Abstract
Background
Bystander cardiopulmonary resuscitation (CPR) is the cornerstone in managing out-of-hospital cardiac arrest (OHCA). However, India lacks a formal sudden cardiac arrest (SCA) registry and the infrastructure for a robust emergency medical services (EMS) response system. Also, there exists an opportunity to improve widespread health literacy and awareness regarding SCA. Other confounding variables, including religious, societal, and cultural sentiments hindering timely intervention, need to be considered for better SCA outcomes.
Objectives
We highlight the current trends and practices of managing OHCA in India and lay the groundwork for improving the awareness, education, and infrastructure regarding the management of SCA.
Conclusion
Effective management of OHCA in India needs collaborative grassroots reformation. Establishing a large-scale SCA registry and creating official and societal guidelines will be pivotal for transforming OHCA patient outcomes.
Keywords: Sudden cardiac arrest, Cardiopulmonary resuscitation, India, Reforms
1. Introduction
Out-of-hospital cardiac arrest (OHCA) is a public health burden accounting for nearly 10% of global mortality and 50% of cardiovascular deaths.1, 2, 3 Its worldwide incidence is 55 per 100,000 person-years.1 Providing cardiopulmonary resuscitation (CPR) is the most critical step in the survival link chain of OHCA, and it is imperative to recognize symptoms and signs of sudden cardiac arrest (SCA) to ensure timely intervention.4,5 However, the bystander CPR rate in India is reported to be only 1.3%–9.8%, as per previous studies.6,7 This is far below the target goal of 62% set by the American Heart Association Emergency Cardiovascular Care (AHA-ECC).8 With an estimated survival of less than 10%, OHCA remains one of India's leading causes of death.6,9 In addition, education and awareness regarding the identification of SCA remains low, contributing to poor bystander CPR rates.10,11 Furthermore, emergency medical services (EMS) expansion is needed to ensure shorter wait and ambulance-to-emergency department transfer times.12 We address the current trends and suggest nationwide reforms that can improve the survival rates of patients that have experienced an OHCA.
2. Current evidence and review of literature
Currently, few studies and international registries provide preliminary data on OHCA in India.6,7,13, 14, 15, 16, 17, 18 These studies highlight a staggering rate of bystander CPR ranging from 0% to under 10% in these studies, except for a single study reporting bystander CPR delivery up to 27.8%. (WACAR Study) [Table 1]. We hereby dive in more depth to understand these studies and the implications from their outcomes:
Table 1.
Incidence of out of hospital cardiac arrest (OHCA) and associated bystander CPR resuscitative efforts and AED use in India, as reported in studies and registries.6,7,13, 14, 15, 16, 17, 18
| Study | Publication year | Type of Study | No. of Patient population from India | No./% received CPR | No./% AED use |
|---|---|---|---|---|---|
| P. Sajithkumar, Dr. Ratna Prakash | 2015 | Descriptive Survey | 350 patientsa | 8 patients | Not reported |
| Pandian et al. | 2016 | Retrospective Study | 67 OHCA out of 254 total arrests | 7.4% (5 out of 67 patients) | Not reportedb |
| CARO study | 2017 | Retrospective Study | 80 patientse | 1.3% | Not reported |
| WACAR study | 2020 | Prospective observational study | 574 out of 814c patients with available data | 27.8% (139 of 500 patients) (accounted only for patients with data reported) | 17 out of 44 patients (accounted only for patients with data reported) |
| Bhat R. et al. | 2021 | Observational prospective study | 205 patients | 9.8% | 1% |
| DA-CPR study | 2021 | Prospective, multinational, implementation study | 2775 patientsd (served as control group in the study) | 0% | 0% |
| PAROS registry | 2022 | Registry based study | 2006 patientsd | 0% | Not reported |
Abbreviations:
DA-CPR Dispatcher-Assisted CPR
PAROS Pan-Asian Resuscitation Outcomes Study
WACAR Warangal Area out-of-hospital Cardiac Arrest Registry
Cumulative results from 21 emergency departments from Kerala, India.
Of the total study population of 254 [including both OHCA (67patient) and IHCA (187 patients)], 21 (8%) had shockable rhythms (VT/VF) and received defibrillation. Data on outside hospital AED use not reported.
Patient population from Warangal area, Telangana, India.
Patient population from Telangana, India.
Single center study from New Delhi, India.
Sajithkumar and colleagues reported their multicenter experience in 2015 from 21 emergency room (ER) departments in Kerela, India with a retrospective descriptive study where data were primarily collected from self-reporting and interview of individuals that brought the cardiac arrest victim to the ER. This study showed a dismal 8 out of 350 patients received bystander resuscitation.18 The leading cause for lack of bystander resuscitation was reported to be lack of awareness regarding cardiac arrest and proper training in the general population. Interestingly, 58% of all bystanders were reported to have college education, however only 8 bystanders performed CPR (7 learned from health care professionals, while 1 bystander reported vague knowledge from media/movie). A single center study from Tamil Nadu, India by Pandian et al in 2016 similarly analyzed the outcomes of sudden cardiac death in the ER and the associated bystander resuscitation in both in-hospital and out-of-hospital arrests.14 Out of the 254 cardiac arrests presenting to their ER, 67 (26.4%) were noted to be out of hospital cardiac arrests with only 5 patients that received bystander CPR. Though 76% of the patients from this study had a non-shockable rhythm (and hence not requiring an AED) during the arrest, the authors attribute this characteristic to the group of patients excluded due to direct admission to the chest pain unit and thereafter suffering ventricular arrhythmias. Nonetheless, the study investigators highlighted the overall suboptimal rates of bystander resuscitation. Similarly, CARO study (2017) from the ER department of a multispecialty hospital in urban settings of New Delhi showed that despite 46 out of the 80 patients suffering a witnessed out of hospital cardiac arrest [most commonly in residential settings (92%)], only 1 patient received bystander CPR.6 26 patients in this study had survival to hospital admission, but only 3 out of 7 discharged patients had favorable neurological outcomes. A similar study from a tertiary care hospital in Manipal was undertaken by Bhat et al (2021) underpinning the evidence of dismal bystander CPR rates.7 With 205 patients in this prospective observational study, only 9.8% (20 patients) received bystander CPR (15 out of 20 received CPR in the ambulance). Importantly, this study highlighted that 41.5% of patients were brought to the hospital by means other than ambulance, while only 12.5% of the ambulance had BLS trained personnel. WACAR study (2020) is the largest prospective observation study from Warangal region with inclusion of 814 patients with non-traumatic out of hospital cardiac arrest (OHCA).13 Despite attrition of data due to reporting bias, this study extensively highlights several factors that play a role in lower bystander CPR rates. With symptom onset up to an hour preceding the cardiac arrest, only a small proportion [38 out of 159 patients (24%)] of reported cases contacted any physician to seek medical advice. 27.8% out of 500 patients received CPR. The study also sheds light on the delay in initiation of CPR, underutilization of ambulance services and delay in time of arrival of EMS.
Recently, two international studies/registries have added similar evidence to the dismal bystander CPR rates in India with DA-CPR study (2021) (reporting none out of the 2775 patients receiving bystander CPR) and PAROS registry (2022) (reporting none out of the 2006 patients receiving bystander CPR).15,19
3. Recent trends and practices
Efforts for population-based awareness regarding sudden cardiac death and importance of bystander CPR are scattered and underwhelming. Currently, there is no legislation mandating CPR training for employees working in major institutions, students in schools or for those acquiring important official documents (for e.g. Passport, driver's license, Aadhar Card etc). In 2017, the Indian Resuscitation Council (IRC), an initiative of Indian Society of Anesthesiologists, had created an exemplary guideline document for Compression-only-Life Support (COLS) in keeping with resource constraints, lack of adequate infrastructure, level of literacy among population and cultural constraints.20 However, this document has not been translated into visual infographics yet for better spread of awareness among the masses. IRC has made several efforts to perform large-scale CPR training camps in the past. Similarly, American Heart Association (AHA) has recently started efforts in collaboration with All India Institute of Medical Sciences (AIIMS) to train the community members with bystander CPR with a plan to expansion to over 12 institutions in the country over five years. Since the 1990s, the Indian Government has set up Centralized Accidents and Trauma Services (CATS) which provides two primary emergency response system alerts – 102/108 (free services) and 1298 (paid service). Despite having a centralized number response system and a nationwide expansion, it has failed to gain acceptance equal to western EMS and comparable bystander resuscitative measures.
4. Limitations and challenges
Demographically, similar to global incidences, men are more susceptible to developing SCA than women.13,17,21,22 Globally, advanced age, cardiovascular risk factors, event location, a witnessed versus unwitnessed arrest, a shockable rhythm at onset, time to resuscitation efforts, and bystander CPR have been the driving forces in predicting mortality and morbidity.23, 24, 25, 26 However, for India, in addition to these factors, there are several other contributing factors at different levels that add more challenges to achieving optimal bystander CPR rates.
4.1. National level
We currently lack nationwide uniform initiatives to promote bystander resuscitation. These include, but are not limited to, population-based spread of bystander CPR awareness from ministry of health and state health departments. Our ongoing efforts for promoting bystander CPR training are in isolation in regions or institutions with limited impact. Similarly, previously reported studies have been undertaken by motivated group of researchers in isolation in different regions but lacked at source data collection across the population of interest due to recall bias.
4.2. Institutional level (EMS, hospitals and healthcare providers)
Lack of consistent EMS protocols, limited training in basic (BLS) and advanced cardiac life support (ACLS) (even amongst healthcare professionals), under-resourced and overburdened EMS infrastructure reflected as longer wait times, and lack of ambulance availability leading to utilization of private vehicles have been critical determinants of dismal outcomes from OHCA.27, 28, 29, 30, 31 Even if available, there is a lack of provision of pre-hospital care during transfer to a hospital. These include, but are not limited to, fully equipped ambulances, timely notification of hospital en-route, availability of critical medications and infusions, and understaffed ambulance personnel.7,31 It has also been found that there is underutilization of automated external defibrillator (AED) to perform immediate rhythm analysis and identify shockable rhythms, which have favorable outcomes compared with non-shockable rhythms.7
4.3. Individual level
Inadequate provision of bystander CPR due to cultural factors such as gender, race, and class differences also exist in society due to fear of being judged. Inadequate knowledge and skill of understanding what an OHCA event is, the critical role of survival link associated with resuscitative measures, along with lack of training in performing CPR continue to exist.32 Fear of legal issues or litigations and costs associated with it have also been reported in one of the studies as a factor preventing bystanders from providing CPR. The perceived notion that bystander resuscitation needs formal training in BLS to provide effective CPR can also be accounted for such hesitation in the general population.
5. Proposed reforms
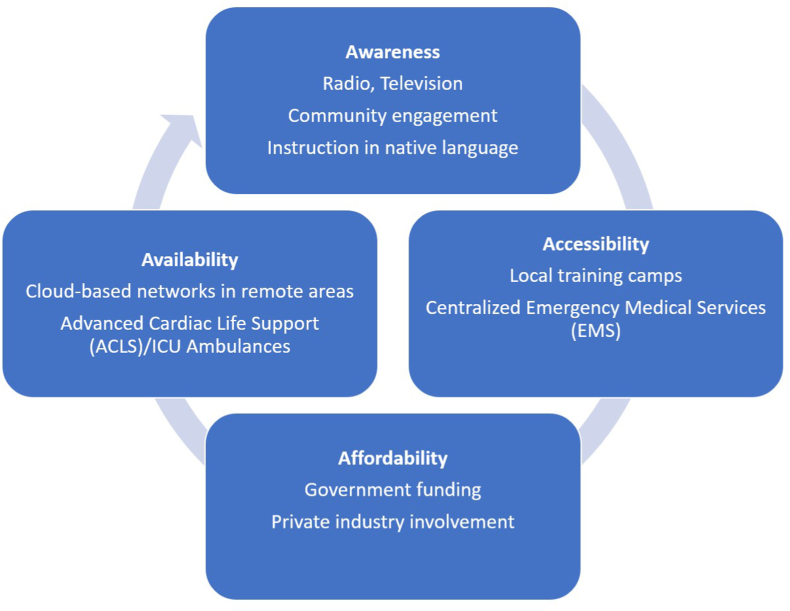
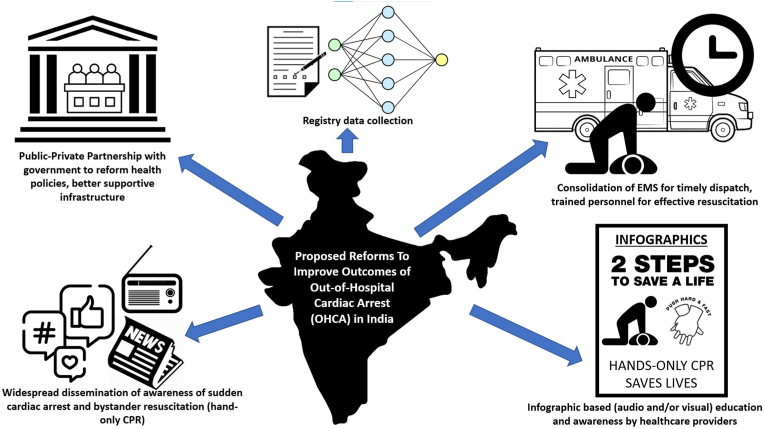
With a population of over 1.3 billion in India, there is a varied socioeconomic and educational skill set within the communities. We suggest reforms addressing the availability of resources to improve survival, accessibility to hands-on only CPR teaching platforms and educational initiatives, and affordability of AEDs (Fig. 1). We expand further on some of these reforms below (Fig. 2).
Fig. 1.
Core structure for proposed reforms.
Fig. 2.
Proposed reforms to improve outcomes of out-of-hospital cardiac arrest (OHCA) in India.
5.1. SCA awareness and role of hands-only CPR
As the efforts to raise such awareness need to be nationwide, we recommend reforms that can be cost-effective for such a large-scale initiative. Televised commercials in various languages and the utilization of widely used social media platforms are ways of reaching the masses. Another effective public service announcement can be the radio, especially in areas with limited telecommunication network systems. In rural areas, volunteers can be recruited to receive formal education in identifying signs and symptoms of OHCA and initial training of BLS, following which regular community training camps can be held by these volunteers overseen by medical personnel from the primary health centers or district hospitals. The goal of these initiatives must focus on helping the general population understand SCA and its presentation, the need for timely intervention, and critical aspects of bystander and community engagement to help save a life by understanding of the chain of survival for adequate resuscitation.
Adequate funding needs to be assigned to purchase mannequins for training purposes and can be sponsored by government-owned organizations like the National Health Mission of the Ministry of Health, the Ayushman Bharat Program, and the Health and Wellness Centers, or as a part of philanthropy efforts. To improve adequate understanding and accessibility, training for hands-only CPR will need to be provided in different regional languages and dialects. These can be simplified with pictographs and voice-over instructions to overcome literacy barriers. An ‘each one, teach one’ model can also be utilized to spread such knowledge and psychomotor skills. Schools in rural and urban areas must have regular classes for students (for instance, on a biannual basis) on identifying the signs and symptoms of OHCA and the subsequent action plan for learning bystander CPR. Posters depicting signs and symptoms of cardiac arrest can also be placed strategically around the city and villages to spread awareness. These can be in an easy-to-read format in various national and regional languages to facilitate accurate content delivery. These efforts should also be supported by prevailing nationwide Good Samaritan Law to help promote the general population to participate in bystander resuscitation efforts without fear of litigation.33
5.2. Role of nationwide OHCA registry
Currently, studies focus on SCA from specific regions and provinces in India. However, a nationwide registry would help identify the actionable items for policymakers to implement changes with the active involvement of key stakeholders. State-level sub-registry data can help specific regions to overcome barriers and challenges resulting from local funding, socioeconomic status and geographic limitations. Due to an inadequate EMS infrastructure, the CARES registry was implemented in Atlanta, Georgia, and later expanded to other cities in the United States.21 India can implement a similar model by identifying areas for piloting resuscitative efforts in certain regions to start a database. Once implemented, such a registry could be compared with registries from other countries to help consolidate resuscitative measures further. The WACAR study serves as a valuable learning experience to understand the factors that resulted in under-reporting, and future efforts can be channeled to build a registry with wider regions of interest and consistent data collection. One crucial measure includes mandating OHCA as a reportable event throughout the nation.
5.3. Centralized EMS response
A centralized EMS response remains a critical challenge in a country of diverse terrain. We propose establishing EMS infrastructure and protocols supported by government funding with a strategic private-public sector partnership. Availing a standard emergency number for EMS services, similar to the 911 service currently employed in the United States, would be ideal. It is also vital to ensure the functionality and accessibility of such emergency numbers, even in poor telecommunication or electricity outages, to continue the availability of critical care services. Incorporating government-subsidized cloud-based networks can help overcome such hurdles. One of the major challenges results from the substantial traffic in poorly planned cities, significant proportion of motorbike use for transportation, and populous neighborhoods, resulting in a delay in EMS response and accessibility. It would be desirable to have ambulances equipped with trained medical personnel well-versed with BLS and ACLS protocols, and critical response resources to account for the delay in reaching a tertiary care center. It is essential to have a portable defibrillator in each ambulance to ensure accurate recognition of heart rhythms and delivery of appropriate shocks. These defibrillators must be equipped with voice commands and visual directions for placing pads that can be tailored to regional languages. With challenging geographic access, local provision of AEDs to healthcare teams at the primary health centers or community centers is another viable idea. Engaging the community and volunteers can help initiate the early chain of survival until more advanced medical assistance arrives. The inaccessible terrains continue to pose a constant threat to resuscitative efforts. Large-scale initiatives with improved accessibility and roads will need to be prioritized by private and public sectors.
5.4. Publicly accessible automated cardiac defibrillators (AEDs)
Our fourth proposed reform is to increase accessibility by placing AEDs in strategic public locations, including malls, movie theatres, buses, trains, temples, churches, mosques, schools, universities, and concert venues. BLS training must be provided to the staff on duty in such locations, including the security personnel, teachers, priests, drivers, and ticket collectors. AED instructions with the visual representation of protocols can be tailored to regional languages to facilitate an easy-to-understand format.
5.5. Social reforms
Our last proposal would be to try and overcome the social, cultural, and societal stigmatization currently associated with providing CPR. One of the most important ones is the delivery of chest compressions to a woman; studies have shown that women are prone to not receiving CPR due to the fear of judgments such as sexual misconduct.34,35 Gender bias that may limit the provision of this life-saving measure in emergencies must be abolished. Women and men must have equal rights and freedom to provide and receive bystander CPR without social, cultural, or societal prejudices. A common myth remains that giving mouth-to-mouth rescue breaths with chest compression is an integral part of successful resuscitation.36,37 We must educate the population that mouth-to-mouth rescue breaths within the BLS protocol are no longer required and that bystander hands-only CPR improves the probability of survival significantly after an OHCA.38 Demystifying incorrect facts should be included in the school and college curricula, and training police personnel, fire officers, and community members should be a priority. Social barriers may require consistent efforts over a long period to change; educating women on identifying SCA and delivering prompt hands-only CPR to other women would be an effective solution in the interim. With different religious beliefs, it is challenging to have different customs and beliefs to help support CPR. Alternatively, organizing hands-only CPR campaigns during major religious events or health camps, and training the religious representatives at places of worship to help deliver the key message may be a vital strategy, as they are idolized by the masses.
Given the emphasis on the Make-in-India policy and the push towards low-cost technologies, the government should encourage manufacturing low-cost portable defibrillators and placements in public locations, public transport networks such as railways, work sites, gyms, large corporate offices, and places of worship. Increasing the government funding at central and state levels, and setting aside budget for the SCA survival improvement strategies are few potential solutions to overcome the affordability barrier. Encouraging private industries to “Adopt-a-region,” to fund AEDs and CPR-education resources will allow for a collaborative reformation. Moreover, a multi-disciplinary teamwork approach that includes engineers from both the public sector (institutions like the Indian Institute of Technology) and the private sector, cardiac electrophysiologists, preventive cardiologists, and patient networks can work collaboratively. Innovative approaches and resources such as “photovoice” can be used to popularize and educate the general public.
6. Conclusion
This review is a starting point for initiating a dialogue regarding OHCA efforts in India. The rapid population expansion, increased longevity, and cardiovascular disease burden contribute to an enormous load on India's healthcare infrastructure. Being proactive with the personalized-for-India OHCA registry will allow us to understand the regional, cultural, and societal factors that interplay with SCA events and responses. We understand that our review scrapes the tip of the iceberg of the complexity of OHCA in India, and that some of these suggested reforms might take a long time to enforce. Moreover, limited resources, health illiteracy, and food and shelter poverty will be potential barriers that need more grassroots engagement of political and public entities, which are out of the limits of medical organizations alone. The cost-effective analysis and health economy data evaluation is out of the scope of our review and is a vital issue that can be investigated in the future.
In conclusion, raising awareness and understanding of SCA, enhancing the training of bystanders, and improving the EMS infrastructure will aid in improving outcomes for patients who suffer an OHCA in India. As India moves towards self-sustenance and reliance in various sectors, we must also make headway in managing OHCA by creating a registry and improving the EMS response system. By doing so, we can gain in-depth knowledge and identify factors responsible for the high mortality and morbidity rates without relying on registries from other countries.
7. Take home summary
-
1.
Bystander cardiopulmonary resuscitation (CPR) rates in India remain dismal resulting in poor survival rates and neurological outcomes. Several factors contribute interchangeably to poor bystander outcomes (mainly lack of awareness and training for bystander CPR, healthcare policies supporting infrastructure for prompt care for OHCA patients, uniform EMS availability and utilization and others).
-
2.
With lack of uniform evidence to explore such limitations from the prior studies, there exists a dire need to establish nationwide registry with state level sub-registries to support healthcare reforms and advocacy measures proposed by government.
-
3.
Tireless efforts for bystander CPR training at different levels of communities, institutions and throughout the nation will help build a nation of lifesavers.
Author contributions
H.P, A.U.M: Prepared, reviewed, and edited the manuscript. L.M., A.K., P.D., R.Y., N.N., K.T.: Reviewed and edited the manuscript.
Disclosures
None.
Funding
No financial support.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The abstract for this manuscript was presented for “Young Investigator Award” at the American Association of Cardiologist of Indian Origin (AACIO) Meeting – March 2023 at New Orleans, Louisiana (United States).
References
- 1.Berdowski J., Berg R.A., Tijssen J.G., Koster R.W. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81(11):1479–1487. doi: 10.1016/j.resuscitation.2010.08.006. [DOI] [PubMed] [Google Scholar]
- 2.Myat A., Song K.J., Rea T. Out-of-hospital cardiac arrest: current concepts. Lancet (London, England) 2018;391(10124):970–979. doi: 10.1016/S0140-6736(18)30472-0. [DOI] [PubMed] [Google Scholar]
- 3.Sasson C., Rogers M.A., Dahl J., Kellermann A.L. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3(1):63–81. doi: 10.1161/CIRCOUTCOMES.109.889576. [DOI] [PubMed] [Google Scholar]
- 4.Ritter G., Wolfe R.A., Goldstein S., et al. The effect of bystander CPR on survival of out-of-hospital cardiac arrest victims. Am Heart J. 1985;110(5):932–937. doi: 10.1016/0002-8703(85)90187-5. [DOI] [PubMed] [Google Scholar]
- 5.Adielsson A., Hollenberg J., Karlsson T., et al. Increase in survival and bystander CPR in out-of-hospital shockable arrhythmia: bystander CPR and female gender are predictors of improved outcome. Experiences from Sweden in an 18-year perspective. Heart. 2011;97(17):1391–1396. doi: 10.1136/hrt.2011.222711. [DOI] [PubMed] [Google Scholar]
- 6.Krishna C.K., Showkat H.I., Taktani M., Khatri V. Out of hospital cardiac arrest resuscitation outcome in North India - CARO study. World J Emerg Med. 2017;8(3):200–205. doi: 10.5847/wjem.j.1920-8642.2017.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhat R., Ravindra P., Sahu A.K., Mathew R., Wilson W. Study of pre-hospital care of out of hospital cardiac arrest victims and their outcome in a tertiary care hospital in India. Indian Heart J. 2021;73(4):446–450. doi: 10.1016/j.ihj.2021.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kronick S.L., Kurz M.C., Lin S., et al. Part 4: systems of care and continuous quality improvement: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18 Suppl 2):S397–S413. doi: 10.1161/CIR.0000000000000258. [DOI] [PubMed] [Google Scholar]
- 9.Yan S., Gan Y., Jiang N., et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care. 2020;24(1):61. doi: 10.1186/s13054-020-2773-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aroor A.R., Saya R.P., Attar N.R., Saya G.K., Ravinanthanan M. Awareness about basic life support and emergency medical services and its associated factors among students in a tertiary care hospital in South India. J Emergencies, Trauma, Shock. 2014;7(3):166–169. doi: 10.4103/0974-2700.136857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Joseph N., Narayanan T., Bin Zakaria S., et al. Awareness, attitudes and practices of first aid among school teachers in Mangalore, south India. J prim. health care. 2015;7(4):274–281. doi: 10.1071/hc15274. [DOI] [PubMed] [Google Scholar]
- 12.Lindquist B.D., Koval K.W., Acker P.C., et al. Continuing education for prehospital healthcare providers in India - a novel course and concept. Open Access Emerg Med : OAEM. 2020;12:201–210. doi: 10.2147/OAEM.S249447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ramaka S., Nazir N.T., Murthy V.S., et al. Epidemiology of out-of-Hospital Cardiac Arrests, knowledge of cardiovascular disease and risk factors in a regional setting in India: the Warangal Area out-of-hospital Cardiac Arrest Registry (WACAR) Indian Heart J. 2020;72(6):517–523. doi: 10.1016/j.ihj.2020.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pandian G.R., Thampi S.M., Chakraborty N., Kattula D., Kundavaram P.P. Profile and outcome of sudden cardiac arrests in the emergency department of a tertiary care hospital in South India. J Emerg Trauma Shock. 2016;9(4):139–145. doi: 10.4103/0974-2700.193348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ong M.E.H., Shin S.D., Ko P.C., et al. International multi-center real world implementation trial to increase out-of-hospital cardiac arrest survival with a dispatcher-assisted cardio-pulmonary resuscitation package (Pan-Asian resuscitation outcomes study phase 2) Resuscitation. 2022;171:80–89. doi: 10.1016/j.resuscitation.2021.12.032. [DOI] [PubMed] [Google Scholar]
- 16.Liu N., Ning Y., Ong M.E.H., et al. Gender disparities among adult recipients of layperson bystander cardiopulmonary resuscitation by location of cardiac arrest in Pan-Asian communities: a registry-based study. EClinicalMedicine. 2022;44 doi: 10.1016/j.eclinm.2022.101293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ong M.E., Shin S.D., De Souza N.N., et al. Outcomes for out-of-hospital cardiac arrests across 7 countries in asia: the Pan asian resuscitation outcomes study (PAROS) Resuscitation. 2015;96:100–108. doi: 10.1016/j.resuscitation.2015.07.026. [DOI] [PubMed] [Google Scholar]
- 18.Sajithkumar P., Ratna P. Bystander CPR during out-of-hospital cardiac arrest among patients brought to emergency department. IOSR J Nurs Health Sci. 2015;3(4):43–45. [Google Scholar]
- 19.Liu N., Ning Y., Ong M.E.H., et al. Gender disparities among adult recipients of layperson bystander cardiopulmonary resuscitation by location of cardiac arrest in Pan-Asian communities: a registry-based study. eClinicalMedicine. 2022;44 doi: 10.1016/j.eclinm.2022.101293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ahmed S.M., Garg R., Divatia J.V., et al. Compression-only life support (COLS) for cardiopulmonary resuscitation by layperson outside the hospital. Indian J Anaesth. 2017;61(11):867–873. doi: 10.4103/ija.IJA_636_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McNally B., Robb R., Mehta M., et al. Morbidity and Mortality Weekly Report Surveillance Summaries (Washington, DC : 2002. 2011. Out-of-hospital cardiac arrest surveillance --- cardiac arrest registry to enhance survival (CARES), United States, october 1, 2005--december 31, 2010; pp. 1–19. 60(8. [PubMed] [Google Scholar]
- 22.Cheema M.A., Ullah W., Abdullah H.M.A., Haq S., Ahmad A., Balaratna A. Duration of in-hospital cardiopulmonary resuscitation and its effect on survival. Indian Heart J. 2019;71(4):314–319. doi: 10.1016/j.ihj.2019.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Herlitz J., Svensson L., Engdahl J., et al. Characteristics of cardiac arrest and resuscitation by age group: an analysis from the Swedish Cardiac Arrest Registry. Am J Emerg Med. 2007;25(9):1025–1031. doi: 10.1016/j.ajem.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 24.Al-Dury N., Ravn-Fischer A., Hollenberg J., et al. Identifying the relative importance of predictors of survival in out of hospital cardiac arrest: a machine learning study. Scand J Trauma Resuscitation Emerg Med. 2020;28(1):60. doi: 10.1186/s13049-020-00742-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pollack R.A., Brown S.P., Rea T., et al. Impact of bystander automated external defibrillator use on survival and functional outcomes in shockable observed public cardiac arrests. Circulation. 2018;137(20):2104–2113. doi: 10.1161/CIRCULATIONAHA.117.030700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dahan B., Jabre P., Karam N., et al. Impact of neighbourhood socio-economic status on bystander cardiopulmonary resuscitation in Paris. Resuscitation. 2017;110:107–113. doi: 10.1016/j.resuscitation.2016.10.028. [DOI] [PubMed] [Google Scholar]
- 27.Kumar S., Agarwal A.K., Kumar A., Agrawal G.G., Chaudhary S., Dwivedi V. A study of knowledge, attitude and practice of hospital consultants, resident doctors and private practitioners with regard to pre-hospital and emergency care in Lucknow. Indian J Surg. 2008;70(1):14–18. doi: 10.1007/s12262-008-0003-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nambiar M., Nedungalaparambil N.M., Aslesh O.P. Is current training in basic and advanced cardiac life support (BLS & ACLS) effective? A study of BLS & ACLS knowledge amongst healthcare professionals of North-Kerala. World j emerg med. 2016;7(4):263–269. doi: 10.5847/wjem.j.1920-8642.2016.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tiwari Y., Goel S., Singh A. Arrival time pattern and waiting time distribution of patients in the emergency outpatient department of a tertiary level health care institution of North India. J Emergencies, Trauma, Shock. 2014;7(3):160–165. doi: 10.4103/0974-2700.136855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mehta S., Granger C., Grines C.L., et al. Confronting system barriers for ST- elevation MI in low and middle income countries with a focus on India. Indian Heart J. 2018;70(1):185–190. doi: 10.1016/j.ihj.2017.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ravindra P., Bhat R., Karanth N., et al. Patterns and predictors of emergency medical services utilisation by patients attending the emergency medicine department of a tertiary care hospital in India. J Emergencies, Trauma, Shock. 2022;15(2):99–104. doi: 10.4103/jets.jets_83_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Duber H.C., McNellan C.R., Wollum A., et al. Public knowledge of cardiovascular disease and response to acute cardiac events in three cities in China and India. Heart. 2018;104(1):67–72. doi: 10.1136/heartjnl-2017-311388. [DOI] [PubMed] [Google Scholar]
- 33.Ministry of Road Transport and Highways . August 25. 2019. https://morth.nic.in/good-samaritan#:%7E:text=The%20Good%20Samaritan%20Law%20allows,crash%2C%20or%20emergency%20medical%20condition (Good Samaritan). [Google Scholar]
- 34.Perman S.M., Shelton S.K., Knoepke C., et al. Public perceptions on why women receive less bystander cardiopulmonary resuscitation than men in out-of-hospital cardiac arrest. Circulation. 2019;139(8):1060–1068. doi: 10.1161/CIRCULATIONAHA.118.037692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Brady W.J., Mattu A., Slovis C.M. Lay responder care for an adult with out-of-hospital cardiac arrest. N Engl J Med. 2019;381(23):2242–2251. doi: 10.1056/NEJMra1802529. [DOI] [PubMed] [Google Scholar]
- 36.Urban J., Thode H., Stapleton E., Singer A.J. Current knowledge of and willingness to perform Hands-Only CPR in laypersons. Resuscitation. 2013;84(11):1574–1578. doi: 10.1016/j.resuscitation.2013.04.014. [DOI] [PubMed] [Google Scholar]
- 37.Braslow A., Brennan R.T. Layperson CPR: a response to "A reappraisal of mouth-to-mouth ventilation during bystander-initiated cardiopulmonary resuscitation". Prehospital Disaster Med. 1999;14(2):113–114. [PubMed] [Google Scholar]
- 38.Svensson L., Bohm K., Castrèn M., et al. Compression-only CPR or standard CPR in out-of-hospital cardiac arrest. N Engl J Med. 2010;363(5):434–442. doi: 10.1056/NEJMoa0908991. [DOI] [PubMed] [Google Scholar]