Abstract
We identified preferences toward Community Preventive Services Task Force (CPSTF)-recommended intervention approaches among screen-eligible Zuni Pueblo members in New Mexico, USA and assessed if there were significant differences in those preferences, with the goal of informing the selection of intervention approaches for use in the Zuni Pueblo. We utilize data from a population-based survey (n = 280) focused on 15 CPSTF-recommended intervention approaches designed to improve screening for cervical, breast, and/or colorectal cancer screening. Model-adjusted results suggest some intervention approaches garnered significantly higher support than others. We offer six, data-driven recommendations for consideration by public health practitioners as they endeavor to improve cancer prevention in the Zuni Pueblo. This study provides a replicable model for other public health practitioners and health services researchers to incorporate community preferences in community-level intervention approach selection.
Keywords: Breast neoplasm, Colorectal neoplasm, Cervical neoplasm, Cancer screening, Health equity, American Indians, Community-based participatory research
1. Introduction
The Community Preventive Services Task Force (CPSTF) recommends multicomponent interventions to increase breast, cervical, and colorectal cancer screenings. CPSTF currently recommends that public health practitioners implement two or more intervention approaches intervention approaches that increase community demand or provider delivery of screening services, as well as two or more intervention approaches that reduce structural barriers (CPSTF, 2016). However, this leaves perpetually strained public health systems to choose from over a dozen CPSTF-recommended intervention approaches, many of which are labor and/or capital intensive. Additionally, CPSTF recommends that community preferences should also be considered. Specific demographic, structural, cultural, and/or socioeconomic matters may exist in certain communities, that may attenuate the effectiveness of some, or all, of the recommended intervention approaches (Braun et al., Jun 2005, Blumenthal et al., 2010, Mishra et al., 2023). Public health practitioners therefore need to strategically choose from these intervention approaches to maximize their impact on screening rates and, ultimately, decrease cancer incidence and mortality. The confluence of these three factors—a strained public health system, a unique sociocultural context, and below-average cancer screening rates (Cartwright et al., 2023, Edwardson et al., 2023) —occurs in the Zuni Pueblo, a relatively isolated, rural American Indian community in western New Mexico. To begin to address this dilemma, we present survey results among screen-eligible members of the Zuni Pueblo on their preferences toward CPSTF-recommended intervention approaches and assess if there are significant differences in those preferences. These findings will inform public health practitioners in the Zuni Pueblo of their population’s preferences, optimize their selection of intervention approaches, provide a replicable model for other community-based public health practitioners, and further contribute to the CPSTF evidence base.
2. Materials and methods
We conducted an observational, cross-sectional study using a population-based survey on the Zuni Pueblo in October 2020 through April 2021. Zuni is a Pueblo Tribe located approximately 150 miles west of Albuquerque, New Mexico, in a relatively isolated, rural setting. Information on the survey sample and design has been previously published (Cartwright et al., 2023, Edwardson et al., 2023). The final completed sample consisted of 280 participants, all of whom had to self-identify as American Indian, be a member of the Zuni tribe, or be married to a Zuni tribal member, and had to be sex- and age-eligible for screening for any of the three cancer types (cervical: female, 21–75; breast: female, 50–75; and colorectal: 50–75). The focus of this study included questions regarding preferences for 15 CPSTF-recommended intervention approaches. Participants were asked to indicate (Yes or No) if they would like to see implementation any of the 15 intervention approaches (see Table 1) to help increase cervical, breast, and/or colorectal cancer screening. The Southwest Tribal Institutional Review Board (IRB) (SWT-2018–004) and the University of New Mexico Health Sciences Center IRB (HRRC # 18–264) approved the protocol.
Table 1.
Number and percentage of respondent preferences for CPSTF intervention approaches (IAs).
 |
*Bonferroni-corrected p value cutoff = 0.05/60 = 0.00083.
We compared preferences across age categories, sex, and whether a respondent had ever been screened for breast, cervical, and/or colorectal cancer using chi-square, while adjusting for multiple comparisons (Bonferroni-corrected p value cutoff = 0.05/60 = 0.00083). We used a single logistic regression model to simultaneously predict the probability that each intervention approach was endorsed while adjusting for repeated responses per individual using generalized estimating equations (Hanley et al., 2003) (GEE) and to simultaneously test for differences among the intervention approach-specific endorsement probabilities. We estimated predicted probabilities and their confidence intervals for each intervention approach and tested for differences in endorsement probabilities between all intervention approach pairs. To confirm that our GEE approach adequately accounted for potential differences among respondents based on individual-level characteristics, we also ran a separate, confirmatory multivariable logistic regression model that adjusted for within-person correlations via our original GEE approach while also including age, sex, and prior screening status as adjustment factors. The comparisons between the two models’ estimated predicted probabilities were essentially unchanged. For parsimony, we report only the GEE estimated predicted probabilities here. (Multivariable model results and predictions are available from authors upon request.) To further inform Zuni public health practitioners in their selection of intervention approaches, we attempted to group intervention approaches by levels of preference and CPSTF categorization by evaluating all pairwise differences in endorsement probabilities for the intervention approaches.
3. Results
Among the 280 respondents, 61 % (171/280) were female. Among female respondents, 36 % (61/171) were aged 21–49 years old, with the remainder aged 50–75 years old. Among respondents and their screening status, 42 % (92/219) reported having never been screened for colorectal cancer, 25 % (43/171) reported having never been screened for cervical cancer, and 14 % (15/110) reported having never been screened for breast cancer.
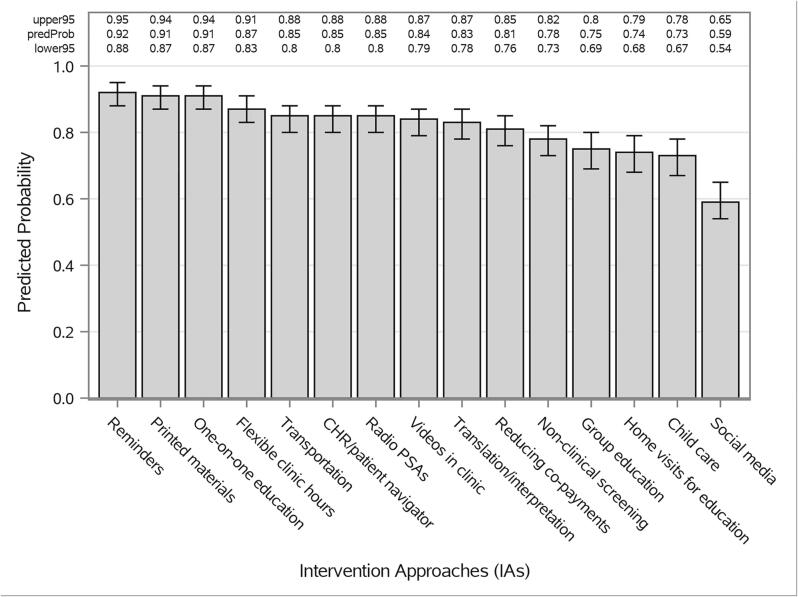
Preferences for the 15 intervention approaches were generally favorable, although some intervention approaches received more support than others (Table 1). Three intervention approaches—reminders, printed informational materials, and one-on-one education—were endorsed by 91 % or more of respondents. Seven intervention approaches received levels of support between 81 % and 88 %, four received 73 % to 78 % support, and one—using social media—garnered the least support at 60 %.
Support of intervention approaches did not differ significantly across categories of age and sex, and whether a respondent had ever been screened for breast, cervical, and/or colorectal cancer after Bonferroni correction for 60 comparisons (Table 1).
There were significant differences in degree to which intervention approaches were endorsed (p < 0.001). The least popular option—using social media—had significantly lower support than all other intervention approaches (Fig. 1). The next four least popular options—offering screening through non-clinical settings; group education; home visits for education; and offering childcare services—were significantly less preferred than all other options, with the exception that offering screening through non-clinical settings was not significantly less preferred than reducing co-payments for testing. The three most popular options—reminders, printed materials, and one-on-one education—did not differ significantly from one another but did differ significantly from almost all other options. The exceptions were that printed materials and one-on-one education did not differ significantly from having flexible clinic hours.
Fig. 1.
Predicted Probabilities and their 95% Confidence Intervals for all Intervention Approaches (IAs).
4. Discussion
Despite their growing evidence of effectiveness, CPSTF-recommended intervention approaches can require substantial time and resource investments. Not all intervention approaches, and in most cases only a select few, can be implemented and sustained by public health practitioners (Mishra et al., 2023). In this study we identified preferences toward intervention approaches among Zuni Pueblo members and assessed differences in those preferences, with the goal of informing Zuni public health practitioners in their selection of intervention approaches.
Results point to three statistically significant preferred intervention approaches: reminders, printed materials, and one-on-one education. While no other studies have evaluated preferences among Zuni adults, other similar studies in localized communities yielded similar preferences for these three intervention approaches (Shokar et al., 2021). These three intervention approaches fit within CPSTF’s category of “Increasing community demand,” of which CPSTF recommends implementing two or more intervention approaches. This leaves two additional intervention approaches that would need to be selected from CPSTF’s category of “Reducing structural barriers.” Conveniently, according to our model the next three most preferred intervention approaches—having flexible clinic hours; offering transportation to the clinic; and having community health representatives (CHRs) help obtain screening—all fall within this category. Each of these three intervention approaches were endorsed by more than 85 % of respondents and should be given strong consideration.
A pleasantly surprising finding was that no significant differences for intervention approach preferences were found across participants who had, versus those who had never been screened for the three cancer types, with differences between these groups typically being less than five percentage points. This finding should reassure Zuni public health practitioners, who need to simultaneously focus on both those who have never been screened and those who are due for repeat screenings. CPSTF notes in their systematic reviews that few, if any, studies have evaluated the effectiveness of recommended intervention approaches for repeat screening (CPSTF, 2016).
This study is not without limitations. Given the cross-sectional design of the survey and its quasi-convenience sample strategy, participation rate and non-response bias could not be addressed. It is also possible that different groups of Zuni adults might have different preferred intervention approaches according to their individual characteristics. To examine this in a preliminary fashion, we performed analyses that tested for evidence of significantly different patterns or participant preferences of the various intervention approaches across groups defined by age, gender, income, education, and employment. These comparisons were not pre-planned and were based on a sample size that was not adequate to robustly evaluate the presence or absence of meaningful interactions. Furthermore, most of them failed to demonstrate differences in endorsement probabilities for specific intervention approaches across these different groups. However, exploratory analysis suggested that there may be differences according to an individual’s age group. For example, those aged 21–49 appear to be less interested in receiving home visits for education and more interested in taking advantage of flexible clinic hours than those aged 50–75. These exploratory findings suggest that further study is likely warranted to explore the potential for differences in preferences for intervention approaches by age and other key individual-level characteristics. Additionally, given the focused intent of the study—to evaluate preferences of Zuni adults whose culture and beliefs are as unique as their geography and history—these results have limited generalizability. For example, the intervention approach “reducing co-payments for testing” may have been a less preferred intervention approach in this context as Zuni adults who do not have private insurance are offered no cost screening services through Indian Health Services providers. Therefore, it is possible that this specific intervention approach does not resonate with Zuni adults to the same degree it might in other communities and patient populations. But this limitation is also a strength—this study contributes to a greater understanding of a specific American Indian Tribe’s distinct preferences within the context of improved cancer prevention and control. This study offers specific, data-driven recommendations to be considered by Zuni public health practitioners as they endeavor to improve the health of their Tribal members. Additionally, this study provides a replicable model for other public health practitioners and health services researchers to incorporate community preferences in community-level intervention approach selection, which is recommended by CPSTF but for which no specific guidance has been provided to date.
Funding
This research was supported by the National Cancer Institute of the National Institutes of Health grant R01CA192967 (Mishra PI), UNM Comprehensive Cancer Center (UNMCCC) Support Grant NIH/NCI P30CA118100 (Sanchez, PI), supplements to the UNMCCC Support Grant P30CA118100 (Sanchez PI; Mishra, PD), UNMCCC institutional pilot awards (PP-U1418-RS, PP-U1402-CaC, Mishra, PI), the UNMCCC Behavioral Measurement and Population Science and the Biostatistics Shared Resources, and the Institutional Development Award (IDeA) from the NIH/NIGMS P20GM103451 under the New Mexico IDeA Networks of Biomedical Research (NM-INBRE) Developmental Research Project Program (Mishra, PI of the Developmental Research Project).
CRediT authorship contribution statement
Nicholas Edwardson: Conceptualization, Formal analysis, Investigation, Writing – original draft. Mikaela Kosich: Methodology, Formal analysis, Investigation, Writing – review & editing. V. Shane Pankratz: Methodology, Formal analysis, Investigation, Writing – review & editing. Judith Sheche: Formal analysis, Investigation, Writing – review & editing, Resources. Kate Cartwright: Formal analysis, Investigation, Writing – review & editing. Deborah Kanda: Methodology, Formal analysis, Investigation, Writing – review & editing. Samantha Leekity: Writing – review & editing, Resources. Shiraz I. Mishra: Conceptualization, Formal analysis, Investigation, Writing – review & editing, Funding acquisition, Resources, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors gratefully acknowledge the Tribal stakeholders, including the Zuni Tribal Governor and Tribal Council members and the Tribal Advisory Panel members who contributed to the study activities. The authors are also grateful to the Zuni people for welcoming us into their lives, and sincerely thank the men and women from the Zuni Pueblo who participated in the survey. The authors also acknowledge the contributions of the University of New Mexico Health Sciences Center staff (Donica Ghahate and Keith Kelly) and the UNMCCC’s Behavioral Measurement and Population Science Shared Resource staff (Joseph Rodman).
Data availability
The authors do not have permission to share data.
References
- Blumenthal D.S., Smith S.A., Majett C.D., Alema-Mensah E. A trial of 3 interventions to promote colorectal cancer screening in African Americans. Cancer. 2010;116(4):922–929. doi: 10.1002/cncr.24842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braun K.L., Fong M., Kaanoi M.E., Kamaka M.L., Gotay C.C. Testing a culturally appropriate, theory-based intervention to improve colorectal cancer screening among Native Hawaiians. Prev. Med. Jun 2005;40(6):619–627. doi: 10.1016/j.ypmed.2004.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cartwright K., Leekity S., Sheche J., Kanda D., Kosich M., Rodman J., Gonya M., Kelly K., Edwardson N., Pankratz V.S., Mishra S.I. Health literacy, health numeracy, and cancer screening patterns in the Zuni Pueblo: insights from and limitations of “standard” questions. J. Cancer Educ. 2023;38(3):1023–1033. doi: 10.1007/s13187-022-02227-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Community Preventive Services Task Force (CPSTF). Cancer Screening: Multicomponent Interventions—Colorectal Cancer. The Community Guide. 2016.
- Edwardson N., Cartwright K., Sheche J., Pankratz V.S., Kosich M., Kanda D., Leekity S., Mishra S.I. Colorectal cancer screening among adults in zuni pueblo: factors associated with FOBT and colonoscopy utilization. J Commun Health. 2023;48(4):565–575. doi: 10.1007/s10900-023-01196-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanley J.A., Negassa A., Edwardes M.D., Forrester J.E. Statistical analysis of correlated data using generalized estimating equations: an orientation. Am. J. Epidemiol. 2003;157(4):364–375. doi: 10.1093/aje/kwf215. [DOI] [PubMed] [Google Scholar]
- Mishra S.I., Adsul P., Leekity S., Rodman J., Sussman A.L., Kelly K., Sheche J., Faber T., Shah V. A culturally informed model to enhance breast, cervical, and colorectal cancer screenings: perspectives of American Indian adults and healthcare providers in rural New Mexico. Cancer Cause Control. 2023;34(10):855–871. doi: 10.1007/s10552-023-01721-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shokar N.K., Calderon-Mora J., Molokwu J., Byrd T., Alomari A., Mallawaarachchi I., Dwivedi A. Outcomes of a multicomponent culturally tailored cervical cancer screening intervention among underserved hispanic women (De Casa en Casa) Health Promot. Pract. 2021;22(1):112–121. doi: 10.1177/1524839919893309. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The authors do not have permission to share data.