Key Points
Question
What factors are associated with caregiver-reported vision testing among adolescents in the US?
Findings
In this cross-sectional study of 24 752 US adolescents who participated in a nationally representative survey, approximately 1 in 4 adolescents did not receive vision testing within the previous 12 months. Vision testing was less frequently reported among adolescents who were older, male, or uninsured; had caregivers with less than high school education; and were from a family born outside the US.
Meaning
These findings suggest that efforts to expand the role of school-based vision testing for older adolescents from socioeconomically disadvantaged backgrounds may offer avenues to address existing disparities in untreated refractive error in this population.
Abstract
Importance
Untreated refractive error contributes to the racial, ethnic, and socioeconomic disparities in visual function of adolescent children in the US.
Objective
To describe patterns in vision testing as a function of age among US adolescents and identify sociodemographic factors associated with vision testing.
Design, Setting, and Participants
This cross-sectional study used data from the National Survey of Children’s Health (2018-2019), a nationally representative survey of the noninstitutionalized US pediatric population. A total of 24 752 adolescent children (aged 12 to <18 years) were included. Data were analyzed from March 22 to August 11, 2023.
Main Outcomes and Measures
The primary outcome was the caregiver report of vision testing within the last 12 months. Linear regression was used to describe the patterns in reported vision testing as a function of participant age. Logistic regression was used to describe the association of sociodemographic factors with the report of vision testing in each setting.
Results
Among 24 752 adolescents, the median (IQR) age was 14 (13-16) years; 12 918 (weighted, 51%) were male. Vision testing in any setting within the previous year was reported by caregivers of 18 621 adolescents (weighted, 74%). Vision testing was reported to have occurred at an eye clinic in 13 323 participants (weighted, 51%), at a primary care clinic in 5230 participants (weighted, 22%), at a school in 2594 participants (weighted, 11%), and at a health center in 635 participants (weighted, 4%). The percentage of adolescents reported to have vision tested decreased with age (−1.3% per year; 95% CI, −2.5% to 0% per year) due to a decrease in testing in primary care and school settings. After adjusting for age and sex, there were lower odds of vision testing reported for adolescents who were uninsured vs insured (adjusted odds ratio [AOR], 0.81; 95% CI, 0.76-0.87), had caregivers with less than vs greater than high school education (AOR, 0.89; 95% CI, 0.84-0.95), and were from a family born outside vs inside the US (AOR, 0.90; 95% CI, 0.82-0.98).
Conclusions and Relevance
In this cross-sectional study, vision testing in adolescents decreased as a function of age due to fewer reported tests performed in primary care and school-based settings. Relative to children in socioeconomically advantaged families, those from disadvantaged families were less likely to report receiving vision testing in clinical settings. Efforts to expand the role of school-based vision testing for older adolescents from disadvantaged backgrounds may enable opportunities to address disparities in untreated refractive error.
This cross-sectional study uses data from the National Survey of Children’s Health to describe patterns in vision testing as a function of age and identify sociodemographic factors associated with vision testing among US adolescents.
Introduction
Refractive error is the most common cause of visual impairment during adolescence.1 Untreated refractive error contributes to the racial, ethnic, and socioeconomic disparities in visual function of adolescent children in the US.2,3 Visual impairment may interfere with academic and social development and negatively impact future career trajectories.4,5,6 Vision testing can help identify individuals with ocular conditions such as untreated refractive error, amblyopia, and strabismus. However, few states have mandates for vision testing in adolescents compared with early school-aged children.7 The settings in which vision evaluations are performed, the patterns in vision testing as a function of age, and the sociodemographic factors associated with vision testing have not been described using a nationally representative cohort of US adolescents.
Methods
This cross-sectional study using deidentified data from the National Survey of Children’s Health (NSCH) was not considered human participants research by the Boston Children’s Hospital Institutional Review Board and was exempt from review. The study followed STROBE reporting guidelines.
The NSCH is a nationally representative annual survey of the noninstitutionalized US pediatric population.8 Children are selected to participate using stratified random sampling, and the caregiver most knowledgeable about the well-being of the child (ie, parent or other legal guardian) completes the survey (Supplement 1). We included all adolescent children (aged 12 to <18 years) in the 2018 and 2019 NSCH survey cycles. Data were analyzed from March 22 to August 11, 2023. Caregivers were asked, “During the past 12 months, has this child had their vision tested, such as with pictures, shapes, or letters?” Caregivers were further asked to select all the settings in which vision testing occurred (eye clinic, primary care clinic, school, health center, or other). The primary outcome was the caregiver report of vision testing in any setting within the previous 12 months; the secondary outcome was reported vision testing in each setting.
Variables collected from the survey included age, sex, race, ethnicity, insurance type, household income, educational level of caregivers, household generation, and primary household language. Caregiver-reported race and ethnicity were categorized into Hispanic, non-Hispanic Asian, non-Hispanic Black, non-Hispanic White, and other race (including American Indian or Alaska Native, Native Hawaiian or Other Pacific Islander, and multiple races). Insurance type was categorized into private, public, or uninsured. The highest educational level among caregivers was grouped into less than high school, high school, and greater than high school. Household income was divided with respect to the federal poverty level (FPL; 0% to <99%, 100% to <199%, 200% to <299%, 300% to <399%, and ≥400%). Household generation was categorized based on the country of birth of the child and parents. The primary household language was categorized into English, Spanish, or other.
We used linear regression to describe the patterns in reported vision testing as a function of age. We used logistic regression models to evaluate the association between report of vision testing and each sociodemographic factor, adjusting for participant age and sex. Imputed data files provided by the NSCH were used for the missing values in race and ethnicity, caregiver education, and household income (Supplement 1). All statistical analyses were performed with the appropriate survey weights to account for the NSCH sampling design using R software, version 4.2.0 (R Foundation for Statistical Computing). We used 2-tailed tests with significance defined as 2-tailed P < .05 and without adjustment for multiple comparisons.
Results
This study included 24 752 adolescents (median [IQR] age, 14 [13-16] years; 12 918 male [weighted, 51%] and 11 834 female [weighted, 49%]). The cohort demographic characteristics are summarized in Table 1. Vision testing in any setting within the previous year was reported by the caregivers of 18 621 adolescents (weighted, 74%). Vision testing was reported to have occurred at an eye clinic (13 323 participants [weighted, 51%]), primary care clinic (5230 participants [weighted, 22%]), school (2594 participants [weighted, 11%]), and health center (635 participants [weighted, 4%]).
Table 1. Caregiver-Reported Vision Testing Within the Previous 12 Months for US Adolescents in Any Setting.
| Variable | Overall participants, No. (N = 24 752) | Participants with vision tested within previous 12 mo, unweighted No. (weighted %)a | OR (95% CI)b | P value | |
|---|---|---|---|---|---|
| No (n = 6131) | Yes (n = 18 621) | ||||
| Sex | |||||
| Female | 11 834 | 2655 (24) | 9179 (76) | 1 [Reference] | NA |
| Male | 12 918 | 3476 (27) | 9442 (73) | 0.96 (0.94-0.99) | .006 |
| Race and ethnicityc,d | |||||
| Hispanic | 2821 | 708 (27) | 2113 (73) | 0.99 (0.95-1.03) | .60 |
| Non-Hispanic Asian | 1211 | 278 (28) | 933 (72) | 0.99 (0.93-1.04) | .62 |
| Non-Hispanic Black | 1633 | 379 (23) | 1254 (77) | 1.03 (0.99-1.07) | .10 |
| Non-Hispanic White | 17 463 | 4394 (26) | 13 069 (74) | 1 [Reference] | NA |
| Othere | 1624 | 372 (21) | 1252 (79) | 1.05 (1.00-1.09) | .04 |
| Type of insurancef | |||||
| Private | 17 850 | 4197 (24) | 13 653 (76) | 1 [Reference] | NA |
| Public | 5245 | 1321 (24) | 3924 (76) | 1.00 (0.97-1.03) | .94 |
| Uninsured | 1237 | 490 (45) | 747 (55) | 0.81 (0.76-0.87) | <.001 |
| Highest level of education among caregiversd | |||||
| More than high school | 20 544 | 4869 (24) | 15 675 (76) | 1 [Reference] | NA |
| High school | 3475 | 1004 (27) | 2471 (73) | 0.96 (0.93-0.99) | .01 |
| Less than high school | 733 | 258 (35) | 475 (65) | 0.89 (0.84-0.95) | <.001 |
| Household income, % of FPLd | |||||
| >400 | 10 069 | 2261 (23) | 7808 (77) | 1 [Reference] | NA |
| 300-399 | 4044 | 982 (24) | 3062 (76) | 1.00 (0.97-1.03) | .96 |
| 200-299 | 4140 | 1098 (27) | 3042 (73) | 0.96 (0.92-1.00) | .03 |
| 100-199 | 4163 | 1143 (28) | 3020 (72) | 0.95 (0.92-0.99) | .02 |
| 0-99 | 2336 | 647 (27) | 1689 (73) | 0.97 (0.93-1.01) | .11 |
| Household generationg | |||||
| Child and all parents born in US | 19 257 | 4680 (24) | 14 577 (76) | 1 [Reference] | NA |
| Child born in US and ≥1 parent born outside US | 3398 | 800 (28) | 2598 (72) | 0.96 (0.92-1.00) | .03 |
| Child born in US and parent birth location not listed | 1258 | 394 (33) | 864 (67) | 0.90 (0.84-0.97) | .004 |
| Child and parents born outside US | 518 | 166 (35) | 352 (65) | 0.90 (0.82-0.98) | .01 |
| Household primary languageh | |||||
| English | 23 190 | 5679 (25) | 17 511 (75) | 1 [Reference] | NA |
| Spanish | 801 | 224 (31) | 577 (69) | 0.94 (0.88-1.00) | .05 |
| Other | 642 | 200 (37) | 442 (63) | 0.88 (0.82-0.96) | .002 |
Abbreviations: FPL, federal poverty level; NA, not applicable; OR, odds ratio.
Survey-weighted percentages.
OR of reported vision test, adjusted for age and sex.
Caregiver-reported race and ethnicity.
The National Survey of Children’s Health provides imputed data files for the missing values in race and ethnicity, caregiver education, and household income that were calculated using sequential regression imputation methods.
Other included American Indian or Alaska Native, Native Hawaiian or Other Pacific Islander, and multiple races.
Data were missing for 420 participants.
Data were missing for 321 participants.
Data were missing for 119 participants.
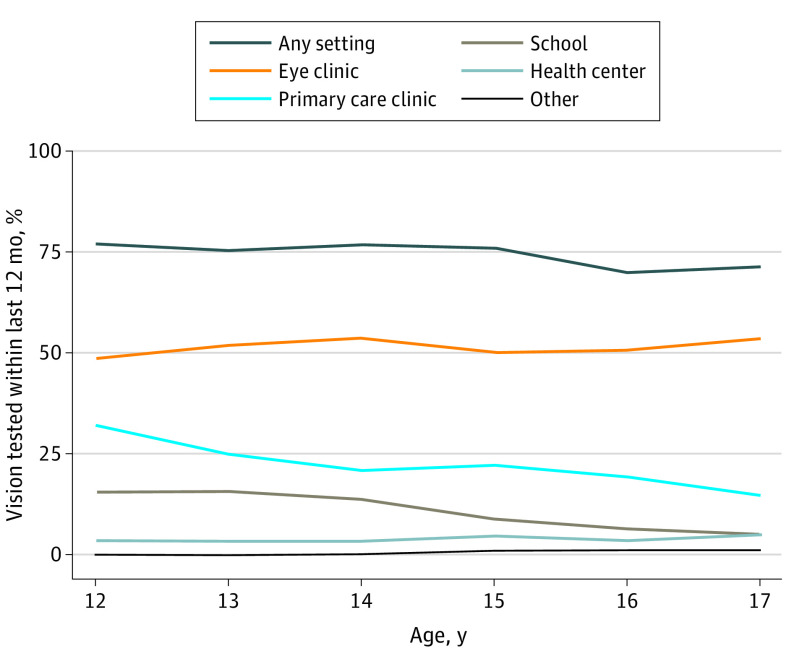
In the univariate analysis, the percentage of adolescents reported receiving vision testing in any setting decreased with age (−1.3% per year; 95% CI, −2.5% to 0% per year). This pattern was associated with a decrease in the adolescents reported receiving vision testing in the primary care setting (−2.8% per year; 95% CI, −4.3% to −1.4% per year) and the school setting (−2.4% per year; 95% CI, −3.3% to −1.5% per year). The percentage of adolescents reported receiving vision testing in an eye clinic did not differ by age (0.5% per year; 95% CI, −0.7% to 1.6% per year) (Figure).
Figure. Patterns in the Setting of Caregiver-Reported Vision Testing by Age for US Adolescents in the 2018-2019 National Survey of Children’s Health (N = 24 752).
In bivariate comparisons, adolescents not reported to have vision tested within the previous year were more likely to be male, uninsured, or living in lower income households; have caregivers with lower educational levels; be born outside of the US; and have a non-English primary language spoken at home (Table 1). After adjusting for age and sex in the multivariable analysis, there were lower odds of vision testing for adolescents who were uninsured vs insured (adjusted odds ratio [AOR], 0.81; 95% CI, 0.76-0.87), had caregivers with less than vs greater than high school education (AOR, 0.89; 95% CI, 0.84-0.95), and were from a family born outside vs inside the US (AOR, 0.90; 95% CI, 0.82-0.98). Analysis of the vision testing settings revealed that adolescents who were uninsured, were living in low-income households, had caregivers with lower educational levels, or were born outside the US were less likely to have reported vision testing in an eye clinic or primary care clinic but similarly likely to have reported testing in a school-based setting (Table 2).
Table 2. Caregiver-Reported Vision Testing Within the Previous 12 Months for US Adolescents in an Eye Clinic, Primary Care Clinic, or School Setting.
| Variable | Eye clinica | Primary care clinica | Schoola | ||||
|---|---|---|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | OR (95% CI) | P value | ||
| Sex | |||||||
| Female | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | |
| Male | 0.91 (0.89-0.94) | <.001 | 1.03 (1.01-1.06) | .008 | 1.00 (0.98-1.02) | .80 | |
| Race and ethnicityb | |||||||
| Hispanic | 0.99 (0.95-1.03) | .56 | 0.97 (0.94-1.01) | .11 | 0.99 (0.96-1.01) | .41 | |
| Non-Hispanic Asian | 1.07 (1.01-1.13) | .03 | 0.96 (0.92-1.01) | .10 | 0.96 (0.93-0.99) | .02 | |
| Non-Hispanic Black | 1.04 (0.99-1.08) | .09 | 1.00 (0.96-1.04) | .93 | 0.99 (0.97-1.02) | .59 | |
| Non-Hispanic White | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | |
| Otherc | 0.98 (0.93-1.03) | .42 | 1.03 (0.99-1.08) | .14 | 1.04 (0.99-1.08) | .10 | |
| Type of insurance | |||||||
| Private | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | |
| Public | 0.97 (0.93-1.00) | .04 | 0.97 (0.95-1.00) | .08 | 1.00 (0.98-1.02) | .74 | |
| Uninsured | 0.84 (0.79-0.90) | <.001 | 0.90 (0.86-0.94) | <.001 | 1.02 (0.97-1.07) | .44 | |
| Highest level of education among caregivers | |||||||
| More than high school | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | |
| High school | 1.01 (0.97-1.05) | .65 | 0.93 (0.90-0.96) | <.001 | 0.99 (0.97-1.01) | .21 | |
| Less than high school | 0.87 (0.81-0.93) | <.001 | 0.90 (0.86-0.94) | <.001 | 0.99 (0.95-1.03) | .62 | |
| Household income, % of FPL | |||||||
| >400 | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | |
| 300-399 | 0.99 (0.95-1.03) | .66 | 1.00 (0.96-1.03) | .93 | 1.03 (1.00-1.05) | .04 | |
| 200-299 | 0.98 (0.94-1.02) | .25 | 0.96 (0.92-0.99) | .01 | 1.02 (0.99-1.05) | .19 | |
| 100-199 | 0.96 (0.92-1.00) | .04 | 0.94 (0.91-0.98) | <.001 | 1.01 (0.99-1.03) | .37 | |
| 0-99 | 0.93 (0.89-0.98) | .004 | 0.93 (0.90-0.97) | <.001 | 1.01 (0.99-1.04) | .31 | |
| Household generation | |||||||
| Child and all parents born in US | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | |
| Child born in US and ≥1 parent born outside US | 0.97 (0.93-1.01) | .09 | 0.98 (0.95-1.01) | .16 | 0.95 (0.93-0.98) | <.001 | |
| Child born in US and parent birth location not listed | 0.88 (0.83-0.94) | <.001 | 0.94 (0.89-1.00) | .06 | 0.97 (0.94-1.00) | .07 | |
| Child and parents born outside US | 0.85 (0.78-0.93) | <.001 | 0.95 (0.89-1.00) | .07 | 1.06 (0.98-1.14) | .16 | |
| Household primary language | |||||||
| English | 1 [Reference] | NA | 1 [Reference] | NA | 1 [Reference] | NA | |
| Spanish | 0.88 (0.82-0.94) | <.001 | 0.97 (0.92-1.02) | .21 | 0.98 (0.94-1.02) | .36 | |
| Other | 0.92 (0.86-1.00) | .04 | 0.91 (0.86-0.96) | <.001 | 0.96 (0.93-0.99) | .02 | |
Abbreviations: FPL, federal poverty level; NA, not applicable; OR, odds ratio.
The binary outcome for each regression model is report of vision testing in the specified setting (eye clinic, primary clinic, or school) vs no report of vision screening in that setting.
Caregiver-reported race and ethnicity.
Other included American Indian or Alaska Native, Native Hawaiian or Other Pacific Islander, and multiple races.
Discussion
Although most adolescents in the US were reported by their caregivers to have had their vision tested within the previous year, individuals from socioeconomically disadvantaged backgrounds, including those lacking health insurance and living in low-income households, were less likely to have reported receiving a vision test. Our findings further suggest that language- and education-related barriers may also contribute to differences in caregiver-reported vision testing. Limited access to vision testing may delay the identification and treatment of ocular conditions and contribute to the inequities in visual function (and related educational and employment opportunities) in the adolescent population.2
Vision testing in adolescents is recommended every 1 to 2 years by the American Academy of Ophthalmology.9 Although schools and primary care clinics contribute to preventive vision care for young children,10,11 both play a lesser role for older children. Few states have school screening mandates for adolescents,7 and the recommended frequency of vision screening by pediatricians decreases in adolescence.12 As a result, a greater proportion of adolescents rely on eye clinics for routine vision evaluations. Shifts in the setting of care delivery may create barriers for those who have difficulty accessing subspecialty care. Health insurance, transportation, and language barriers may delay the establishment of care and interfere with the appropriate treatment and follow-up.13
Limitations
This study is limited by the reliance on caregiver recall. Sociodemographic factors may be associated with the ability of caregivers to accurately recall whether vision testing took place and may reflect the degree of involvement in the child’s health care and likelihood of being aware of vision testing being performed. Future studies should consider using alternative data sources to validate caregivers’ recollections and reduce the potential for recall bias.
Conclusions
Innovative approaches are needed to identify children who would benefit most from eye examinations. These findings suggest that adolescents from socioeconomically disadvantaged backgrounds are less likely to have vision tested in clinic-based settings, while this is not the case in school-based settings. Consideration should be given to strategies that expand the role of school-based vision testing for older children who are not otherwise receiving vision care.
eMethods. The National Survey of Children's Health 2018 and 2019
Data Sharing Statement
References
- 1.Evans JR, Morjaria P, Powell C. Vision screening for correctable visual acuity deficits in school-age children and adolescents. Cochrane Database Syst Rev. 2018;2(2):CD005023. doi: 10.1002/14651858.CD005023.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adomfeh J, Jastrzembski BG, Oke I. Association of race, ethnicity, and socioeconomic status with visual impairment in adolescent children in the US. JAMA Ophthalmol. 2022;140(10):1006-1010. doi: 10.1001/jamaophthalmol.2022.3627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Qiu M, Wang SY, Singh K, Lin SC. Racial disparities in uncorrected and undercorrected refractive error in the United States. Invest Ophthalmol Vis Sci. 2014;55(10):6996-7005. doi: 10.1167/iovs.13-12662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wood JM, Black AA, Hopkins S, White SLJ. Vision and academic performance in primary school children. Ophthalmic Physiol Opt. 2018;38(5):516-524. doi: 10.1111/opo.12582 [DOI] [PubMed] [Google Scholar]
- 5.Hopkins S, Black AA, White SLJ, Wood JM. Visual information processing skills are associated with academic performance in grade 2 school children. Acta Ophthalmol. 2019;97(8):e1141-e1148. doi: 10.1111/aos.14172 [DOI] [PubMed] [Google Scholar]
- 6.Hopkins S, Narayanasamy S, Vincent SJ, Sampson GP, Wood JM. Do reduced visual acuity and refractive error affect classroom performance? Clin Exp Optom. 2020;103(3):278-289. doi: 10.1111/cxo.12953 [DOI] [PubMed] [Google Scholar]
- 7.Wahl MD, Fishman D, Block SS, et al. A comprehensive review of state vision screening mandates for schoolchildren in the United States. Optom Vis Sci. 2021;98(5):490-499. doi: 10.1097/OPX.0000000000001686 [DOI] [PubMed] [Google Scholar]
- 8.Ghandour RM, Jones JR, Lebrun-Harris LA, et al. The design and implementation of the 2016 National Survey of Children’s Health. Matern Child Health J. 2018;22(8):1093-1102. doi: 10.1007/s10995-018-2526-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wallace DK, Morse CL, Melia M, et al. ; American Academy of Ophthalmology Preferred Practice Pattern Pediatric Ophthalmology/Strabismus Panel . Pediatric Eye Evaluations Preferred Practice Pattern®: I. vision screening in the primary care and community setting; II. comprehensive ophthalmic examination. Ophthalmology. 2018;125(1):P184-P227. doi: 10.1016/j.ophtha.2017.09.032 [DOI] [PubMed] [Google Scholar]
- 10.Ambrosino C, Dai X, Aguirre BA, Collins ME. Pediatric and school-age vision screening in the United States: rationale, components, and future directions. Children (Basel). 2023;10(3):490. doi: 10.3390/children10030490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Donahue SP, Nixon CN; Section on Ophthalmology, American Academy of Pediatrics; Committee on Practice and Ambulatory Medicine, American Academy of Pediatrics; American Academy of Ophthalmology; American Association for Pediatric Ophthalmology and Strabismus; American Association of Certified Orthoptists . Visual system assessment in infants, children, and young adults by pediatricians. Pediatrics. 2016;137(1):28-30. doi: 10.1542/peds.2015-3596 [DOI] [PubMed] [Google Scholar]
- 12.Committee on Practice and Ambulatory Medicine; Bright Futures Periodicity Schedule Workgroup . 2023 Recommendations for preventive pediatric health care. Pediatrics. 2023;151(4):e2023061451. doi: 10.1542/peds.2023-061451 [DOI] [PubMed] [Google Scholar]
- 13.Varadaraj V, Frick KD, Saaddine JB, Friedman DS, Swenor BK. Trends in eye care use and eyeglasses affordability: the US National Health Interview Survey, 2008-2016. JAMA Ophthalmol. 2019;137(4):391-398. doi: 10.1001/jamaophthalmol.2018.6799 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eMethods. The National Survey of Children's Health 2018 and 2019
Data Sharing Statement