Abstract
The recent technological advances allowed us to produce some new wearable devices, such as smartphones and smartwatches (SW). These devices provide different services to their users through different software applications installed even in the SW or smartphones. Health monitoring functionalities, among these services, are nowadays the new technological fashion. In fact, the monitoring is ensured by the sensor incorporated in the SW. The SW allows the record of only one single lead Electrocardiogram (ECG), which is sufficient to screen or diagnosis of rhythm and conduction disorders, especially during the onset of cardiac symptoms, but insufficient for the detection of ischemic disease and cardiomyopathies. In this context, this paper aims to evaluate the feasibility, and reliability of a SW to obtain ECG recordings in comparison with a standard ECG. For that purpose, 140 patients were recruited for this analysis. At the first step, the 12 lead ECG followed with four lead SW-ECG; using the Withings Scanwatch device, were recorded in the same resting conditions. The four lead SW-ECG consists of Einthoven DI lead recorded with the SW, where the SW was on the left wrist and the right index finger on the crown, and three Wilson-type leads, in the which the V1 was recorded in the fourth right parasternal intercostal space, V3 was recorded in the fifth intercostal space on the midclavicular line, and V6 was recorded in the fifth intercostal space on the left midaxillary line with the right index finger placed on the crown and the left hand encompassing the right wrist. 700 ECGs recordings were collected and statistically analyzed in this study. In total, 97 % of the patients were able to obtain an ECG through the SW. A strong correlation was observed between the two recording methods concerning the duration of the studied parameters (r >90 %). The correlation coefficient showed that 33 out of 44 parameters have a strong correlation with the standard ECG. The similarity of the combined leads in the 4 established subgroups was significantly higher, meaning that increasing the number of leads would improve the detection of electrical anomalies. Our findings confirm the existing data on the high similarity between SW and standard 12-leads ECG. Despite SW not having the accuracy and utility of the standard ECG machine, they should be considered as an interesting screening tool for cardiac rhythm disorders, and a compelling solution to electrical documentation of general cardiac symptoms.
Keywords: ECG, Heart, Correlation, Likelihood similarity, Smartwatch, Withings scanwatch
1. Introduction
Recent statistics provided by the World Health Organization (WHO) states that the primary cause of death is cardiovascular diseases (CVDs) [1].In fact, according to estimations, 17.9 million deaths worldwide in 2019 were attributable to CVDs and representing 32 % of all deaths. Moreover, most of the CVD mortality occur in low- and middle-income nations, like Morocco.
Early detection of CVDs symptoms enhances the probability of receiving adequate treatment, which ultimately raises the chance of saving lives. Furthermore, patient life or death could depend on the early detection of CVDs. In fact, these diseases continue to be a major public health problem which requires a high level of precaution. Indeed, the primary objective of physicians is the decrease of CVDs death through an early screening. However, this process is quite challenging since it requires the use of Electrocardiogram (ECG) machines, which is not always available immediately or accessible in underdeveloped countries. The ECG medical equipment helps physicians diagnose some important CVDs such as arrhythmias, conduction disorders, coronary artery disease, and it is considered as a reliable method not only for screening and diagnosing, but also for the post-treatment follow-up. The standard ECG has 12 leads obtained using 10 electrodes attached to the body, to capture the electrical activity of the heart and report it into a graphed paper or digital form. However, to accurately perform the diagnosis process using the ECG device, patients need to be present in a medical facility, then a trained health professional is required to use the device and interpret the results.
Recent advances in wearable technologies have offered new opportunities to promote public health, especially when it comes to remotely monitoring the patient's condition. Among these recent technologies are smartwatch (SW) and smartphones. In fact, nowadays some versions of smartwatches are incorporated with single-lead ECG recorders. Moreover, these devices can capture different health related parameters such as physical activity, oxygen saturation (SpO2), and heart rate using the photoplethysmography (PPG) technique [2]. Some of these devices are already approved and certified by Food and Drug Administration (FDA) in US and in Europe [3]. In fact, the technology used in smartwatches is based on LEDs flashed against the skin which allows sensors to detect and collect the smallest variations in light intensity associated with blood flow. Thereafter, the collected data is processed through special algorithms to report the heartbeats, and alert if an abnormal rhythm is detected [4]. The collected data can be exported through the application installed in the smartphone. However, to obtain a final decision about heart conditions, the patient needs further examination by a qualified health professional.
One of the major challenges facing correct screening and diagnosing of CVDs is that a significant portion of patients would usually present to a medical facility after the occurrence of symptoms (post-event consultation), and therefore no electrical data during the occurrence of symptoms can be documented. Screening and diagnosis of atrial fibrillation and heart blocs in their paroxysmal forms would represent a great example [5].
Whitin this context, this paper aims at shedding light on the capability of SW-ECG recordings to have sufficient sensibility and sensitivity compared to a standard ECG, and whether it might be considered as a reliable screening device. The Withings Scanwatch; which is FDA-cleared, was used for recording ECG. This device is dotted with three electrodes: two are integrated into the back of the watch and the third is placed in the stainless-steel bezel that surrounds the watch glass. To start recording the single-lead ECG, the user simply places his finger on the bezel. The ECG graph can be exported in PDF format through the Health Mate application. Four-lead ECG were recorded using the SW and compared to 12-leads standard ECG. Two rational reasons behind the choice of this device: its availability in Moroccan market with a cheapest price compared to other SWs and the growing number of its users in Morocco.
This paper represents a prospective study conducted on 140 participants, and aims to address the following research questions (RQs).
-
1.
Whether the results reported by the four-lead SW-ECG recordings have a significant correlation compared to standard 12-Leads ECG results.
-
2.
Whether the SW-ECGs recording can be used as a reliable electrical documentation tool during occurrence of cardiac symptoms.
The main contributions of this study are.
-
•
To conduct an extensive experiment including 140 patients in Cardiology department in Cheikh Zaid International University Hospital in Morocco.
-
•
To examine the capability of four-lead SW-ECG (i.e., Withings Scanwatch) to screen and monitor accurately the heart conditions as a standard ECG.
-
•
To offer an alternative reliable and accurate way to screen and monitor the heart condition using lead recorded by SW-ECG.
The remainder of this paper is structured as follow: Section 2 describes the materials and methods used to conduct this study including the study design the inclusion and exclusion criteria to include participants, the devices used, studied parameters and statistical analysis used. Section 3, 4 present and discuss the obtained results. Conclusions and further work are presented in Section 5.
2. Materials and methods
This section describes the methodology followed in this study to answer the two RQs defined in Section 1, starting by presenting the population cohort included in this experiment, the inclusion and exclusion criteria adopted to select participants, the device used to record the 12-lead ECG and the four-lead ECG, the health parameters monitored, the process of data collection and statistical techniques used.
2.1. Study design
The population cohort of 140 participants aged 18–95 years, were recruited between December 2021 and June 2022 at Cheikh Zaid University Hospital in Rabat, Morocco. These participants were either admitted in the cardiology department or presented to the Cardiology consultation. The participants were not exclusively living in the area of Rabat, as the hospital receives patients from all across the country as well as some sub-Saharans countries. Ethical approval was granted by the Cheikh Zaid University board, and all participants consented formally to their participation in the study.
2.2. Inclusion criteria
-
•
Participants who presented to cardiology consultation at Cheikh Zaid University Hospital and had a 12-leads ECG.
-
•
Participants who were admitted to Cardiology department at Cheikh Zaid University hospital and had a 12-leads ECG.
-
•
Patients with sufficient cognitive ability to independently manipulate a smartwatch.
2.3. Exclusion criteria
-
•
Participants not fitting one of the inclusion criteria.
-
•
Patients suffering from Parkinson Disease or other causes of tremors.
-
•
Patients admitted in the cardiology Intensive Care Unit of Cheikh Zaid University Hospital.
2.4. Standard ECG used
The standard ECG device used to record the 12-lead ECGs was Mortara Eli 250 model, with a paper speed of 25 mm/s and a 10 mm/mV of voltage. The ECG signals were recorded for all population cohort after 2 min rest period in the supine position.
2.5. Scanwatch trace recording
Immediately after finishing the 12-lead ECG recording process, the four-lead ECG recordings process started. Each recording lead lasted 30s making a total of 2 min This recording was performed using the Withings Scanwatch. Some general instructions on how to use this device to record the single lead ECG were presented to every cohort participant. The recording process was performed on the same condition as the previous recording. A nurse assisted a participant in recording steps.
The four-lead ECG recording were collected pursuing the following instructions.
-
•
The first recording signal; denoted by DI, was performed with the watch on the left wrist and the right index finger on the crown.
-
•
The second recording signal; denoted by V1 in the standard ECG, was recorded in fourth right parasternal intercostal space.
-
•
The third recording signal; denoted by V3 in the standard ECG, was recorded in the midway between the Fourth intercostal space at the left sternum and the fifth intercostal space at the midclavicular line.
-
•
The fourth recording signal; denoted by V6 in the standard ECG, was recorded in the fifth intercostal space on the left midaxillary line.
Fig. 2 illustrates the four locations in which the SW-ECGs were recorded.
Fig. 1.
Flowchart of patient's recruitment.
Fig. 2.
The four-lead ECG recordings locations.
Fig. 2.(d): DI recording location.
Fig. 2.(c): V6 recording location.
Fig. 2.(b): V3 recording location.
Fig. 2.(a): V1 recording location.
For the three later recording, which are Wilson-type chest lead recordings, were performed by placing the SW in the above-mentioned location, the right index finger was placed on the crown, the left hand encompassed the right wrist and both hands and forearms were also in contact with the chest.
In contrast to the standard ECG in which the recording is done simultaneously, the SW-ECG is performed in a sequential way. As for the SW-ECG recording configuration, it was like the configuration of the standard ECG.
The SW-ECGs signals were nominally stored using the Health Mate application available for download from the Google/Apple store. Therefore, they were exported in PDF format using the “Send PDF to your doctor” functionality.
2.6. Studied parameters
This study focuses on analyzing six parameters, which are listed below (Fig. 3).
-
•
P wave: amplitude (in millivolts), duration (in milliseconds), and morphology (positive/negative).
-
•
PR interval duration (in milliseconds).
-
•
QRS complex: amplitude (in millivolts), duration (in milliseconds), and morphology (narrow/wide).
-
•
ST segment morphology (ST elevation/depression/isoelectrical).
-
•
T wave: amplitude (in millivolts), and morphology (positive/negative/flat).
-
•
QT interval duration (in milliseconds) calculated using Bazett formula.
Fig. 3.
Basic principles of ECG analysis.
The abovementioned parameters were obtained directly from ECG device for the standard ECGs recording, and from the printed SW-ECG recording using a standard ECG ruler.
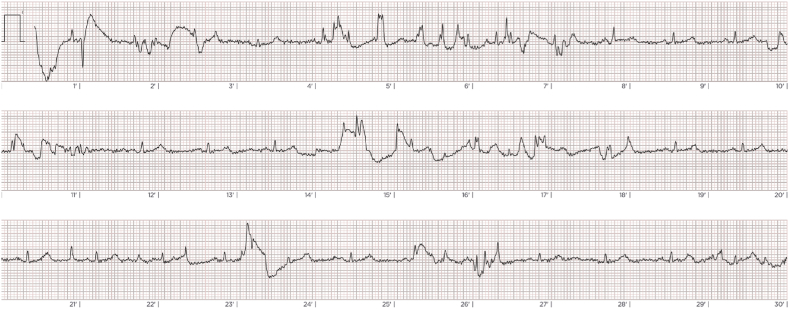
Although the standard ECGs differed in appearance from the SW-ECGs (as stated in Fig. 4), the recordings were blinded randomized. The analysts, therefore, could not know which standard ECG belonged to which SW-ECG (see Fig. 5).
Fig. 4.
Comparison of the S-ECG recording and the four-lead SW-ECG recording.
Fig. 5.
Example of a poor quality SW recording.
Fig. 4(a) Standard 12-Leads ECG trace: ST segment elevation in V1 to V3 leads, ST depression in V6 with negative T wave in the lateral territory.
Fig. 4(b) SW ECG trace (From top to bottom): Negative T wave in D1, ST segment elevation in V1 and V3, ST segment depression in V6.
2.7. Data collection and labeling
The collected SW-ECG graphs were classified into two main categories.
-
•
Poor quality: if the SW displayed the message “tracing parasitized”, and an analysist considered the recording as not interpretable.
-
•
Good quality: if everything went well in graph generating process.
The step consists of labeling the ECG graphs belonging to the good quality sample, according to electrical abnormalities observed. We have chosen to adopt 6 labels.
-
•
Atrial fibrillation (Afib)
-
•
Premature ventricular complex (PVC)
-
•
Left ventricular hypertrophy (LVH)
-
•
Ischemic disorder
-
•
Atrioventricular blocks (AVB)
-
•
Normal
For a more accurate comparison, we have established 4 sub-groups of patients based on the above labels.
-
•
Rhythm abnormalities (Patients that had Afib or PVC)
-
•
Conduction abnormalities (Patients that had AVB)
-
•
Repolarization abnormalities (Patients that had electrical signs of Ischemia)
-
•
Normal (Patients that didn't have rhythm, conduction or repolarization abnormalities, and patients that had LVH)
2.8. Statistical analysis
The statistical analysis was performed using SPSS Statistics version 25. The Pearson correlation test was performed to check whether SW-ECG derivations and the standard ECG recording have the same trend. This test assumes that their relationship is linear. For the categorical data, the Chi-square test was used to determine if there is a significant association, if the p-value is less than a predetermined significance level (e.g., 5 %), we calculate the correlation coefficient named Cramer's V to assess the relationship between categorical variables. All statistical tests performed at 95 % confidence level. We mention that some data transformations were performed in this study before proceeding to statistical tests: a Likert scale was adopted to encode the categorical variables that have at least three possibilities, and binary transformation if the variable have two possibilities. Finally, the Jaccard similarity or likelihood similarity was used to compute the probability of similarity between the SW-ECG and the 12 leads ECG according to the four-lead derivation for each studied sub-group of pathology. In fact, the Jaccard similarity is a measure of similarity between two sets of items, defined as the size of the intersection of the sets divided by the size of the union of the sets. The Jaccard similarity coefficient ranges from 0 to 1, with 0 indicating no overlap between the sets (i.e., the sets are completely different) and 1 indicating that the sets are identical. Values between 0 and 1 indicate varying degrees of similarity.
3. Results
3.1. Population cohort description
Table 1 lists the descriptive statistics of patients recruited in our study. 89 out of 140 patients were male with an average age of 61.13 and a standard deviation of 15. As for female, the average age was 67.16 and a standard deviation of 14.98.
Table 1.
Population cohort epidemiological characteristics.
| Variable | Number of patients |
|---|---|
| Age (years) | 63.33 ± 15.22 |
| Gender (male/female) | 89/51 |
| HTN | 94 |
| Diabetes | 46 |
| Smoking | 27 |
| Obesity | 28 |
| Dyslipidemia | 20 |
| Prior stroke | 20 |
| Chronic renal impairment | 8 |
| Ischemic cardiopathy | 10 |
| Valvular Heart disease | 18 |
| Body mass index | 24.77 ± 3.6 |
Table 2 reports the clinical characteristics of our population. The mean systolic arterial pressure was 134 mmHg, mean heart rate was 76 beat per minute, and mean oxygen saturation was 97 %, as the majority of our population had a stable hemodynamic status. The most common reason for admission was dyspnea (50 % of the population) followed by chest discomfort (24 %).
Table 2.
Population cohort clinical characteristics.
| Variable | Number of patients (%) |
|---|---|
| Systolic Arterial Pressure (mmHg) | 134.13 ± 22.13 |
| Heart rate (beat per minute) | 76.92 ± 19.83 |
| SpO2 (%) | 97.35 ± 2.02 |
| Dyspnea | 71 (50.71 %) |
| Chest discomfort | 34 (24.28%) |
| Palpitation | 18 (12.85 %) |
| Syncope | 2 (1.42 %) |
The average heart rate reported by the standard ECG was 77.08 beats per minute and a standard deviation of 19.78, whereas for the SW-ECG reported a mean of 77.11 beats per minute and a standard deviation of 18.29.
The standard and SW ECGs characteristics for all ECG measurements are reported in Table 3, Table 4, Table 5, Table 6, Table 7, Table 8, along with the statistical test results.
Table 3.
ECG P-wave characteristics (duration, amplitude, and morphology) and correlation coefficients comparison between Smartwatch and standard 12-leads ECG.
| Variables | Lead | SW-ECG | 12-Leads ECG | Correlation coefficient with S-ECG | p-value |
|---|---|---|---|---|---|
| Presence of P-wave | DI | Absence = 45 | Absence = 44 | 91.4 % | <0.01 |
| Presence = 91 | Presence = 95 | ||||
| V1 | Absence = 76 | Absence = 44 | 64.81 % | <0.01 | |
| Presence = 60 | Presence = 95 | ||||
| V3 | Absence = 55 | Absence = 44 | 79.6 % | <0.01 | |
| Presence = 80 | Presence = 95 | ||||
| V6 | Absence = 42 | Absence = 44 | 88.0 % | <0.01 | |
| Presence = 93 | Presence = 95 | ||||
| Duration (milliseconds) | DI | 72.61 ± 24.49 | 80.71 ± 20.81 | 94.3 % | <0.05 |
| V1 | 51.53 ± 14.94 | 81.04 ± 22.58 | 73.3 % | <0.05 | |
| V3 | 60.26 ± 19.19 | 81.54 ± 21.82 | 83.9 % | <0.05 | |
| V6 | 70.65 ± 26.46 | 82.12 ± 23.83 | 90.9 % | <0.05 | |
| Amplitude (millivolts) | DI | 1.21 ± 0.43 | 1.4 ± 0.82 | 90.3 % | <0.05 |
| V1 | 1.07 ± 0.192 | 1.6 ± 0.63 | 75.6 % | <0.05 | |
| V3 | 1.04 ± 0.169 | 1.7 ± 0.31 | 82.8 % | <0.05 | |
| V6 | 1.16 ± 0.38 | 1.5 ± 0.55 | 88.7 % | <0.05 | |
| Morphology (Normal/LAH/RAH) | DI (n = 91) | Normal = 84 | Normal = 76 | 84.1 % | <0.01 |
| LAH = 6 | LAH = 12 | ||||
| RAH = 1 | RAH = 7 | ||||
| V1 (n = 60) | Normal = 60 | Normal = 76 | 44.9 % | <0.01 | |
| LAH = 0 | LAH = 12 | ||||
| RAH = 0 | RAH = 7 | ||||
| V3 (n = 80) | Normal = 76 | Normal = 76 | 67.6 % | <0.01 | |
| LAH = 4 | LAH = 12 | ||||
| RAH = 0 | RAH = 7 | ||||
| V6 (n = 93) | Normal = 83 | Normal = 76 | 80 % | <0.01 | |
| LAH = 8 | LAH = 12 | ||||
| RAH = 2 | RAH = 7 | ||||
| LAH: left atrial hypertropia RAH: right atrial hypertropia | |||||
Table 4.
ECG PR interval duration and correlation coefficients comparison between Smartwatch and standard 12-leads ECG.
| Variables | Lead | SW-ECG | 12-Leads ECG | Correlation coefficient | p-value |
|---|---|---|---|---|---|
| Duration (milliseconds) | DI | 165.91 ± 30.74 | 170.38 ± 34.04 | 92.8 % | <0.05 |
| V1 | 174.10 ± 30.52 | 169.67 ± 36.094 | 87.2 % | <0.05 | |
| V3 | 179.46 ± 31.75 | 168.22 ± 35.19 | 92.7 % | <0.05 | |
| V6 | 169.61 ± 30.97 | 171.11 ± 31.22 | 94.3 % | <0.05 |
Table 5.
ECG QRS characteristics (duration, amplitude, and morphology) and correlation coefficients comparison between Smartwatch and standard 12-leads ECG.
| Variables | Lead | SW-ECG | 12-Leads ECG | Correlation coefficient* | p-value |
|---|---|---|---|---|---|
| Duration (milliseconds) | DI | 84.13 ± 18.35 | 101.92 ± 21.02 | 97.3 % | <0.05 |
| V1 | 96.43 ± 21.29 | 102.04 ± 19.32 | 98.1 % | <0.05 | |
| V3 | 96.99 ± 21.13 | 102.74 ± 18.52 | 97.6 % | <0.05 | |
| V6 | 85.13 ± 22.41 | 103.04 ± 20.41 | 96.3 % | <0.05 | |
| Amplitude (millivolts) | DI | 7.9 ± 7.83 | 9,72 ± 6.22 | 68.7 % | <0.05 |
| V1 | 2.36 ± 1.79 | 8.48 ± 4.22 | 69.6 % | <0.05 | |
| V3 | 4.00 ± 2.84 | 9.08 ± 3.92 | 77.6 % | <0.05 | |
| V6 | 11.06 ± 8.63 | 9.88 ± 5.02 | 80 % | <0.05 | |
| Morphology (Narrow/Wide) | DI | N = 124/W = 13 | N = 110/W = 27 | 84.3 % | <0.05 |
| V1 | N = 110/W = 26 | N = 108/W = 29 | 68.9 % | <0.05 | |
| V3 | N = 108/W = 28 | N = 105/W = 26 | 66.6 % | <0.05 | |
| V6 | N = 114/W = 22 | N = 106/W = 27 | 53 % | <0.05 | |
| N: Narrow/W: Wide. | |||||
A strong correlation between the segment ST of the SW and standard ECG was found, except for DI lead, where the correlation coefficient was 55 %, as reported in Table 6.
Table 6.
ECG ST segment morphology and correlation coefficients comparison between Smartwatch and standard 12-leads ECG.
| Variables | Lead | SW-ECG | 12-Leads ECG | Correlation coefficient | p-value |
|---|---|---|---|---|---|
| Morphology | DI | E = 7/I+130/D = 0 | E = 1/I = 137/D = 2 | 55.1 % | <0.01 |
| V1 | E = 1/I = 127/D = 8 | E = 4/I = 133/D = 3 | 97.2 % | <0.01 | |
| V3 | E = 1/I = 120/D = 15 | E = 2/I = 133/D = 5 | 97.3 % | <0.01 | |
| V6 | E = 12/I = 124/D = 0 | E = 4/I = 135/D = 1 | 95.5 % | <0.01 | |
| E: ST elevation/D: ST depression/I: ST isoelectrical | |||||
As can be observed in Table 7, only the V6 lead was strongly correlated with the S-ECG (r = 87 %).
Table 7.
ECG T-wave morphology and correlation coefficients comparison between Smartwatch and standard 12-leads ECG.
| Variables | Lead | SW-ECG | 12-Leads ECG | Correlation coefficient* | p-value |
|---|---|---|---|---|---|
| Morphology (Positive/flat/negative) | DI (n = 136) | Positive = 103 | Positive = 111 | 56.7 % | <0.05 |
| Flat = 22 | Flat = 4 | ||||
| Negative = 11 | Negative = 24 | ||||
| V1 (n = 136) | Positive = 107 | Positive = 109 | 43.6 % | <0.05 | |
| Flat = 13 | Flat = 6 | ||||
| Negative = 15 | Negative = 25 | ||||
| V3 (n = 136) | Positive = 110 | Positive = 109 | 58.2 % | <0.05 | |
| Flat = 10 | Flat = 6 | ||||
| Negative = 26 | Negative = 25 | ||||
| V6 (n = 136) | Positive = 111 | Positive = 110 | 87.5 % | <0.05 | |
| Flat = 4 | Flat = 5 | ||||
| Negative = 21 | Negative = 25 |
The results of Pearson statistical test show that there is a strong correlation between the QT-interval duration from the two devices. As the lowest correlation coefficient found was 99.1 %, Table 8.
Table 8.
ECG QT interval duration and correlation coefficients comparison between Smartwatch and standard 12-leads ECG.
| Variables | Lead | SW-ECG | 12-Leads ECG | Correlation coefficient | p-value |
|---|---|---|---|---|---|
| QT duration (milliseconds) | DI | 380.3 ± 41.85 | 385.01 ± 36.86 | 99.2 % | <0.05 |
| V1 | 379.58 ± 52.57 | 384.32 ± 33.75 | 98.8 % | <0.05 | |
| V3 | 370.09 ± 36.97 | 386.28 ± 35.46 | 99.3 % | <0.05 | |
| V6 | 374.71 ± 36.93 | 382.11 ± 34.63 | 99.5 % | <0.05 | |
| Corrected QT duration (milliseconds) | DI | 417.53 ± 41.85 | 410.21 ± 31.3 | 99.4 % | <0.05 |
| V1 | 417.48 ± 47.98 | 409.18 ± 32.5 | 99.1 % | <0.05 | |
| V3 | 411.37_±35.83 | 411.44 ± 30.2 | 99.4 % | <0.05 | |
| V6 | 412.56 ± 37.15 | 408.98 ± 31.8 | 99.7 % | <0.05 |
As it can be seen from Table 3, a strong correlation between P-wave duration and amplitude of SW-ECG and S-ECG. In fact, the correlation coefficient shows at least 73 % correlation in all leads. As for the P-wave morphology, the Pearson correlation test revealed that the correlation remains strong in two leads (i.e., DI and V6), as for the other leads the correlations were 45 % and 68 % for V1 and V3 respectively.
A strong correlation was observed between the PR-interval duration from the two devices, as presented in Table 4. In fact, the lowest correlation coefficient was 87 %.
Table 5 lists the characteristics of the QRS complex duration, amplitude, and morphology reported by the SW along with the correlation coefficient with the S-ECG. As it can be seen, a strong correlation was detected between QRS complex duration of the two devices (r>96 %). The same remarks were reported for the QRS complex amplitude in lead V3 and V6. As for the QRS complex morphology, only the DI lead has a strong correlation (r = 84 %) with the S-ECG.
Table 9 shows the compatibility of SW and 12-lead ECG results according to the subgroups in each lead studied. The correlation results are between 70 and 85 % for all leads combined for rhythm disorders. Good results were observed for cardiac repolarization disorders, mainly in the anterior territory, with correlation values of around 78 %. Regarding conduction disorders, maximum results were observed in V1, with a likelihood of similarity of 77.8 %. For normal ECGs, the likelihood of similarity was 100 %.
Table 9.
Details of probability of similarity between the SW-ECG and S-ECG according to four lead derivation for the studied sub-groups.
| SW vs 12-leads ECG | Subgroups | Likelihood of similarity |
|---|---|---|
| DI | Rhythm abnormalities | 71 % |
| V1 | 85 % | |
| V3 | 70.45 % | |
| V6 | 79.54 % | |
| DI | Conduction abnormalities | 33.4 % |
| V1 | 77.8 % | |
| V3 | 66.7 % | |
| V6 | 55.6 % | |
| DI | Repolarization abnormalities | 15 % |
| V1 | 78 % | |
| V3 | 78 % | |
| V6 | 37 % | |
| DI | Normal | 100 % |
| V1 | 100 % | |
| V3 | 100 % | |
| V6 | 100 % |
As it can be observed in Table 10, Comparing smartwatch data from all leads with the standard 12-lead ECG, the detection rate increased considerably, reaching 89 % for conduction abnormalities, 93 % for arrhythmias and 100 % for repolarization disorders, as well as for normal ECGs.
Table 10.
Probability of similarity between SW-ECG and S-ECG according to studied sub-groups.
| Subgroups | Likelihood of similarity SW vs 12-leads ECG |
|---|---|
| Rhythm abnormalities | 93 % |
| Conduction abnormalities | 89 % |
| Repolarization abnormalities | 100 % |
| Normal | 100 % |
4. Discussion
Telemedicine is a medical novelty service that is rapidly developing to provide better and easier access to high-quality, efficient, and cost-effective healthcare. Indeed, this development is due to advances in the technological fields, particularly in data and telecommunication [6].
This research study is being conducted to shed light on the ability of SW to provide useful information about heart condition and check whether it can be a reliable tool to screen, diagnosis and monitor the patient.
In fact, the possibility of performing ECG recordings without medical assistance could help improve healthcare services by increasing the detection rate of certain cardiac electrical disorders. This will enable patients to be treated earlier and improve their prognosis. Not to mention that this asset will relieve the economic burden on the healthcare system by preventing serious complications such as strokes and heart failure. Recent studies like the Apple Heart Study and the Huawei Heart Study [3,7] had shown promising results in terms of the SW's ability to detect and monitor atrial fibrillation as a concrete example.
In our study, a population cohort of 140 patients (89 men and 51women) were recruited in Cheikh Zaid University Hospital in Rabat, Morocco. We have chosen the Withings Scanwatch for its availability in Morocco, as it is the only smartwatch has operational ECG recording in Morocco, other brands haven't been authorized yet.
On a general scale, our statistical analysis demonstrated a strong correlation between most lead derivations recorded by the SW and the standard ECG recordings at 5 % and 1 % confidence level. Moreover, the correlation coefficient reached 98 % in some cases. Precisely, 33 out of 44 correlation coefficients showed a strong correlation (r > 70 %), five correlation coefficients were between 66.6 % and 69.6 %, four were between 53 % and 58.2 %, and two correlation coefficients were 43.6 % and 44.9 %.
Our results found that P wave and the PR interval characteristics had their best correlation in D1 and V6 leads, though morphology of P wave had lesser correlation value. As D1 lead being the easiest one to be recorded by the patient, the high correlation suggests then a useful use of the SW for documentation of atrial fibrillation mainly, during palpitations, or heart blocks during extreme fatigue and dizziness, as it would be impossible for a patient to use the device during a syncope.
During similar symptoms, ventricular tachycardia, a sever arrythmia characterized by high heart rate, absence of P wave, and wide QRS complexes, would also be screened upon its symptoms, since QRS duration had a significantly high correlation in all studied leads.
Concerning ST morphology, despite having an excellent correlation of its morphology on V1, V3, and V6 leads, SW wouldn't be of much use since precise screening for ischemia consist of observing significant ST abnormalities on a specific arterial territory. None of the 3 main coronary territories on ECG were covered in our study. Moreover, the correlation of T wave morphology was only high in V6 leads, yet insufficient.
QT interval duration (including corrected QT) had correlation above 99 % in every studied lead. We suggest that our results the use of SW for monitoring patients under medications known for QT interval prolonging, or screening for primary Long QT Syndrome (LQTS). Our results were similar, if not better, than the measurement reported in the work of Spaccarotella and al [8]. LQTS remaining one of the causes of sudden death among athletes and young children, its screening would a major asset of SWs if adopted and approved.
We must emphasize that these results were obtained in a cohort with a mean age of 63 years, most of our patients being unfamiliar with smart devices use. We assume that better results may be obtained with a younger population. In fact, a recent study showed that aged people in their population cohort cannot use properly smartwatches to record the single lead ECG [9]. To address this issue, our team assisted the patients in gathering a first SW recording. We believe that the establishment of a practical guide for SW ECG recording would be very helpful.
The comparison of similarity between the standard ECG recording and SW on each of the leads showed better results in rhythm and repolarization abnormalities detection than conduction defects. The similarity of the combined leads in the 4 established subgroups was significantly higher, meaning that increasing the number of leads would improve the detection of electrical anomalies. Our findings are consistent with the work of Avila and al. on the Apple SW [10]. The false positive detection of abnormalities, is still a considerable issue of SW as described by Perino and al. who had a false notification of irregular pulse in 40 % of their population [11]. As we hadn't faced similar issues, false positive detection couldn't be evaluated in our work.
4.1. Study limitations
The main limitation of our study was that the recordings of standard ECG and SW ECG were not conducted simultaneously. The movements of patients’ upper limbs necessary for the SW recording resulted in a poor standard ECG trace quality, not to mention the interference between the two electronic systems.
We must also mention the limited size of our cohort population compared with the previous studies, due to the small size of our hospital and cardiology department.
5. Conclusions and further work
Wearable devices are the present and near future of patient health monitoring, waiting for lesser invasive implantable cardiac monitoring systems. Smartwatches are a democratically spreading fashion among the youth, but it might be as attractive for elder populations once convinced of the medical reliability of their use. Our findings confirm the existing data on the high similarity between SW and standard 12-leads ECG. Despite SW not having the accuracy and utility of the standard ECG machine, they should be considered as an interesting screening tool for cardiac rhythm disorders, and a compelling solution to electrical documentation of general cardiac symptoms. SW are still incomplete systems and further development of their health monitoring features is only a matter of time.
Ongoing work aims at developing a deep learning model for better detection of heart abnormalities using the SW-ECG recordings as inputs. We believe that such models may act as decision support systems to help physicians reach more accurate screening and monitoring tools.
Ethics statement
This study was approved by the Ethics Committee of Cheikh Zaid foundation CEFCZ/PR/03/03/23 approved the present study. The need for informed consent was waived because of the anonymity of the data, CEFCZ certified that the study was performed in accordance with the ethical standards as laid down in the Declaration of Helsinki.
Data availability statement
Data will be made available on request.
Additional information
No additional information is available for this paper.
CRediT authorship contribution statement
Soufiane Touiti: All authors listed have significantly contributed to the development and the writing of this article, Conceived and designed the experiments, Performed the experiments, Analyzed and interpreted the data. Ibtissam Medarhri: All authors listed have significantly contributed to the development and the writing of this article, Conceived and designed the experiments, Performed the experiments, Contributed reagents, materials, analysis tools or data. Kamal Marzouki: Performed the experiments. Nabil Ngote: All authors listed have significantly contributed to the development and the writing of this article, Conceived and designed the experiments, Performed the experiments, Contributed reagents, materials, analysis tools or data. Amale Mezalek Tazi: Analyzed and interpreted the data.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
The authors would like to thank the Fondation Cheikh-Zaid (Abulcasis University and Cheikh Zaid Hospital) for their support.
References
- 1.World Health Organization, WHO https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds (n.d.)
- 2.Giggins O.M., Doyle J., Smith S., Crabtree D.R., Fraser M. Measurement of heart rate using the Withings ScanWatch device during free-living activities: validation study, JMIR form. Res. 2022;6 doi: 10.2196/34280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Turakhia M.P., Desai M., Hedlin H., Rajmane A., Talati N., Ferris T., Desai S., Nag D., Patel M., Kowey P., Rumsfeld J.S., Russo A.M., Hills M.T., Granger C.B., Mahaffey K.W., Perez M.V. Rationale and design of a large-scale, app-based study to identify cardiac arrhythmias using a smartwatch: the Apple Heart Study. Am. Heart J. 2019;207:66–75. doi: 10.1016/j.ahj.2018.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Prasitlumkum N., Cheungpasitporn W., Chokesuwattanaskul A., Thangjui S., Thongprayoon C., Bathini T., Vallabhajosyula S., Kanitsoraphan C., Leesutipornchai T., Chokesuwattanaskul R. Diagnostic accuracy of smart gadgets/wearable devices in detecting atrial fibrillation: a systematic review and meta-analysis. Arch. Cardiovasc. Dis. 2021;114:4–16. doi: 10.1016/j.acvd.2020.05.015. [DOI] [PubMed] [Google Scholar]
- 5.Behzadi A., Shamloo A.S., Mouratis K., Hindricks G., Arya A., Bollmann A. Feasibility and reliability of smartwatch to obtain 3-lead electrocardiogram recordings. Sensors. 2020;20:1–11. doi: 10.3390/s20185074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moore M. 1999. The Evolution of Telemedicine. [Google Scholar]
- 7.Guo Y., Wang H., Zhang H., Liu T., Liang Z., Xia Y., Yan L., Xing Y., Shi H., Li S., Liu Y., Liu F., Feng M., Chen Y., Lip G.Y.H., Lane D.A., Wang L., Eckstein J., Thomas G.N., Tong L., Mei F., Xuejun L., Xiaoming L., Zhaoliang S., Xiangming S., Wei Z., Yunli X., Jing W., Fan W., Sitong Y., Xiaoqing J., Bo Y., Xiaojuan B., Yuting J., Yangxia L., Yingying S., Zhongju T., Li Y., Tianzhu L., Chunfeng N., Lili Z., Shuyan L., Zulu W., Bing X., Liming L., Yuanzhe J., Yunlong X., Xiaohong C., Fang W., Lina Z., yihong S., shujie J., Jing L., Nan L., shijun L., huixia L., Rong L., Fan L., qingfeng G., tianyun G., Yuan W., Xin L., Yan R., xiaoping C., ronghua C., Yun S., yulan Z., haili S., yujie Z., quanchun W., weidong S., Lin W., Chan E., Guangliang S., Chen Y., Wei Z., Dandi C., Xiang H., Anding X., Xiaohan F., Ziqiang Y., Xiang G., Fulin G. Mobile photoplethysmographic technology to detect atrial fibrillation. J. Am. Coll. Cardiol. 2019;74:2365–2375. doi: 10.1016/j.jacc.2019.08.019. [DOI] [PubMed] [Google Scholar]
- 8.Spaccarotella C.A.M., Migliarino S., Mongiardo A., Sabatino J., Santarpia G., De Rosa S., Curcio A., Indolfi C. Measurement of the QT interval using the Apple watch. Sci. Rep. 2021;11:1–8. doi: 10.1038/s41598-021-89199-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Desteghe L., Raymaekers Z., Lutin M., Vijgen J., Dilling-Boer D., Koopman P., Schurmans J., Vanduynhoven P., Dendale P., Heidbuchel H. Performance of handheld electrocardiogram devices to detect atrial fibrillation in a cardiology and geriatric ward setting. Europace. 2017;19:29–39. doi: 10.1093/europace/euw025. [DOI] [PubMed] [Google Scholar]
- 10.Avila C.O. Novel use of Apple watch 4 to obtain 3-lead electrocardiogram and detect cardiac ischemia. Perm. J. 2019;23 doi: 10.7812/TPP/19-025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Perino A.C., Gummidipundi S.E., Lee J., Hedlin H., Garcia A., Ferris T., Balasubramanian V., Gardner R.M., Cheung L., Hung G., Granger C.B., Kowey P., Rumsfeld J.S., Russo A.M., True Hills M., Talati N., Nag D., Tsay D., Desai S., Desai M., Mahaffey K.W., Turakhia M.P., Perez M.V. Arrhythmias other than atrial fibrillation in those with an irregular pulse detected with a smartwatch: findings from the Apple heart study. Circ. Arrhythm. Electrophysiol. 2021;14 doi: 10.1161/CIRCEP.121.010063. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.