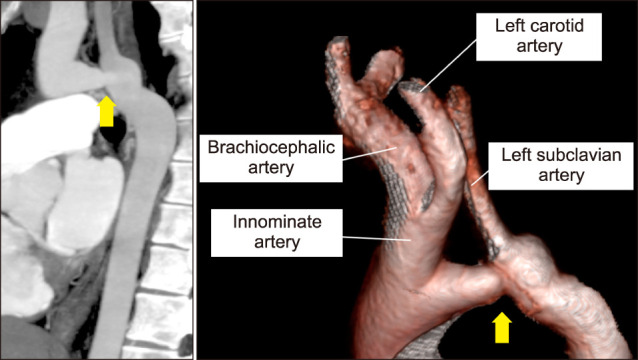
A 24-year-old man was presented to our hospital after a medical check-up revealed a chest murmur. Although previous medical check-ups noted a right-left difference in blood pressure (BP), it was considered normal because both BP values were within the normal range. He reported no symptoms, but a discrepancy in blood pressure was observed with readings of 123/77 mmHg and 98/71 mmHg on the right and left sides, respectively. A systolic murmur (Levine 2/6) was heard in the left margin of the second intercostal sternum and also in the left infrascapular region. The pulses in the left radial and femoral arteries were slightly weaker and delayed compared to the right radial artery. Electrocardiogram and echocardiography showed no abnormalities. To investigate the discrepancy in blood pressure and the murmur, we performed contrast-enhanced computed tomography (CT) scan, which revealed a bovine aortic arch and an aortic coarctation in the aortic arch (Fig. 1).
FIG. 1. Maximum intensity projection image on computed tomography shows coarctation of the aortic arch proximal to the left subclavian artery. The volume rendering image shows the common origin of the brachiocephalic artery and the left common carotid artery, also known as the bovine aortic arch.
Adult patients with coarctation of the aorta (CoA) are typically diagnosed clinically when they present with heart failure, hypertension, or a discrepancy in blood pressure between extremities.1,2 It is rare for CoA to be incidentally diagnosed during routine medical check-ups.2 Although the diagnosis of CoA in adult patients does not require complicated examination, the diagnosis is often delayed. In fact, patients who have been referred to the hospital because of a heart murmur are sometimes overlooked for CoA.3 Therefore, In CoA patients without symptoms, hypertension, blood pressure measurement, and pulse palpation in the extremities are important for the detection of CoA. If left untreated, the mean survival of patients with CoA is reduced to mid-adulthood due to long-term sequelae such as heart failure, endocarditis, aortic rupture or cerebrovascular hemorrhage.1 The treatment of CoA, such as surgery or balloon dilatation with stenting, is associated with lower risks of long-term morbidity and mortality.2 Therefore, we subsequently referred him to a hospital where he could undergo the necessary invasive treatment for CoA, and he underwent surgery at a later time.
Footnotes
CONFLICT OF INTEREST STATEMENT: None declared.
References
- 1.Dijkema EJ, Leiner T, Grotenhuis HB. Diagnosis, imaging and clinical management of aortic coarctation. Heart. 2017;103:1148–1155. doi: 10.1136/heartjnl-2017-311173. Erratum in: Heart 2019;105:e6. [DOI] [PubMed] [Google Scholar]
- 2.Alkashkari W, Albugami S, Hijazi ZM. Management of coarctation of the aorta in adult patients: state of the art. Korean Circ J. 2019;49:298–313. doi: 10.4070/kcj.2018.0433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Strafford MA, Griffiths SP, Gersony WM. Coarctation of the aorta: a study in delayed detection. Pediatrics. 1982;69:159–163. [PubMed] [Google Scholar]


