Highlights
-
•
Hepatitis B virus infection prevalence was lower than previously reported.
-
•
The risk of vertical transmission was low.
-
•
The rate of exposure of the population remains however high.
-
•
More actions are needed to inform and educate populations.
-
•
Optimal prevention of this infection in this region is possible.
Keywords: Hepatitis B virus, Pregnant women, Mother-to-child transmission, Gabon, Africa
Abstract
Objectives
Hepatitis B virus (HBV) infection remains a public health threat in middle- and low-income countries, where mother-to-child transmission plays an important role. The aim of this study was to assess the burden of this infection among pregnant women in southern Gabon and the risk of vertical transmission.
Methods
The study was a prospective investigation conducted from April 2021 to January 2022. Study participants were pregnant women aged 18 and over attending antenatal clinics in Franceville. Blood samples were collected to test for HBV surface antigen, anti-hepatitis B core, hepatitis B e antigen, and anti-hepatitis B e markers and to assess HBV infection.
Results
We recruited 901 women with a median age of 26 years (interquartile range: 21-32). Overall prevalence of infection was 3.9% (confidence interval: 2.7-5.4%). 418/901 or 46.4% were anti-hepatitis B core positive. Among HBV surface antigen-positive women, 1/35 were hepatitis B e antigen-positive with a viral load >200,000 IU/ml. Over 64% of participants had no information about HBV infection, and none knew that the virus could be transmitted from mother to child.
Conclusions
This study reveals a low HBV prevalence in pregnant women in Gabon and a low risk of vertical transmission of the virus. However, the rate of exposure of the population to the virus remains high and calls for improving actions and interventions for potential elimination goals.
Introduction
Hepatitis B virus (HBV) infection remains a major public health concern, with a global high morbidity and mortality consequences [1,2]. According to the World Health Organization (WHO), approximately 296 million people worldwide are living with chronic hepatitis B infection [3]. Because HBV infection is a chronic infection with no cure options, prevention remains a major strategy for a potential future elimination of this infection [4,5]. Moreover, the high rate of new infections worldwide, estimated at 1.5 million in 2020 [6], emphasizes the need to improve current prevention and care strategies, especially in middle-and-low-income countries, where the burden of this infection is high. According to the systematic analysis of the Global Burden Disease 2019, the prevalence of HBV surface antigen (HBsAg) carriage in the world population is estimated at 4.1% [7]. Depending on the effectiveness of vaccination programs and other preventive measures taken by many countries, we observe a disparity in the geographic distribution of HBV infection. In fact, European and American regions where the HBV vaccination coverage is high [8] have HBsAg prevalence of less than 1.5%. However, despite the introduction of vaccination since 1990, the Western Pacific and African Regions remain the most affected areas with HBsAg prevalence ranging between 8.3% and 7.8% respectively [7]. Moreover, in most of the highly affected regions in the middle-and-low-income countries, vertical transmission of the virus, via the infected mother to her child, has been found and reported as the current most important transmission route [9], [10], [11]. In addition, children with HBV infection have up to 90% risk of developing a chronic infection and are at higher risk of later liver complications [4,12,13]. Therefore, improving the prevention of mother-to-child transmission (MTCT) of the virus is a major priority and one of the key components of WHO elimination goal.
Over the past three decades, Gabon has moved from a highly endemic area to an intermediate endemic area for HBV infection with an estimated prevalence of 7.4% in the general population [14]. However, there are very limited data on the current burden of this infection in the Gabonese population and more specifically in pregnant women, who may transmit the virus to their newborn.
The aim of this study was to estimate the prevalence of HBV infection in pregnant women living in the southern Gabon, as well as assess the risk of vertical transmission and the level of knowledge on HBV infection.
Materials and methods
Study design
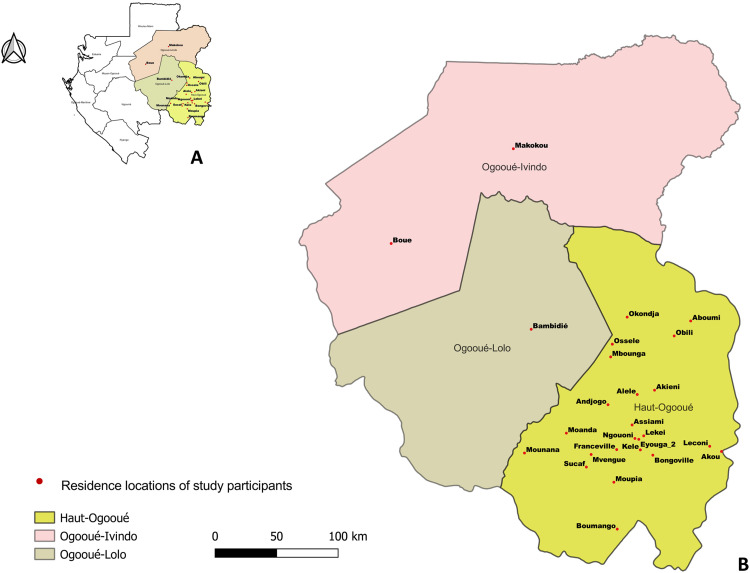
We conducted a cross-sectional study in the Haut-Ogooué region of Gabon, across three major maternity facilities located in Franceville, the capital city of this region. Most of the participants in our study resided in Franceville, but some of them were from other neighboring towns located in this region, as Aboumi, Akieni, Akou, Alele, Andjogo, Assiami, Bambidié, Bongoville, Boue, Boumango, Eyouga_2, Franceville, Kele, Leconi, Lekei, Makokou, Mbounga, Moanda, Mounana, Moupia, Mvengue, Ngouoni, Obili, Okondja, Ossele and Sucaf (Figure 1). These participants were recruited from April 2021 to January 2022 at the Hôpital Régional Amissa Bongo (CHRAB), the Hôpital de l'Amitié Sino-Gabonaise (HASG) and the Service de Santé Maternelle et Infantile (SMI). Throughout the study period, pregnant women attending any of these maternity facilities for a routine medical visit were offered the possibility to be part of the study. Inclusion criteria were as follows: being a pregnant woman, aged 18 years or older, consent to be part of the study, and providing written informed consent. Individuals not meeting these criteria were not recruited. A study questionnaire was administered to collect socio-demographic information including age, place of residence, marital status, occupation, education level, and number of children. A set of questions was also designed to assess participants’ knowledge of HBV infection, HBV vaccination status, and previous HBV testing.
Figure 1.
Map of the Ogooué region in Gabon and indication of cities where study participants live. Red dots represent each of these cities. A represents the map pf Gabon. B represents the Ogooué region.
Sample collection and laboratory analyses
For each study participant, a 4 ml whole blood sample was collected in an ethylene diamine tetra acetic tube. Blood samples were sent within the day to the Virology Laboratory of the Centre Interdisciplinaire de Recherches Médicales de Franceville (CIRMF), Franceville, Gabon. Samples were processed upon reception to collect the plasma and the buffy-coat in aliquots, and stored at −80°C until testing.
Serological tests
Plasma samples were screened for the presence of HBsAg and antibody to the hepatitis B core antigen (HBcAb) using the Monolisa ™ HBsAg ULTRA and Monolisa™ Anti-HBc PLUS (Bio-Rad, Marnes la Coquette, France) kits, respectively. HBsAg-positive samples were further tested for the presence of hepatitis B e antigen (HBeAg) and antibody to the hepatitis B e antigen (HBeAb), using the Monolisa™ HBe Ag-Ab PLUS Kit. All assays were performed according to the manufacturer's instructions.
HBV DNA levels
We tested the level of HBV DNA in all HBsAg positive samples. HBV DNA quantification was performed using the Xpert HBV Viral Load Assay on the GeneXpert Cepheid instrument following the manufacturer's recommendations (Cepheid, Sunnyvale, California, USA). The limit of quantitation of the assays is 10 IU/ml and samples with HBV values below 3.2 IU/ml are classified as undetectable.
Statistical analysis
We estimated the study sample size assuming a HBsAg prevalence of 7% to 10%, based on a pilot study that we conducted in this regions in 2019 (unpublished data), and previously published data in Gabon [15]. To achieve an expected prevalence at 95% confidence interval and 5% accuracy, we estimated the required sample size at 800. Prevalences were estimated by sample frequencies, and their 95% confidence intervals, as reported in Tables 1, 2 and 3, were exact binomial confidence intervals. All computations were performed with the R software.
Table 1.
Characteristics of the study population and their distribution in the three facilities.
| Characteristics | Overall N = 901 (%) |
SMI n = 227 (%) |
HASG n = 415 (%) |
HRAB n = 259 (%) |
|---|---|---|---|---|
| Median age (interquartile range) | 26 (21-32) | 25 (21-31) | 26 (22-31.5) | 27 (22-33) |
| 18-25 | 431 (47.8) | 125 (55.1) | 191 (46) | 115 (44.4) |
| 26-45 | 470 (52.2) | 102 (44.9) | 224 (54) | 144 (55.6) |
| Marital status | ||||
| Single | 377 (41.8) | 105 (46.3) | 172 (41.4) | 100 (38.6) |
| Not single | 524 (58.2) | 122 (53.7) | 243 (58.6) | 159 (61.4) |
| Educational level | ||||
| No education | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Primary | 122 (13.5) | 19 (8.4) | 72 (17.4) | 31 (12) |
| Secondary | 670 (74.4) | 181 (79.7) | 296 (71.3) | 193 (74.5) |
| University | 109 (12.1) | 27 (11.9) | 47 (11.3) | 35 (13.5) |
| Occupation | ||||
| No occupation | 389 (43.2) | 84 (37) | 196 (47.2) | 109 (42.1) |
| Student | 300 (33.3) | 106 (46.7) | 109 (26.3) | 85 (32.8) |
| In activity | 212 (23.5) | 37 (16.3) | 110 (26.5) | 65 (25.1) |
| Nationality | ||||
| Gabonese | 840 (93.2) | 224 (98.7) | 378 (91.1) | 238 (91.9) |
| Others | 61 (6.8) | 3 (1.3) | 37 (8.9) | 21 (8.1) |
| Parity | ||||
| 0 | 238 (26.4) | 65 (28.6) | 109 (26.3) | 64 (24.7) |
| 1 | 223 (24.8) | 64 (28.2) | 101 (24.3) | 58 (22.4) |
| ≥ 2 | 440 (48.8) | 98 (43.2) | 205 (49.4) | 137 (52.9) |
| HBV vaccination status | ||||
| Declared vaccinated | 24 (4.5) | 5 (3.2) | 9 (3.7) | 10 (7.4) |
| Declared not vaccinated | 511 (95.5) | 151 (96.8) | 234 (96.3) | 126 (92.6) |
| Do not know if vaccinated | 366 (40.6) | 71 (31.3) | 172 (41.4) | 123 (47.5) |
| Previously tested for HBV | ||||
| Do not know | 306 (34) | 43 (18.9) | 120 (28.9) | 143 (55.2) |
| Have been tested | 73 (12.3) | 12 (6.5) | 35 (11.9) | 26 (22.4) |
| Have not been tested | 522 (87.7) | 172 (93.5) | 260 (88.9) | 90 (77.6) |
HASG: Hôpital de l'Amitié Sino-Gabonaise; HBV: hepatitis B virus; HRAB: Hôpital Régional Amissa Bongo; SMI: Service de Santé Maternelle et Infantile.
Table 2.
Knowledges and information status on HBV infection and transmission modes.
| Knowledge Items | Correct answer overall N=901 (%) |
Correct Answers, n (%) |
||
|---|---|---|---|---|
| SMI n=227 (%) |
HASG n=415 (%) |
HRAB n=259 (%) |
||
| Have heard of HBV infection | 324 (36%, 33-39) | 91 (40.1%, 33.7-46.8) | 129 (31%, 26.7-35.8) | 104 (40.2%, 34.1-46.4) |
| Through media | 28 (3.1%, 2.1-4.5) | 6 (2.6%, 1.0 - 5.7) | 15 (3.6%, 2.0-5.9) | 7 (2.7%, 1.1-5.5) |
| Family members | 42 (4.7%, 3.4-6.2) | 17 (7.5%, 4.4-11.7) | 13 (3.1%, 1.7-5.3) | 12 (4.6%, 2.4-8.0) |
| At school | 61 (6.8%, 5.2-8.6) | 19 (8.4%, 5.1-12.8) | 23 (5.5%, 3.5-8.2) | 19 (7.3%, 4.5-11.2) |
| At hospital | 53 (5.9%, 4.4-7.6) | 10 (4.4%, 2.1-8.0) | 27 (6.5%, 4.3-9.3) | 16 (6.2%, 3.6-9.8) |
| Others | 70 (7.8%, 6.1-9.7) | 18 (7.9%, 4.8-12.2) | 29 (7.0%, 4.7-9.9) | 23 (8.9%, 5.7-13.0) |
| Hepatitis B is caused by a virus | 54 (6.0%, 4.5-7.7) | 3 (1.3%, 0.3-3.8) | 26 (6.3%, 4.1-9.0) | 25 (9.7%, 6.3-13.9) |
| HBV can be transmitted | 235 (26.1%, 23.2-29.1) | 55 (24.2%, 18.8-30.3) | 91 (21.9%, 18% - 26.2) | 89 (34.4%, 28.6-40.5) |
| By saliva | 136 (15.1%, 12.8-17.6) | 30 (13.2%, 9.1-18.3) | 62 (14.9%, 11.6-18.7) | 44 (17.0%, 12.6-22.1) |
| By blood | 38 (4.2%, 3.0-5.7) | 3 (1.3%, 0.3-3.8) | 24 (5.8%, 3.7-8.5) | 11 (4.2%, 2.1-7.5) |
| Sexually (if unprotected) | 85 (9.4%, 7.6-11.5) | 15 (6.6%, 3.7-10.7) | 38 (9.2%, 6.6-12.4) | 32 (12.4%, 8.6-17.0) |
| By sweats | 4 (0.4%, 0.1-1.1) | 0 (0%, 0.0-1.6) | 1 (0.2%, 0.0-1.3) | 3 (1.2%, 0.2-3.3) |
HASG: Hôpital de l'Amitié Sino-Gabonaise; HBV: hepatitis B virus; HRAB: Hôpital Régional Amissa Bongo; SMI: Service de Santé Maternelle et Infantile.
Table 3.
Hepatitis B serological markers and DNA viral load levels in HBsAg-positive participants.
| HBV markers | Overall N = 901 (%) |
SMI n = 227 (%) |
HASG n = 415 (%) |
HRAB n = 259 (%) |
|---|---|---|---|---|
| HBsAg | ||||
| Positive | 35 (3.9%, 2.7-5.4) | 8 (3.5%, 1.5-6.8) | 14 (3.4%, 1.9-5.8) | 13 (5%, 2.7-8.4) |
| Negative | 866 (96.1) | 219 (96.5) | 401 (96.6) | 246 (95) |
| HBeAg | ||||
| Positive | 1 (2.9%, 0.07-15) | 0 (0%, 0.0-37) | 1 (7.1%, 0.2-34) | 0 (0%, 0.0-25) |
| Negative | 34 (97.1) | 8 (100) | 13 (92.9) | 13 (100) |
| HBcAb | ||||
| Positive | 418 (46.4%, 43-50) | 93 (41%, 35-48) | 203 (48.9%, 44-54) | 122 (47.1%, 41-53) |
| Negative | 483(53.6) | 134 (59) | 212 (51.1) | 137 (52.9) |
| HBeAb | ||||
| Positive | 31 (88.6%, 73-97) | 8 (100%, 63-100) | 11 (78.6%, 49-95) | 12 (92.3%, 64-100) |
| Negative | 4 (11.4) | 0 (0) | 3 (21.4) | 1 (7.7) |
| Viral load DNA (IU/ml) | ||||
| ND | 7 (20%, 8.4-37) | 3 (37.5%, 8.5-76) | 3 (21.4%, 4.7-51) | 1 (7.7%, 0.2-36) |
| <5000 | 27 (77.1%, 60-90) | 5 (62.5%, 24-91) | 10 (71.4%, 42-92) | 12 (92.3%, 64-100) |
| >200 000 | 1 (2.9%, 0.07-15) | 0 (0%, 0-37) | 1 (7.2%, 0.2-34) | 0 (0%, 0-25) |
HASG: Hôpital de l'Amitié Sino-Gabonaise; HBcAb: antibody to the hepatitis B core antigen; HBeAb, antibody to the hepatitis B e antigen; HBeAg: hepatitis B e antigen; HBsAg: Hepatitis B surface antigen; HRAB: Hôpital Régional Amissa Bongo; ND, not detectable; SMI: Service de Santé Maternelle et Infantile.
Results
Characteristics of the study participants
Overall, we recruited 901 pregnant women; half of them, 415 (46.1%), were recruited in HASG maternity facility, while 259 (28.7%) and 227 (25.2%) were recruited in HRAB and SMI, respectively. The overall median age was 26 years (interquartile range: 21-32) and ranged from 18 years to 45 years old. 41.8% were single and up to 74.4% had a secondary school level, with all had at least a primary school level. Regarding HBV vaccination status, 24 (4.5%) declared being vaccinated and the others were either not vaccinated or did not know. Also, 73 (12.3%) declared having been tested for HBV infection in their lifetime, while the others had never been tested or did not know (Table 1).
Knowledge of HBV infection
Most of the study participants had a poor knowledge of HBV infection. Indeed, only 36% (324 out of 901) had heard about the infection before our interview (Table 2). Participants obtained information about HBV infection either during their studies, medical consultation, through a family member, or through the media. Overall, 54 out of 901, representing 6% of the participants knew that the infection was related to a virus. In addition, only 26.1% knew that HBV could be transmitted, and none of them were aware of the MTCT capacity of the virus.
Prevalence of HBV infection
Of the 901 participants, 35 representing 3.9%, (95% confidence interval: 2.7-5.4) of the study population, were tested positive for HBsAg. The prevalence of HBV infection at HRAB, SMI, and HASG was 5%, 3.5%, and 3.4% respectively (Table 3). Of the 35 HBsAg-positive women, only one was HBeAg positive. HBeAb was detected in 88.6% of HBeAg-positive women (31 out of 35). Regarding previous exposure to HBV, the overall prevalence of HBcAb was 46.4%. In the different recruitment centers (HASG, HRAB, SMI), the proportion of HBcAb-positive persons was 48.9%, 47.1%, and 41% respectively. HBV DNA was detected in 28 of the 35 HBsAg-positive women (Table 3). Viral load levels ranged from undetectable to 5,890,000 IU/ml, with a median value of 182 IU/ml (interquartile range: 81.5-1699.5). Sixteen out of 35 had a value below the detection limit (<10 IU/ml); 14/35 were below 2000 IU/ml; 4/35 participants had viral load between 2000 IU/ml and 5000 IU/ml; and 1/35 had viral load >200,000 IU/ml.
Discussion
The aim of this study was to determine the prevalence of HBV infection in pregnant women attending antenatal clinics in southern Gabon and to assess the level of knowledge on this infection in this population. Indeed, because vertical transmission of HBV represents one of the major routes of the spread of this virus, understanding the magnitude of the infection in this population, especially in sub-Saharan African is essential for the elaboration and implementation of current and future prevention and care strategies.
In this study, we found an overall HBV prevalence of 3.9%. Previous studies conducted in the country have reported a prevalence of HBsAg of 7.4% in the general population [14]. A recent study conducted among blood donors, and including 69 862 participants, reported HBV prevalence ranging from 4.4-9.9% from 2009 to 2016 in Gabon [16]. In pregnant women, a study conducted in 2008 and including five sites (Libreville, Port-Gentil, Oyem, Lambaréné et Franceville), from 1187 participants, reported 9.2% HBsAg prevalence, and the highest prevalence, 11.9%, was reported in the region of Franceville [15]. Because of the heterogenicity of these studies in their design, sampling locations, recruitment periods, and type of population assessed, it is still hard to estimate the real burden of HBV infection in the Gabonese population, stressing the need for large-scale studies such as the one we here conducted. Compared to other resource-limited countries, our results are in line with recent data on HBV burden in pregnant women. Indeed, a study conducted in Ghana between 2018 and 2019 found an HBsAg prevalence of 3.3% in 213 pregnant women [17]. Other recent studies, conducted in this population in Tanzania, Rwanda, and the Democratic Republic of Congo, reported HBsAg prevalence of 3%, 3.1%, and 3.9%, respectively [18], [19], [20]. Other studies from South Africa and Ghana reported 0.67% and 2.4% prevalence, respectively [21,22]. Most of these countries have implemented HBV vaccination programs in the past 20 years and this may be a potential benefit of these programs. However, HBV infection is still a major public health problem in Africa, and many other studies still report high infection rates in pregnant women. Eyong et al. [23] recently reported 5.7% in Cameroon, while Atilola et al. [24] reported up to 10.5% in the South-West region of Nigeria. Thus, continuous improvement of preventive actions is still essential, including reinforcing vaccination programs, better education, sensitization and information of populations, and implementation of large-scale surveillance studies to assess the efficacy of these strategies. Indeed, our results highlighted the poor participant knowledge and information on this infection, stressing the need for more information and population education on HBV and other infectious diseases that are frequently found in the country. Implementing such actions is of high importance in the context of Sub-Saharan Africa where HBV infection and exposure to this virus remain major public health concerns. Indeed, as reported by other studies in this region; Fomulu et al. [25] reported an anti-HBc prevalence of 40.8% in Cameroon, while Mansour et al. [26] reported a prevalence of 66.3% in Mauritania; we found a very high level of total HBcAb in our study population, with almost half of the participants carrying HBcAb and negative for HBsAg, indicating passed HBV infection and ongoing high level of exposure to this virus in the population.
In the goal to reduce the burden of HBV infection worldwide and potentially move to viral hepatitis elimination by 2030-2035, WHO considers the prevention of the vertical transmission of the virus from infected mother to child as a key priority [27]. In this regard, WHO recommends that pregnant women tested positive for HBV infection, with an HBV DNA ≥5.3 log10 IU/ml, means ≥200,000 IU/ml be considered for a preventive prophylaxis to prevent MTCT of HBV [27]. In this study, only one participant out of the 35 HBsAg-positive, representing less than 0.1% of our total study population, had a viral load level meeting these treatment recommendations. The majority of the remaining study participants who were HBsAg-positive had profiles of inactive HBV infection, with low risk of transmission [28]. Because access to molecular testing, especially for HBV remains very limited in the majority of African countries, including Gabon, testing for HBeAg is recommended as an alternative approach, as HBeAg is considered a marker of active HBV infection [28,29]. In our study, we found a strong correlation between the HBV DNA found and HBeAg reactivity. Indeed, the only participants we found HBeAg-positive was one with the highest HBV DNA level, ≥200,000 IU/ml, and the only one eligible for a preventive treatment according to the WHO recommendations. These results indicate that HBeAg can be a reliable marker in this context to identify HBsAg-positive pregnant women who are eligible for preventive prophylaxis. The current major issue is that access to this treatment is still very limited, and many African countries has not yet implemented national policies and guidelines for access and monitoring of this prophylactic treatment to prevent MTCT of HBV, despite the fact that tenofovir is now widely available in many countries through HIV treatment programs.
Overall, the possible significance of our work is that the real burden of HBV infection in key populations as the pregnant women may be lower than previously reported and believed in Gabon, and therefore, the elimination of the vertical transmission of the virus from the mother to child in such settings may be possible, provided that improved actions and interventions are implemented to educate the populations, increase access to testing and diagnosis and access to prophylactic treatment for eligible HBV-positive pregnant women.
Our study has some limitations. First, this was a cross-sectional intervention, and thus, participants were assessed at a single time point. Also, for participants tested HBsAg positive, there was no clinical assessment (liver enzymes, assessment of liver fibrosis, etc.) and no information on potential clinical evolution. Finally, self-reported answers to questions on HBV knowledge and previous testing can generate uncertainty.
In conclusion, in a large-scale study we conducted in south-Gabon, we found a high level of exposure of pregnant women to HBV, although with a low proportion of HBV infection (HBsAg-positive). Moreover, the proportion of women at risk of vertically transmitting HBV to their children was very low, but as access to preventive prophylaxis remains scarce, immediate vaccination of children at birth remains a priority to improve this prevention and move to a potential future elimination.
Declarations of competing interest
The authors have no competing interests to declare.
Acknowledgments
Funding
This work was supported by the Institut de Recherche pour le Développement (IRD).
Ethical approval
The study protocol was approved by the National Ethics Committee of Gabon under authorization N 0021/2020/PR/SG/CNER. All participants provided signed informed consent before their inclusion in the study and anonymous identifiers were assigned to preserve participant's confidentiality.
Acknowledgments
We thank all the pregnant women who participated in this study and the midwives of the HRAB, HASG, and SMI who contributed to the implementation of this work. We thank the Gabon Health Authorities for providing the necessary authorizations for this research.
Author contributions
AFA, EE, NN, AMO, and DSKM designed the study. DSKM, EE, LBK, AD, SEKM, and YM contributed to the recruitment, sampling, laboratory testing, data interpretation, and statistical analyses. AFA, NN, DSKM, EE, and AMO contributed to the writing of the manuscript.
References
- 1.World Health Organization . 2016. Global health sector strategy on viral hepatitis 2016–2021. [Google Scholar]; https://www.who.int/publications/i/item/WHO-HIV-2016.06/ [accessed 04 July 2022].
- 2.Stanaway JD, Flaxman AD, Naghavi M, Fitzmaurice C, Vos T, Abubakar I, et al. The global burden of viral hepatitis from 1990 to 2013: findings from the Global Burden of Disease Study 2013. Lancet. 2016;388:1081–1088. doi: 10.1016/S0140-6736(16)30579-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization (WHO) 2021. Interim guidance for country validation of viral hepatitis elimination. [DOI] [PubMed] [Google Scholar]; https://www.who.int/publications/i/item/9789240028395/ [accessed 26 September 2022].
- 4.Seto W, Lo Y, Pawlotsky J, Yuen M. Chronic hepatitis B virus infection. Lancet. 2018;392:2313–2324. doi: 10.1016/S0140-6736(18)31865-8. [DOI] [PubMed] [Google Scholar]
- 5.Thomas DL. Global elimination of chronic hepatitis. N Engl J Med. 2019;380:2041–2050. doi: 10.1056/NEJMra1810477. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization (WHO) 2022. Global health sector strategies on, respectively, HIV, viral hepatitis and sexually transmitted infections for the period 2022–2030. [Google Scholar]; https://www.who.int/teams/global-hiv-hepatitis-and-stisprogrammes/strategies/global-health-sector-strategies/ [accessed 25 September 2022].
- 7.GBD Global, regional, and national burden of hepatitis B, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Gastroenterol Hepatol. 2022;7:796–829. doi: 10.1016/S2468-1253(22)00124-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Flores JE, Thompson AJ, Ryan M, Howell J. The global impact of hepatitis B vaccination on hepatocellular carcinoma. Vaccines. 2022;10:793. doi: 10.3390/vaccines10050793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hambridge T, Nartey Y, Duah A, Plymoth A. Hepatitis B mother-to-child transmission in the eastern region of Ghana: a cross-sectional pilot study. Pan Afr Med J. 2019;33:218. doi: 10.11604/pamj.2019.33.218.17242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Noubjap JJ, Ndoula ST. Prevention of mother-to-child transmission of hepatitis B: birth-dose vaccination is not enough. Lancet Glob Heal. 2022;10:e455–e456. doi: 10.1016/S2214-109X(22)00046-8. [DOI] [PubMed] [Google Scholar]
- 11.Johannessen A, Mekasha B, Desalegn H, Aberra H, Stene-Johansen K, Berhe N. Mother-to-child transmission of hepatitis B virus in Ethiopia. Vaccines. 2021;9:1–10. doi: 10.3390/vaccines9050430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chilaka VN, Konje JC. Viral Hepatitis in pregnancy. Eur J Obstet Gynecol Reprod Biol. 2021;256:287–296. doi: 10.1016/j.ejogrb.2020.11.052. [DOI] [PubMed] [Google Scholar]
- 13.Jefferies M, Rauff B, Rashid H, Lam T, Rafiq S. Update on global epidemiology of viral hepatitis and preventive strategies. World J Clin Cases. 2018;6:589–599. doi: 10.12998/wjcc.v6.i13.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Groc S, Abbate JL, Le Gal F, Gerber A, Tuaillon E, Albert JL, et al. High prevalence and diversity of hepatitis B and hepatitis delta virus in Gabon. J Viral Hepat. 2019;26:170–182. doi: 10.1111/jvh.12991. [DOI] [PubMed] [Google Scholar]
- 15.Makuwa M, Caron M, Souquière S, Malonga-Mouelet G, Mahé A, Kazanji M. Prevalence and genetic diversity of hepatitis B and delta viruses in pregnant women in gabon: molecular evidence that hepatitis delta virus clade 8 originates from and is endemic in Central Africa. J Clin Microbiol. 2008;46:754–756. doi: 10.1128/JCM.02142-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Eko Mba JM, Bisseye C, Ntsame Ndong JM, Mombo LE, Bengone C, Mouelet Migolet G, et al. Prevalent hepatitis B surface antigen among first-time blood donors in Gabon. PLoS One. 2018;13 doi: 10.1371/journal.pone.0194285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kwadzokpui PK, Akorsu EE, Abaka-Yawson A, Quarshie SS, Amankwah SA, Tawiah PA. Prevalence and knowledge of hepatitis B virus infection among pregnant women in the Ningo-Prampram District, Ghana. Int J Hepatol. 2020;2020 doi: 10.1155/2020/7965146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Geffert K, Maponga TG, Henerico S, Preiser W, Mongella S, Stich A, et al. Prevalence of chronic HBV infection in pregnant woman attending antenatal care in a tertiary hospital in Mwanza, Tanzania: a cross-sectional study. BMC Infect Dis. 2020;20:395. doi: 10.1186/s12879-020-05096-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nyamusi M, Marete O, Waweru W. Seroprevalence of hepatitis B among pregnant women in Kigali, Rwanda. Int J Community Med Public Health. 2016;3:3096–3101. doi: 10.18203/2394-6040.ijcmph20163918. [DOI] [Google Scholar]
- 20.Mudji J, Madinga B, Horsmans Y. Seroprevalence of viral hepatitis B and C and knowledge of the hepatitis B virus among pregnant women attending prenatal care in the Democratic Republic of Congo. Am J Trop Med Hyg. 2021;104:1096–1100. doi: 10.4269/ajtmh.20-0804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Joseph Davey D, Hsiao N, Wendy Spearman C, Sonderup M, Hu N, Mashele N, et al. Low prevalence of hepatitis B virus infection in HIV-uninfected pregnant women in Cape Town, South Africa: implications for oral pre-exposure prophylaxis roll out. BMC Infect Dis. 2022;22:1–5. doi: 10.1186/s12879-022-07697-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Luuse A, Dassah S, Lokpo S, Ameke L, Noagbe M, Adatara P, et al. Sero-prevalence of hepatitis B surface antigen amongst pregnant women attending an antenatal clinic, Volta region, Ghana. J Public Health Afr. 2017;7:584. doi: 10.4081/jphia.2016.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Eyong EM, Yankam BM, Seraphine E, Ngwa CH, Nkfusai NC, Anye CS, et al. The prevalence of HBsAg, knowledge and practice of hepatitis B prevention among pregnant women in the limbe and Muyuka health districts of the south west region of Cameroon: a three-year retrospective study. Pan Afr Med J. 2019;32:122. doi: 10.11604/pamj.2019.32.122.16055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Atilola G, Tomisin O, Randle M, Isaac KO, Odutolu G, Olomu J, et al. Epidemiology of HBV in pregnant women, South West Nigeria. J Epidemiol Glob Health. 2018;8:115–123. doi: 10.2991/j.jegh.2018.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fomulu NJ, Morfaw FL, Torimiro JN, Nana P, Koh MV, William T. Prevalence, correlates and pattern of hepatitis B among antenatal clinic attenders in Yaounde-Cameroon: is perinatal transmission of HBV neglected in Cameroon? BMC Pregnancy Childbirth. 2013;13:1–10. doi: 10.1186/1471-2393-13-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mansour W, Malick FZ, Sidiya A, Ishagh E, Chekaraou MA, Veillon P, et al. Prevalence, risk factors, and molecular epidemiology of hepatitis B and hepatitis delta virus in pregnant women and in patients in Mauritania. J Med Virol. 2012;84:1186–1198. doi: 10.1002/jmv.23336. [DOI] [PubMed] [Google Scholar]
- 27.World Health Organization . 2020. Prevention of mother-to-child transmission of hepatitis B virus: guidelines on antiviral prophylaxis in pregnancy. [PubMed] [Google Scholar]; http://www.ncbi.nlm.nih.gov/pubmed/32833415/ [accessed 14 July 2022].
- 28.Veronese P, Dodi I, Esposito S, Indolfi G. Prevention of vertical transmission of hepatitis B virus infection. World J Gastroenterol. 2021;27:4182–4193. doi: 10.3748/wjg.v27.i26.4182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bonino F, Colombatto P, Brunetto MR. HBeAg-negative/anti-HBe-positive chronic hepatitis B : a 40-year-old history. Viruses. 2022;14:169. doi: 10.3390/v14081691. [DOI] [PMC free article] [PubMed] [Google Scholar]