Abstract
Background:
In early 2021, CDC released the CORE Health Equity Strategy, which resolves to integrate a comprehensive health equity approach to the work of the Agency. One priority of the Injury Center’s Division of Injury Prevention is to move health equity research in injury forward. The purpose of this research is to perform an initial exploration of health equity guiding frameworks and indices to better understand which of these has been applied to injury research topics.
Methods:
A PubMed and CINAHL search of meta-analysis and systematic review articles was conducted from January 1998 through April 2022. Articles of any type and additional frameworks/indices were also identified from staff knowledge of the literature. Books were also considered, where accessible. The following areas were reviewed for each resource: population addressed, guiding framework/index, other health equity variables, gaps identified, and whether the articles addressed an injury topic.
Findings:
The PubMed/CINAHL search produced 230 articles, and an additional 29 articles and 8 books were added from previous knowledge of the literature, resulting in a total of 267 resources for review. There were 60 frameworks/indices compiled that were relevant to health equity. Out of all the resources, three reported on an injury topic and used the PROGRESS-Plus framework, the WHO Social Determinants of Health Conceptual Framework, and a social-ecological framework.
Conclusions:
This study found there were many frameworks/indices for measuring health equity; however, there were few injury-related meta-analysis and systematic review articles. Some frameworks/indices may be more appropriate than others for measuring health equity in injury topic areas, depending on which social determinants of health (SDOHs) they address.
Practical Applications:
Measuring health equity in injury and other public health research areas can help build a foundation of evidence. Moving forward, injury researchers can consider the frameworks/indices identified through this study in their health equity injury research.
Keywords: Injury, Framework, Index, Health equity, Social determinants of health
1. Introduction
The Centers for Disease Control and Prevention (CDC) defines health equity as the opportunity for all persons to attain their highest level of health, regardless of social position or other socially determined conditions (CDC NCCDPHP, 2020). Health disparities explain health differences between groups that are related to economic, social, or environmental disadvantage (Department of Health and Human Services, 2020). The metrics for gauging progress towards health equity are disparities in health and disparities in the key determinants of and obstacles to health (Robert Wood Johnson Foundation, 2017). Economic and social obstacles such as poverty, unemployment, and lack of access to health care prohibit underserved communities from achieving optimal health, leading to higher rates of disease, decreased access to treatment, and premature death. These barriers often disproportionally impact people of color, rural and low-income urban communities, individuals with disabilities, and members of the LGBTQ + community (CDC NCCDPHP, 2020).
Injuries, both intentional and unintentional, are a significant public health challenge. In 2020, injuries and violence accounted for almost 280,000 deaths in the United States and represented the leading causes of death among those aged 1–44 (CDC NCIPC, 2020). Recent publications highlight disparities in rates of injuries by socio-demographic groups, geography, and other factors (Clemens et al., 2021; Ehlman et al., 2022; Daugherty et al., 2021; Moore et al., 2019). For example, an analysis of trends from 1999–2019 in fatal unintentional drowning among persons aged < 29 found continuing racial/ethnic disparities. Non-Hispanic (NH) American Indian/Alaskan Native (AI/AN) and NH Black persons experienced the highest rates (Clemens et al., 2021). An analysis of suicide rates from 2019 to 2020 likewise found demographic and geographic disparities with higher rates in rural counties and among men, NH AI/AN and NH White persons, and specific age groups (Ehlman et al., 2022). A study of traumatic brain injuries demonstrated geographic variability across regions of the United States with more rural states exhibiting higher rates (Daugherty et al., 2021). Moore et al.’s (2019) scoping review identified a significant body of research seeking to understand injuries and disparities and underscored the need to better measure and understand the demographic, economic, social, and environmental factors impacting risk and effective interventions to advance health equity.
In April 2021, Dr. Rochelle P. Walensky, Director of the CDC, declared racism a critical public health threat. In response, CDC released the CORE Health Equity Strategy to ensure the work of every center, division, and program remains committed to addressing health disparities in science, research, and partnerships (CDC OMHHE, 2022). Furthermore, the CORE Health Equity Strategy utilizes a comprehensive health equity approach to guide CDC and the field of public health in advancing efforts towards eliminating health disparities:
C: Cultivate comprehensive health equity science
O: Optimize interventions
R: Reinforce and expand robust partnerships
E: Enhance capacity and workforce engagement (CDC OMHHE, 2022).
To help move the work of the CORE Health Equity Strategy forward, the Injury Center’s Division of Injury Prevention (DIP) aims to broaden understanding of health equity within the Division and the field of public health more broadly, including how health equity can be measured. The purpose of this research is to begin to compile and categorize health equity guiding frameworks and indices and document those that have already been applied to injury research topics. This study focused largely on meta-analysis and systematic review articles due to the high volume of individual studies that incorporate a health equity guiding framework or index. In this study, the term ‘injury’ is used to refer to both unintentional and intentional injury. The findings of this study can be used to assist researchers in understanding the scope and characteristics of health equity guiding frameworks and indices captured in the literature.
2. Method
The study included meta-analysis and systematic review articles published between January 1, 1998, through April 30, 2022, and also included articles and health equity guiding frameworks and indices sourced from previous knowledge of the literature. A literature search was conducted through PubMed and CINAHL (using the search terms “Health Equity”[Mesh] OR “Social Determinants of Health”[Mesh]). Books were considered, where accessible, and attempts were made to source books from university syllabi. Exclusion criteria were applied to focus the content of articles captured in the review. Articles were excluded if they were clinical-specific, were not written in English, did not have a full text available, were duplicates, or if they did not address SDOHs and/or health equity using a specific framework or measurement. For the purposes of this research, a health equity guiding framework/index was defined as a theoretical construct or standardized measure that assesses key domains and concepts associated with health equity. These key categories included: income, education, geography, gender, race/ethnicity, occupation/employment, housing, food access, energy access, childcare, transportation, environmental conditions/exposure, nativity/country of origin, power/prestige, social capital, health literacy, and access to health care.
Citations for each article and book identified in the searches were exported into an Excel file to organize for reviewing. The full text articles were split for reviewing between two reviewers (NL and AC), and data were abstracted for the following categories, when available: population addressed, health equity guiding framework/index, other notable health equity variables, gaps identified, and whether the articles addressed an injury topic. Each reviewer reviewed a sample of five articles reviewed by the other reviewer, to ensure consistency of coding.
3. Results
The database search produced 227 articles from PubMed and 3 articles from CINAHL, and an additional 29 articles and 8 books were added from previous knowledge of the literature, resulting in a total of 267 resources (articles and books) identified for review (Fig. 1). Seventeen resources were clinical-specific, eight resources were not written in English, six resources did not have full text available, and one resource was a duplicate, and thus 32 resources were excluded from the study. Out of the remaining 235 resources, upon review it was found that 160 resources did not mention a specific health equity framework or index addressing social determinants of health (SDOH) and/or health equity and were excluded from the study. In total, 75 resources were categorized as mentioning a health equity guiding framework or index (Table 1).
Fig. 1.
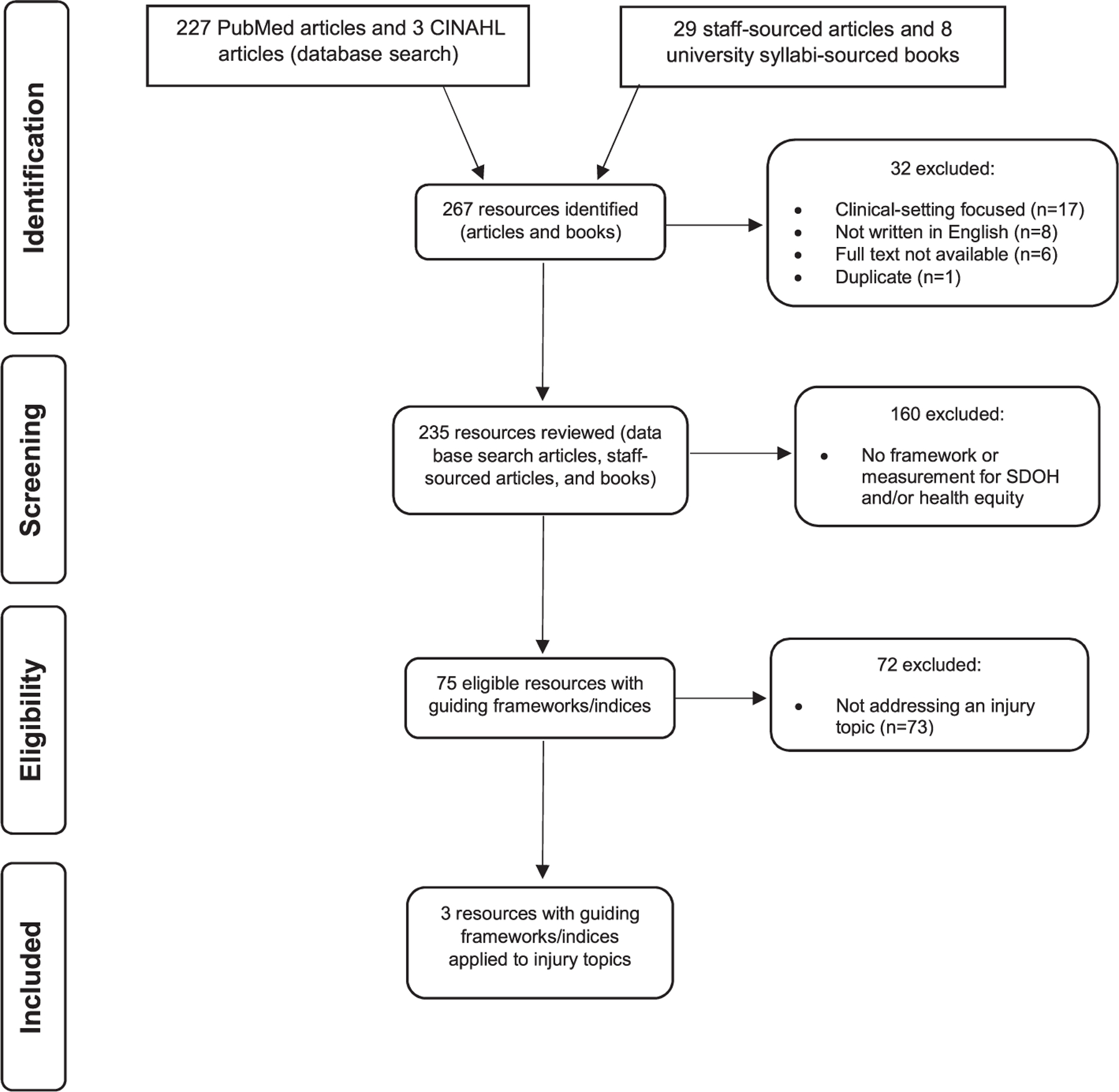
Flowchart.
Table 1.
Characteristics of eligible resources mentioning health equity guiding frameworks and indices.
| Citation1 | Population(s) Addressed | Guiding Framework/Index | Injury related? |
|---|---|---|---|
| Armstead et al., 2021 2 | Not specified | WHO Conceptual SDOH Framework | Yes (violence indicators) |
| Brown et al., 2017b | Caribbean residents | PROGRESS-Plus | Yes (suicide/depression) |
| Reno & Hyder, 2018 | African American infants | Social-Ecological Model | Yes (infant mortality-safe sleep, drugs, abuse) |
| Abbott & Williams, 2015 | African Americans living with HIV in rural southeast | Healthy People 2020 SDOH Framework | No (HIV) |
| Ahmed et al., 2022 | Community health workers in low- and middle-income countries | PROGRESS | No (community health worker interventions) |
| Allen et al., 2020 | Not specified | WHO Conceptual SDOH Framework; Social-Ecological Model | No (noncommunicable diseases) |
| Aves et al., 2017 | Not specified | PROGRESS-Plus | No (HIV) |
| Batista et al., 2018 | Immigrants | WHO Conceptual SDOH Framework | No (health care models) |
| Berkman et al., 2014 | Not specified | Gini coefficient | No (general concepts) |
| Bhojani et al., 2019 | Ethnic and religious minorities in India | WHO Conceptual SDOH Framework | No (legislation) |
| Bowers et al., 2020 | Inuit population in Canada | Dimensions of food security (Food and Agricultural Organization) | No (food security) |
| Braveman, 1998 2 | Low- and middle-income countries | Policy-oriented approach | No (social disparities) |
| Braveman, 2003 2 | Social groups with varying levels of social advantage | Conceptual framework for monitoring equity in health and healthcare | No (conceptual model for health and healthcare equity) |
| Brown et al., 2017a | Caribbean women | WHO Conceptual Social Determinants of Health Framework (adaptation) | No (breast cancer) |
| Buttazzoni et al., 2020 | Urban cities | PROGRESS-Plus; Smart City 2.0 Paradigm | No (urban health) |
| Campos-Matos et al., 2016 | Portuguese individuals | PROGRESS | No (general health) |
| Chandanabhumma & Narasimhan, 2020 | Marginalized communities | Applied Decolonial Framework for Health Promotion | No (social justice/health promotion) |
| Chandler et al., 2022 | Public health students | Three Levels of Racism Framework | No (student training) |
| Chen et al., 2020 | Not specified | Healthy People 2020 SDOH Framework; Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE); WHO Conceptual SDOH Framework | No (healthcare) |
| Chhibber et al., 2021 | Policies | PROGRESS-Plus | No (policy) |
| Christidis et al., 2021 | Australian Aboriginal and Torres Strait Islanders | Social-Ecological Model | No (Aboriginal health/nutrition) |
| Cohn & Harrison, 2022 | Black women | PROGRESS-Plus | No (sexual health) |
| De Lima Silva et al., 2014 | Elderly | Dahlgren and Whitehead model | No (mortality) |
| Diez Roux, 2012 2 | Racial/ethnic minorities | Fundamental Cause Model; Interaction Model; Pathways Model; | No (conceptual frameworks) |
| Dover & Belon, 2019 | Public health workforce | Health equity measurement framework; WHO Conceptual SDOH Framework | No (health equity framework/measurement) |
| Dressler et al., 2005 2 | Black Americans | Health behavior model; socioeconomic status model; psychosocial stress model; structural-constructivist model | No (theoretical models) |
| Driscoll et al., 2013 | Not specified | Dahlgren and Whitehead model | No (circumpolar population health) |
| Fairfield et al., 2020 2 | Rural; low SES | Area Deprivation Index (ADI) | No (lung cancer) |
| Forde et al., 2019 | Socially and economically disadvantaged groups | Weathering hypothesis | No (racial health disparities) |
| Freire et al., 2018 | Older adults | Human Development Index (HDI) | No (gait performance) |
| Gee & Payne-Sturges, 2004 2 | Racial/ethnic minorities | Community Stress Theory; Index of Dissimilarity; Stress-Exposure Disease Framework | No (environmental health) |
| Ghiasvand et al., 2020 | HIV infected populations | Social and demographic determinants of health-related quality of life (QoL) | No (disparities in HIV QoL) |
| Greenbaum et al., 2018 | Human trafficking victims and their families and communities | Social-Ecological Model | No (human trafficking) |
| Habbab & Bhutta, 2020 | Saudi adolescents | Social-Ecological Model | No (pediatric obesity) |
| Hu et al., 2018 2 | Urban; low SES | Area Deprivation Index (ADI) | No (readmissions) |
| Karger et al., 2022 | Indigenous and culturally and linguistically diverse (CALD) infants | Social-Ecological Model | No (pregnancy andchildbirth) |
| Kolahdooz et al., 2015 | Indigenous Canadian populations | Integrated Life Course and Social Determinants Model of Aboriginal Health | No (SDoH) |
| Krieger et al., 2003 2 | Diverse race/ethnicity-gender groups | Area-based socioeconomic measures (ABSMs) | No (public health monitoring) |
| Lehne & Bolte, 2017 | Older adults aged 50+ | PROGRESS-Plus | No (physical activity) |
| Lorenc et al., 2014 | Local policymakers, practitioners or anyone with a local-level decision-making role | Health In All Policies | No (policy) |
| Lund et al., 2018 | Not specified | Social and cultural determinants of mental disorders | No (mental disorders) |
| Malele-Kolisa et al., 2019 | Children in Africa | International Classification of Functioning, Disability and Health (ICF) model; Oral health-related quality of life (OHRQoL) conceptual framework | No (children’s oral health/quality of life) |
| Maness & Buhi, 2016 | Young females of reproductive age (aged 13–25) | Healthy People 2020 SDOH Framework | No (pregnancy) |
| Min et al., 2022 | Asian Americans (and subgroups) | Healthy People 2030 SDOH Framework; WHO Conceptual SDOH Framework | No (cardiometabolic disease) |
| Mohan & Chattopadhyay, 2020 | Underserved, vulnerable populations | Healthy People 2020 SDOH Framework; Public Health 3.0 Model | No (cost-effectiveness) |
| Morton et al., 2016 | Adults with moderate to severe chronic kidney disease (CKD) | PROGRESS | No (kidney disease) |
| Nooh et al., 2019 | Mobile pastoralist communities in Ethiopia | Equity-effectiveness model | No (disease control) |
| Ortiz et al., 2020 | Not specified | Community-based participatory research (CBPR) conceptual model | No (community engagement) |
| Owusu-Addo et al., 2018 | Those targeted by either conditional or unconditional cash transfers | WHO Conceptual SDOH Framework | No (cash transfers) |
| Payne-Sturges & Gee, 2006 2 | Racial/ethnic minorities; low SES | Framework for understanding racial/ethnic disparities in environmental health; Index of dissimilarity | No (environmental health) |
| Payne-Sturges et al., 2006a 2 | Racial/ethnic minorities; low SES | Stress-Exposure Disease Framework | No (environmental health) |
| Payne-Sturges et al., 2006b 2 | Racial/ethnic minorities | Multi-level systems approach | No (environmental health) |
| Pereira et al., 2019 | Children w/obesity | Social-Ecological Model | No (children’s health) |
| Peterson et al., 2021 | Public health practitioners and researchers | Health equity framework | No (health equity frameworks/framework development) |
| Rajmil et al., 2020 | Children in European countries | Social determinants on child health (SDCH) | No (children’s health) |
| Restar et al., 2021 | Transgender populations | Gender-based health equity framework for transgender populations | No (gender-based framework/framework development) |
| Salgado et al., 2020 | Urban settings | Environmental determinants of health (EDoH) | No (urban health) |
| Schröders et al., 2015 | Disadvantaged groups in Indonesia | PROGRESS | No (child/infant mortality) |
| Schüz et al., 2021 | Not specified | PROGRESS-Plus | No (dietary nudging interventions) |
| Sokol et al., 2019 | Children | Healthy People 2020 SDOH Framework | No (children’s health) |
| Srivastava et al., 2022 | Not specified | Area Deprivation Index (ADI); COVID-19 Community Vulnerability Index (CCVI); Healthy Places Index (HPI); Social Vulnerability Index (SVI) | No (COVID-19 vaccination) |
| Taggart et al., 2020 | Black adolescent girls and young adult women | Life Course Approach | No (women’s health) |
| Taylor & Lamaro Haintz, 2018 | Australian refugees | Social-Ecological Model | No (healthcare services access) |
| The National Academies of Sciences, Engineering, and Medicine, 2016 | Not specified | Danaher Framework; Rural Community Health & Well-Being Framework; WHO Conceptual SDOH Framework; The Frieden Framework; A Public Health Framework for Reducing Health Inequities | No (education for health professionals) |
| Tulier et al., 2019 | Urban populations | Fundamental Cause Model | No (urban health inequities) |
| Turnbull et al., 2020 | People with chronic health conditions | PROGRESS-Plus | No (chronic disease interventions) |
| van Daalen et al., 2021 | Not specified | Health equity audits (HEA) | No (service provision) |
| van Hees et al., 2019 | Low- and middle-income countries; vulnerable groups | Equiframe; Social, Political, Economic and Cultural (SPEC) conceptual model (WHO) | No (health care reform) |
| Wang et al., 2020 | Pregnant women | WHO Conceptual SDOH Framework | No (maternal health) |
| Welch et al., 2022 | Not specified | PROGRESS-Plus | No (interventions) |
| Wilder et al., 2021 | United States adults | Healthy People 2020 SDOH Framework | No (chronic disease management) |
| Wilkerson, 2021 2 | Communities; racial/ethnic minorities; low SES | Systems perspective | No (social connection) |
| Yelton et al., 2022 | Adult African American population in the United States | Healthy People 2030 SDOH Framework | No (depression/mental health) |
| Yiga et al., 2020 | Women of reproductive age in sub-Saharan Africa | Yiga et al., 2020 | Women of reproductive age in sub-Saharan Africa |
| Zahnd & McLafferty, 2017 | People with cancer | Warnecke’s Model for Analysis of Population Health and Disparities | No (cancer) |
Citations were sourced from a PubMed/CINAHL literature search of meta-analysis and systematic review articles using the search terms ‘‘Health Equity”[Mesh] OR ‘‘Social Determinants of Health”[Mesh] and CDC Injury Center staff previous knowledge of the literature.
Indicates citations sourced from previous knowledge of the health equity literature.
There were 60 unique health equity guiding frameworks/indices abstracted from the resources (Table 2). Fourteen resources mentioned more than one health equity guiding framework/index. The most commonly mentioned health equity guiding frameworks/indices were the PROGRESS/PROGRESS-Plus framework (n = 13), the World Health Organization (WHO) SDOH Conceptual Framework (n = 11), and the Social-Ecological Model (n = 9) (Table 2). The most common SDOHs addressed by the health equity guiding frameworks/indices were income, education, race/ethnicity, and occupation/employment.
Table 2.
Health equity guiding frameworks and indices.
| Health Equity Guiding Framework/Index | Description | Scale (where applicable) | Citations1 |
|---|---|---|---|
| A Public Health Framework for Reducing Health Inequities | Depicts the relationship between social inequalities and health, with a specific focus on inequities related to social, institutional, and living conditions. | The National Academies of Sciences, Engineering, and Medicine, 2016 | |
| AHRQ Social Determinants of Health Beta Data Files3 | With funding from the Patient-Centered Outcomes Research Trust Fund, AHRQ has created multi-year (2009−2018) social determinants of health (SDOH) beta data files curated from multiple federal and other data sources; variables in the beta data files correspond to five key SDOH domains: (1) social context, (2) economic context, (3) education, (4) physical infrastructure, and (5) healthcare context. | Agency for Healthcare Research and Quality, 2021 | |
| Applied Decolonial Framework for Health Promotion | Provides guidance to public health practitioners on integrating decolonial processes into health promotion practice to achieve social justice and eliminate health inequities. | Chandanabhumma & Narasimhan, 2020 | |
| Area Deprivation Index (ADI) | Assesses a region’s socioeconomic conditions to identify areas that have high levels of deprivation and may be more vulnerable to adverse health outcomes. | Geographic percentile rankings range from 1–100; higher score = more highly disadvantaged | Srivastava et al., 20223; Hu et al., 20183; Fairfield et al., 20203 |
| Area-based socioeconomic measures (ABSMs) | Draws on multilevel frameworks and area-based measures to characterize the cases (numerator) and catchment population (denominator), therefore enabling the calculation of rates stratified by the socioeconomic characteristics of a particular residential area. | Higher value = less advantaged | Krieger et al., 2003 3 |
| Community Resilience Estimate (CRE)3 | Uses three different data sources (Community Resilience Estimates, American Community Survey, and Census Bureau’s Planning Database) to provide information about the capacity of communities and neighborhoods in the United States to respond to the impacts of disasters. | CREs are categorized into three groups: 0 risks, 1–2 risks, and 3 plus risks | United States Census Bureau, 2019 |
| Community Stress Theory | Stressors, such as issues related to inequality, can weaken the body’s ability to respond to external challenges. | Gee & Payne-Sturges, 2004 3 | |
| Community Well-Being Index3 | Combines the Well-Being Index and the Social Determinants of Health Index into a single score to assess self-reported health-related behaviors and perceptions through five interrelated domains: (1) healthcare access, (2) food access, (3) resource access, (4) housing and transportation, and (5) economic security. | Scale ranges from 0–100; lower score = low community well-being | Sharecare, 2021 |
| Community-based participatory research (CBPR) conceptual model | Partnership approach which involves all stakeholders (e.g., community members, organizational representatives, researchers) in the research and decision-making process with the goal of increasing knowledge and driving political and/or social change. | Ortiz et al., 2020 | |
| Conceptual framework for monitoring equity in health and healthcare | Designed to help guide the development of approaches (using existing data and simple methods) to monitoring equity in health and health care—e.g., formulating key questions, defining the social groups to be compared, and selecting health indicators and measures of disparity that are fundamental to monitoring health equity. | Braveman, 2003 3 | |
| County Health Rankings3 | Measures the health of nearly all counties across the United States by applying county-level measures from national and state data sources to help communities understand the health of their residents. | Lower ranking/higher percentile = healthier county | University of Wisconsin Population Health Institute, 2022 |
| COVID-19 Community Vulnerability Index (CCVI) | Expands upon the Centers for Disease Control and Prevention’s (CDC) Social Vulnerability Index (SVI) to incorporate additional variables that assess individual- and community-level vulnerability within the context of the coronavirus pandemic. | Values range from 0–1; higher value = higher level of vulnerability | Srivastava et al., 2022 3 |
| Dahlgren and Whitehead model | Maps the influence of individual (e.g., lifestyle factors) and environmental factors (e.g., community influences, living and working conditions, etc.) on health. | de Lima Silva et al., 2014; Driscoll et al., 2013 | |
| Danaher Framework | Describes how contributions from the community sector can help reduce health disparities and improve population health. | The National Academies of Sciences, Engineering, and Medicine, 2016 | |
| Dimensions of food security (Food and Agricultural Organization) | Measures the availability of food and an individual’s ability to access it through the following four dimensions: (1) availability, (2) access, (3) utilization, and (4) stability. | Bowers et al., 2020 | |
| Environmental determinants of health | Environmental determinants include the physical, chemical, and biological factors external to a person and their impact on health (e.g., sanitation, exposure to toxins, climate change, pollution, etc.). | Salgado et al., 2020 | |
| Equiframe | Analyzes the inclusion of vulnerable groups and human rights in health policies through three summary indices: core concept coverage, vulnerable group coverage, and core concept quality. | Overall ranking: High = policy achieved ≥ 50 % on all 3 indices; Moderate = policy achieved ≥ 50 % on 2 indices; Low = policy achieved < 50 % on 2 or 3 indices | van Hees et al., 2019 |
| Equity-Effectiveness Model | The effectiveness of community-level interventions decreases along a set of parameters which measures access to, and quality of, care. | Nooh et al., 2019 | |
| Expansive gender equity continuum | Expands upon previous gender equity models that define equity on a continuum from gender unequal to gender transformative, by including a broader definition of gender identity ranging from exclusive (i.e., only considers cisgender identities) to gender inclusive (i.e., considers people of all gender identities, including trans people and nonbinary individuals). | Restar et al., 2021 | |
| Framework for understanding racial/ethnic disparities in environmental health | Health disparities are partially caused by differential access to resources and exposures to hazards and can be grouped into four categories: (1) social processes, (2) environmental contaminants/exposures, (3) body burdens of environmental contaminants, and (4) health outcomes. | Payne-Sturges & Gee, 2006 3 | |
| Fundamental Cause Model | Examines the relationship between socioeconomic inequalities and health; the ability to control disease/death is influenced by access to fundamental resources (e.g., knowledge, money, power, prestige, and beneficial social connections). | Tulier et al., 2019; Diez Roux, 20123 | |
| Gini Coefficient | Statistical measure for assessing income inequality across a population. | 0 = Perfect equality 1 = Perfect inequality | Berkman et al., 2014 |
| Health-Behavior Model | Social psychological model used to understand and predict health-related behaviors among individuals and communities, particularly in the uptake of health services. | Dressler et al., 2005 3 | |
| Health equity audits | Measures and addresses inequalities in the delivery of and access to health services, associated health outcomes, and determinants of health between different population groups. | van Daalen et al., 2021 | |
| Health equity framework | Outlines how health outcomes are influenced by complex interactions between people and their environments and centers around three foundational concepts: (1) equity at the core of health outcomes; (2) multiple, interacting spheres of influence; and a (3) historical and life-course perspective. | Peterson et al., 2021 | |
| Health equity measurement framework | Comprehensive model that describes the social determinants of health in a causal context and can be used to measure and monitor health equity; includes an expansive list of social determinants of health, such as the socioeconomic, cultural, and political context, health policy context, social stratification, social location, material and social circumstances, environment, quality of care, etc. | Dover & Belon, 2019 | |
| Health in All Policies | Health in All Policies (HiAP) is a collaborative approach that integrates and articulates health considerations into policymaking across sectors to improve the health of all communities and people. HiAP recognizes that health is created by a multitude of factors beyond healthcare and, in many cases, beyond the scope of traditional public health activities. | Lorenc et al., 2014 | |
| Healthy People (2020 and 2030) | Provides science-based, national objectives each decade dedicated to improving the health of all Americans. Healthy People 2020 developed a framework that organized the social determinants of health into five key domains: (1) Economic Stability, (2) Education, (3) Health and Health Care, (4) Neighborhood and Built Environment, and (5) Social and Community Context. Healthy People 2030 established a framework to describe the initiative’s rationale and approach, including its vision, mission, foundational principles, plan of action, and overarching goals (new objectives are underway). | Wilder et al., 2021; Chen et al., 2020; Mohan & Chattopadhyay, 2020; Sokol et al., 2019; Min et al., 2022; Yelton et al., 2022; Maness & Buhi, 2016; Abbott & Williams, 2015 | |
| Healthy Places Index (HPI) | Tool used to explore the social conditions that affect health and includes indicators such as food access, job opportunities, clean air and water, single parent households, education, and others. | Value ranges from 0–100; lower score = more healthy conditions | Srivastava et al., 2022 3 |
| Human Development Index (HDI) | Standardized measure used to assess the extent of human development in a country through three key dimensions: (1) life expectancy, (2) education, and (3) per capita income. | Values range from 0–1; Higher score = higher lifespan, higher education level, and higher per capita income | Freire et al., 2018 |
| Index of Dissimilarity | Measures the evenness of groups over space and can be interpreted as the percentage of a particular group who would have to move in order to integrate the two groups over the region as a whole. | Value ranges from 0–1; 0 = fully integrated environment 1 = full segregation | Payne-Sturges & Gee, 20063; Gee & Payne-Sturges, 20043 |
| Integrated Life Course and Social Determinants Model of Aboriginal Health | Conceptual framework for understanding the social determinants of health that impact Aboriginal and Torres Strait Islander people as organized into three categories: (1) proximal (e.g., income, education, housing, individual health), (2) intermediate (e.g., resources, opportunities, and infrastructure), and (3) distal (e.g., colonialism, racial discrimination, natural environment, healthcare systems). | Kolahdooz et al., 2015 | |
| Interaction Model | Emphasizes the interaction between genes and their environment, such that individuals with different genotypes experience differential effects of environmental exposures and disease risk. | Diez Roux, 2012 3 | |
| International Classification of Functioning, Disability and Health (ICF) model | In-depth classification of holistic components of functioning, disability, and health-related domains. | Malele-Kolisa et al., 2019 | |
| Life Course Approach (World Health Organization) | Applies a temporal and social perspective to analyze people’s lives within social, economic, and cultural contexts across different generations to understand current patterns of health and disease. | Taggart et al., 2020 | |
| Minority Health Social Vulnerability Index (MHSVI)3 | Expands upon the Social Vulnerability Index to include additional factors that impact COVID-19 outcomes, as organized into the following six themes: (1) Socioeconomic Status, (2) Household Composition and Disability, (3) Minority Status and Language, (4) Housing Type and Transportation, (5) Health Care Infrastructure and Access, and (6) Medical Vulnerability. | Values range from 0–1; higher value = more vulnerable | CDC & HHS OMH, 2021 |
| Multi-Level Systems Approach | Focuses on individuals within broader contexts, such as within neighborhoods or communities, who may share similar characteristics and therefore may experience similar health outcomes. | Payne-Sturges et al., 2006b 3 | |
| Pathways Model | This model aims to reduce health and social disparities in communities by connecting high-risk individuals to care and tracking the associated outcomes. | Diez Roux, 2012 3 | |
| Policy-oriented approach3 | Analysis of patterns and trends of social inequalities in health over time and their determinants, with a specific focus on inequalities that are commonly viewed as unjust and avoidable. | Braveman, 1998 | |
| PROGRESS/PROGRESS Plus2 | Acronym used to identify dimensions across which health inequities may occur, specifically, place of residence; race/ethnicity /culture/language; occupation; gender/sex; religion; education; socioeconomic status; and social capital. | Turnbull et al., 2020; Chhibber et al., 2021; Schröders et al., 2015; Lehne & Bolte, 2017; Schüz et al., 2021; Campos-Matos et al., 2016; Aves et al., 2017; Welch et al., 2022; Morton et al., 2016; Buttazzoni et al., 2020; Brown et al., 2017b; Ahmed et al., 2022; Cohn & Harrison, 2022 | |
| Protocol for Responding to and Assessing Patients’ Assets, Risks, and Experiences (PRAPARE) | Risk assessment tool to help healthcare providers collect data on patients’ social determinants of health to improve health, reduce costs, and ensure needs are met. | Chen et al., 2020 | |
| Psychosocial stress model | Health disparities arise from the stresses associated with institutional and interpersonal racism. | Dressler et al., 2005 3 | |
| Public Health 3.0 Model | A model which suggests that building healthy communities requires cross-sector collaboration with various stakeholders in order to advance health and achieve health equity. | Mohan & Chattopadhyay, 2020 | |
| Rural Community Health & Well-Being Framework | Identifies key drivers (i.e., social, economic, and environmental factors) that influence health in rural communities and includes additional categories of important factors highlighted by rural residents. | The National Academies of Sciences, Engineering, and Medicine, 2016 | |
| Smart City 2.0 Paradigm | Any initiative, policy, promotion, program, or strategy developed to serve the needs of citizens. | Buttazzoni et al., 2020 | |
| Social and cultural determinants of mental disorders | Conceptual framework to understand how social determinants interact with key genetic determinants to influence mental disorders. | Lund et al., 2018 | |
| Social and demographic determinants of health-related quality of life (QoL) | An individual’s overall sense of wellbeing including aspects of happiness, satisfaction of life, and physical, mental, psychological, and social perceptions. | Ghiasvand et al., 2020 | |
| Social determinants of child health (SDCH) | Examines how social determinants impact child health across time and generations through distal social factors such as poverty, material deprivation, and social inequalities. | Rajmil et al., 2020 | |
| Social Vulnerability Index (SVI) | Uses U.S. Census data to assess the extent to which communities are socially vulnerable to disasters by ranking each census tract on 15 social factors, including poverty, lack of vehicle access, and crowded housing, and grouping them into four related themes. | Values range from 0–1; higher value = higher level of vulnerability | CDC ATSDR, 2011; Srivastava et al., 20223 |
| Social, Political, Economic and Cultural (SPEC) conceptual model (WHO) | Explains social exclusions as a process rather than a state operating along different dimensions and individual, regional, and global levels. | van Hees et al., 2019 | |
| Social-Ecological Model2 | Theory-based framework for understanding how social and structural determinants influence health and wellbeing. | Habbab & Bhutta, 2020; Yiga et al., 2020; Pereira et al., 2019; Reno & Hyder, 2018; Greenbaum et al., 2018; Christidis et al., 2021; Allen et al., 2020; Karger et al., 2022; Taylor & Lamaro Haintz, 2018 | |
| Socioeconomic Status Model | Emphasizes that race/ethnicity and socioeconomic status (SES) are related, such that certain race/ethnicity groups are disproportionately represented in lower SES groups. | Dressler et al., 2005 3 | |
| Stress-Exposure Disease Framework | Conceptual framework that outlines the relationships between race, environmental conditions, and health. | Gee & Payne-Sturges, 20043; Payne-Sturges et al., 2006a3 | |
| Structural-Constructivist Model | Integrates a dual perspective focused on (1) socially constructed cognitive representations within a society and (2) external factors that restrict individuals, specifically social relationships, and expectations of others (e.g., race, as a concept, is socially or culturally constructed). | Dressler et al., 2005 3 | |
| Systems perspective | Describes communities as a set of institutions which represent various sectors, each with their own policies and decision-making processes which influence behavior and investments in the community. | Wilkerson, 2021 3 | |
| The Frieden Framework | Five-tier pyramid for improving public health; the base of the pyramid includes (1) interventions that impact social determinants of health (e.g., poverty, education), followed by (2) interventions that benefit the general population (e.g., fluoridated water), (3) interventions that help large segments of the population (e.g., immunizations), (4) clinical interventions for the prevention of certain conditions (e.g., cardiovascular disease), and (5) health education interventions (i.e., most labor-intensive and potentially lowest impact). | The National Academies of Sciences, Engineering, and Medicine, 2016 | |
| Three Levels of Racism Framework | Theoretical framework for understanding racial health inequities and developing effective interventions to reduce inequities on three distinct levels: (1) institutionalized, (2) personally mediated, and (3) internalized. | Chandler et al., 2022 | |
| Warnecke’s Model for Analysis of Population Health and Disparities | Defines factors impacting health disparities as proximal, intermediate, or distal and focuses on individual-level outcomes as they relate to specific determinants (i.e., social conditions and policies, institutional context, social context, and physical context). | Zahnd & McLafferty, 2017 | |
| Weathering Hypothesis | Proposes that cumulative exposure to social, economic, and political disadvantage leads to rapid decline in physical health. | Forde et al., 2019 | |
| WHO Conceptual SDOH Framework2 | Outlines how social, economic, and political factors (e.g., income, education, occupation, gender, race, and ethnicity) impact an individual’s socioeconomic position, which, in turn, influences their vulnerability and exposure to health conditions. | Chen et al., 2020; Bhojani et al., 2019; Dover & Belon, 2019; Wang et al., 2020; Allen et al., 2020; Armstead et al., 20213; Batista et al., 2018; Owusu-Addo et al., 2018; The National Academies of Sciences, Engineering, and Medicine, 2016; Brown et al., 2017a; Min et al., 2022 |
Citations were sourced from a PubMed/CINAHL literature search of meta-analysis and systematic review articles using the search terms ‘‘Health Equity”[Mesh] OR ‘‘Social Determinants of Health”[Mesh] and CDC Injury Center staff previous knowledge of the literature.
Indicates a health equity guiding framework that was applied to an injury topic in this study.
Indicates a framework, index, or article sourced from previous knowledge of the health equity literature.
Three of the identified resources reported on one or more injury topics including suicide/depression (Brown et al., 2017b), violence indicators (Armstead et al., 2021), and injury related to infant mortality (e.g., safe sleep, intimate partner violence, child abuse, and drug use during pregnancy) (Reno & Hyder, 2018) (Table 1, Table 2), and used the PROGRESS-Plus framework, the WHO SDOH Conceptual Framework, and a social ecological framework, respectively. The SDOHs analyzed in the group of three injury resources included residence, crowding, physical infrastructure, ethnicity, occupation, gender, religion, education, socioeconomic position, income, social capital, household structure, marital status, social support, and age (Brown et al., 2017b); determinants relevant to the socioeconomic and political context, socioeconomic community condition, and socioeconomic position (Armstead et al., 2021); and individual, interpersonal, organizational, community, and public policy determinants (Reno & Hyder, 2018) (data not shown). These injury articles addressed Caribbean residents (Brown et al., 2017b), African American infants (Reno & Hyder, 2018), and unspecified populations (Armstead et al., 2021) (Table 2).
4. Discussion
4.1. Summary of findings
The resources examined in our research studied a wide variety of populations experiencing diverse health disparities through the application of an array of different health equity guiding frameworks and indices. Only three resources identified in our search applied health equity frameworks or indices to injury topics (Brown et al., 2017b; Armstead et al., 2021; Reno & Hyder, 2018). Our findings suggest that there remain areas of opportunity within the health equity space for injury-specific research. This includes identifying additional health equity guiding frameworks and indices suitable for specific injury topic areas from other meta-analysis, systematic reviews, and individual studies and assessing the utility and quality of well-referenced health equity guiding frameworks and indices—or their adaptations—for injury research.
4.2. Health equity guiding frameworks applied to injury
The three resources that mention the application of a specific health equity guiding framework or index to an injury topic area covered the injury topics of suicide/depression (Brown et al., 2017b), violence indicators (Armstead et al., 2021), and injury related to infant mortality (safe sleep, intimate partner violence, child abuse, and drug use during pregnancy) (Reno & Hyder, 2018), and used the PROGRESS-Plus framework, the WHO SDOH Conceptual Framework, and a variation of the Social-Ecological Model, respectively.
Depression is a risk factor for suicide (CDC NCIPC, 2021a). Brown et al conducted a systematic review that used the PROGRESS-Plus framework to examine the role of SDOHs on depression among individuals in the Caribbean (2017b). ‘‘PROGRESS” is an acronym that refers to a core set of SDOHs: place of residence, race or ethnicity, occupation, gender, religion, education, socio-economic position, and social capital. “Plus” in PROGRESS-Plus refers to other SDOHs identified based on evidence from previous literature and can include personal characteristics associated with discrimination (e.g., disability), features of relationships (e.g., bullied at school), and time-dependent relationships (e.g., hospital stays) (Cochrane, 2022). The Brown et al study identified age as an additional SDOH to analyze (2017b). Using the PROGRESS-Plus framework as a guide, Brown et al found the SDOHs that contributed most to inequalities in suicidal ideation, self-directed harm or suicide attempt, and suicide were gender, age, residence, marital status, and education (2017b).
The WHO SDOH Conceptual Framework illustrates how the structural and social determinants of health inequities (e.g., policies and social class) and intermediary determinants of SDOHs (e.g., behaviors and biological factors) work together to impact equity in health and well-being (Solar & Irwin, 2010). One review used the WHO SDOH Conceptual Framework to identify violence risk factors found in varying contexts (Armstead et al., 2021). Indicators from articles were categorized in four categories: socioeconomic and political context, socioeconomic community conditions, social and physical environments, and bridging community dynamics. The most common indicators within each of these categories were measures of income inequality (a structural determinant of health and risk factor for violence), socioeconomic disadvantage or deprivation, social disorganization, and social capital/collective efficacy, respectively.
A systematic review from 2018 used a social-ecological framework to categorize risk factors for infant mortality (specifically, mortality of African American and multiracial infants) at multiple levels (Reno & Hyder, 2018). While this study does not solely focus on injury topics, it mentions safe sleep, intimate partner violence, child abuse, and drug use while pregnant. The social-ecological framework used in this study consists of five different levels (individual, interpersonal, organizational, community, and public policy) and acknowledges the interplay that occurs between these levels. Safe sleep, drug use during pregnancy, and child abuse were all categorized as SDOHs found within the individual level, while intimate partner violence was categorized at the interpersonal level but associated with factors at the individual level (e.g., maternal drug use).
The use of health equity guiding frameworks in these studies helped to identify research gaps in health equity injury research. Namely, the studies identified the need for further examination of sociodemographic inequalities and the need to explore relationships and interactions between SDOHs as important to achieving progress towards health equity in injury, since these factors can influence an injury outcome. It is important to note that structural forces and societal constructs must also be considered in research addressing health disparities and SDOHs, since these are responsible for the inequitable distribution of SDOHs that cause health disparities and create more or less disadvantaged groups of individuals. CDC uses a four-level social ecological model to understand the interplay of risk and protective factors, inclusive of SDOHs, for various forms of injury and to guide prevention strategies, and includes levels at the individual, relationship, community, and societal levels (CDC NCIPC, 2021b). The paucity of health equity meta-analysis and systematic reviews using guiding frameworks or indices that address injury topic areas was observed in our study, suggesting areas of opportunity for injury researchers.
4.3. Limitations
This study is subject to several known limitations. For this formative study, PubMed and CINAHL were used to identify systematic review and meta-analysis articles that mention social determinants of health and health equity. Exploring other databases and broadening the article type would have produced additional results. Books were difficult to access and may also have captured more health equity guiding frameworks or indices not included in this study. Some studies may have selected certain SDOHs to focus on, but did not apply a specific name to the set of SDOHs being researched. These articles were categorized as not mentioning a health equity guiding framework or index. Lastly, the health equity guiding frameworks and indices reported here were not assessed for quality.
5. Conclusion
The findings from this study revealed that the application of health equity guiding frameworks and indices in research have been used to measure and characterize health equity within populations. Though many health equity guiding frameworks and indices were documented for measuring health equity, few were applied in meta-analyses or systematic reviews to an injury topic. However, there are large numbers of individual studies that apply health equity guiding frameworks and indices to injury topics. Some guiding frameworks/indices may be more appropriate than others for measuring health equity in injury topic areas, depending on which SDOH they address. Measuring health equity is important for understanding progress towards reducing health disparities within populations and is helpful for identifying where and for whom additional or improved programs and interventions may be necessary.
5.1. Practical Applications
Measuring health equity in injury and other public health research areas can help build a foundation of evidence. Moving forward, injury researchers can consider the health equity guiding frameworks and indices identified through this study in their health equity injury research.
Acknowledgements
We would like to acknowledge Amy Wolkin, Heather Clayton, and Martevia Bledsoe for contributing articles and health equity guiding frameworks and indices for this review.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Biographies
Natalie Lennon, MPH graduated from Emory University in 2021 with her MPH in Behavioral Sciences and Health Education. She is currently an ORISE fellow for the Division of Injury Prevention in the CDC’s Injury Center, where she works on research related to nonfatal injury, health equity, and suicide prevention. Before joining CDC, Natalie completed her practicum at the Georgia Health Policy Center in the Center of Excellence for Children’s Behavioral Health. Her research interests include preventing suicide and other forms of injury among disproportionally affected populations.
Andrea Carmichael, MPH graduated from George Mason University in 2018 with her MPH in Epidemiology and completed her practicum at the EPA’s Office of Children’s Health protection. She is currently an Associate Service Fellow for the Division of Injury Prevention in the CDC’s Injury Center, where she has presented and published on various injury topics including suicide prevention, drug overdose, and nonfatal injury data. She volunteered for two COVID-19 response deployments, which involved monitoring and reporting cases among the general population and among people experiencing homelessness. Her current research interests focus on incorporating health equity into injury research.
Judy Qualters, PhD, MPH is the director of the Division of Injury Prevention (DIP) in the National Center for Injury Prevention and Control (NCIPC) at CDC. In this role, Dr. Qualters provides leadership to bridge science and practice in an effort to move the field of violence and injury prevention forward. She also leads a diverse port-folio of work that includes surveillance, data and economic analysis, information technology, policy research, evaluation, and technical assistance to state health departments.
Footnotes
The Journal of Safety Research has partnered with the Office of the Associate Director for Science, Division of Injury Prevention, National Center for Injury Prevention and Control at the CDC in Atlanta, Georgia, USA, to briefly report on some of the latest findings in the research community. This report is the 71st in a series of “Special Report from the CDC” articles on injury prevention.
Declaration of Interest
None.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention. All materials in this report are in the public domain and may be used and copied without permission but require citation.
References
- Abbott LS, & Williams CL (2015). Influences of social determinants of health on African Americans living with HIV in the rural southeast: A qualitative meta-synthesis. Journal of the Association of Nurses in AIDS Care, 26(4), 340–356. 10.1016/j.jana.2015.03.004. [DOI] [PubMed] [Google Scholar]
- Agency for Healthcare Research and Quality (2021). Social Determinants of Health Database (Beta Version) [Available from: https://www.ahrq.gov/sdoh/dataanalytics/sdoh-data.html].
- Ahmed S, Chase LE, Wagnild J, Akhter N, Sturridge S, Clarke A, Chowdhary P, Mukami D, Kasim A, & Hampshire K (2022). Community health workers and health equity in low- and middle-income countries: Systematic review and recommendations for policy and practice. International Journal for Equity in Health, 21(1), 49. 10.1186/s12939-021-01615-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen LN, Smith RW, Simmons-Jones F, Roberts N, Honney R, & Currie J (2020). Addressing social determinants of noncommunicable diseases in primary care: A systematic review. Bulletin of the World Health Organization, 98(11), 754–765B. 10.2471/BLT.19.248278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armstead TL, Wilkins N, & Nation M (2021). Structural and social determinants of inequities in violence risk: A review of indicators. Journal of Community Psychology, 49(4), 878–906. 10.1002/jcop.22232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aves T, Kredo T, Welch V, Mursleen S, Ross S, Zani B, Motaze NV, Quinlan L, & Mbuagbaw L (2017). Equity issues were not fully addressed in Cochrane human immunodeficiency virus systematic reviews. Journal of Clinical Epidemiology, 81, 96–100. 10.1016/j.jclinepi.2016.09.008. [DOI] [PubMed] [Google Scholar]
- Batista R, Pottie K, Bouchard L, Ng E, Tanuseputro P, & Tugwell P (2018). Primary health care models addressing health equity for immigrants: A systematic scoping review. Journal of Immigrant and Minority Health, 20(1), 214–230. 10.1007/s10903-016-0531-y. [DOI] [PubMed] [Google Scholar]
- Berkman L, Kawachi I, & Glymour MM (2014). Social epidemiology Oxford: Oxford University Press. [Google Scholar]
- Bhojani U, Madegowda C, Prashanth NS, Hebbar P, Mirzoev T, Karlsen S, & Mir G (2019). Affirmative action, minorities, and public services in India: Charting a future research and practice agenda. Indian Journal of Medical Ethics, 4(4), 265–273. 10.20529/ijme.2019.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowers R, Turner G, Graham ID, Furgal C, & Dubois L (2020). Piecing together the Labrador Inuit food security policy puzzle in Nunatsiavut, Labrador (Canada): A scoping review. International Journal of Circumpolar Health, 79(1), 1799676. 10.1080/22423982.2020.1799676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braveman P (1998). Monitoring equity in health: A policy-oriented approach in low- and middle-income countries Geneva: Department of Health Systems, World Health Organization. [Available from: https://apps.who.int/iris/handle/10665/65228]. [Google Scholar]
- Braveman P (2003). Monitoring equity in health and healthcare: A conceptual framework Available from. Journal of Health and Population Nutrition, 21(3), 181–192 https://www.jstor.org/stable/23499216?seq=1. [PubMed] [Google Scholar]
- Brown CR, Hambleton IR, Hercules SM, Alvarado M, Unwin N, Murphy MM, Harris EN, Wilks R, MacLeish M, Sullivan L, & Sobers-Grannum N (2017a). Social determinants of breast cancer in the Caribbean: A systematic review. International Journal of Equity in Health, 16(1), 60. 10.1186/s12939-017-0540-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown CR, Hambleton IR, Sobers-Grannum N, Hercules SM, Unwin N, Nigel Harris E, Wilks R, MacLeish M, Sullivan L, Murphy MM, & Caribbean US Alliance for Health Disparities Research Group (USCAHDR) (2017b). Social determinants of depression and suicidal behaviour in the Caribbean: A systematic review. BMC Public Health, 17(1), 577. 10.1186/s12889-017-4371-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buttazzoni A, Veenhof M, & Minaker L (2020). Smart city and high-tech urban interventions targeting human health: An equity-focused systematic review. International Journal of Environmental Research in Public Health, 17(7). 10.3390/ijerph17072325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos-Matos I, Russo G, & Perelman J (2016). Connecting the dots on health inequalities–a systematic review on the social determinants of health in Portugal. International Journal of Equity in Health, 15, 26. 10.1186/s12939-016-0314-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention, Agency for Toxic Substances and Disease Registry (2011). Social Vulnerability Index [Available from: https://www.atsdr.cdc.gov/placeandhealth/svi/index.html].
- Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion (2020). Health Equity 2020 [Available from: https://www.cdc.gov/chronicdisease/healthequity/index.htm].
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control (2020). Web-based Injury Statistics Query and Reporting System (WISQARS) [online] [Available from: http://www.cdc.gov/injury/wisqars].
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control (2021). Risk and Protective Factors [Available from: https://www.cdc.gov/suicide/factors/index.html].
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control (2021). The Social-Ecological Model: A Framework for Prevention [Available from: https://www.cdc.gov/violenceprevention/about/social-ecologicalmodel.html].
- Centers for Disease Control and Prevention, Office of Minority Health and Health Equity (2022). CDC Core Health Equity Science and Intervention Strategy [Available from: https://www.cdc.gov/healthequity/core/index.html].
- Centers for Disease Control and Prevention & United States Department of Health and Human Services Office of Minority Health (2021). Minority Health Social Vulnerability Index [Available from: https://www.minorityhealth.hhs.gov/minority-health-svi/].
- Chandanabhumma PP, & Narasimhan S (2020). Towards health equity and social justice: An applied framework of decolonization in health promotion. Health Promotion International, 35(4), 831–840. 10.1093/heapro/daz053. [DOI] [PubMed] [Google Scholar]
- Chandler CE, Williams CR, Turner MW, & Shanahan ME (2022). Training public health students in racial justice and health equity: A systematic review. Public Health Report, 137, 375–385. 10.1177/00333549211015665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen M, Tan X, & Padman R (2020). Social determinants of health in electronic health records and their impact on analysis and risk prediction: A systematic review. Journal of the American Medical Informatics Association, 27(11), 1764–1773. 10.1093/jamia/ocaa143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chhibber A, Kharat A, Kneale D, Welch V, Bangpan M, & Chaiyakunapruk N (2021). Assessment of health equity consideration in masking/PPE policies to contain COVID-19 using PROGRESS-plus framework: A systematic review. BMC Public Health, 21(1), 1682. 10.1186/s12889-021-11688-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christidis R, Lock M, Walker T, Egan M, & Browne J (2021). Concerns and priorities of Aboriginal and Torres Strait Islander peoples regarding food and nutrition: A systematic review of qualitative evidence. International Journal of Equity in Health, 20(1), 220. 10.1186/s12939-021-01551-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clemen T., Morelan B., & Le R. (2021). Persistent racial/ethnic disparities in fatal unintentional drowning rates among persons aged 29 Years — United States, 1999–2019. Morbidity and Mortality Weekly Report, 70, 869–874. 10.15585/mmwr.mm7024a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohn T, & Harrison CV (2022). A systematic review exploring racial disparities, social determinants of health, and sexually transmitted infections in Black women. Nursing for Women’s Health, 26, 128–142. 10.1016/j.nwh.2022.01.006. [DOI] [PubMed] [Google Scholar]
- Daugherty J, Zhou H, Sarmiento K, & Waltzman D (2021). Differences in state traumatic brain injury–related deaths, by principal mechanism of injury, intent, and percentage of population living in rural areas — United States, 2016–2018. Morbidity and Mortality Weekly Report, 70, 1447–1452. 10.15585/mmwr.mm7041a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Lima Silva V, Cesse E, & de Albuquerque MF (2014). Social determinants of death among the elderly: A systematic literature review. Revista Brasileira de Epidemiologia, 17(Suppl 2), 178–193. 10.1590/1809-4503201400060015. [DOI] [PubMed] [Google Scholar]
- Department of Health and Human Services (2020). Healthy People 2020 [Available from: https://www.healthypeople.gov/2020].
- Diez Roux AV (2012). Conceptual approaches to the study of health disparities. Annual Review of Public Health, 33, 41–58. 10.1146/annurev-publhealth-031811-124534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dover DC, & Belon AP (2019). Correction to: The health equity measurement framework: A comprehensive model to measure social inequities in health. International Journal of Equity in Health, 18(1), 58. 10.1186/s12939-019-0949-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dressler W, Oths K, & Gravlee C (2005). Race and ethnicity in public health research: Models to explain health disparities. Annual Reviews, 34, 231–252. 10.1146/annurev.anthro.34.081804.120505. [DOI] [Google Scholar]
- Driscoll DL, Dotterrer B, Brown RA, & 2nd. (2013). Assessing the social and physical determinants of circumpolar population health. International Journal of Circumpolar Health, 72. 10.3402/ijch.v72i0.21400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlman DC, Yard E, Stone DM, Jones CM, & Mack KA (2022). Changes in suicide rates — United States, 2019 and 2020. Morbidity and Mortality Weekly Report, 71, 306–312. 10.15585/mmwr.mm7108a5. [DOI] [PubMed] [Google Scholar]
- Fairfield K, Black A, Ziller E, Murray K, Lucas F, Waterston L, Korsen N, Ineza D, & Han P (2020). Area deprivation index and rurality in relation to lung cancer prevalence and mortality in a rural state. JNCI Cancer. Spectrum, 4(4). 10.1093/jncics/pkaa011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forde AT, Crookes DM, Suglia SF, & Demmer RT (2019). The weathering hypothesis as an explanation for racial disparities in health: A systematic review 1–18.e3. Annals of Epidemiology, 33. 10.1016/j.annepidem.2019.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freire RC, Pieruccini-Faria F, & Montero-Odasso M (2018). Are Human Development Index dimensions associated with gait performance in older adults? A systematic review. Experimental Gerontology, 102, 59–68. 10.1016/j.exger.2017.12.001. [DOI] [PubMed] [Google Scholar]
- Gee GC, & Payne-Sturges DC (2004). Environmental health disparities: A framework integrating psychosocial and environmental concepts. Environmental Health Perspectives, 112(17), 1645–1653. 10.1289/ehp.7074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghiasvand H, Higgs P, Noroozi M, Ghaedamini Harouni G, Hemmat M, Ahounbar E, Haroni J, Naghdi S, Nazeri Astaneh A, & Armoon B (2020). Social and demographical determinants of quality of life in people who live with HIV/AIDS infection: Evidence from a meta-analysis. Biodemography and Social Biology, 65(1), 57–72. 10.1080/19485565.2019.1587287. [DOI] [PubMed] [Google Scholar]
- Greenbaum VJ, Titchen K, Walker-Descartes I, Feifer A, Rood CJ, & Fong HF (2018). Multi-level prevention of human trafficking: The role of health care professionals. Prevention Medicine, 114, 164–167. 10.1016/j.ypmed.2018.07.006. [DOI] [PubMed] [Google Scholar]
- Habbab RM, & Bhutta ZA (2020). Prevalence and social determinants of overweight and obesity in adolescents in Saudi Arabia: A systematic review. Clinical Obesity, 10(6), e12400. 10.1111/cob.12400. [DOI] [PubMed] [Google Scholar]
- Hu J, Kind AJH, & Nerenz D (2018). Area deprivation index predicts readmission risk at an urban teaching hospital. American Journal of Medical Quality, 33(5), 493–501. 10.1177/1062860617753063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karger S, Bull C, Enticott J, & Callander EJ (2022). Options for improving low birthweight and prematurity birth outcomes of indigenous and culturally and linguistically diverse infants: A systematic review of the literature using the social-ecological model. BMC Pregnancy and Childbirth, 22(1), 3. 10.1186/s12884-021-04307-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolahdooz F, Nader F, Yi KJ, & Sharma S (2015). Understanding the social determinants of health among Indigenous Canadians: Priorities for health promotion policies and actions. Global Health Action, 8, 27968. 10.3402/gha.v8.27968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Chen JT, Waterman PD, Rehkopf DH, & Subramanian SV (2003). Race/ethnicity, gender, and monitoring socioeconomic gradients in health: A comparison of area-based socioeconomic measures–the public health disparities geocoding project. American Journal of Public Health, 93(10), 1655–1671. 10.2105/ajph.93.10.1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehne G, & Bolte G (2017). Impact of universal interventions on social inequalities in physical activity among older adults: An equity-focused systematic review. International Journal of Behavioral and Nutrition and Physical Activity, 14(1), 20. 10.1186/s12966-017-0472-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorenc T, Tyner EF, Petticrew M, Duffy S, Martineau FP, Phillips G, & Lock K (2014). Cultures of evidence across policy sectors: Systematic review of qualitative evidence. European Journal of Public Health, 24(6), 1041–1047. 10.1093/eurpub/cku038. [DOI] [PubMed] [Google Scholar]
- Lund C, Brooke-Sumner C, Baingana F, Baron EC, Breuer E, Chandra P, Haushofer J, Herrman H, Jordans M, Kieling C, Medina-Mora ME, Morgan E, Omigbodun O, Tol W, Patel V, & Saxena S (2018). Social determinants of mental disorders and the Sustainable Development Goals: A systematic review of reviews. Lancet Psychiatry, 5(4), 357–369. 10.1016/s2215-0366(18)30060-9. [DOI] [PubMed] [Google Scholar]
- Malele-Kolisa Y, Yengopal V, Igumbor J, Nqcobo CB, & Ralephenya TRD (2019). Systematic review of factors influencing oral health-related quality of life in children in Africa. African Journal of Primary Health Care and Family Medicine, 11(1), e1–e12. 10.4102/phcfm.v11i1.1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maness SB, & Buhi ER (2016). Associations between social determinants of health and pregnancy among young people: A systematic review of research published during the past 25 years. Public Health Report, 131(1), 86–99. 10.1177/003335491613100115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Min LY, Islam RB, Gandrakota N, & Shah MK (2022). The social determinants of health associated with cardiometabolic diseases among Asian American subgroups: A systematic review. BMC Health Service Research, 22(1), 257. 10.1186/s12913-022-07646-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohan G, & Chattopadhyay S (2020). Cost-effectiveness of leveraging social determinants of health to improve breast, cervical, and colorectal cancer screening: A systematic review. JAMA Oncolology, 6(9), 1434–1444. 10.1001/jamaoncol.2020.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore M, Conrick K, Fuentes M, Rowhani-Rahbar A, Graves JM, Patil D, Herrenkohl M, Mills B, Rivara FP, Ebel B, & Vavilala MS (2019). Research on injury disparities: A scoping review. Health Equity, 3(1), 504–511. 10.1089/heq.2019.0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton RL, Schlackow I, Mihaylova B, Staplin ND, Gray A, & Cass A (2016). The impact of social disadvantage in moderate-to-severe chronic kidney disease: An equity-focused systematic review. Nephrology Dialysis Transplantation, 31(1), 46–56. 10.1093/ndt/gfu394. [DOI] [PubMed] [Google Scholar]
- Nooh F, Crump L, Hashi A, Tschopp R, Schelling E, Reither K, Hattendorf J, Ali SM, Obrist B, Utzinger J, & Zinsstag J (2019). The impact of pastoralist mobility on tuberculosis control in Ethiopia: A systematic review and meta-synthesis. Infectious Diseases of Poverty, 8(1), 73. 10.1186/s40249-019-0583-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz K, Nash J, Shea L, et al. (2020). Partnerships, Processes, and Outcomes: A Health Equity-Focused Scoping Meta-Review of Community-Engaged Scholarship. Annual Review of Public Health, 41, 177–199. 10.1146/annurev-publhealth-040119-094220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Owusu-Addo E, Renzaho AMN, & Smith BJ (2018). The impact of cash transfers on social determinants of health and health inequalities in sub-Saharan Africa: A systematic review. Health Policy and Planning, 33(5), 675–696. 10.1093/heapol/czy020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payne-Sturges D, & Gee GC (2006). National environmental health measures for minority and low-income populations: Tracking social disparities in environmental health. Environmental Research, 102(2), 154–171. 10.1016/j.envres.2006.05.014. [DOI] [PubMed] [Google Scholar]
- Payne-Sturges D, Gee GC, Crowder K, Hurley BJ, Lee C, Morello-Frosch R, Rosenbaum A, Schulz A, Wells C, Woodruff T, & Zenick H (2006a). Workshop summary: Connecting social and environmental factors to measure and track environmental health disparities. Environmental Research, 102(2), 146–153. 10.1016/j.envres.2005.11.001. [DOI] [PubMed] [Google Scholar]
- Payne-Sturges D, Zenick H, Wells C, & Sanders W (2006b). We cannot do it alone: Building a multi-systems approach for assessing and eliminating environmental health disparities. Environmental Research, 102(2), 141–145. 10.1016/j.envres.2006.01.011. [DOI] [PubMed] [Google Scholar]
- Pereira M, Padez CMP, & Nogueira H (2019). Describing studies on childhood obesity determinants by Socio-Ecological Model level: A scoping review to identify gaps and provide guidance for future research. International Journal of Obesity (London), 43(10), 1883–1890. 10.1038/s41366-019-0411-3. [DOI] [PubMed] [Google Scholar]
- Peterson A, Charles V, Yeung D, & Coyle K (2021). The health equity framework: A science- and justice-based model for public health researchers and practitioners. Health Promotion and Practice, 22(6), 741–746. 10.1177/1524839920950730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajmil L, Hjern A, Spencer N, Taylor-Robinson D, Gunnlaugsson G, & Raat H (2020). Austerity policy and child health in European countries: A systematic literature review. BMC Public Health, 20(1), 564. 10.1186/s12889-020-08732-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reno R, & Hyder A (2018). The evidence base for social determinants of health as risk factors for infant mortality: A systematic scoping review. Journal of Health Care for the Poor and Underserved, 29(4), 1188–1208. 10.1353/hpu.2018.0091. [DOI] [PubMed] [Google Scholar]
- Restar AJ, Sherwood J, Edeza A, Collins C, & Operario D (2021). Expanding gender-based health equity framework for transgender populations. Transgender Health, 6(1), 1–4. 10.1089/trgh.2020.0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robert Wood Johnson Foundation (2017). What is Health Equity? [Available from: https://www.buildhealthyplaces.org/content/uploads/2017/05/rwjf436997.pdf].
- Salgado M, Madureira J, Mendes AS, Torres A, Teixeira JP, & Oliveira MD (2020). Environmental determinants of population health in urban settings. A systematic review. BMC Public Health, 20(1), 853. 10.1186/s12889-020-08905-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schröders J, Wall S, Kusnanto H, & Ng N (2015). Millennium development goal four and child health inequities in Indonesia: A systematic review of the literature. PLoS One, 10(5), e0123629. 10.1371/journal.pone.0123629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schüz B, Meyerhof H, Hilz LK, & Mata J (2021). Equity effects of dietary nudging field experiments: Systematic review. Frontier Public Health, 9, 668998. 10.3389/fpubh.2021.668998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharecare (2021). Community Well-Being Index [Available from: https://wellbeingindex.sharecare.com/].
- Sokol R, Austin A, Chandler C, Byrum E, Bousquette J, Lancaster C, Doss G, Dotson A, Urbaeva V, Singichetti B, Brevard K, Wright ST, Lanier P, & Shanahan M (2019). Screening children for social determinants of health: A systematic review. Pediatrics, 144(4), e20191622. 10.1542/peds.2019-1622. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solar O, & Irwin A (2010). A conceptual framework for action on the social determinants of health Available from:. Geneva: World Health Organization; https://www.who.int/publications-detail-redirect/9789241500852. [Google Scholar]
- Srivastava T, Schmidt H, Sadecki E, & Kornides M (2022). Disadvantage indices deployed to promote equitable allocation of COVID-19 vaccines in the US: A scoping review of differences and similarities in design. JAMA, 3(1), e214501. 10.1001/jamahealthforum.2021.4501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taggart T, Milburn NG, Nyhan K, & Ritchwood TD (2020). Utilizing a life course approach to examine HIV risk for Black adolescent girls and young adult women in the United States: A systematic review of recent literature. Ethnic Disparities, 30(2), 277–286. 10.18865/ed.30.2.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor J, & Lamaro Haintz G (2018). Influence of the social determinants of health on access to healthcare services among refugees in Australia. Australian Journal of Primary Health, 24(1), 14–28. 10.1071/PY16147. [DOI] [PubMed] [Google Scholar]
- The Cochrane Collaboration. (2022). PROGRESS-Plus [Available from: https://methods.cochrane.org/equity/projects/evidence-equity/progress-plus].
- The National Academies of Sciences, Engineering, and Medicine (U.S.). (2016). A framework for educating health professionals to address the social determinants of health [Available from: https://www.ncbi.nlm.nih.gov/books/NBK395983/]. [PubMed]
- Tulier ME, Reid C, Mujahid MS, & Allen AM (2019). ‘‘Clear action requires clear thinking”: A systematic review of gentrification and health research in the United States. Health Place, 59, 102173. 10.1016/j.healthplace.2019.102173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turnbull S, Cabral C, Hay A, & Lucas PJ (2020). Health equity in the effectiveness of web-based health interventions for the self-care of people with chronic health conditions: Systematic review. Journal of Medical Internet Research, 22(6), e17849. 10.2196/17849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Census Bureau (2019). Community Resilience Estimates [Available from: https://www.census.gov/programs-surveys/community-resilience-estimates.html].
- University of Wisconsin Population Health Institute (2022). County Health Rankings Model [Available from: https://www.countyhealthrankings.org/explore-health-rankings/measures-data-sources/county-health-rankings-model].
- van Daalen KR, Davey F, Norman C, & Ford JA (2021). Health equity audits: A systematic review of the effectiveness. BMJ Open, 11(11), e053392. 10.1136/bmjopen-2021-053392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Hees SGM, O’Fallon T, Hofker M, Dekker M, Polack S, Banks LM, & Spaan E (2019). Leaving no one behind? Social inclusion of health insurance in low- and middle-income countries: A systematic review. International Journal of Equity in Health, 18(1), 134. 10.1186/s12939-019-1040-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang E, Glazer KB, Howell EA, & Janevic TM (2020). Social determinants of pregnancy-related mortality and morbidity in the United States: A systematic review. Obstetrics & Gynecology, 135(4), 896–915. 10.1097/aog.0000000000003762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Welch V, Dewidar O, Tanjong Ghogomu E, Abdisalam S, Al Ameer A, Barbeau VI, Brand K, Kebedom K, Benkhalti M, Kristjansson E, Madani MT, Antequera Martín AM, Mathew CM, McGowan J, McLeod W, Park HA, Petkovic J, Riddle A, Tugwell P, Petticrew M, Trawin J, & Wells GA (2022). How effects on health equity are assessed in systematic reviews of interventions. The Cochrane Database of Systematic Reviews, 1(1), MR000028. 10.1002/14651858.MR000028.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkerson R (2021). Socially connected communities: Solutions for social isolation. In: Moore S, ed.: Healthy Places by Design [Available from: Socially-Connected-Communities_Solutions-for-Social-Isolation.pdf].
- Yelton B, Friedman DB, Noblet S, Lohman MC, Arent MA, Macauda MM, Sakhuja M, & Leith KH (2022). Social determinants of health and depression among African American adults: A scoping review of current research. International Journal of Environmental Researchin Public Health, 19(3). 10.3390/ijerph19031498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yiga P, Seghers J, Ogwok P, & Matthys C (2020). Determinants of dietary and physical activity behaviours among women of reproductive age in urban sub-Saharan Africa: A systematic review. British Journal of Nutrition, 124(8), 761–772. 10.1017/s0007114520001828. [DOI] [PubMed] [Google Scholar]
- Zahnd WE, & McLafferty SL (2017). Contextual effects and cancer outcomes in the United States: A systematic review of characteristics in multilevel analyses 739–48.e3. Annals of Epidemiology, 27(11). 10.1016/j.annepidem.2017.10.002. [DOI] [PubMed] [Google Scholar]


