Abstract
Pituitary stalk interruption syndrome (PSIS) is a rare congenital abnormality. It comprises the triad of thin or interrupted pituitary stalk, aplasia or hypoplasia of anterior pituitary gland, and absent or ectopic posterior pituitary gland. The patient usually presents with a spectrum of symptoms predominantly secondary to anterior pituitary hormonal deficiency. The etiology of this syndrome is not well-established but the genetic cause is considered to be the most common etiology. Early diagnosis is crucial in preventing and reducing morbidity. The prognosis is good if the condition is diagnosed early and the hormonal therapy is started promptly. The diagnosis of PSIS is primarily based on magnetic resonance imaging (MRI) findings.
Keywords: Ectopic, Hypoplastic, Pituitary stalk interruption syndrome
Case presentation
A 14-year-old female presented with short stature and delayed puberty. The patient was born via normal vaginal delivery at home and the birth history was uneventful with a normal cry at birth. The birth and childhood measurements are not available. There was no history of developmental milestones (gross motor, fine motor, social) delay. She had no other no chronic medical problems, hospitalizations, or surgeries. She was at an age-appropriate grade in school. There is no such history in family members and relatives.
On examination, the height of the patient was 127 cm (<3rd percentile), lower segment (LS) was 60 cm, upper segment (US) was 67 cm, US/LS was 1.1, weight was 35.7 kg and BMI was 21.7 kg/m2. The patient had no sign of thelarche or pubarche.
Complete blood count (CBC), erythrocyte sedimentation rate (ESR), urinalysis, and serum electrolytes were normal. Hormonal analysis showed prolactin: 1.13 ng/mL (N = 2.8-29.2 ng/mL), total testosterone: <7 ng/mL (N = 14-76 ng/mL), ACTH: 7.93 pg/mL (N=<46 pg/mL), fasting morning cortisol: 7.53 µg/dL (N = 6.4-22.8 µg/dL) and IGF-1; Somatomedin- C: 30.2 ng/mL (N=170-527 ng/mL).
USG abdomen/pelvis showed a small uterus and bilateral ovaries were visualized.
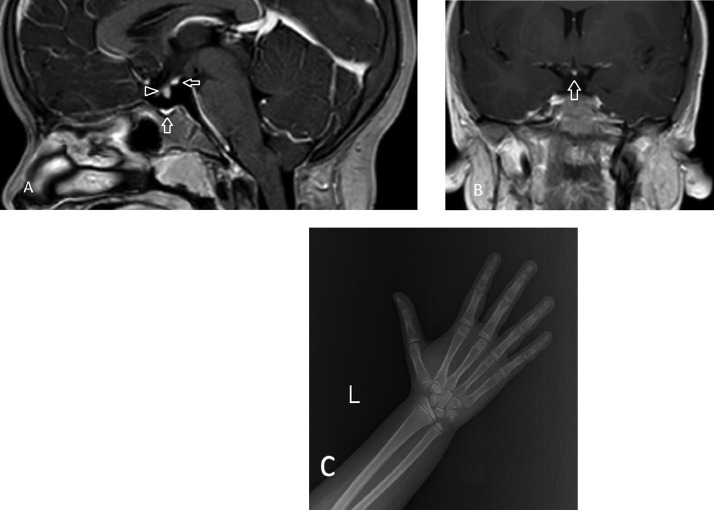
X-ray left hand for bone age was done which showed the bone age to be 11-12 years (As per Greulich and Pyle bone atlas) with the standard deviation for bone age being 1 year for the chronological age of the patient (Fig. 1C).
Fig. 1.
(A) T1 weighted postcontrast Sagittal image showing hypoplastic anterior pituitary (vertical arrow), short and interrupted pituitary stalk (arrowhead), and ectopic posterior pituitary in the region of median eminence (horizontal arrow). (B) T1 weighted postcontrast coronal image showing ectopic posterior pituitary (vertical arrow). (C) X-ray of PA left hand for bone age.
MRI brain showed a hypoplastic anterior pituitary gland, short and interrupted pituitary stalk with ectopic posterior pituitary in the region of median eminence (Figs. 1A and B).
On the basis of MRI findings, a diagnosis of pituitary stalk interruption syndrome (PSIS) was made. The patient and her legal guardian were and counseled for hormonal therapy. However, due to poor economic background, the patient couldn't afford the treatment and was lost to follow-up.
Discussion
PSIS is a rare congenital condition with an estimated incidence rate of 0.5/1,000,000 births [1]. The syndrome has a male predominance with a male: female sex ratio of 2.3-6.9:1 pointing to X-linked inheritance and the mean age at diagnosis is 9.4 ± 11.6 years [2]. The exact cause of PSIS is unknown and different theories have been proposed including perinatal injuries, and defective organogenesis due to genetic or environmental factors during pregnancy. Rare mutations of HESX1, LH4, OTX3, and SOX3 have been postulated in PSIS in familial cases. Between 20% and 50% of patients with PSIS also have different malformations mainly midline ones such as cleft lip, absence of diaphragm, hypoplasia of optic nerve, bulging brain, or harelip which indicates that the gene defect corresponding to this disease may be related to the genes responsible for embryonic development of the hypothalamus-pituitary area. Moreover, patients with isolated growth hormone deficiency are seen to have a higher risk of congenital malformations as compared to those having multiple anterior pituitary deficiencies [3]. The patient presents with the features of anterior pituitary hormonal deficiency however mild hyperprolactinemia may be seen due to the inability of dopamine to inhibit the lactotrophs in the absence of the pituitary stalk [4]. PSIS is characterized by the presence of a thin or interrupted pituitary stalk, associated hypoplastic or aplastic anterior pituitary, and ectopic posterior pituitary (EPP) on magnetic resonance imaging (MRI) [5]. The ectopic neurohypophysis is most commonly seen in the infundibular recess (60.4%) or the hypothalamus (18.9%) [6]. Location of EPP has functional prognostic significance since a greater number of anterior pituitary hormone deficiencies is seen when the posterior pituitary is present at the median eminence or hypothalamic region [7]. The importance of early diagnosis and treatment lies in the fact that firstly, if it remains untreated it is associated with significant mortality and morbidity, and secondly, insufficient height at the onset of puberty leads to short final height. Early diagnosis and treatment of growth hormone deficiency is necessary to allow growth to reach a normal height before puberty [8].
Conclusion
PSIS is a rare congenital abnormality and should be kept as a differential in a patient presenting with anterior pituitary hormonal deficiency. Early diagnosis is crucial for preventing adverse effects on long-term growth and development. MRI findings are confirmatory for the diagnosis of PSIS.
Patient consent
All the images used in this manuscript are anonymized. Consent for the publication of this case report was obtained from the patient's legal guardian.
Footnotes
Competing Interests: We do not have any financial/personal interests for the publication of this case report.
References
- 1.El Chehadeh-Djebbar S, Callier P, Masurel-Paulet A, et al. 17q21.31 microdeletion in a patient with pituitary stalk interruption syndrome. Eur J Med Genet. 2011;54(3):369–373. doi: 10.1016/j.ejmg.2011.03.001. [DOI] [PubMed] [Google Scholar]
- 2.Tauber M, Chevrel J, Diene G, et al. Long-term evolution of endocrine disorders and effect of GH therapy in 35 patients with pituitary stalk interruption syndrome. Hormone Res Paediatr. 2005;64(6):266–273. doi: 10.1159/000089425. [DOI] [PubMed] [Google Scholar]
- 3.Pinto G, Netchine I, Sobrier ML, Brunelle F, Souberbielle JC, Brauner R. Pituitary stalk interruption syndrome: a clinical-biological-genetic assessment of its pathogenesis. J Clin Endocrinol Metab. 1997;82(10):3450–3454. doi: 10.1210/jcem.82.10.4295. [DOI] [PubMed] [Google Scholar]
- 4.Gosi SK, Kanduri S, Garla VV. Pituitary stalk interruption syndrome. BMJ Case Rep. 2019;12(4):25–26. doi: 10.1136/bcr-2019-230133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Simmons GE, Suchnicki JE, Rak KM, Damiano TR. MR imaging of the pituitary stalk: size, shape, and enhancement pattern. Am J Roentgenol. 1992;159(2):375–377. doi: 10.2214/ajr.159.2.1632360. [DOI] [PubMed] [Google Scholar]
- 6.Yang Y, Guo QH, Wang BA, Dou JT, Lv ZH, Ba JM, et al. Pituitary stalk interruption syndrome in 58 Chinese patients: clinical features and genetic analysis. Clin Endocrinol. 2013;79(1):86–92. doi: 10.1111/cen.12116. [DOI] [PubMed] [Google Scholar]
- 7.Chen S, Léger J, Garel C, Hassan M, Czernichow P. Growth hormone deficiency with ectopic neurohypophysis: anatomical variations and relationship between the visibility of the pituitary stalk asserted by magnetic resonance imaging and anterior pituitary function. J Clin Endocrinol Metab. 1999;84(7):2408–2413. doi: 10.1210/jcem.84.7.5849. [DOI] [PubMed] [Google Scholar]
- 8.Papastathopoulou L, Tzanela M, Vlassopoulou V, Vassiliadi D, Thalassinos N. Untreated hypopituitarism due to absence of the pituitary stalk with normal adult height: report of two cases. Endocrine. 2006;29(1):175–180. doi: 10.1385/endo:29:1:175. [DOI] [PubMed] [Google Scholar]