Summary
Background
Promoting active, balanced lifestyles among children may be an important approach to optimising their health-related quality of life (HRQoL). However, the relationships between children's movement behaviours and HRQoL remain unclear.
Methods
We examined the associations between movement behaviours (sleep, inactivity, light and moderate-to-vigorous intensity physical activity) assessed using accelerometers at ages 8 and 10 years and self-reported HRQoL scores (overall, and physical and emotional well-being, self-esteem, relationship with family and friends, and school functioning domains) at age 10 years among 370 children in a local birth cohort using compositional isotemporal substitution techniques.
Findings
Cross-sectionally, light and moderate-to-vigorous intensity physical activities were associated with better self-esteem (β = 15.94 [2.71, 29.18]) and relationship with friends (β = 10.28 [3.81, 16.74]) scores respectively. Prospectively, inactivity was associated with lower overall HRQoL (β = −10.00 [−19.13, −0.87]), relationship with friends (β = −16.41 [−31.60, −1.23]) and school functioning (β = −15.30 [−29.16, −1.44]) scores, while sleep showed a positive trend with overall HRQoL (β = 10.76 [−1.09, 22.61]) and school functioning (β = 17.12 [−0.87, 35.10]) scores. Children's movement behaviours were not associated with their physical and emotional well-being, or relationship with family scores. The isotemporal substitution analyses suggest that increasing time spent in physical activity and/or sleep at the expense of inactivity may benefit children's HRQoL.
Interpretation
Our findings suggest that sleep and physical activity may be associated with better HRQoL, with the inverse for inactivity. However, the relationship between children's movement behaviours and HRQoL is complex and warrants further research.
Funding
Singapore National Research Foundation, Singapore Institute for Clinical Sciences, Agency for Science, Technology and Research.
Keywords: Children, Adolescent, Health-related quality of life, Movement behaviour, Physical activity, Sleep, Inactivity, Time-use, Cross-sectional, Prospective
Research in context.
Evidence before this study
Concerningly, HRQoL of children in various countries was observed to decline with age; in Singapore, this decline was observed to occur from the age of 10 years. While this decline may be attributed to lesser leisure time, increased academic pressure, and the transition into puberty as children grow older, poorer HRQoL among older children may also be associated with their changes in sleep, inactivity, and physical activity (of light and moderate-to-vigorous intensity) patterns, collectively referred to as movement behaviours. Studies have found that children who were more active had better physical and psychosocial functioning as they had healthier weight status, better self-esteem, opportunities for socialisation, and increased endorphin levels that promote a sense of pleasure and well-being. Sleep on the other hand was associated with mood and emotional regulation wherein inadequate sleep was associated with poorer HRQoL among children aged 9–11 years. Though the mechanisms of inactivity on HRQoL were less explored, it is postulated that time spent in inactivity may displace physical activity and/or sleep, explaining the negative associations with HRQoL. Given that physical activity levels were observed to decline as children grow older and transition into adolescence, promoting active and balanced lifestyles among children may be an approach to improve their self-perceived well-being and functioning, leading to functional, optimal lives.
Added value of this study
To date, most studies have only examined single behaviours in association with HRQoL, without accounting for the interrelatedness of the movement behaviours in a constrained 24-h day, resulting in inaccurate estimates of association. Further, existing studies have largely been cross-sectional by design and are thus susceptible to reverse causation, warranting prospective or longitudinal studies to confirm these trends. HRQoL research in children have also been concentrated in Western contexts, with limited representation of Asian populations. Since perception of HRQoL reflects one's life experiences which could depend on political, social, economic, and environmental factors, findings from other populations have limited generalisability to other contexts.
The present study aimed to fill these gaps by examining the cross-sectional and prospective associations between children's movement behaviours at 10 and 8 years and their HRQoL at 10 years. To appropriately account for the compositional nature of 24-h time-use and the interrelatedness of the movement behaviours, a compositional data analysis approach was implemented. We further predicted the change in HRQoL score at 10 years when 30 min is reallocated between the four movement behaviours at 10 and 8 years. These findings seek to contribute to the current evidence base regarding the movement behaviours of children in an Asian sample and their HRQoL.
Implications of all the available evidence
Our study is novel in that it is, to our knowledge, the first that examined the cross-sectional and prospective associations between the full movement spectrum of children and their overall and domain specific HRQoL, in the less studied Asian population. Generally, we suggest that sleep and physical activity may be positively associated with HRQoL, while inactivity may be negatively associated with HRQoL. However, our findings also demonstrate the complexity of the relationship between children's movement behaviours and HRQoL, highlighting the need for further research.
Introduction
Research on health-related quality of life (HRQoL), a subjective multi-dimensional construct encompassing physical, psychological, and social health,1,2 has been gaining traction.3 Being a strong predictor of morbidity and mortality,4,5 suboptimal HRQoL presents an important public health concern, especially since awareness of the importance of optimal functioning beyond the absence of ill health is increasing.6 Concerningly, HRQoL of children in various countries was observed to decline with age7, 8, 9; in Singapore, this decline was observed to occur from the age of 10 years.8
While this decline may be attributed to lesser leisure time, increased academic pressure, and the transition into puberty as children grow older,7 poorer HRQoL among older children may also be associated with their changes in sleep, inactivity, and physical activity (of light and moderate-to-vigorous intensity) patterns, collectively referred to as movement behaviours.10 Studies have found that children who engaged in more physical activity had better physical and psychosocial functioning as they had healthier weight status, better self-esteem, opportunities for socialisation, and increased endorphin levels that promote a sense of pleasure and well-being.11, 12, 13 Sleep on the other hand was associated with mood and emotional regulation14,15 wherein inadequate sleep was associated with poorer HRQoL among children aged 9–11 years.16 Though the mechanisms of inactivity on HRQoL were less explored,10 it is postulated that time spent in inactivity may displace physical activity and/or sleep, explaining the associations with poorer HRQoL.10
As children grow older and gain autonomy over their lifestyle aspects, they become less physically active and increasingly sedentary.17, 18, 19, 20, 21, 22 A recent study in the Growing Up in Singapore Towards healthy Outcomes (GUSTO) cohort revealed that between the ages of 5.5 and 8 years, children's movement behaviours transitioned towards being more sedentary and less physically active.23 Other studies have found that particularly from the age of around 10 years, children tended to be more sedentary and have less physical activity and inadequate sleep as they transitioned into adolescence.16,24
Promoting children's movement behaviours may therefore be an approach to improve their self-perceived well-being and functioning, leading to functional, optimal lives. Yet, the relationship between children's movement behaviours and their HRQoL remains unclear. To date, most studies have only examined single behaviours in association with HRQoL, without accounting for the interrelatedness of the movement behaviours in a constrained 24-h day,10 resulting in inaccurate estimates of association.25,26 Given that physical activity intensity, beyond just quantity, has been associated with better outcomes in children,27 research differentiating the effects of physical activity at various intensities on outcomes are needed. Few have examined if light physical activity (LPA) and moderate-to-vigorous physical activity (MVPA) differ in association with HRQoL,11 warranting more research to confirm existing findings. Further, studies to date have largely been cross-sectional by design and are thus susceptible to reverse causation, whereby prospective or longitudinal studies are required to confirm these trends.10,11,28 HRQoL research in children have also been concentrated in Western contexts, with limited representation of Asian populations.11,28 Since perception of HRQoL reflects one's life experiences29 which could depend on political, social, economic, and environmental factors,30 findings from other populations have limited generalisability to other contexts.
The limitations of the existing literature warrant further investigations to bridge important knowledge gaps relating to children's movement behaviours and their HRQoL, particularly in the Asian context. The present study aimed to fill these gaps by examining the cross-sectional and prospective associations between children's movement behaviours at 10 and 8 years and their HRQoL at 10 years. To appropriately account for the compositional nature of 24-h time-use and the interrelatedness of the movement behaviours, a compositional data analysis approach was implemented. We further predicted the change in HRQoL score at 10 years when 30 min is reallocated between the four movement behaviours at 10 and 8 years. We hypothesise that the four movement behaviours would differentially influence HRQoL outcomes cross-sectionally and/or prospectively. These findings seek to contribute to the current evidence base regarding the movement behaviours of children in an Asian sample and their HRQoL.
Methods
Study design
Child participants in the present study were part of the GUSTO mother-offspring cohort. Details of the cohort have been published previously.31 In brief, the GUSTO study was started in 2009. Pregnant women were recruited from two major public maternity units in Singapore, KK Women's and Children's Hospital, and National University Hospital. To be eligible, they had to be aged at least 18 years, of Chinese, Malay, or Indian ethnicity with a same-ethnicity partner, Singapore citizens or permanent residents, and were intending to deliver in one of the two above-mentioned maternity units and remain in Singapore for the following five years. All participants provided written informed consent at enrolment. The study was ethically reviewed and approved by the National Healthcare Group Domain Specific Review Board and the SingHealth Centralised Institutional Review Board.
Data collection
Covariates
Sociodemographic information was collected from medical records at birth, or via interviewer administered questionnaires at various stages of follow up. These included variables such as the child's sex, ethnicity, and maternal education at age 5 years, used as proxy for socioeconomic status (SES). Child body mass index (BMI) was derived based on anthropometric measurements obtained at the follow up visit at age 8 years. Height and weight were measured up to thrice using a weighing scale (SECA model 803) and stadiometer (SECA model 213, Hamburg, Germany), respectively; repeated measures were averaged. BMI was calculated using the formula: weight (in kg)/squared height (in m2) and classified as underweight, normal weight, and overweight based on age- and sex-specific cut-offs for Singaporean children.32 For participants with missing covariate information (n = 39 for maternal education at age 5 years, n = 2 for BMI at age 8 years), data from the preceding timepoint (pregnancy week 11 and age 7 years respectively) were used to impute missing information.
24-h Movement behaviours
During the follow up at ages 8 and 10 years, participants were asked to wear a triaxial accelerometer (ActiGraph wGT3X + -BT; ActiGraph Pensacola, FL, USA) on their non-dominant wrist using a non-removable strap to monitor their movement behaviours at both timepoints. Accelerometers were initialized with a sampling rate of 80 Hz. Parents were instructed to remove the device from the child's wrist on the ninth day following the visit, allowing for 7 complete days of continuous, 24-h data capture. Upon return of the device, raw data were extracted with the ActiLife software, then processed using the GGIR package available in R (version 2.0–0) according to a published protocol.33 In brief, raw accelerometer signals were auto-calibrated and expressed as gravity-corrected vector magnitude units (Euclidean Norm Minus One [ENMO]). Non-wear time was estimated based on standard deviations and value range of each accelerometer axis at 60-min windows in 15-min increments. To be considered valid and included for analyses, each participant's accelerometer data must have a minimum of 16 h of valid wear time per day for at least three days (two weekdays and one weekend day). Of the valid days, non-wear time in blocks of 15 min were imputed based on the mean value from other valid days.34 Time spent in sleep, inactivity (ENMO <35.0 mg), LPA (ENMO 35.0–200 mg), and MVPA (ENMO>200 mg) were derived based on previously established protocols and acceleration thresholds according to van Hees, Hildebrand, and colleagues.35, 36, 37 For the present study, inactivity was used as proxy for sedentary behaviour (defined as activities “≤1.5 metabolic equivalents while in a sitting, reclining or lying posture”38) since wrist-worn accelerometers cannot determine whole body posture. Sleep was quantified as the sum of night sleep and naps, defined as periods exceeding 15 min of sustained inactivity during wear time. Weekday and weekend day data were weighted using the ratio of 5:2 and averaged, such that the averaged data were representative of a full seven-day week.
Health-related quality of life
HRQoL was collected using the KINDL-Kid questionnaire administered to the child participants during their follow up at age 10 years. This questionnaire has been validated among local Singaporean children.39 It comprises 24 questions that assess six domains of HRQoL (four questions per domain, each question with five answer categories), namely physical well-being, emotional well-being, self-esteem, relationship with family, relationship with friends, and school functioning, which are summed to provide an overall HRQoL score. Domain-specific (original scale: 4–20) and overall HRQoL scores (original scale: 24–120) were transformed to a scale of 0–100 to facilitate interpretation.
Statistical analyses
Participants with complete data were included in the analyses. Test for differences in characteristics between included and excluded participants were conducted using Pearson's Chi-squared tests. Mean and standard deviation values described the distribution of movement behaviour durations and HRQoL scores among included participants.
Compositional data analysis was performed to explain the relationship between movement behaviour compositions and HRQoL26 based on previously developed methods by Dumuid and colleagues for epidemiological research.40 Time spent in each movement behaviour at age 10 years was transformed using sequential binary partitioning and expressed as isometric log ratios (ilr),41 such that the first coordinate presented one movement behaviour (e.g., sleep) as the numerator, and the geometric mean of the remaining behaviours (i.e., inactivity, LPA, and MVPA) as the denominator.25 This coordinate therefore contained information regarding one movement behaviour as a variable relative to the other three behaviours.40 A total of four sets of ilr coordinates were purposefully created to ensure that each behaviour could be represented as a numerator relative to the remaining behaviours as the first coordinate.40 As each set of ilr coordinates were included as predictors in a model, four models were generated for each of the four sets. The beta coefficients and 95% confidence interval from the multiple linear regression models of the first coordinates of each set of ilr coordinates were interpreted as the positive or negative association between each movement behaviour, relative to the remaining behaviours, and each HRQoL outcome. The models were adjusted for the following potential confounders: sex, ethnicity, maternal education level, and the child's weight status at age 8 years. Given that the year in which children turned 10 years old coincided with the COVID-19 pandemic which may influence their HRQoL, we also accounted for whether the child was followed up at age 10 years before or after the onset of the COVID-19 pandemic.
Using the models created in the compositional data analysis, isotemporal substitution was performed to investigate the theoretical effects of replacing specific amounts of time in one behaviour with that of another while time spent in other behaviours remained constant, on each HRQoL outcome (i.e., overall and domain scores). The mean movement behaviour composition of our sample was used as the reference composition for isotemporal substitution.42 For example, to increase time spent in sleep by 30 min, we decreased the time spent in MVPA by 30 min, with the time spent in inactivity and LPA remaining the same. 30 min reallocations were selected to provide meaningful interpretation of our isotemporal substitution analysis findings as sleep, inactivity and LPA constitute most of a 24-h day (i.e., each 5–9 h on average a day), and reallocations using shorter durations (<30 min) would result in very small magnitudes of difference in HRQoL scores.
To examine the prospective associations between the movement behaviours and HRQoL, the above analyses were repeated using movement behaviours at age 8 years as the exposure variable and HRQoL at 10 years as the outcome variable. Similarly, the models were adjusted for the following covariates: sex, ethnicity, maternal education level, child's weight status at age 8 years, and whether the participant was followed up before or after the onset of the COVID-19 pandemic at age 10 years.
All analyses were performed in R (version 4.1.1) using the compositions,43 robCompositions,44 lmtest,45 and car46 packages.
Role of the funding source
The funders had no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Results
Participant characteristics
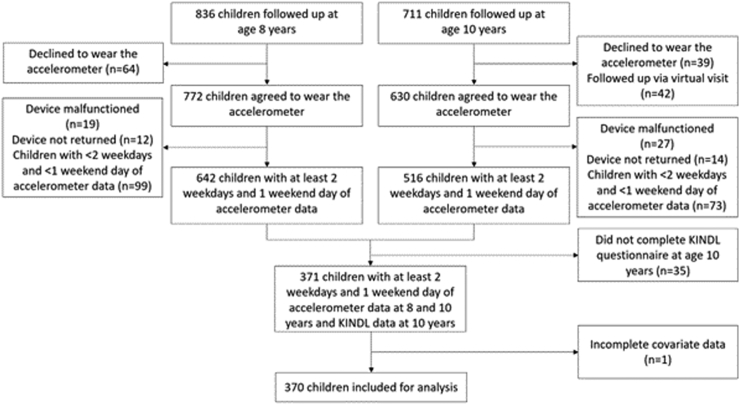
Of the 836 and 711 children followed up at ages 8 and 10 years respectively, 370 children with valid accelerometer data at both time points and complete KINDL-Kid questionnaire and covariate data were included in the present analyses (Fig. 1). Most were girls (50.5%), of Chinese ethnicity (58.4%), of mothers with at least a degree-level education (48.9%), of normal weight (78.9%), and completed their KINDL questionnaire after the onset of the COVID-19 pandemic in Singapore (94.9%) (Table 1). Included and excluded participants did not differ in characteristics significantly (Supplementary Table S1).
Fig. 1.
Flowchart of the GUSTO participants examined in the present study.
Table 1.
Descriptives of final sample.
| Study sample (n = 370) | |
|---|---|
| Sex, n (%) | |
| Boys | 183 (49.5) |
| Girls | 187 (50.5) |
| Ethnicity, n (%) | |
| Chinese | 216 (58.4) |
| Malay | 101 (27.3) |
| Indian | 53 (14.3) |
| Maternal education, n (%) | |
| No education/Primary/Secondary | 112 (30.3) |
| Post-secondary | 77 (20.8) |
| Degree and above | 181 (48.9) |
| Weight status at age 8 years, n (%) | |
| Underweight | 43 (11.6) |
| Normal weight | 292 (78.9) |
| Overweight | 35 (9.5) |
| Completion of KINDL questionnaire, n (%) | |
| After onset of COVID-19 pandemic | 351 (94.9) |
| Before onset of COVID-19 pandemic | 19 (5.1) |
| Movement behaviours at age 8 years, mean (s.d.) | |
| Sleep, h/day | 8.6 (0.8) |
| Inactivity, h/day | 8.4 (1.1) |
| LPA, h/day | 5.6 (0.9) |
| MVPA, min/day | 71.5 (28.6) |
| Movement behaviours at age 10 years, mean (s.d.) | |
| Sleep, h/day | 8.5 (0.8) |
| Inactivity, h/day | 9.6 (1.2) |
| LPA, h/day | 5.0 (1.0) |
| MVPA, min/day | 49.6 (23.9) |
| HRQoL scores at age 10 years, mean (s.d.) | |
| Total HRQoL | 66.4 (12.8) |
| Physical well-being | 79.3 (14.7) |
| Emotional well-being | 74.1 (16.3) |
| Self-esteem | 46.0 (23.0) |
| Relationship with family | 71.3 (17.6) |
| Relationship with friends | 65.8 (21.5) |
| School functioning | 62.0 (19.7) |
Abbreviations: light intensity physical activity (LPA), moderate-to-vigorous intensity physical activity (MVPA), health-related quality of life (HRQoL).
Children's time spent in sleep, inactivity, LPA and MVPA at ages 8 and 10 years, and their HRQoL scores at age 10 years were presented in Table 1.
Cross–sectional associations between movement behaviours and HRQoL
Table 2 presents the cross–sectional association between each movement behaviour (e.g., sleep) relative to the remaining behaviours (i.e., inactivity, LPA, and MVPA).
Table 2.
Compositional time use at age 10 years and its association with HRQoL.
| Overall HRQoL | Physical well-being | Emotional well-being | Self-esteem | Relationship with family | Relationship with friends | School functioning | |
|---|---|---|---|---|---|---|---|
| Sleep | −6.82 (−17.39, 3.75) (p = 0.205) | 0.50 (−11.78, 12.78) (p = 0.936) | −9.62 (−23.10, 3.86) (p = 0.161) | −16.80 (−35.84, 2.23) (p = 0.083) | −9.42 (−24.02, 5.17) (p = 0.205) | −3.33 (−20.79, 14.13) (p = 0.708) | −2.23 (−18.39, 13.91) (p = 0.785) |
| Inactivity | −1.54 (−9.89, 6.81) (p = 0.717) | −3.37 (−13.07, 6.32) (p = 0.494) | 1.33 (−9.32, 11.98) (p = 0.806) | 1.87 (−13.17, 16.90) (p = 0.807) | 4.22 (−7.31, 15.75) (p = 0.472) | −7.00 (−20.79, 6.78) (p = 0.318) | −6.28 (−19.04, 6.47) (p = 0.333) |
| LPA | 5.40 (−1.94, 12.75) (p = 0.149) | −1.34 (−9.88, 7.19) (p = 0.757) | 5.18 (−4.19, 14.54) (p = 0.278) | 15.94 (2.71, 29.18) (p = 0.018) | 5.11 (−5.03, 15.26) (p = 0.322) | 0.06 (−12.07, 12.19) (p = 0.992) | 7.48 (−3.75, 18.71) (p = 0.191) |
| MVPA | 2.95 (−0.96, 6.87) (p = 0.139) | 4.22 (−0.33, 8.77) (p = 0.069) | 3.11 (−1.88, 8.11) (p = 0.221) | −1.01 (−8.06, 6.04) (p = 0.778) | 0.09 (−5.32, 5.49) (p = 0.975) | 10.28 (3.81, 16.74) (p = 0.002) | 1.04 (−4.94, 7.03) (p = 0.732) |
Analysis performed using multivariable linear regression models; results presented as β (95% confidence intervals). Models were adjusted for sex, ethnicity, maternal education level, child's categorical weight status at age 8 years, and whether the participant was followed up before or after the onset of the COVID-19 pandemic.
Abbreviations: light intensity physical activity (LPA), moderate-to-vigorous intensity physical activity (MVPA), health-related quality of life (HRQoL).
Cross-sectionally, LPA was associated with better self-esteem (β = 15.94 [2.71, 29.18]) and MVPA was associated with better relationship with friends (β = 10.28 [3.81, 16.74]). We found no cross–sectional association between movement behaviours and overall HRQoL, or with the domains of HRQoL relating to physical and emotional well-being, relationship with family, and school functioning at 10 years of age.
Isotemporal substitution analyses largely concurred with the previous findings on the associations between LPA and MVPA and better self-esteem and relationship with friends respectively (Table 3). The analyses suggested that displacement of 30 min between sleep and LPA was associated with children's self-esteem: increasing time spent in sleep at the expense of LPA was associated with poorer self-esteem (β = −2.29 [−4.10, −0.48]), and the inverse was observed when time spent in LPA was increased at the expense of sleep (β = 2.20 [0.45, 3.95]). There was also a trend where increasing time spent in inactivity at the expense of LPA was associated with poorer self-esteem (β = −1.39 [−2.85, 0.07]).
Table 3.
Reallocation of 30 min between pairs of movement behaviours at age 10 years and on the predicted change in HRQoL scores at age 10 years (95% confidence intervals).
| Overall HRQoL | Physical well-being | Emotional well-being | Self-esteem | Relationship with family | Relationship with friends | School functioning | |
|---|---|---|---|---|---|---|---|
| Increase sleep | |||||||
| Reduce inactivity | −0.26 (−1.12, 0.59) (p = 0.547) | 0.18 (−0.81, 1.17) (p = 0.722) | −0.53 (−1.62, 0.56) (p = 0.339) | −0.91 (−2.44, 0.63) (p = 0.248) | −0.65 (−1.83, 0.53) (p = 0.276) | 0.16 (−1.25, 1.57) (p = 0.824) | 0.18 (−1.13, 1.48) (p = 0.787) |
| Reduce LPA | −0.83 (−1.83, 0.17) (p = 0.105) | 0.15 (−1.02, 1.31) (p = 0.803) | −0.95 (−2.23, 0.33) (p = 0.147) | −2.29 (−4.10, −0.48) (p = 0.013) | −0.93 (−2.32, 0.45) (p = 0.187) | −0.17 (−1.83, 1.49) (p = 0.842) | −0.80 (−2.33, 0.74) (p = 0.307) |
| Reduce MVPA | −3.14 (−7.02, 0.73) (p = 0.112) | 3.99 (−8.49, 0.51) (p = 0.082) | −3.43 (−8.37, 1.51) (p = 0.173) | 0.14 (−6.84, 7.12) (p = 0.969) | −0.54 (−5.89, 4.81) (p = 0.842) | −9.93 (−16.33, −3.53) (p = 0.002) | −1.10 (−7.02, 4.82) (p = 0.715) |
| Increase inactivity | |||||||
| Reduce sleep | 0.28 (−0.58, 1.15) (p = 0.518) | −0.17 (−1.18, 0.83) (p = 0.735) | 0.55 (−0.55, 1.66) (p = 0.324) | 0.95 (−0.61, 2.51) (p = 0.232) | 0.67 (−0.52, 1.87) (p = 0.270) | −0.13 (−1.56, 1.30) (p = 0.854) | −0.16 (−1.48, 1.16) (p = 0.814) |
| Reduce LPA | −0.57 (−1.37, 0.24) (p = 0.170) | −0.02 (−0.96, 0.92) (p = 0.961) | −0.42 (−1.45, 0.61) (p = 0.425) | −1.39 (−2.85, 0.07) (p = 0.062) | −0.29 (−1.40, 0.83) (p = 0.614) | −0.31 (−1.65, 1.03) (p = 0.647) | −0.96 (−2.20, 0.27) (p = 0.126) |
| Reduce MVPA | −2.88 (−6.52, 0.77) (p = 0.121) | −4.16 (−8.39, 0.07) (p = 0.054) | −2.90 (−7.55, 1.74) (p = 0.220) | 1.04 (−5.52, 7.60) (p = 0.755) | 0.10 (−4.93, 5.13) (p = 0.968) | −10.07 (−16.09, −4.05) (p = 0.001) | −1.27 (−6.83, 4.30) (p = 0.655) |
| Increase LPA | |||||||
| Reduce sleep | 0.80 (−0.17, 1.77) (p = 0.105) | −0.14 (−1.27, 0.99) (p = 0.810) | 0.93 (−0.31, 2.17) (p = 0.142) | 2.20 (0.45, 3.95) (p = 0.014) | 0.91 (−0.43, 2.26) (p = 0.182) | 0.18 (−1.43, 1.78) (p = 0.828) | 0.74 (−0.75, 2.22) (p = 0.329) |
| Reduce inactivity | 0.52 (−0.24, 1.28) (p = 0.180) | 0.04 (−0.84, 0.93) (p = 0.924) | 0.37 (−0.60, 1.34) (p = 0.455) | 1.24 (−0.13, 2.62) (p = 0.076) | 0.23 (−0.82, 1.29) (p = 0.665) | 0.33 (−0.93, 1.59) (p = 0.610) | 0.91 (−0.25, 2.08) (p = 0.125) |
| Reduce MVPA | −2.36 (−6.43, 1.71) (p = 0.255) | −4.12 (−8.85, 0.60) (p = 0.087) | −2.53 (−7.72, 2.66) (p = 0.338) | 2.29 (−5.03, 9.61) (p = 0.539) | 0.34 (−5.27, 5.96) (p = 0.904) | −9.76 (−16.48, −3.05) (p = 0.004) | −0.37 (−6.58, 5.85) (p = 0.907) |
| Increase MVPA | |||||||
| Reduce sleep | 1.66 (−0.27, 3.59) (p = 0.092) | 1.84 (−0.40, 4.09) (p = 0.108) | 1.87 (−0.59, 4.34) (p = 0.136) | 0.42 (−3.06, 3.90) (p = 0.812) | 0.53 (−2.14, 3.19) (p = 0.700) | 4.71 (1.52, 7.91) (p = 0.004) | 0.58 (−2.38, 3.53) (p = 0.701) |
| Reduce inactivity | 1.38 (−0.29, 3.05) (p = 0.106) | 2.02 (0.08, 3.96) (p = 0.041) | 1.32 (−0.81, 3.45) (p = 0.225) | −0.53 (−3.54, 2.47) (p = 0.728) | −0.16 (−2.46, 2.15) (p = 0.894) | 4.87 (2.11, 7.63) (p = 0.001) | 0.75 (−1.80, 3.30) (p = 0.564) |
| Reduce LPA | 0.81 (−1.35, 2.96) (p = 0.461) | 1.99 (−0.51, 4.49) (p = 0.119) | 0.90 (−1.85, 3.65) (p = 0.520) | −1.92 (−5.80, 1.96) (p = 0.332) | −0.43 (−3.41, 2.54) (p = 0.775) | 4.54 (0.98, 8.10) (p = 0.013) | −0.23 (−3.52, 3.06) (p = 0.892) |
Results are interpreted as the difference in HRQoL when time spent in one behaviour is increased at the expense of another, while the remaining two behaviours remain constant.
Analysis performed using multivariable linear regression models, results presented as the predicted changes in HRQoL scores at age 10 years and their 95% confidence intervals reported within the brackets. Models were adjusted for sex, ethnicity, maternal education level, child's categorical weight status at age 8 years, and whether the participant was followed up before or after the onset of the COVID-19 pandemic.
Abbreviations: light intensity physical activity (LPA), moderate-to-vigorous intensity physical activity (MVPA), health-related quality of life (HRQoL).
For MVPA, increasing time spent in sleep (β = −9.93 [−16.33, −3.53]), inactivity (β = −10.07 [−16.09, −4.05]), or LPA (β = −9.76 [−16.48, −3.05]) by 30 min at the expense of MVPA was associated with poorer relationship with friends. These associations were of greater magnitude than the inverse, that is when MVPA was increased by 30 min at the expense of sleep (β = 4.71 [1.52, 7.91]), inactivity (β = 4.87 [2.11, 7.63]), or LPA (β = 4.54 [0.98, 8.10]), suggesting that the relationship between MVPA and relationship with friends is not symmetrical.
Additionally, we observed that increasing time spent in MVPA at the expense of inactivity was associated with better physical well-being (β = 2.02 [0.08, 3.96]), with the inverse observed when time is reallocated from MVPA to inactivity (β = −4.16 [−8.39, 0.07]).
There were no association between any of the movement behaviours and overall HRQoL, emotional well-being, relationship with family, and school functioning; displacing time between the movement behaviours did not influence these outcome variables (Table 3).
Prospective associations between movement behaviours and HRQoL
Prospectively, inactivity was associated with poorer overall HRQoL (β = −10.00 [−19.13, −0.87]), relationship with friends (β = −16.41 [−31.60, −1.23]), and school functioning (β = −15.30 [−29.16, −1.44]), while sleep showed a positive trend with overall HRQoL (β = 10.76 [−1.09, 22.61]) and school functioning (β = 17.12 [−0.87, 35.10]). There were no associations between the movement behaviours and the domains of HRQoL relating to physical and emotional well-being, self-esteem, and relationship with family, though the direction of associations suggested that sleep and inactivity were consistently associated with better and poorer overall HRQoL and all HRQoL domains, respectively. LPA and MVPA were not associated with overall HRQoL and any of the HRQoL domains (Table 4).
Table 4.
Compositional time use at age 8 years and its association with HRQoL.
| Overall HRQoL | Physical well-being | Emotional well-being | Self-esteem | Relationship with family | Relationship with friends | School functioning | |
|---|---|---|---|---|---|---|---|
| Sleep | 10.76 (−1.09, 22.61) (p = 0.075) | 8.87 (−4.84, 22.58) (p = 0.204) | 4.42 (−10.67, 19.52) (p = 0.565) | 8.83 (−12.55, 30.22) (p = 0.417) | 10.73 (−5.52, 26.99) (p = 0.195) | 14.57 (−5.13, 34.28) (p = 0.147) | 17.12 (−0.87, 35.10) (p = 0.062) |
| Inactivity | −10.00 (−19.13, −0.87) (p = 0.032) | −8.87 (−19.44, 1.69) (p = 0.100) | −5.95 (−17.59, 5.68) (p = 0.315) | −6.34 (−22.82, 10.14) (p = 0.450) | −7.13 (−19.66, 5.39) (p = 0.264) | −16.41 (−31.60, −1.23) (p = 0.034) | −15.30 (−29.16, −1.44) (p = 0.031) |
| LPA | −0.41 (−8.89, 8.06) (p = 0.923) | −1.21 (−11.02, 8.59) (p = 0.808) | 0.23 (−10.57, 11.04) (p = 0.966) | −0.25 (−15.55, 15.05) (p = 0.974) | −0.67 (−12.30, 10.96) (p = 0.910) | −1.71 (−15.80, 12.39) (p = 0.812) | 1.12 (−11.75, 13.99) (p = 0.864) |
| MVPA | −0.34 (−4.76, 4.08) (p = 0.879) | 1.22 (−3.90, 6.33) (p = 0.640) | 1.29 (−4.34, 6.92) (p = 0.652) | −2.24 (−10.22, 5.74) (p = 0.581) | −2.93 (−9.00, 3.13) (p = 0.342) | 3.54 (−3.81, 10.89) (p = 0.344) | −2.94 (−9.65, 3.77) (p = 0.390) |
Analysis performed using multivariable linear regression models; results presented as β (95% confidence intervals). Models were adjusted for sex, ethnicity, maternal education level, child's categorical weight status at age 8 years, and whether the participant was followed up before or after the onset of the COVID-19 pandemic.
Abbreviations: light intensity physical activity (LPA), moderate-to-vigorous intensity physical activity (MVPA), health-related quality of life (HRQoL).
Isotemporal substitution analyses suggested that increasing sleep at the expense of inactivity may be associated with better overall HRQoL (β = 1.04 [0.05, 2.03]), school functioning (β = 1.62 [0.12, 3.13]), and possibly relationship with friends (β = 1.56 [−0.09, 3.21]). The inverse was observed for overall HRQoL (β = −1.04 [−2.03, −0.04]), school functioning (β = −1.62 [−3.14, −0.11]) and possibly relationship with friends (β = −1.55 [−3.21, 0.11]) when inactivity was increased at the expense of sleep (Table 5).
Table 5.
Reallocation of 30 min between pairs of movement behaviours at age 8 years and the predicted change in HRQoL scores at age 10 years (95% confidence intervals).
| Overall HRQoL | Physical well-being | Emotional well-being | Self-esteem | Relationship with family | Relationship with friends | School functioning | |
|---|---|---|---|---|---|---|---|
| Increase sleep | |||||||
| Reduce inactivity | 1.04 (0.05, 2.03) (p = 0.040) | 0.89 (−0.26, 2.04) (p = 0.128) | 0.52 (−0.74, 1.79) (p = 0.415) | 0.75 (−1.03, 2.54) (p = 0.407) | 0.89 (−0.47, 2.25) (p = 0.200) | 1.56 (−0.09, 3.21) (p = 0.064) | 1.62 (0.12, 3.13) (p = 0.035) |
| Reduce LPA | 0.55 (−0.52, 1.61) (p = 0.313) | 0.52 (−0.71, 1.75) (p = 0.405) | 0.19 (−1.16, 1.55) (p = 0.781) | 0.44 (−1.48, 2.36) (p = 0.652) | 0.57 (−0.89, 2.02) (p = 0.446) | 0.83 (−0.93, 2.60) (p = 0.355) | 0.72 (−0.89, 2.34) (p = 0.378) |
| Reduce MVPA | 0.69 (−1.78, 3.16) (p = 0.583) | −0.21 (−3.07, 2.65) (p = 0.886) | −0.46 (−3.60, 2.69) (p = 0.775) | 1.58 (−2.87, 6.04) (p = 0.486) | 2.03 (−1.36, 5.42) (p = 0.239) | −1.14 (−5.25, 2.96) (p = 0.585) | 2.34 (−1.41, 6.09) (p = 0.221) |
| Increase inactivity | |||||||
| Reduce sleep | −1.04 (−2.03, −0.04) (p = 0.041) | −0.89 (−2.04, 0.26) (p = 0.131) | −0.52 (−1.79 0.75) (p = 0.422) | −0.76 (−2.56, 1.04) (p = 0.406) | −0.90 (−2.26, 0.47) (p = 0.199) | −1.55 (−3.21, 0.11) (p = 0.067) | −1.62 (−3.14, −0.11) (p = 0.036) |
| Reduce LPA | −0.46 (−1.33, 0.40) (p = 0.293) | −0.34 (−1.34, 0.66) (p = 0.502) | −0.31 (−1.42, 0.79) (p = 0.575) | −0.29 (−1.86, 1.27) (p = 0.711) | −0.30 (−1.49, 0.89) (p = 0.620) | −0.68 (−2.12, 0.76) (p = 0.356) | −0.85 (−2.16, 0.46) (p = 0.204) |
| Reduce MVPA | −0.32 (−2.53, 1.89) (p = 0.777) | −1.07 (−3.63, 1.48) (p = 0.410) | −0.96 (−3.78, 1.85) (p = 0.501) | 0.85 (−3.14, 4.83) (p = 0.677) | 1.16 (−1.86, 4.19) (p = 0.450) | −2.65 (−6.32, 1.02) (p = 0.157) | 0.76 (−2.59, 4.11) (p = 0.655) |
| Increase LPA | |||||||
| Reduce sleep | −0.57 (−1.61, 0.47) (p = 0.279) | −0.54 (−1.74, 0.66) (p = 0.380) | −0.21 (−1.53, 1.12) (p = 0.760) | −0.46 (−2.34, 1.41) (p = 0.627) | −0.59 (−2.02, 0.83) (p = 0.416) | −0.86 (−2.59, 0.87) (p = 0.327) | −0.78 (−2.36, 0.80) (p = 0.332) |
| Reduce inactivity | 0.50 (−0.34, 1.33) (p = 0.242) | 0.38 (−0.59, 1.34) (p = 0.442) | 0.33 (−0.73, 1.39) (p = 0.540) | 0.32 (−1.19, 1.82) (p = 0.680) | 0.33 (−0.82, 1.47) (p = 0.575) | 0.74 (−0.65, 2.12) (p = 0.296) | 0.89 (−0.38, 2.15) (p = 0.168) |
| Reduce MVPA | 0.15 (−2.53, 2.82) (p = 0.914) | −0.72 (−3.82, 2.38) (p = 0.647) | −0.65 (−4.06, 2.76) (p = 0.707) | 1.14 (−3.69, 5.97) (p = 0.642) | 1.47 (−2.20, 5.14) (p = 0.432) | −1.96 (−6.41, 2.49) (p = 0.386) | 1.61 (−2.46, 5.67) (p = 0.438) |
| Increase MVPA | |||||||
| Reduce sleep | −0.65 (−2.31, 1.00) (p = 0.438) | −0.05 (−1.97, 1.86) (p = 0.955) | 0.19 (−1.91, 2.30) (p = 0.857) | −1.17 (−4.15, 1.82) (p = 0.442) | −1.48 (−3.75, 0.78) (p = 0.199) | 0.41 (−2.34, 3.16) (p = 0.772) | −1.81 (−4.32, 0.70) (p = 0.157) |
| Reduce inactivity | 0.42 (−0.95, 1.79) (p = 0.550) | 0.86 (−0.73, 2.45) (p = 0.287) | 0.73 (−1.02, 2.48) (p = 0.412) | −0.39 (−2.86, 2.09) (p = 0.758) | −0.57 (−2.45, 1.31) (p = 0.553) | 2.01 (−0.27, 4.29) (p = 0.084) | −0.14 (−2.22, 1.94) (p = 0.895) |
| Reduce LPA | −0.08 (−1.96, 1.80) (p = 0.936) | 0.49 (−1.68, 2.67) (p = 0.658) | 0.40 (−2.00, 2.79) (p = 0.745) | −0.70 (−4.10, 2.69) (p = 0.685) | −0.89 (−3.47, 1.69) (p = 0.498) | 1.28 (−1.85, 4.41) (p = 0.422) | −1.04 (−3.89, 1.82) (p = 0.475) |
Results are interpreted as the difference in HRQoL when time spent in one behaviour is increased at the expense of another, while the remaining two behaviours remain constant.
Analysis performed using multivariate linear regression models, results presented as the predicted changes in HRQoL scores at age 10 years and their 95% confidence intervals reported within the brackets. Models were adjusted for sex, ethnicity, maternal education level, child's categorical weight status at age 8 years, and whether the participant was followed up before or after the onset of the COVID-19 pandemic.
Abbreviations: light intensity physical activity (LPA), moderate-to-vigorous intensity physical activity (MVPA), health-related quality of life (HRQoL).
Displacing time between the movement behaviours did not influence physical well-being, emotional well-being, self-esteem, and relationship with family (Table 5).
Discussion
Our study is, to our knowledge, the first to examine the cross-sectional and prospective associations between the full movement spectrum of children and their overall and domain specific HRQoL. We utilised objectively assessed movement behaviour data and self-reported HRQoL data from a sample of Asian children to better understand the complex relationships between children's movement behaviours and HRQoL. We provide early evidence that certain behaviours may be associated with specific aspects of HRQoL, wherein some relationships emerged cross-sectionally and others prospectively. Generally, our findings suggest that greater sleep and physical activity may be associated with better HRQoL (overall and/or domain-specific scores), while spending more time in inactivity may be associated with poorer HRQoL. Isotemporal substitution analyses were in line with these findings, where HRQoL scores was observed to increase when sleep and/or physical activity displaced inactivity.
In the present study, we found that cross-sectionally, LPA and MVPA were associated with better self-esteem and relationship with friends respectively. To further contextualise these findings, our isotemporal substitution analyses revealed that while the magnitude of differences were small, increasing LPA at the expense of sleep was associated with better self-esteem, with the inverse observed when sleep displaced LPA; LPA displacing or being displaced by inactivity or MVPA did not influence self-esteem scores. On the other hand, increasing MVPA, regardless at the expense of sleep, inactivity, or LPA, was associated with better relationship with friends; an inverse, exponential, and non-symmetrical relationship was observed when MVPA was displaced. The asymmetrical trend observed for MVPA is in line with previous studies among children of a similar age group,11,47 which may be attributed to already suboptimal MVPA durations in children,48,49 whereby further reducing time in MVPA could exacerbate the outcomes (e.g., relationship with friends in the present sample) associated with low MVPA. Our findings support current evidence, with associations between physical activity and various measures of self-esteem and psychosocial well-being widely reported. The association between physical activity and better self-esteem (and its constructs such as self-worth and self-concept)50, 51, 52 may be explained by physical activity contributing to the mastery of one's physique and perception of their physical appearance (i.e., body image).12 Physical activity also provides opportunities for socialisation,12 promotes social skills,53 reduces feelings of social isolation,54 and increases perceived social acceptance,55 all of which are associated with better psychosocial outcomes including social relationships.56 However, we note that associations in the present study were only observed for either physical activity intensity (i.e., either LPA or MVPA and not both). We postulate that there were differing contexts for the light and moderate-to-vigorous intensity physical activities among children in the present study (e.g., active transport, active play, organised sport), contributing to the difference in HRQoL domains associated with these behaviours. Contextual information regarding physical activity was not examined in the present study and should be explored in future research. The intensity of these activities (i.e., light or moderate-to-vigorous) may also differentially influence HRQoL through different neurological pathways, which to date has not been well investigated and warrants further research. We also note that we only observed these associations cross-sectionally and not prospectively, limiting causal inference. This suggests that the relationships may be bidirectional, whereby children with higher self-esteem and better relationship with their friends may instead be more inclined to partake in physical activity.57
To our knowledge, there has not been a prospective or longitudinal study that investigated all four movement behaviours in relation to HRQoL whilst properly accounting for the interrelatedness of the movement behaviours. We bridged this gap by analysing prospectively and found that sleep may be associated with better overall HRQoL and school functioning, while inactivity was associated with poorer overall HRQoL, relationship with friends, and school functioning. While the magnitude of differences in HRQoL scores when 30 min were displaced between the behaviours were small, increasing sleep at the expense of inactivity may benefit overall HRQoL, relationship with friends, and school functioning, with an inversed relationship of similar magnitude observed when inactivity displaced sleep. Current published evidence suggests that sleep may be associated with overall HRQoL, mood and emotional regulation, which could be postulated to influence social relationships and academic performance.14,15,58, 59, 60 These would explain our observations that when sleep was displaced, there was a negative impact on these HRQoL domains and consequentially, overall HRQoL scores. However, existing studies, including the present, have only assessed total sleep duration without considering other sleep dimensions such as sleep disturbances, patterns and quality, that could drive associations between sleep and HRQoL,11,28,61 warranting future studies to examine the role of these dimensions in children's HRQoL more deeply.62
Interestingly, we identified that HRQoL is impacted only when inactivity (and not LPA or MVPA) displaced sleep. Though we did not examine the context of the activities children engaged in, we postulate that these associations could be driven by screen-viewing, which are typically sedentary in nature.63 Studies have found screen-viewing to be associated with poorer overall HRQoL, including HRQoL domains relating to children's physical, psychosocial, mental, emotional, and/or school functioning,10 cross-sectionally64 and prospectively.57,65, 66, 67 Further, night-time screen-viewing has been associated with poorer sleep and HRQoL among children.68 Hence, the associations observed between inactivity and HRQoL in the present study may be attributed to screen-viewing during periods of inactivity. It is worth noting that these associations were only observed prospectively and not cross-sectionally, and the magnitudes of these associations were small. As we did not collect HRQoL information from children at the “baseline” of the present study (i.e., age 8 years), our ability to control for baseline HRQoL when assessing prospective relationships was limited. Findings therefore warrant cautious interpretation and confirmation by future research.
Other than the aforementioned findings, we did not observe any other association between the movement behaviours and HRQoL (overall and/or domain-specific scores). Notably, physical activity (i.e., LPA and MVPA) was not associated with overall HRQoL, and none of the four movement behaviours were associated with physical well-being, emotional well-being, and relationship with family, both cross-sectionally and prospectively. Engagement in physical activity has been thought to improve physical well-being, improve mood, and reduce symptoms associated with depression and anxiety.12,69 However, findings on associations between physical activity and HRQoL have been equivocal, with some studies demonstrating a positive association and others none.10,13,70 Even among studies that have found an association between physical activity and HRQoL, the beta coefficients often do not reach a minimally important difference.13 Hence, more research is warranted to confirm associations and/or establish causal relationships between physical activity and HRQoL in children.
Regarding sleep, though previous studies have found that sleep was associated with better HRQoL,71,72 these studies are sparse, with limited discussion on specific HRQoL domains such as physical or emotional well-being, or on the mechanisms underlying the associations.60 Previous studies have also suggested that sleep may be associated with children's relationship with their family. Poor family relationships (e.g., marital conflicts, family conflicts) were found to influence children's sleep, in particular, their sleep quality,73 while secure parent–child relationships were associated with better sleep.74 We did not observe significant associations between sleep and these HRQoL domains in the present study, which may be attributed to suboptimal sleep durations of children in our sample. In an earlier study of children in the same cohort, only a small proportion of children aged 8 years met the recommended sleep duration (9–11 h).23 We postulate that children in our study sample (at both age 8 and 10 years) may not have achieved sufficient sleep to manifest positive impacts on these aspects of their HRQoL. Further, we did not consider other dimensions of sleep beyond duration in the present analyses, warranting future studies to bridge these knowledge gaps to enhance understanding of associations between sleep and HRQoL in children.
In relation to inactivity, previous studies have largely found inactivity (or sedentary behaviour) to be associated with poorer HRQoL in children, including physical and emotional well-being,10,75 which we did not confirm. However, it is worth noting that these studies typically assessed screen-viewing behaviours as proxy for inactivity, which cannot be assessed objectively, and may not necessarily corroborate with total inactivity time. In the present analysis, we did not review screen-viewing as a component of children's 24-h time use as the four behaviours examined were mutually exclusive parts of a 24-h day25 and screen-viewing would overlap with one or possibly more than one behaviour (e.g., inactivity and/or LPA such as using screen-based devices while walking), complicating the compositional data analysis technique implemented. Future research examining children's movement behaviours and HRQoL should explore accounting for screen-viewing duration and the context of screen-viewing behaviours in their analyses.
We also wish to highlight that differences in our findings compared to other studies may also be attributed to other factors that could have had bigger, more direct impacts on the HRQoL of children in our sample compared to their movement behaviours. In an earlier study among children aged 10–15 years in Singapore, ethnicity was found to be associated with children's HRQoL, with Malay children reporting lower HRQoL than their Chinese and Indian counterparts.8 Previous studies examining the relationship between HRQoL and movement behaviours of children were largely conducted in homogenous samples.11,28 In multi-cultural populations like Singapore, ethnic differences could play an important role in children's HRQoL, attenuating the role of movement behaviours in this relationship. Other factors including sex and SES may also influence children's movement behaviours and/or perceptions of their well-being.8 Future studies investigating other factors influencing the associations between children's movement behaviours and their HRQoL, particularly in non-homogenous samples are therefore warranted.
The present study has several strengths. We assessed children's movement behaviours using accelerometers, reducing the risk of bias by allowing high quality data across the full continuum of movement behaviours to be objectively collected. To the best of our knowledge, our study is the first to date to have examined the prospective associations between all four movement behaviours and HRQoL and HRQoL domains, allowing us to ascertain temporality of the observed relationships. Further, we implemented compositional data analysis techniques to fully account for the interrelatedness of the movement behaviours in our analyses.11,40 These strengthened our conclusions regarding children's movement behaviours and their HRQoL—our findings were largely in line with literature in that physical activity and sleep were associated with better HRQoL, while inactivity was associated with poorer HRQoL. However, we also revealed that the relationships between children's movement behaviours and HRQoL were complex and that conclusions, at least in the present sample, could not be easily made. Notwithstanding, our findings contribute to current understanding of the relationships between children's movement behaviours and their HRQoL, especially in the less studied Asian context, and form the basis from which future research can be undertaken.
We acknowledge several limitations of our research. The magnitudes of some associations discussed were small with wide 95% confidence intervals, attributing to the modest sample size and variability within our sample. Further, should one account for multiple testing (e.g., via Bonferroni correction), most of the observed associations may no longer be statistically significant, suggesting that the observed associations may be attributed to chance. Future research with larger sample sizes to obtain more precise estimates and to strengthen the robustness of the conclusions is warranted. The use of accelerometery for movement data collection meant that information on the context of activities such as location, type of activity (e.g., screen-viewing, organised sport, active transport), and other dimensions of sleep which may have had important implications on HRQoL could not be distinguished, limiting our ability to examine and discuss the influences of these qualitative aspects of movement behaviours on HRQoL. In addition, the classification of the movement behaviours in the present study was algorithm-driven, which could not always differentiate sleep-related behaviours that were neither sleep nor inactivity (e.g., sleep onset latency, night awakenings).76 As such, true periods of inactivity that were hypothesised to be associated with poorer HRQoL could be overestimated in the present study, undermining our conclusions. Future studies could consider complementing objective assessments of movement behaviour with subjective types to capture the qualitative aspects of sleep to provide more context to the observed associations (or lack thereof) between movement behaviours and HRQoL. While the KINDL-Kid questionnaire was previously validated in the local context,39 it was recommended for only the overall and not domain-specific scores to be interpreted as only the overall score demonstrated good internal consistency. Notwithstanding, we presented both overall and domain-specific HRQoL scores to provide insights on the potential associations between the movement behaviours and overall HRQoL and specific HRQoL domains. We also acknowledge that the children of the GUSTO cohort were followed up at age 10 years in unique times that coincided with the onset of the COVID-19 pandemic, which may have influenced our findings. COVID-19 may have impacted children's HRQoL negatively such as increased feelings of loneliness and isolation, wherein effects are disproportional for different social groups (e.g., those of lower socio-economic positions).77,78 Further, the pandemic may also impact children's movement behaviours through restrictions that vary over time (e.g., full versus partial lockdown and the gradual transition towards endemic COVID-19).79 We adjusted for this by accounting for whether the participants were followed up before or after the onset of the pandemic, but this measure is limited in measuring behavioural changes caused by the pandemic and we cannot rule out residual confounding. Finally, although included and excluded participants of the present study did not differ significantly in characteristics (Supplementary Table S1), the overall GUSTO cohort is not representative of the Singapore population.31 As such, our findings should be extrapolated to the Singapore or other general population with caution.
Conclusion
Our study is novel in that it is, to our knowledge, the first that examined the cross-sectional and prospective associations between the full movement spectrum of children and their overall and domain specific HRQoL, in the less studied Asian population. Generally, we suggest that sleep and physical activity may be associated with better HRQoL, while inactivity may be associated with poorer HRQoL. However, our findings also demonstrated the complexity of the relationship between children's movement behaviours and HRQoL, highlighting the need for further research.
Contributors
Authorship: MF-FC and FMR designed the research; YSC, KMG, KHT, and JGE designed and led the GUSTO study; JYT and NP conducted research and/or collected the GUSTO data; SYXT performed the statistical analysis with guidance from JYB, CST, and FMR; SYXT drafted the manuscript; NP, JYB, CST, MF-FC, and FMR critically reviewed the manuscript; all authors read and approved the final manuscript.
Declaration of interests
KMG reports being part of an academic consortium that has received research funding from Nestle Research, unrelated to the present manuscript. JYB is supported by a grant from the Agence Nationale de la Recherche (ANR) (iSCAN project, ANR-20-CE36-0001).
Acknowledgements
The authors thank the participants of the GUSTO study, staff involved in the data collection and management, and the GUSTO study group.
Funding: The study is supported by the National Research Foundation (NRF) under the Open Fund-Large Collaborative Grant (OF-LCG; MOH-000504) administered by the Singapore Ministry of Health's National Medical Research Council (NMRC) and the Agency for Science, Technology and Research (ASTAR). In RIE2025, GUSTO is supported by funding from the NRF's Human Health and Potential (HHP) Domain, under the Human Potential Programme.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2023.100918.
Appendix A. Supplementary data
References
- 1.World Health Organization . 2006. Constitution of the world health organization. [Google Scholar]
- 2.Matza L.S., Swensen A.R., Flood E.M., Secnik K., Leidy N.K. Assessment of health-related quality of life in children: a review of conceptual, methodological, and regulatory issues. Value Health. 2004;7(1):79–92. doi: 10.1111/j.1524-4733.2004.71273.x. [DOI] [PubMed] [Google Scholar]
- 3.World Health Organization Sustainable Development Goals. https://www.who.int/health-topics/sustainable-development-goals#tab=tab_1 Available from:
- 4.Centers for Disease Control and Prevention HRQOL Concepts 2016. https://www.cdc.gov/hrqol/concept.htm Available from:
- 5.Phyo A.Z.Z., Freak-Poli R., Craig H., et al. Quality of life and mortality in the general population: a systematic review and meta-analysis. BMC Public Health. 2020;20:1–20. doi: 10.1186/s12889-020-09639-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Health Promotion Board NurtureSG action plan report. https://www.hpb.gov.sg/docs/default-source/default-document-library/nurturesg-action-plan-report.pdf?sfvrsn=460f572_0 Available from:
- 7.Meyer M., Oberhoffer R., Hock J., Giegerich T., Müller J. Health-related quality of life in children and adolescents: current normative data, determinants and reliability on proxy-report. J Paediatr Child Health. 2016;52(6):628–631. doi: 10.1111/jpc.13166. [DOI] [PubMed] [Google Scholar]
- 8.Ng T.P., Lim L.C.C., Jin A., Shinfuku N. Ethnic differences in quality of life in adolescents among Chinese, Malay and Indians in Singapore. Qual Life Res. 2005;14(7):1755–1768. doi: 10.1007/s11136-005-1741-2. [DOI] [PubMed] [Google Scholar]
- 9.Bolton K., Kremer P., Rossthorn N., et al. The effect of gender and age on the association between weight status and health-related quality of life in Australian adolescents. BMC Public Health. 2014;14(1):1–8. doi: 10.1186/1471-2458-14-898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wu X.Y., Han L.H., Zhang J.H., Luo S., Hu J.W., Sun K. The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: a systematic review. PLoS One. 2017;12(11) doi: 10.1371/journal.pone.0187668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Dumuid D., Maher C., Lewis L.K., et al. Human development index, children's health-related quality of life and movement behaviors: a compositional data analysis. Qual Life Res. 2018;27(6):1473–1482. doi: 10.1007/s11136-018-1791-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lubans D., Richards J., Hillman C., et al. Physical activity for cognitive and mental health in youth: a systematic review of mechanisms. Pediatrics. 2016;138(3) doi: 10.1542/peds.2016-1642. [DOI] [PubMed] [Google Scholar]
- 13.Marker A.M., Steele R.G., Noser A.E. Physical activity and health-related quality of life in children and adolescents: a systematic review and meta-analysis. Health Psychol. 2018;37(10):893. doi: 10.1037/hea0000653. [DOI] [PubMed] [Google Scholar]
- 14.Short M.A., Bartel K., Carskadon M.A. Sleep and mental health in children and adolescents. Sleep Health. 2019:435–445. [Google Scholar]
- 15.Gregory A.M., Sadeh A. Sleep, emotional and behavioral difficulties in children and adolescents. Sleep Med Rev. 2012;16(2):129–136. doi: 10.1016/j.smrv.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 16.Sampasa-Kanyinga H., Standage M., Tremblay M.S., et al. Associations between meeting combinations of 24-h movement guidelines and health-related quality of life in children from 12 countries. Public Health. 2017;153:16–24. doi: 10.1016/j.puhe.2017.07.010. [DOI] [PubMed] [Google Scholar]
- 17.Haerens L., Vereecken C., Maes L., De Bourdeaudhuij I. Relationship of physical activity and dietary habits with body mass index in the transition from childhood to adolescence: a 4-year longitudinal study. Public Health Nutr. 2010;13(10A):1722–1728. doi: 10.1017/S1368980010002284. [DOI] [PubMed] [Google Scholar]
- 18.Leech R., McNaughton S., Timperio A. Clustering of diet, physical activity and sedentary behaviour among Australian children: cross-sectional and longitudinal associations with overweight and obesity. Int J Obes. 2015;39(7):1079–1085. doi: 10.1038/ijo.2015.66. [DOI] [PubMed] [Google Scholar]
- 19.Corder K., Sharp S.J., Atkin A.J., et al. Change in objectively measured physical activity during the transition to adolescence. Br J Sports Med. 2015;49(11):730–736. doi: 10.1136/bjsports-2013-093190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thomas G., Bennie J.A., De Cocker K., Ireland M.J., Biddle S.J. Screen-based behaviors in Australian adolescents: longitudinal trends from a 4-year follow-up study. Prev Med. 2020;141 doi: 10.1016/j.ypmed.2020.106258. [DOI] [PubMed] [Google Scholar]
- 21.Belmon L.S., van Stralen M.M., Busch V., Harmsen I.A., Chinapaw M.J. What are the determinants of children's sleep behavior? A systematic review of longitudinal studies. Sleep Med Rev. 2019;43:60–70. doi: 10.1016/j.smrv.2018.09.007. [DOI] [PubMed] [Google Scholar]
- 22.Spear H.J., Kulbok P. Autonomy and adolescence: a concept analysis. Public Health Nurs. 2004;21(2):144–152. doi: 10.1111/j.0737-1209.2004.021208.x. [DOI] [PubMed] [Google Scholar]
- 23.Padmapriya N., Chen B., Goh C.M.J.L., et al. 24-hour movement behaviour profiles and their transition in children aged 5.5 and 8 years–findings from a prospective cohort study. Int J Behav Nutr Phys Activ. 2021;18(1):1–14. doi: 10.1186/s12966-021-01210-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Khan A., Lee E.Y., Tremblay M.S. Meeting 24-h movement guidelines and associations with health related quality of life of Australian adolescents. J Sci Med Sport. 2021;24(5):468–473. doi: 10.1016/j.jsams.2020.10.017. [DOI] [PubMed] [Google Scholar]
- 25.Dumuid D., Pedišić Ž., Palarea-Albaladejo J., Martín-Fernández J.A., Hron K., Olds T. Compositional data analysis in time-use epidemiology: what, why, how. Int J Environ Res Public Health. 2020;17(7):2220. doi: 10.3390/ijerph17072220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pedišić Ž., Dumuid D., S Olds T. Integrating sleep, sedentary behaviour, and physical activity research in the emerging field of time-use epidemiology: definitions, concepts, statistical methods, theoretical framework, and future directions. Kinesiol. 2017;49(2):252–269. [Google Scholar]
- 27.Chaput J.-P., Willumsen J., Bull F., et al. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5–17 years: summary of the evidence. Int J Behav Nutr Phys Activ. 2020;17(1):141. doi: 10.1186/s12966-020-01037-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tsiros M.D., Samaras M.G., Coates A.M., Olds T. Use-of-time and health-related quality of life in 10-to 13-year-old children: not all screen time or physical activity minutes are the same. Qual Life Res. 2017;26(11):3119–3129. doi: 10.1007/s11136-017-1639-9. [DOI] [PubMed] [Google Scholar]
- 29.Rees G., Dinisman T. Comparing children's experiences and evaluations of their lives in 11 different countries. Child Indicat Res. 2015;8(1):5–31. [Google Scholar]
- 30.Rapley M. Sage; 2003. Quality of life research: a critical introduction. [Google Scholar]
- 31.Soh S.-E., Tint M.T., Gluckman P.D., et al. Cohort profile: Growing up in Singapore Towards healthy Outcomes (GUSTO) birth cohort study. Int J Epidemiol. 2014;43(5):1401–1409. doi: 10.1093/ije/dyt125. [DOI] [PubMed] [Google Scholar]
- 32.HealthHub Did You Know BMI Isn’t The Same For Adults And Kids? 2022. https://www.healthhub.sg/live-healthy/745/differencesbetweenchildandadultbmi Available from:
- 33.Tan S.Y.X., Chia A., Tai B.C., et al. A web-based, time-use app to assess children's movement behaviors: validation study of my E-diary for activities and lifestyle (MEDAL) JMIR Pediatr Parent. 2022;5(2) doi: 10.2196/33312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sabia S.P., Cogranne P.B., van Hees V.T.P., et al. Physical activity and adiposity markers at older ages: accelerometer vs questionnaire data. J Am Med Dir Assoc. 2015;16(5):438.e7–438.e13. doi: 10.1016/j.jamda.2015.01.086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.van Hees V.T., Sabia S., Anderson K.N., et al. A novel, open access method to assess sleep duration using a wrist-worn accelerometer. PLoS One. 2015;10(11) doi: 10.1371/journal.pone.0142533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hildebrand M., VANH V.T., Hansen B.H., Ekelund U. Age group comparability of raw accelerometer output from wrist- and hip-worn monitors. Med Sci Sports Exerc. 2014;46(9):1816–1824. doi: 10.1249/MSS.0000000000000289. [DOI] [PubMed] [Google Scholar]
- 37.Hildebrand M., Hansen B.H., van Hees V.T., Ekelund U. Evaluation of raw acceleration sedentary thresholds in children and adults. Scand J Med Sci Sports. 2017;27(12):1814–1823. doi: 10.1111/sms.12795. [DOI] [PubMed] [Google Scholar]
- 38.Tremblay M.S., Aubert S., Barnes J.D., et al. Sedentary behavior research network (SBRN)–terminology consensus project process and outcome. Int J Behav Nutr Phys Activ. 2017;14(1):75. doi: 10.1186/s12966-017-0525-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wee H.-L., Ravens-Sieberer U., Erhart M., Li S.-C. Factor structure of the Singapore English version of the KINDL® children quality of life questionnaire. Health Qual Life Outcomes. 2007;5(1):1–8. doi: 10.1186/1477-7525-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dumuid D., Stanford T.E., Martin-Fernández J.-A., et al. Compositional data analysis for physical activity, sedentary time and sleep research. Stat Methods Med Res. 2018;27(12):3726–3738. doi: 10.1177/0962280217710835. [DOI] [PubMed] [Google Scholar]
- 41.Egozcue J.J., Pawlowsky-Glahn V. Groups of parts and their balances in compositional data analysis. Math Geol. 2005;37(7):795–828. [Google Scholar]
- 42.Dumuid D., Stanford T.E., Pedišić Ž., et al. Adiposity and the isotemporal substitution of physical activity, sedentary time and sleep among school-aged children: a compositional data analysis approach. BMC Public Health. 2018;18(1):1–10. doi: 10.1186/s12889-018-5207-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Van den Boogaart K.G., Tolosana-Delgado R. “Compositions”: a unified R package to analyze compositional data. Comput Geosci. 2008;34(4):320–338. [Google Scholar]
- 44.Templ M., Hron K., Filzmoser P. 2011. robCompositions: an R-package for robust statistical analysis of compositional data. Compositional data analysis: theory and applications; pp. 341–355. [Google Scholar]
- 45.Hothorn T., Zeileis A., Farebrother R.W., et al. Package ‘lmtest’. Testing linear regression models. https://cran.r-project.org/web/packages/lmtest/lmtest pdf 2015;6.
- 46.Fox J. 2009. Car: companion to applied regression. R package version 1.2-16.http://CRAN.R-project.org/package=car [Google Scholar]
- 47.Carson V., Tremblay M.S., Chaput J.-P., Chastin S.F. Associations between sleep duration, sedentary time, physical activity, and health indicators among Canadian children and youth using compositional analyses. Appl Physiol Nutr Metabol. 2016;41(6):S294–S302. doi: 10.1139/apnm-2016-0026. [DOI] [PubMed] [Google Scholar]
- 48.Aubert S., Barnes J.D., Abdeta C., et al. Global matrix 3.0 physical activity report card grades for children and youth: results and analysis from 49 countries. J Phys Activ Health. 2018;15(s2):S251–S273. doi: 10.1123/jpah.2018-0472. [DOI] [PubMed] [Google Scholar]
- 49.Müller A.M., Khoo S., Lambert R. Review of physical activity prevalence of Asian school-age children and adolescents. Asia Pac J Public Health. 2013;25(3):227–238. doi: 10.1177/1010539513481494. [DOI] [PubMed] [Google Scholar]
- 50.Dale L.P., Vanderloo L., Moore S., Faulkner G. Physical activity and depression, anxiety, and self-esteem in children and youth: an umbrella systematic review. Ment Health Phys Activ. 2019;16:66–79. [Google Scholar]
- 51.Liu M., Wu L., Ming Q. How does physical activity intervention improve self-esteem and self-concept in children and adolescents? Evidence from a meta-analysis. PLoS One. 2015;10(8) doi: 10.1371/journal.pone.0134804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Ekeland E., Heian F., Hagen K.B. Can exercise improve self esteem in children and young people? A systematic review of randomised controlled trials. Br J Sports Med. 2005;39(11):792–798. doi: 10.1136/bjsm.2004.017707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Howie L.D., Lukacs S.L., Pastor P.N., Reuben C.A., Mendola P. Participation in activities outside of school hours in relation to problem behavior and social skills in middle childhood. J Sch Health. 2010;80(3):119–125. doi: 10.1111/j.1746-1561.2009.00475.x. [DOI] [PubMed] [Google Scholar]
- 54.Barber B.L., Eccles J.S., Stone M.R. Whatever happened to the jock, the brain, and the princess? Young adult pathways linked to adolescent activity involvement and social identity. J Adolesc Res. 2001;16(5):429–455. [Google Scholar]
- 55.Boone E.M., Leadbeater B.J. Game on: diminishing risks for depressive symptoms in early adolescence through positive involvement in team sports. J Res Adolesc. 2006;16(1):79–90. [Google Scholar]
- 56.Eime R.M., Young J.A., Harvey J.T., Charity M.J., Payne W.R. A systematic review of the psychological and social benefits of participation in sport for children and adolescents: informing development of a conceptual model of health through sport. Int J Behav Nutr Phys Activ. 2013;10(1):1–21. doi: 10.1186/1479-5868-10-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Omorou A.Y., Langlois J., Lecomte E., Briançon S., Vuillemin A. Cumulative and bidirectional association of physical activity and sedentary behaviour with health-related quality of life in adolescents. Qual Life Res. 2016;25:1169–1178. doi: 10.1007/s11136-015-1172-7. [DOI] [PubMed] [Google Scholar]
- 58.Medic G., Wille M., Hemels M.E. Short-and long-term health consequences of sleep disruption. Nat Sci Sleep. 2017;9:151. doi: 10.2147/NSS.S134864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dewald J.F., Meijer A.M., Oort F.J., Kerkhof G.A., Bögels S.M. The influence of sleep quality, sleep duration and sleepiness on school performance in children and adolescents: a meta-analytic review. Sleep Med Rev. 2010;14(3):179–189. doi: 10.1016/j.smrv.2009.10.004. [DOI] [PubMed] [Google Scholar]
- 60.Chaput J.-P., Gray C.E., Poitras V.J., et al. Systematic review of the relationships between sleep duration and health indicators in school-aged children and youth. Appl Physiol Nutr Metabol. 2016;41(6):S266–S282. doi: 10.1139/apnm-2015-0627. [DOI] [PubMed] [Google Scholar]
- 61.Jalali-Farahani S., Amiri P., Chin Y.S. Are physical activity, sedentary behaviors and sleep duration associated with body mass index-for-age and health-related quality of life among high school boys and girls? Health Qual Life Outcomes. 2016;14:30. doi: 10.1186/s12955-016-0434-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jarrin D.C., McGrath J.J., Drake C.L. Beyond sleep duration: distinct sleep dimensions are associated with obesity in children and adolescents. Int J Obes. 2013;37(4):552–558. doi: 10.1038/ijo.2013.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Butte N.F., Watson K.B., Ridley K., et al. A youth compendium of physical activities: activity codes and metabolic intensities. Med Sci Sports Exerc. 2018;50(2):246–256. doi: 10.1249/MSS.0000000000001430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Finne E., Bucksch J., Lampert T., Kolip P. Physical activity and screen-based media use: cross-sectional associations with health-related quality of life and the role of body satisfaction in a representative sample of German adolescents. Health Psychol Behav Med. 2013;1(1):15–30. doi: 10.1080/21642850.2013.809313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Gopinath B., Louie J.C., Flood V.M., et al. Influence of obesogenic behaviors on health-related quality of life in adolescents. Asia Pac J Clin Nutr. 2014;23(1):121–127. doi: 10.6133/apjcn.2014.23.1.13. [DOI] [PubMed] [Google Scholar]
- 66.Gopinath B., Hardy L.L., Baur L.A., Burlutsky G., Mitchell P. Physical activity and sedentary behaviors and health-related quality of life in adolescents. Pediatrics. 2012;130(1):e167–e174. doi: 10.1542/peds.2011-3637. [DOI] [PubMed] [Google Scholar]
- 67.Chen X., Sekine M., Hamanishi S., Yamagami T., Kagamimori S. Associations of lifestyle factors with quality of life (QOL) in Japanese children: a 3-year follow-up of the Toyama Birth Cohort Study. Child Care Health Dev. 2005;31(4):433–439. doi: 10.1111/j.1365-2214.2005.00529.x. [DOI] [PubMed] [Google Scholar]
- 68.Mireku M.O., Barker M.M., Mutz J., et al. Night-time screen-based media device use and adolescents' sleep and health-related quality of life. Environ Int. 2019;124:66–78. doi: 10.1016/j.envint.2018.11.069. [DOI] [PubMed] [Google Scholar]
- 69.Penedo F.J., Dahn J.R. Exercise and well-being: a review of mental and physical health benefits associated with physical activity. Curr Opin Psychiatry. 2005;18(2):189–193. doi: 10.1097/00001504-200503000-00013. [DOI] [PubMed] [Google Scholar]
- 70.Marquez D.X., Aguiñaga S., Vásquez P.M., et al. A systematic review of physical activity and quality of life and well-being. Transl Behav Med. 2020;10(5):1098–1109. doi: 10.1093/tbm/ibz198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Perkinson-Gloor N., Lemola S., Grob A. Sleep duration, positive attitude toward life, and academic achievement: the role of daytime tiredness, behavioral persistence, and school start times. J Adolesc. 2013;36(2):311–318. doi: 10.1016/j.adolescence.2012.11.008. [DOI] [PubMed] [Google Scholar]
- 72.Do Y.K., Shin E., Bautista M.A., Foo K. The associations between self-reported sleep duration and adolescent health outcomes: what is the role of time spent on Internet use? Sleep Med. 2013;14(2):195–200. doi: 10.1016/j.sleep.2012.09.004. [DOI] [PubMed] [Google Scholar]
- 73.Johnson D.A., Billings M.E., Hale L. Environmental determinants of insufficient sleep and sleep disorders: implications for population health. Curr Epidemiol Rep. 2018;5(2):61–69. doi: 10.1007/s40471-018-0139-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Tu K.M., Marks B.T., El-Sheikh M. Sleep and mental health: the moderating role of perceived adolescent-parent attachment. Sleep Health. 2017;3(2):90–97. doi: 10.1016/j.sleh.2016.12.003. [DOI] [PubMed] [Google Scholar]
- 75.Zhang T., Lu G., Wu X.Y. Associations between physical activity, sedentary behaviour and self-rated health among the general population of children and adolescents: a systematic review and meta-analysis. BMC Public Health. 2020;20(1):1–16. doi: 10.1186/s12889-020-09447-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Barone Gibbs B., Kline C.E. When does sedentary behavior become sleep? A proposed framework for classifying activity during sleep-wake transitions. Int J Behav Nutr Phys Activ. 2018;15(1):1–4. doi: 10.1186/s12966-018-0712-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Nobari H., Fashi M., Eskandari A., Villafaina S., Murillo-Garcia Á, Pérez-Gómez J. Effect of COVID-19 on health-related quality of life in adolescents and children: a systematic review. Int J Environ Res Public Health. 2021;18(9):4563. doi: 10.3390/ijerph18094563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Ahn S.N. The potential impact of COVID-19 on health-related quality of life in children and adolescents: a systematic review. Int J Environ Res Public Health. 2022;19(22) doi: 10.3390/ijerph192214740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Paterson D.C., Ramage K., Moore S.A., Riazi N., Tremblay M.S., Faulkner G. Exploring the impact of COVID-19 on the movement behaviors of children and youth: a scoping review of evidence after the first year. J Sport Health Sci. 2021;10(6):675–689. doi: 10.1016/j.jshs.2021.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.