminoglycoside resistance screen.
NT, not tested.
Investigational drug.
Erythromycin is representative of other macrolides (azithromycin and clarithromycin). Cross-resistance and -susceptibility were essentially complete.
As defined for Table 2.
As defined for Table 3.
TABLE 3.
Activities and spectra of activity of 16 representatives of non-β-lactam drug classes tested against the four most prevalent causes of gram-positive bacteremia in the United States
| Antimicrobial class and agent tested | Activitya againstb:
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
S. aureus (969)
|
CoNS (533)
|
Enterococcus (396)
|
S. pneumoniae (209)
|
|||||||||
| MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | |
| Aminoglycosides | ||||||||||||
| Gentamicin | ≤0.12–>16 | 0.5/>16 | 86.3 | ≤0.12–>16 | 0.5/>16 | 60.0 | NTf | — | — | NT | — | — |
| Gentamicin (HL)c | NT | —g | — | NT | — | — | ≤500–>1,000 | ≤500/>1,000 | 66.7 | NT | — | — |
| Streptomicin (HL) | NT | — | — | NT | — | — | ≤1,000–>2,000 | ≤1,000/>2,000 | 56.7 | NT | — | — |
| Fluoroquinolones | ||||||||||||
| Ciprofloxacin | ≤0.15–>2 | 0.5/>2 | 71.8 | ≤0.15–>2 | 0.5/>2 | 57.5 | ≤0.15–>2 | >2/>2 | 33.9 | 0.12–>2 | 1/2 | — |
| Levofloxacin | NT | — | — | NT | — | — | NT | — | — | ≤0.5–4 | 1/2 | 99.5 |
| Sparfloxacind | ≤0.25–>2 | ≤0.25/>2 | 73.7 | ≤0.25–>2 | ≤0.25/>2 | 58.5 | ≤0.25–>2 | 2/>2 | — | ≤0.12–1 | 0.25/0.5 | — |
| Gatifloxacind | ≤0.03–>4 | 0.12/4 | — | ≤0.03–>4 | 0.12/4 | — | 0.03–>4 | 2/>4 | — | 0.06–1 | 0.5/0.5 | — |
| Trovafloxacind | ≤0.03–>4 | 0.06/2 | — | ≤0.3–>4 | 0.12/>4 | — | 0.03–>4 | 2/>4 | — | ≤0.03–1 | 0.25/0.5 | 100 |
| MLSh | ||||||||||||
| Erythromycin | ≤0.06–>8 | 1/>8 | 35.9 | ≤0.06–>8 | >8/>8 | 22.8 | ≤0.6–>8 | >8/>8 | — | ≤0.25–>32 | ≤0.25/1 | 88.1e |
| Clindamycin | ≤0.06–>8 | 0.25/>8 | 76.0 | ≤0.06–>8 | 0.25/>8 | 57.1 | ≤0.06–>8 | >8/>8 | — | ≤0.06–>8 | 0.12/0.12 | 96.0 |
| Quinupristin-dalfopristind (30:70) | ≤0.06–4 | 0.5/1 | — | ≤0.06–>8 | 0.25/0.5 | — | 0.25–>8 | 4/>8 | — | ≤0.06–>8 | 0.5/11 | — |
| Others | ||||||||||||
| Chloramphenicol | ≤0.12–>16 | 8/16 | 72.7 | ≤0.12–>16 | 8/16 | 88.5 | ≤0.12–>16 | 8/16 | 82.8 | ≤2–>16 | ≤2/≤2 | 96.5 |
| Rifampin | ≤0.015–>2 | ≤0.015/≤0.015 | 96.8 | ≤0.015–>2 | ≤0.015/≤0.015 | 89.7 | ≤0.015–>2 | 2/>2 | — | ≤1–2 | ≤1/≤1 | 99.5 |
| Tetracycline | ≤4–>8 | ≤4/≤4 | 90.9 | ≤4–>8 | ≤4/≤4 | 79.5 | ≤4–>8 | >8/>8 | 33.6 | ≤2–>16 | ≤2/4 | 89.1 |
| Teicoplanin | ≤0.12–>16 | 0.25/1 | 99.8 | ≤0.12–>16 | 1/8 | 95.0 | ≤0.12–>16 | 0.25/≤16 | 87.4 | NT | — | — |
| Vancomycin | 0.25–4 | 0.5/1 | 100 | ≤0.12–4 | 1/2 | 100 | 0.25–>16 | 1/>16 | 82.3 | ≤0.1–1 | 0.25/0.5 | 100 |
| Trimethoprim-sulfamethoxazole | ≤0.5–>1 | ≤0.5/>1 | 89.2 | ≤0.5–>1 | ≤0.5/>1 | 55.6 | ≤0.5–>1 | 1/>1 | — | ≤0.25–>8 | ≤0.25/8 | 74.8 |
MIC50, MIC90, and % S are as defined for Table 2 (see footnote a). MIC units are micrograms per milliliter.
Numbers in parentheses are numbers of isolates.
HL, high-level aminoglycoside resistance screen.
Investigational drug.
Erythromycin is representative of other macrolides (azithromycin and clarithromycin). Cross-susceptibility and -resistance were essentially complete.
NT, not tested.
As defined for Table 2.
MLS, macrolides-lincosamides-streptogramin B.
TABLE 4.
Activities and spectra of activity of 10 β-lactam antimicrobial agents tested against the four most prevalent causes of gram-positive bacteremia in Canada (49% of all bacteremic episodes)
| Antimicrobial class and agent tested | Activitya againstb:
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
S. aureus (185)
|
CoNS (142)
|
Enterococcus (78)
|
S. pneumoniae (59)
|
|||||||||
| MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | |
| Penicillins | ||||||||||||
| Ampicillin-amoxicillin | ≤0.12–>16 | 4/>16 | 9.7 | ≤0.12–>16 | 8/>16 | 22.0 | ≤0.12–>16 | 1/>16 | 75.0 | ≤0.06–4 | ≤0.06/0.25 | 94.9 |
| Oxacillin | ≤0.06–>8 | 0.25/0.5 | 97.3 | ≤0.06–>8 | 4/>8 | 47.8 | 4–>8 | >8/>8 | —c | NTd | — | — |
| Penicillin | ≤0.015–>32 | 8/>32 | 9.3 | ≤0.015–>32 | 8/>32 | 19.9 | 1–>32 | 2/>32 | 74.7 | ≤0.08–2 | 0.06/0.25 | 69.5 |
| Amoxicillin-clavulanate | ≤0.12–>16 | 1/2 | 97.3e | ≤0.12–>16 | 2/16 | 47.8e | ≤0.12–>16 | 1/>16 | — | ≤0.06–4 | ≤0.06/0.25 | 94.9 |
| Piperacillin-tazobactam | ≤0.5–>64 | 1/2 | 97.3e | ≤0.5–>64 | 2/64 | 47.8e | ≤0.5–>64 | 4/>64 | — | NT | — | — |
| Cephalosporins | ||||||||||||
| Cefazolin | ≤2–>16 | ≤2/≤2 | — | ≤2–>16 | ≤2/16 | — | 4–>16 | >16/>16 | — | NT | — | — |
| Cefuroxime | NT | — | — | NT | — | — | NT | — | — | ≤0.06–>8 | ≤0.06/0.25 | 94.9 |
| Cefotaxime-ceftriaxone | ≤0.25–>32 | 2/4 | — | 0.5–>32 | 8/>32 | — | 0.5–>32 | >32/>32 | — | ≤0.008–>16 | 0.03/0.12 | 94.9 |
| Cefepime | 0.25–>16 | 2/8 | — | ≤0.12–>16 | 4/>16 | — | 4–>16 | >16/>16 | — | ≤0.06–2 | ≤0.06/0.25 | 94.9 |
| Other | ||||||||||||
| Imipenem | ≤0.06–>8 | ≤0.06/≤0.06 | — | ≤0.06–>8 | 0.5/>8 | — | 0.5–>8 | 2/>8 | — | NT | — | — |
MIC50, MIC90, and % S are as defined for Table 2 (see footnote a). MIC units are micrograms per milliliter.
Numbers in parentheses are numbers of isolates.
As defined for Table 2.
NT, not tested.
The spectra of activity for all β-lactams versus S. aureus and CoNS are predicted by the oxacillin result.
Oxacillin resistance rates were high among CoNS BSI isolates from both U.S. (56.9%) and Canadian (52.2%) sites (Tables 2 and 4). Although the fluoroquinolones were slightly more active against Canadian isolates (68.2 to 68.9% versus 57.5 to 58.5% susceptible) there were no major differences in activity among the other non-β-lactam agents tested. Neither gatifloxacin nor trovafloxacin demonstrated increased activity against CoNS compared with ciprofloxacin or sparfloxacin. As with S. aureus, quinupristin-dalfopristin, teicoplanin, and vancomycin were all active against these CoNS.
Striking differences in the proportion of enterococcal BSI isolates that were resistant to vancomycin between the United States and Canada were observed. Approximately 18% of U.S. isolates (3.5% of E. faecalis isolates and 53% of Enterococcus faecium isolates) were resistant to vancomycin versus 0% of Canadian isolates. Conversely, high-level resistance (HLR) to aminoglycosides was more common among Canadian isolates (52% had HLR to gentamicin and 49.3% had HLR to streptomycin) than among U.S. isolates (corresponding values are 33.3 and 43.3%, respectively). All E. faecium isolates were inhibited by ≤4 μg of quinupristin-dalfopristin per ml.
Decreased susceptibility to penicillin was noted among both U.S. (41% resistant) and Canadian (30.5% resistant) isolates of S. pneumoniae (Tables 2 and 4). HLR (MIC, ≥2 μg/ml) to penicillin was greater among U.S. isolates (14 versus 6.8%). U.S. isolates were also considerably less susceptible than Canadian isolates to ampicillin-amoxicillin (84.4 versus 94.9%), to extended-spectrum cephalosporins such as cefotaxime-ceftriaxone (86.8 versus 94.9%), and cefepime (83.4 versus 93.2%). Both U.S. and Canadian S. pneumoniae BSI isolates remained highly susceptible to fluoroquinolones (96 to 100%) and vancomycin (100%). Quinupristin-dalfopristin was also quite active, with 99% of all S. pneumoniae BSI isolates inhibited by ≤4 μg/ml.
Antimicrobial susceptibilities of gram-negative pathogens.
Tables 6 to 9 list the results for 26 antimicrobial agents tested against the four most prevalent causes of gram-negative BSI (E. coli, Klebsiella spp., P. aeruginosa, and Enterobacter spp.) in the United States (Tables 6 and 7) and Canada (Tables 8 and 9). These species accounted for 33 to 34% of all bacteremic episodes in the two countries. For E. coli, there were no major differences in the antimicrobial susceptibility profiles between the U.S. and Canadian isolates. Piperacillin-tazobactam was the most active of the penicillins (95.5% susceptible), and cefepime was the most active cephalosporin (99.3 to 100% susceptible). Only 1.1 (Canada) to 2% (United States) of E. coli BSI isolates were resistant to ceftazidime, suggesting a low prevalence of extended-spectrum β-lactamase (ESBL)-producing strains, although these isolates were not tested further to confirm ESBL production (14). Virtually all isolates remained susceptible to the carbapenems (imipenem and meropenem; >99% susceptible) and aztreonam (96.1 to 98.3% susceptible). Similarly, the vast majority of E. coli isolates remained susceptible to the aminoglycosides (94.3 to 98.9%) and fluoroquinolones (96.6 to 97.6%). Notably, only 74.3 and 80.7% of U.S. and Canadian E. coli BSI isolates, respectively, were susceptible to trimethoprim-sulfamethoxazole.
TABLE 6.
Activities and spectra of activity of 15 β-lactam antimicrobial agents tested against the four most prevalent causes of gram-negative bacteremia in the United States (34% of all bacteremic episodes)
| Antimicrobial class and agent tested | Activitya againstb:
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
E. coli (769)
|
Klebsiella (311)
|
P. aeruginosa (189)
|
Enterobacter (151)
|
|||||||||
| MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | |
| Penicillins | ||||||||||||
| Ampicillin-amoxicillin | 0.25–>16 | 8/16 | 52.4 | 4–>16 | >16/>16 | 2.7 | 16–>16 | >16/>16 | 0.0 | 4–>16 | >16/>16 | 1.4 |
| Piperacillin | ≤1–>128 | 2/>128 | 57.0 | ≤1–>128 | 8/>128 | 80.7 | ≤1–>128 | 4/64 | 93.0 | ≤1–>128 | 4/>128 | 63.9 |
| Ticarcillin | ≤1–>128 | 8/>128 | 53.6 | ≤1–>128 | >128/>128 | 2.3 | ≤1–>128 | 32/128 | 86.6 | ≤1–>128 | 8/>128 | 59.2 |
| Amoxicillin-clavulanate | 0.5–>16 | 8/16 | 68.8 | 1–>16 | 4/16 | 89.7 | 2–>16 | >16/>16 | 1.6 | 4–>16 | >16/>16 | 2.8 |
| Ticarcillin-clavulanate | ≤1–>128 | 4/64 | 67.1 | ≤1–>128 | 4/32 | 88.2 | ≤1–>128 | 32/128 | 87.6 | ≤1–>128 | 8/>128 | 58.5 |
| Piperacillin-tazobactam | ≤0.5–>64 | 2/4 | 95.5 | ≤0.5–>64 | 4/16 | 94.0 | ≤0.5–>64 | 4/32 | 92.4 | ≤0.5–>64 | 4/>64 | 68.8 |
| Cephalosporins | ||||||||||||
| Cefazolin | ≤2–>16 | ≤2/16 | 88.0 | ≤2–>16 | ≤2/>16 | 86.0 | 1–>16 | >16/>16 | 1.1 | ≤2–>16 | >16/>16 | 1.4 |
| Cefuroxime | ≤0.12–>16 | 4/8 | 94.9 | 0.25–>16 | 4/8 | 90.2 | >16 | >16/>16 | 0.0 | 0.5–>16 | >16/>16 | 29.9 |
| Cefoxitin | ≤0.25–>32 | 4/8 | 93.0 | ≤0.25–>32 | 4/8 | 90.5 | 0.5–>32 | >32/>32 | 1.1 | 8–>32 | >32/>32 | 2.0 |
| Cefotaxime-ceftriaxone | ≤0.25–>32 | ≤0.25/≤0.25 | 98.3 | ≤0.25–>32 | ≤0.25/≤0.25 | 97.3 | 0.5–>32 | >32/>32 | 18.5 | ≤0.25–>32 | 0.5/>32 | 69.5 |
| Ceftazidime | ≤0.12–>16 | ≤0.12/0.5 | 98.0 | ≤2–>16 | 0.25/1 | 96.4 | 1–>16 | 2/16 | 87.1 | ≤0.25–>16 | 0.5/>16 | 69.4 |
| Cefepime | ≤0.12–16 | ≤0.12/0.25 | 99.3 | ≤0.12–>16 | ≤0.12/0.25 | 98.7 | 0.5–>16 | 2/16 | 87.0 | ≤0.12–>16 | ≤0.12/4 | 99.3 |
| Others | ||||||||||||
| Aztreonam | ≤0.12–>16 | ≤0.12/≤0.12 | 97.6 | ≤0.12–>16 | ≤0.12/0.25 | 96.1 | 0.25–>16 | 8/>16 | 77.4 | ≤0.12–>16 | ≤0.12/>16 | 70.7 |
| Imipenem | ≤0.06–2 | 0.25/0.5 | 99.5 | ≤0.06–4 | 0.25/0.5 | 100 | 0.12–>8 | 2/8 | 88.0 | ≤0.06–8 | 0.5/2 | 98.6 |
| Meropenem | ≤0.06–1 | ≤0.06/≤0.06 | 99.6 | ≤0.06–2 | ≤0.06/≤0.06 | 100 | ≤0.06–>8 | 0.5/2 | 95.2 | ≤0.06–>8 | ≤0.06/0.25 | 99.3 |
MIC50, MIC90, and % S are as defined for Table 2. MIC units are micrograms per milliliter.
Numbers in parentheses are numbers of isolates.
TABLE 9.
Activities and spectra of activity of 11 representatives of non-β-lactam drug classes tested against the four most prevalent causes of gram-negative bacteremia in Canada
| Antimicrobial class and agent tested | Activity againsta:
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
E. coli (181)
|
Klebsiella (53)
|
P. aeruginosa (45)
|
Enterobacter (34)
|
|||||||||
| MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | |
| Aminoglycosides | ||||||||||||
| Amikacin | ≤0.25–>32 | 4/8 | 98.9 | 0.5–8 | 2/4 | 100 | 0.5–>32 | 4/16 | 95.5 | 1–>32 | 2/4 | 96.9 |
| Gentamicin | ≤0.12–>16 | 1/4 | 94.3 | ≤0.12–>16 | 0.5/2 | 94.1 | 0.25–>16 | 2/8 | 84.1 | 0.5–2 | 1/2 | 100 |
| Tobramycin | ≤0.12–>16 | 94.4 | 96.7 | 0.25–16 | 1/1 | 96.1 | ≤0.012–>16 | 1/2 | 95.5 | 0.5–>16 | 1/1 | 96.9 |
| Fluoroquinolones | ||||||||||||
| Ciprofloxacin | ≤0.015–>2 | ≤0.015/0.06 | 96.6 | ≤0.015–>2 | 0.3/0.12 | 98.0 | 0.03–>2 | 0.12/>2 | 79.5 | ≤0.015–0.25 | ≤0.015/0.06 | 100 |
| Ofloxacin | ≤0.03–>4 | 0.06/0.12 | 96.6 | ≤0.03–>4 | 0.12/0.25 | 98.0 | 0.25–>4 | 1/>4 | 63.6 | 0.06–0.12 | 0.12/0.12 | 100 |
| Levofloxacin | ≤0.5–>4 | ≤0.5/≤0.5 | 97.2 | ≤0.5–>4 | ≤0.5/≤0.5 | 98.0 | ≤0.5–>4 | ≤0.5/>4 | 70.5 | ≤0.5 | ≤0.5/≤0.5 | 100 |
| Sparfloxacinc | ≤0.25–>2 | ≤0.25/≤0.25 | —b | ≤0.025–>2 | ≤0.25/≤0.25 | — | ≤0.25–>2 | 1/>2 | — | ≤0.25 | ≤0.25/≤0.25 | — |
| Gatifloxacinc | ≤0.03–>4 | ≤0.03/0.06 | — | ≤0.03–>4 | 0.06/0.25 | — | 0.06–>4 | 1/>4 | — | ≤0.03–0.5 | 0.06/0.12 | — |
| Trovafloxacinc | ≤0.03–>4 | ≤0.03/0.12 | — | ≤0.03–>4 | 0.06/0.25 | — | ≤0.03–>4 | 0.5/>4 | — | ≤0.03–0.5 | 0.06/0.12 | — |
| Others | ||||||||||||
| Tetracycline | ≤4–>8 | ≤4/>8 | 73.3 | ≤4–>8 | ≤4/>8 | 80.4 | ≤4–>8 | >8/>8 | 4.5 | ≤4–>8 | ≤4/≤4 | 93.8 |
| Trimethoprim-sulfamethoxazole | ≤0.5–>1 | ≤0.5/>1 | 80.7 | ≤0.5–>1 | ≤0.5/>1 | 82.4 | ≤0.5–>1 | >1/>1 | 2.3 | ≤0.5–>1 | ≤0.5/≤0.5 | 96.9 |
TABLE 7.
Activities and spectra of activity of 11 representatives of non-β-lactam drug classes tested against the four most prevalent causes of gram-negative bacteremia in the United States
| Antimicrobial class and agent tested | Activity againsta:
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
E. coli (769)
|
Klebsiella (311)
|
P. aeruginosa (189)
|
Enterobacter (151)
|
|||||||||
| MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | |
| Aminoglycosides | ||||||||||||
| Amikacin | 1–>32 | 4/8 | 98.5 | ≤0.25–32 | 2/4 | 99.0 | ≤0.25–>32 | 4/8 | 98.4 | ≤0.25–16 | 2/4 | 100 |
| Gentamicin | ≤0.12–>16 | 1/2 | 96.0 | ≤0.12–>16 | 1/1 | 95.3 | ≤0.12–>16 | 2/8 | 89.7 | 0.25–>16 | 1/2 | 94.3 |
| Tobramycin | ≤0.12–>16 | 1/2 | 96.7 | ≤0.12–>16 | 1/1 | 95.1 | ≤0.12–>16 | 1/2 | 95.7 | 0.25–>16 | 1/2 | 93.9 |
| Fluoroquinolones | ||||||||||||
| Ciprofloxacin | ≤0.015–>2 | ≤0.015/0.03 | 97.2 | ≤0.015–>2 | 0.03/0.25 | 96.3 | 0.03–>2 | 0.12/2 | 89.1 | ≤0.015–>2 | 0.03/0.5 | 92.2 |
| Ofloxacin | ≤0.03–>4 | 0.06/0.12 | 97.1 | ≤0.03–>4 | 0.12/0.5 | 96.1 | 0.12–>4 | 1/>4 | 80.6 | ≤0.03–>4 | 0.12/2 | 91.2 |
| Levofloxacin | ≤0.5–>4 | ≤0.5/≤0.5 | 97.6 | ≤0.05–>4 | ≤0.5/≤0.5 | 97.7 | ≤0.5–>4 | ≤0.5/4 | 84.9 | ≤0.5–>4 | ≤0.5/1 | 93.2 |
| Sparfloxacinc | ≤0.25–>2 | ≤0.25/≤0.25 | —b | ≤0.25–>2 | ≤0.25/≤0.25 | — | ≤0.25–>2 | 1/>2 | — | ≤0.25–>2 | ≤0.25/1 | — |
| Gatifloxacinc | ≤0.03–>4 | ≤0.03/0.06 | — | ≤0.03–>4 | 0.12/0.25 | — | 0.25–>4 | 1/>4 | — | ≤0.03–>4 | 0.06/0.5 | — |
| Trovafloxacinc | ≤0.03–>4 | ≤0.03/0.12 | — | ≤0.03–>4 | 0.12/0.5 | — | 0.06–>4 | 0.5/4 | — | ≤0.03–>4 | 0.12/0.5 | — |
| Others | ||||||||||||
| Tetracycline | ≤4–>8 | ≤4/>8 | 72.5 | ≤4–>8 | ≤4/8 | 85.4 | ≤4–>8 | >8/>8 | 3.3 | ≤4–>8 | ≤4/8 | 83.0 |
| Trimethoprim-sulfamethoxazole | ≤0.5–>1 | ≤0.5/>1 | 74.3 | ≤0.5–>1 | ≤0.5/>1 | 87.4 | ≤0.5–>1 | >1/>1 | 2.2 | ≤0.5–>1 | ≤0.5/>1 | 84.4 |
TABLE 8.
Activities and spectra of activity of 15 β-latam antimicrobial agents tested against the four most prevalent causes of gram-negative bacteremia in Canada (33% of all bacteremic episodes)
| Antimicrobial class and agent tested | Activitya againstb:
|
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
E. coli (181)
|
Klebsiella (53)
|
P. aeruginosa (45)
|
Enterobacter (34)
|
|||||||||
| MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | MIC range | MIC50/ MIC90 | % S | |
| Penicillins | ||||||||||||
| Ampicillin-amoxicillin | 1–>16 | 8/16 | 54.0 | 4–>16 | >16/>16 | 2.0 | 8–>16 | >16/>16 | 2.3 | >16 | >16/>16 | 0.0 |
| Piperacillin | ≤1–>128 | 2/>128 | 59.9 | 2–>128 | 8/>128 | 78.4 | ≤1–>128 | 4/32 | 95.5 | ≤1–>128 | 2/>128 | 84.4 |
| Ticarcillin | ≤1–>128 | 8/>128 | 57.1 | 4–>128 | >128/>128 | 3.9 | 8–>128 | 16/64 | 90.9 | ≤1–>128 | 4/>128 | 71.9 |
| Amoxicillin-clavulanate | 1–>16 | 8/>16 | 67.0 | 1–>16 | 4/8 | 90.2 | 1–>16 | >16/>16 | 2.3 | 2–>16 | >16/>16 | 3.1 |
| Ticarcillin-clavulanate | ≤1–>128 | 4/128 | 72.3 | ≤1–>128 | 4/16 | 90.2 | 4–>128 | 32/64 | 90.9 | ≤1–>128 | 2/128 | 71.9 |
| Piperacillin-tazobactam | ≤0.5–>64 | 2/8 | 95.5 | ≤0.5–>64 | 4/16 | 90.2 | 1–>64 | 4/64 | 95.5 | 1–>64 | 2/16 | 93.8 |
| Cephalosporins | ||||||||||||
| Cefazolin | ≤2–>16 | ≤2/16 | 86.4 | ≤2–>16 | ≤2/8 | 92.2 | ≤2–>16 | >16/>16 | 2.3 | ≤2–>16 | >16/>16 | 3.1 |
| Cefuroxime | 0.5–>16 | 4/8 | 94.9 | 0.5–>16 | 2/8 | 96.1 | >16 | >16/>16 | 0.0 | 2–>16 | 16/>16 | 37.5 |
| Cefoxitin | ≤0.25–>32 | 4/8 | 93.2 | 1–>32 | 4/8 | 94.1 | >16 | >32/>32 | 0.0 | 2–>32 | >32/>32 | 6.3 |
| Cefotaxime-ceftriaxone | ≤0.25–32 | ≤0.25/≤0.25 | 99.4 | ≤0.25–>32 | ≤0.25/≤0.25 | 96.1 | 2–>32 | 32/>32 | 18.2 | ≤0.25–>32 | ≤0.25/4 | 93.8 |
| Ceftazidime | ≤0.12–>16 | ≤0.12/0.5 | 98.9 | ≤0.12–16 | ≤0.12/0.5 | 98.0 | 0.5–16 | 2/16 | 86.4 | ≤0.12–>16 | 0.25/2 | 93.8 |
| Cefepime | ≤0.12–4 | ≤0.12/0.25 | 100 | ≤0.12–16 | ≤0.12/0.25 | 98.0 | 0.5–>16 | 2/16 | 84.1 | ≤0.12–4 | ≤0.12/0.5 | 100 |
| Others | ||||||||||||
| Aztreonam | ≤0.12–>16 | ≤0.12/≤0.25 | 98.3 | ≤0.12–>16 | ≤0.12/≤0.12 | 98.0 | 0.5–>16 | 4/16 | 70.5 | ≤0.12–>16 | ≤0.12/0.5 | 93.8 |
| Imipenem | ≤0.06–8 | 0.25/0.5 | 99.4 | 0.12–2 | 0.25/1 | 100 | ≤0.06–>8 | 2/>8 | 72.7 | 0.12–2 | 0.5/1 | 100 |
| Meropenem | ≤0.06–8 | ≤0.06/≤0.06 | 99.4 | ≤0.06–0.5 | ≤0.06/≤0.06 | 100 | ≤0.06–>8 | 0.5/8 | 88.6 | ≤0.06–0.12 | ≤0.06/≤0.06 | 100 |
MIC50, MIC90, and % S are as defined for Table 2.
Numbers in parentheses are numbers of isolates.
As for E. coli, there were no important differences in the susceptibility profiles of Klebsiella sp. BSI isolates from the United States and Canada. Piperacillin-tazobactam (90.2 to 94% susceptible) and cefepime (98 to 98.7% susceptible) were the most active agents among the penicillins and cephalosporins, respectively. Approximately 2 to 4% of Klebsiella sp. BSI isolates exhibited an ESBL phenotype (resistant to ceftazidime) (14). All of the Klebsiella spp. were susceptible to meropenem and imipenem. As with E. coli, the aminoglycosides and fluoroquinolones retained activity against Klebsiella spp.
Comparable susceptibilities to piperacillin (93 versus 95.5%), piperacillin-tazobactam (92.4 versus 95.5%), ceftazidime (87.1 versus 86.4%), and cefepime (87 versus 84.1%) were observed for P. aeruginosa BSI isolates from the United States and Canada, respectively. The Canadian P. aeruginosa isolates were less susceptible than the U.S. isolates to the carbapenems (72.7 to 88.6% versus 88 to 95.2%), aztreonam (70.5 versus 77.4%), and the fluoroquinolones (63.6 to 79.5% versus 80.6 to 89.1%). Against these isolates, meropenem was the most active of the carbapenems (88.6 to 95.2% susceptible) and ciprofloxacin was the most active of the fluoroquinolones (79.5 to 89.1% susceptible). Not surprisingly, tobramycin (95.5 to 95.7% susceptible) and amikacin (95.5 to 98.4% susceptible) were more active than gentamicin (84.1 to 89.7% susceptible).
The Enterobacter sp. BSI isolates from Canada were substantially more susceptible than those from the United States to virtually every class of antimicrobial agent tested in this study. Canadian Enterobacter sp. isolates were more susceptible than U.S. isolates to piperacillin (84.4 versus 63.9%), piperacillin-tazobactam (93.8 versus 68.8%), ticarcillin (71.9 versus 59.2%), and ticarcillin-clavulanate (71.9 versus 58.5%). Among the cephalosporins, carbapenems, and monobactams, cefepime (99.3 and 100% susceptible), meropenem (99.3 and 100% susceptible), and imipenem (98.6 and 100% susceptible) were highly active against both U.S. and Canadian isolates, but ceftazidime (69.4 versus 93.8% susceptible), cefotaxime-ceftriaxone (69.5 versus 93.8% susceptible), and aztreonam (70.7 versus 93.8% susceptible) were more active against Canadian isolates. The aminoglycosides and fluoroquinolones inhibited the majority of Enterobacter sp. isolates; however, 6.8 to 8.8% of U.S. isolates were resistant to fluoroquinolones, whereas none of the Canadian isolates were resistant to these agents. Canadian isolates were also more susceptible to tetracycline (93.8 versus 83%) and trimethoprim-sulfamethoxazole (96.9 versus 84.4%) than U.S. isolates.
Antimicrobial susceptibilities of selected nosocomial and community-acquired pathogens.
Among the 4,119 BSI isolates from U.S. centers, 819 (20%) were determined to be of nosocomial origin (obtained after ≥72 h in hospital), 1,481 (36%) were nonnosocomial or community acquired, and for 1,819 (44%) the status (nosocomial versus community acquired) could not be ascertained. Although differences in the rank orders of the various pathogens between nosocomial and community-acquired BSI were observed, S. aureus, CoNS, enterococci, and E. coli accounted for >50% of infections in both groups (data not shown). In order to evaluate and compare antimicrobial resistance in nosocomial and community settings, the eight sentinel antimicrobial-organism combinations designated by Archibald et al. (1) were selected (Table 10). These combinations included oxacillin-S. aureus, oxacillin-CoNS, ceftazidime-Enterobacter cloacae, ceftazidime-P. aeruginosa, imipenem-P. aeruginosa, ceftazidime-E. coli, ciprofloxacin-E. coli, and vancomycin-Enterococcus spp. The extent of antimicrobial resistance in nosocomial BSI isolates was higher than that in isolates from community-acquired BSI for all of the antimicrobial-organism combinations except ciprofloxacin-E. coli (Table 10).
TABLE 10.
Antimicrobial resistance in bloodstream isolates from nosocomial versus community-acquired infections for selected antimicrobial pathogen combinations
| Organism | Antimicrobial agent | % Resistant (no. tested)
|
|
|---|---|---|---|
| Nosocomial | Community | ||
| S. aureus | Oxacillin | 31 (193) | 25.1 (370) |
| CoNS | Oxacillin | 68 (144) | 41.5 (142) |
| E. cloacae | Ceftazidime | 38.5 (39) | 19.2 (26) |
| P. aeruginosa | Ceftazidime | 7.8 (51) | 1.9 (52) |
| Imipenem | 13.7 (51) | 5.8 (52) | |
| E. coli | Ceftazidime | 7.3 (55) | 0.6 (360) |
| Ciprofloxacin | 1.7 (58) | 1.1 (360) | |
| Enterococcus spp. | Vancomycin | 20 (130) | 7.1 (84) |
DISCUSSION
It is abundantly clear that surveillance programs are necessary to identify changes in the spectrum of microbial pathogens causing serious infection and to monitor trends in antimicrobial resistance patterns in nosocomial and community-acquired infections (1, 8, 9, 15, 16). The information gleaned from surveillance efforts is integral to the design of empirical approaches to the therapy of serious infection and also to defining appropriate control measures for antimicrobial-resistant pathogens (1, 8, 9). Such information has been provided in recent years by programs such as the National Nosocomial Infection Surveillance (NNIS) system (4, 6), the Surveillance and Control of Pathogens of Epidemiologic Importance (SCOPE) program (10, 11, 17, 21), and the Intensive Care Antimicrobial Resistance Epidemiology (ICARE) project (1). These programs have been limited by their focus on nosocomial infections (NNIS and SCOPE) and by the lack of validated identification and antimicrobial susceptibility testing performed in a central laboratory (NNIS and ICARE). The SENTRY program was initiated in January 1997 and was designed to monitor the spectrum of microbial pathogens and antimicrobial resistance trends for both nosocomial and community-acquired infections on a broad geographic scale by using validated reference quality identification and susceptibility testing methods performed in a central laboratory. Because rapid communication and dissemination of information is an important component of any surveillance program, we are summarizing the first 6 months of data for BSI in the present report.
The early findings of the SENTRY Program for BSI (objective A) underscore the prominence of gram-positive cocci and E. coli as etiologic agents of both community-acquired and nosocomial BSI (Table 1). These findings are consistent with the recent observations of Weinstein et al. (22) and also confirm those of the NNIS (3, 5, 7) and SCOPE (10, 11) programs regarding the importance of staphylococci and enterococci.
The most striking finding of the SENTRY program was the degree of antimicrobial resistance among key pathogens in the United States (Table 10). Resistance to oxacillin among staphylococci, to vancomycin among enterococci, and to ceftazidime among Enterobacter spp. was observed for nosocomial and community-acquired pathogens alike. It is notable that in almost every instance the percentage of resistant strains was higher among nosocomial isolates than among those from the community (Table 10). Unfortunately, this analysis is compromised by the fact that for 44% of the BSI the status of nosocomial or community acquired could not be confirmed. Thus, although the apparent increased resistance among nosocomial BSI isolates compared to those from the community is consistent with that reported by Archibald et al. (1) for the ICARE program, these findings must be tempered by the fact that a large number of isolates were excluded from the analysis.
Of note, in the current survey, among 209 bloodstream isolates of S. pneumoniae in the United States, 59.0% were susceptible to penicillin; in Canada, 69.5% of 59 isolates were susceptible. In objective B of the SENTRY study (data not shown), the percentage of penicillin-susceptible strains among 845 outpatient respiratory tract isolates of S. pneumoniae collected during roughly the same period in the United States was 56.2%; among 202 such isolates in Canada, 69.2% were susceptible. In other words currently there exist only minor differences in rates of penicillin resistance among bloodstream versus respiratory tract isolates of S. pneumoniae in North America. Comparisons of resistance rates with other antimicrobial agents revealed the same degree of concordance between bloodstream and respiratory tract isolates of the pneumococci.
Although the rank orders of pathogens in the United States and Canada were very similar (Table 1), distinct differences were observed in the antimicrobial susceptibilities of several pathogens. Overall, U.S. isolates were considerably more resistant than those from Canada. This was most apparent with S. aureus, Enterococcus spp., and Enterobacter spp. For oxacillin-resistant S. aureus, vancomycin-resistant enterococci, and ceftazidime-resistant Enterobacter spp., the percentages of resistant U.S. isolates were 26, 17.7, and 30.6%, respectively; the corresponding values for resistant Canadian isolates were 2.7, 0, and 6.2%, respectively. This comparison dramatically emphasizes the differences and points to the relative lack of specific antimicrobial resistance genes (mecA, vanA, and vanB) in the Canadian microbial population. The in vitro susceptibilities of U.S. and Canadian E. coli, Klebsiella spp., and P. aeruginosa were generally comparable, although the Canadian P. aeruginosa isolates were somewhat less susceptible than U.S. isolates to carbapenems and fluoroquinolones. The reasons for these differences in antimicrobial susceptibility are unclear but may be due to differences in antimicrobial utilization practices.
Although high rates of antimicrobial resistance were observed in this survey, there were several encouraging observations regarding specific antimicrobial agents. First, we did not observe any vancomycin-resistant or -intermediate strains among 1,829 U.S. and Canadian isolates of staphylococci. Second, the investigational agent quinupristin-dalfopristin appeared to be quite active against oxacillin-resistant staphylococci, vancomycin-resistant E. faecium, and penicillin-resistant S. pneumoniae. Third, the extended-spectrum cephalosporin cefepime and the carbapenems imipenem and meropenem were highly active against the major gram-negative BSI pathogens, including those strains of Enterobacteriaceae that were resistant to ceftazidime and other extended-spectrum β-lactam and monobactam agents.
In conclusion, ongoing surveillance of microbial pathogens and their resistance profiles is essential on national and international scales. The SENTRY program will continue to monitor these trends in both nosocomial and community-acquired BSI. Comparisons of the results both internally within the SENTRY program and with other ongoing programs such as NNIS and ICARE will enhance our knowledge base regarding the problem of antimicrobial resistance and will serve as a basis for policies and practices that might serve to limit the scope and magnitude of this problem.
ACKNOWLEDGMENTS
Kay Meyer provided excellent support in the preparation of this paper. We express our appreciation to all SENTRY participants.
The SENTRY program was sponsored by a research grant from Bristol-Myers Squibb.
Appendix
SENTRY participants contributing data and/or isolates to the study include Lynn Steele-Moore, The Medical Center of Delaware, Wilmington; Gerald Denys, Methodist Hospital of Indiana, Indianapolis; Carol Staley, Henry Ford Hospital, Detroit, Mich.; Joseph R. Dipersio, Summa Health Systems, Akron, Ohio; Michael Saubolle, Good Samaritan Regional Medical Center, Phoenix, Ariz.; Michael L. Wilson, Denver General Hospital, Denver, Colo.; Gary D. Overturf, University of New Mexico Hospital, Albuquerque; Lance R. Peterson, Northwestern Memorial Hospital, Chicago, Ill.; Paul C. Schreckenberger, University of Illinois at Chicago, Chicago; Ronald N. Jones, University of Iowa Hospitals and Clinics, Iowa City; Stephen Cavalieri, Creighton University, Omaha, Neb.; Sue Kehl, Froedtert Memorial Lutheran Hospital-East, Milwaukee, Wis.; Stephen Brecher, Boston VAMC, Boston, Mass.; Phyllis Della-Latta, Columbia Presbyterian Medical Center, New York, N.Y.; Henry Isenberg, Long Island Jewish Medical Center, New Hyde Park, N.Y.; Dwight Hardy, Strong Memorial Hospital, Rochester, N.Y.; Dennis Koga, St. Jude Medical Center, Fullerton, Calif.; Judy Fusco, Kaiser Laboratory, Berkeley, Calif.; Marcy Hoffmann, Sacred Heart Medical Center, Spokane, Wash.; Thomas Fritsche, University of Washington, Seattle; Patrick R. Murray, Barnes-Jewish Hospital, St. Louis, Mo.; Paul Southern, Parkland Health and Hospital System, Dallas, Tex.; Audrey Wanger, The University of Texas Medical School, Houston; Gail L. Woods, University of Texas Medical Branch at Galveston, Galveston; Joseph Chiao, University Medical Center, Jacksonville, Fla.; James Snyder, University of Louisville Hospital, Louisville, Ky.; Joe Humphrey, University of Mississippi Medical Center, Jackson; Steve Jenkins, Carolinas Medical Center, Charlotte, N.C.; Kevin Hazen, University of Virginia Health Sciences Center, Charlottesville; Robert Rennie, University of Alberta Hospital, Edmonton, Alberta, Canada; Michael Noble, The Vancouver Hospital and Health Science Center, Vancouver, British Columbia, Canada; Daryl Hoban, Health Sciences Centre, Winnipeg, Manitoba, Canada; Kevin Forward, Queen Elizabeth II Health Sciences Centre, Halifax, Nova Scotia, Canada; Don Low, Mount Sinai Hospital, Toronto, Ontario, Canada; Baldwin Toye, Ottawa General Hospital, Ottawa, Ontario, Canada; Andrew Simor, Sunnybrook Health Science Centre, Toronto, Ontario, Canada; Susan Richardson, The Hospital for Sick Children, Toronto, Ontario, Canada; Hugh Robson, Royal Victoria Hospital, Montreal, Quebec, Canada; Joseph Blondeau, Royal University Hospital, Saskatoon, Saskatchewan, Canada.
REFERENCES
- 1.Archibald L, Phillips L, Monnet D, McGowan J E, Jr, Tenover F, Gaynes R. Antimicrobial resistance in isolates from inpatients and outpatients in the United States: increasing importance of the intensive care unit. Clin Infect Dis. 1997;24:211–215. doi: 10.1093/clinids/24.2.211. [DOI] [PubMed] [Google Scholar]
- 2.Ballow C H, Schentag J J. Trends in antibiotic utilization and bacterial resistance: report of the National Nosocomial Resistance Surveillance Group. Diagn Microbiol Infect Dis. 1992;15:37S–42S. [PubMed] [Google Scholar]
- 3.Banerjee, S. N., T. G. Emori, D. H. Culver, R. P. Gaynes, W. R. Jarvis, T. Horan, J. R. Edwards, J. Tolson, T. Henderson, and W. J. Martone. 1991. Secular trends in nosocomial primary bloodstream infections in the United States, 1980–1989. Am. J. Med. 91(Suppl. 3B):86S–89S. [DOI] [PubMed]
- 4.Emori T G, Culver D H, Horan T C. National Nosocomial Infections Surveillance (NNIS) system: description of surveillance methods. Am J Infect Control. 1991;19:19–35. doi: 10.1016/0196-6553(91)90157-8. [DOI] [PubMed] [Google Scholar]
- 5.Emori T G, Gaynes R P. An overview of nosocomial infections, including the role of the microbiology laboratory. Clin Microbiol Rev. 1993;6:428–442. doi: 10.1128/cmr.6.4.428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jarvis, W. R., J. R. Edwards, D. H. Culver, J. M. Hughes, T. C. Horan, T. G. Emori, S. N. Banerjee, J. S. Tolson, T. S. Henderson, R. P. Gaynes, and W. J. Martone. 1991. Nosocomial infection rates in adult and pediatric intensive care units in the United States. Am. J. Med. 91(Suppl. 3B):185S–191S. [DOI] [PubMed]
- 7.Jarvis, W. R., and W. J. Marton. 1992. Predominant pathogens in hospital infections. J. Antimicrob. Chemother. 29(Suppl. A):19–24. [DOI] [PubMed]
- 8.Jones R N. The emergent needs for basic research, education, and surveillance of antimicrobial resistance. Diagn Microbiol Infect Dis. 1996;25:1–9. doi: 10.1016/s0732-8893(96)00099-5. [DOI] [PubMed] [Google Scholar]
- 9.Jones R N, Kehrberg E N, Erwin M E, Anderson S C the Fluoroquinolone Resistance Surveillance Group. Prevalence of important pathogens and antimicrobial activity of parenteral drugs at numerous medical centers in the United States. I. Study on the threat of emerging resistances: real or perceived? Diagn Microbiol Infect Dis. 1994;19:203–215. doi: 10.1016/0732-8893(94)90033-7. [DOI] [PubMed] [Google Scholar]
- 10.Jones R N, Marshall S A, Pfaller M A, Wilke W W, Hollis R J, Erwin M E, Edmond M B, Wenzel R P the SCOPE Hospital Study Group. Nosocomial enterococcal bloodstream infections in the SCOPE Program: antimicrobial resistance, species occurrence, molecular testing results, and laboratory testing accuracy. Diagn Microbiol Infect Dis. 1997;29:95–102. doi: 10.1016/s0732-8893(97)00115-6. [DOI] [PubMed] [Google Scholar]
- 11.Marshall S A, Wilke W W, Pfaller M A, Jones R N. Staphylococcus aureus and coagulase-negative staphylococci from blood stream infections: frequency of occurrence, antimicrobial susceptibility, and molecular (mec A) characterization of oxacillin resistance in the SCOPE Program. Diagn Microbiol Infect Dis. 1998;30:205–214. doi: 10.1016/s0732-8893(97)00212-5. [DOI] [PubMed] [Google Scholar]
- 12.Murray P R, Baron E J, Pfaller M A, Tenover F C, Yolken R H, editors. Manual of clinical microbiology. 6th ed. Washington, D.C: ASM Press; 1995. [Google Scholar]
- 13.National Committee for Clinical Laboratory Standards. Methods for dilution antimicrobial tests for bacteria that grow aerobically. Approved standard M7-A4. Wayne, Pa: National Committee for Clinical Laboratory Standards; 1997. [Google Scholar]
- 14.National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing. Supplemental tables, M100-S8. Wayne, Pa: National Committee for Clinical Laboratory Standards; 1998. [Google Scholar]
- 15.Osterholm M T, MacDonald K L. Antibiotic-resistant bugs: when, where, and why? Infect Control Hosp Epidemiol. 1995;16:382–384. doi: 10.1086/647134. [DOI] [PubMed] [Google Scholar]
- 16.Paul S M, Finelli L, Crane G L, Spitalny K C. A statewide surveillance system for antimicrobial-resistant bacteria: New Jersey. Infect Control Hosp Epidemiol. 1995;16:385–390. doi: 10.1086/647135. [DOI] [PubMed] [Google Scholar]
- 17.Pfaller M A, Jones R N, Marshall S A, Coffman S L, Hollis R J, Edmond M B, Wenzel R P. Inducible Amp C β-lactamase producing Gram-negative bacilli from bloodstream infections: frequency, antimicrobial susceptibility, and molecular epidemiology in a national surveillance program (SCOPE) Diagn Microbiol Infect Dis. 1997;28:211–219. doi: 10.1016/s0732-8893(97)00064-3. [DOI] [PubMed] [Google Scholar]
- 18.Pinner R W, Teutseh S M, Simonsen L, Klug L A, Graber J M, Clarke M J, Berkelman R L. Trends in infectious disease mortality in the United States. JAMA. 1996;275:189–193. [PubMed] [Google Scholar]
- 19.Pittet D, Li N, Woolson R F, Wenzel R P. Microbiological factors influencing the outcome of nosocomial bloodstream infections: a 6-year validated, population-based model. Clin Infect Dis. 1997;24:1068–1078. doi: 10.1086/513640. [DOI] [PubMed] [Google Scholar]
- 20.Reimer L G, Wilson M L, Weinstein M P. Update on detection of bacteremia and fungemia. Clin Microbiol Rev. 1997;10:444–465. doi: 10.1128/cmr.10.3.444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Voelker R. New group tracks hospital’s drug-resistant bugs. JAMA. 1996;275:177–178. [PubMed] [Google Scholar]
- 22.Weinstein M P, Towns M L, Quartey S M, Mirrett S, Reimer L G, Parmigiani G, Reller L B. The clinical significance of positive blood cultures in the 1990s: a prospective comprehensive evaluation of microbiology, epidemiology, and outcome of bacteremia and fungemia in adults. Clin Infect Dis. 1997;24:584–602. doi: 10.1093/clind/24.4.584. [DOI] [PubMed] [Google Scholar]