Abstract
This article has been temporarily removed by the publisher, Wolters Kluwer, due to a data quality issue. We regret any confusion this may have caused. This article will be published once production is complete on the Public Health Workforce Interest and Needs Survey supplemental issue.
Context:
There is little empirical evidence regarding the magnitude of the COVID-19 response across the public health workforce and the extent to which other public health programs were called upon to contribute to the response, potentially leading to less work being done in other public health programs during the COVID-19 pandemic.
Objectives:
To assess the composition of the workforce that contributed to the COVID-19 pandemic response during 2020-2022.
Design:
A large, cross-sectional, nationally representative survey of the state and local public health agency workforce through the Public Health Workforce Interest and Needs Survey (PH WINS).
Setting:
Nearly all state health agency-central offices (SHA-COs) and Big City Health Coalition (BCHC) member public health departments as well as a nationally representative sample of other local health departments (LHDs) with more than 25 staff members and serving more than 25 000 people participated in fall 2021.
Participants:
A sample of all individuals working at each SHA-CO or LHD as part-time or full-time employees, contractors, or other employee types was used. A total of 44 732 responses (35% of eligible respondents) were received.
Main Outcome Measure:
Main outcomes included the proportion of full-time equivalent (FTE) effort devoted to COVID-19 response work by quarter (Q) from Q1 2020 through Q1 2022. Predictors of interest included individual- and agency-level demographics, most notably an individual's self-reported public health program area.
Results:
Staffing and hiring for the COVID-19 pandemic response was an ongoing effort that began in 2020 and lasted through 2022. During the pandemic, all public health program areas contributed at least 20% of their workforce time to COVID-19 response, peaking at 47-83% of the staff time, depending on the program area.
Conclusions:
There was a considerable public health opportunity cost to the public health systems' large and prolonged COVID-19 response. Persistent understaffing in the public health system remains an important issue.
Keywords: COVID-19, emergency preparedness and response, PH WINS, public health workforce, opportunity cost
In the decade prior to the COVID-19 pandemic, health care spending in the United States increased by a trillion dollars or roughly 38%,1,2 while state and local governmental public health spending was stagnant or declining.3–5 This absence of commensurate growth in governmental public health funding has contributed to declines in the size of the state and local governmental public health agency workforce estimated at approximately 30 000 full-time equivalents (FTEs).4,5 There is no reason to believe that there is less need for public health services in US communities, nor has there been a reduction in the scope of essential public health services.6,7 Therefore, discussion of a public health workforce shortage has arisen. As of 2021, the de Beaumont Foundation and the Public Health National Center for Innovations (PHNCI) estimate that the public health workforce would need to increase by roughly 80% in order for state and local public health agencies to provide the core set of essential public health services to their jurisdictions.8,9 This equates to a workforce shortage of more than 80 000 FTEs.8
A major implication of the state and local governmental public health workforce shortage is a lack of spare bandwidth capacity to mobilize the necessary response to COVID-19. To deliver the appropriate response, state and local governmental public health agencies were required to draw resources from existing public health work, potentially causing those services to severely decline or pause altogether. This may have important opportunity costs for public health, especially if the public health need persists and no others in the community are available to backfill. There are also important ramifications resulting from having the existing workforce work longer or harder, including burnout, negative impacts to mental and emotional wellness, or other related issues.10
Having an excess of resources, or “slack resources,” available to produce a minimum level of services11 is a consistent and well-known predictor of organizational success overall12 and within health care, specifically.13–15 When slack resources are not present, such as in the governmental public health workforce, workers may be asked to pause existing work to support emergent needs, to work faster to produce more in the same time period, or to work longer (ie, overtime) hours to ensure that existing and emergent needs are all met. Although there is little evidence regarding the effect of slack resources on public health agencies or outcomes, it is reasonable to hypothesize that slack resources could yield better public health outcomes as they do elsewhere. Some data suggest that public health agencies may be able to handle temporary periods of relatively high need, but at relatively high organizational and financial cost.16 Slack resources could abate some of that cost by allowing workers and teams to more easily absorb emergent tasks, provide cover during periods of low workforce capacity/high work need, improve or enhance existing work products, and or avoid burnout by maintaining a manageable workload on an indefinite basis.12,15
The goal of this analysis was to provide an initial descriptive picture of the implications of expanded public health workload demands during the COVID-19 pandemic, how that expanded workload was addressed by the public health workforce, and its possible effect on ongoing work.
Methods
PH WINS 2021, fielded from September 2021 to January 2022, is the third iteration of the Public Health Workforce Interests and Needs Survey (PH WINS). Conducted first in 2014 and again in 2017, PH WINS is the only survey of its kind, capturing individual governmental public health workers' perspectives on engagement, satisfaction, mental health, and training needs and addressing public health issues, and collects demographic information on the workforce. Unlike in previous years, PH WINS 2021 included survey questions regarding the toll of the COVID-19 pandemic on the workforce. The survey aimed to be inclusive of the workforce's experience with the COVID-19 pandemic and its response without being solely about it.
Several questions were added to PH WINS 2021 to understand the burden of the COVID-19 pandemic, including staffing levels and how COVID-19 activities affected the workforce's ability to meet existing and emergent health department needs and priorities. Respondents were asked about their employment status prior to March 2020; if they were a part of their department's COVID-19 pandemic response; the degree to which they served in a COVID-19 pandemic response role, if applicable, by quarter (Q) from Q1 2020 (January-March) to Q4 2021 (October-December); and the average amount of overtime worked while working in a COVID-19 response role. See Supplemental Digital Content Appendix (available at http://links.lww.com/JPHMP/B83) for a complete set of COVID-19–related questions and response options. Respondents who completed the survey prior to Q4 2021 were not asked about their utilization in a COVID-19 pandemic response role during that quarter.
The PH WINS methodologies are described in more detail elsewhere (Robins et al 2022, in this issue).17 Briefly, using employee rosters from participating departments, PH WINS was sent to 137 446 individuals in the governmental public health workforce representing 47 state health agencies (SHAs) and 288 decentralized local health departments (LHDs) across the United States. Decentralization refers to the governance structure of a health department and describes the relationship an SHA has to the LHDs in the state. There are 4 types of governance: decentralized, centralized, mixed, and shared.18,19 The final nationally representative sample of LHDs includes LHDs from both decentralized and nondecentralized states and excludes those health departments with a staff size of less than 25 or serving a population of less than 25 000. PH WINS received 44 732 responses (35% of eligible respondents). We also report findings from state health agency-central office (SHA-CO) respondents later. Approximately 68% of responses were received between September 13, 2021 (survey start date), and the end of October, an additional 9% by the end of November, an additional 10% by the end of December, and the remainder by survey closure on January 14, 2022.
This article describes the demographics, workforce characteristics, utilization rates, and hiring patterns of the COVID-19 Response Workforce. The COVID-19 Response Workforce is defined here as respondents who indicated serving in a COVID-19 pandemic response role at any point during the pandemic (March 2020 until survey completion) or who were currently serving in the COVID-19 response program area (selected “COVID-19 Response” when asked about their current program area). Those who did not serve in a COVID-19 pandemic response role at any point in time from March 2020 until survey completion are referred to as the “Existing Services Workforce.” Utilization rates refer to the degree to which a respondent served in a COVID-19 pandemic response role by a quarter. Respondents who stated that they were not working at the health department prior to March 2020 or were hired specifically to serve in a COVID-19 pandemic response role were classified as new hires. PH WINS 2021 data were cleaned, managed, and analyzed in Stata 17 (StataCorp LLC, Station College, Texas). Balance repeated replication weights were constructed to account for the complex sampling design and adjust for nonresponse.
Results
Composition of the COVID-19 response workforce
Nearly three-fourths (72%; 95% confidence interval [95% CI], 72-73) of state and local governmental public health employees served in the COVID-19 response workforce (Table 1). A larger proportion of LHD staff (76%; 95% CI 76%-77%) participated in COVID-19 pandemic response activities as compared to SHA-CO staff (62%; 95% CI 61%-63%).
TABLE 1. Descriptives on Those Who Did Versus Did Not Serve in a COVID-19 Response Role.
| COVID-19 Response Workforce (N = 136 591) | Existing Services Workforcea (N = 52 735) | Total (N=189 326) | ||||
|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | |
| Total Workforce | 72.2 | 71.6-72.7 | 27.8 | 27.3-28.4 | 100 | |
| Setting - State CO vs All Local | ||||||
| SHA-CO | 62.3 | 61.4-63.1 | 37.7 | 36.9-38.6 | 100 | |
| Local | 76.4 | 75.7-77.0 | 23.6 | 23.0-24.3 | 100 | |
| Primary program area (categories)b | ||||||
| Communicable Disease | 30.4 | 29.7-31.0 | 7.6 | 7.0-8.1 | 24 | 23.5-24.5 |
| Organizational Competencies | 16.4 | 15.9-16.9 | 22.8 | 21.8-23.7 | 18.2 | 17.7-18.6 |
| Other Health Care | 16 | 15.5-16.5 | 15.4 | 14.6-16.3 | 15.8 | 15.4-16.3 |
| Maternal and Child Health | 10.9 | 10.5-11.4 | 23.1 | 22.2-24.1 | 14.3 | 13.9-14.7 |
| Environmental Health | 8.1 | 7.8-8.5 | 9.6 | 8.9-10.2 | 8.5 | 8.2-8.9 |
| Assessment | 7.3 | 7.0-7.7 | 9.8 | 9.2-10.5 | 8 | 7.7-8.4 |
| Chronic Disease & Injury | 4.2 | 3.9-4.5 | 5 | 4.5-5.5 | 4.4 | 4.2-4.7 |
| Other | 3.3 | 3.1-3.5 | 4.9 | 4.5-5.4 | 3.7 | 3.5-4.0 |
| All Hazards | 1.9 | 1.7-2.1 | 0.4 | 0.3-0.5 | 1.5 | 1.4-1.6 |
| Communications | 1.5 | 1.3-1.6 | 1.4 | 1.2-1.7 | 1.5 | 1.3-1.6 |
| Job classification (categories)b | ||||||
| Public Health Sciences | 41 | 40.3-41.7 | 32.3 | 31.3-33.3 | 38.6 | 38.0-39.1 |
| Administrative | 31.4 | 30.8-32.1 | 42.6 | 41.5-43.8 | 34.5 | 34.0-35.1 |
| Clinical and Lab | 25.7 | 25.1-26.3 | 21.6 | 20.7-22.6 | 24.6 | 24.1-25.1 |
| Social Services and All Other | 1.8 | 1.7-2.0 | 3.5 | 3.1-3.9 | 2.3 | 2.1-2.5 |
| PH Degree (Bach/Mast/Doc) | 16.2 | 15.7-16.7 | 8.8 | 8.2-9.4 | 14.1 | 13.7-14.5 |
| Tenure in Current Position (categories) | ||||||
| 0-5 years | 67.2 | 66.6-67.9 | 61.6 | 60.5-62.7 | 65.7 | 65.1-66.2 |
| 6-10 years | 14.8 | 14.3-15.3 | 14.7 | 13.9-15.5 | 14.7 | 14.3-15.2 |
| 11-15 years | 7.2 | 6.8-7.6 | 9.1 | 8.5-9.8 | 7.7 | 7.4-8.0 |
| 16-20 years | 5 | 4.7-5.3 | 6.4 | 5.9-7.0 | 5.4 | 5.1-5.7 |
| 21 or above | 5.8 | 5.5-6.2 | 8.2 | 7.6-8.8 | 6.5 | 6.2-6.8 |
| Tenure in Current Agency (categories) | ||||||
| 0-5 years | 50.5 | 49.8-51.2 | 47.8 | 46.7-49.0 | 49.8 | 49.2-50.4 |
| 6-10 years | 17 | 16.5-17.5 | 16.3 | 15.6-17.2 | 16.8 | 16.4-17.3 |
| 11-15 years | 11.2 | 10.8-11.7 | 12.2 | 11.5-13.0 | 11.5 | 11.1-11.9 |
| 16-20 years | 9.1 | 8.7-9.5 | 9.5 | 8.8-10.2 | 9.2 | 8.9-9.5 |
| 21 or above | 12.1 | 11.7-12.6 | 14.1 | 13.4-14.9 | 12.7 | 12.3-13.1 |
| Supervisory status | ||||||
| Non-supervisor | 70.9 | 70.3-71.5 | 78.4 | 77.4-79.2 | 73 | 72.5-73.5 |
| Supervisor | 17.2 | 16.7-17.7 | 15 | 14.2-15.8 | 16.6 | 16.2-17.0 |
| Manager | 9 | 8.6-9.4 | 6.1 | 5.6-6.6 | 8.2 | 7.9-8.5 |
| Executive | 2.9 | 2.7-3.2 | 0.6 | 0.4-0.8 | 2.3 | 2.1-2.5 |
| Employment Statusb | ||||||
| Permanent Staff | 85.1 | 84.6-85.5 | 90.4 | 89.7-91.1 | 86.5 | 86.1-86.9 |
| Temporary Staff | 8.7 | 8.3-9.1 | 4.4 | 4.0-4.9 | 7.5 | 7.2-7.8 |
| Contractor | 5.3 | 4.9-5.6 | 3.6 | 3.1-4.1 | 4.8 | 4.5-5.1 |
| Federal Employee | 0.6 | 0.5-0.8 | 1.1 | 0.9-1.4 | 0.8 | 0.7-0.9 |
| Intern | 0.3 | 0.3-0.4 | 0.5 | 0.3-0.7 | 0.4 | 0.3-0.5 |
| New v. Not New Employee 2020-2022 | ||||||
| New Employee | 16.5 | 16.0-17.0 | 13.8 | 13.0-14.6 | 15.7 | 15.3-16.2 |
| Not a New Employee | 83.5 | 83.0-84.0 | 86.2 | 85.4-87.0 | 84.3 | 83.8-84.7 |
| New Employees 2020-2022 | 75.6 | 74.2-76.9 | 24.4 | 23.1-25.8 | 100 | |
aExisting services workforce indicates employees that did not serve in a COVID-19 pandemic response role.
bSorted from largest to smallest based on the COVID-19 Workforce.
Seventy-six percent (95% CI, 74-77) of all new hires (hired between March 2020 and December 2021) worked on COVID-19 pandemic response activities; and 17% (95% CI 16%-17%) of the state and local governmental public health COVID-19 response workforce is a new hire. Most COVID-19 response workers are permanent staff (85%; 95% CI 85%-86%) and serve in non-supervisory roles (71%; 95% CI 70%-72%). Only 16% (95% CI 16%-17%) have a bachelors, masters, or doctoral degree in public health. The largest percentage (41%; 95% CI, 40-42) of the COVID-19 response workforce served in a public health sciences job, which includes epidemiologists, department leadership, program implementation and evaluation staff, and policy analysts, among many others.
Proportion of staff responding to the COVID-19 pandemic by program area
Table 1 shows that nearly one-third (30%; 95% CI 30%-31%) of the COVID-19 response workforce selected communicable diseases as their primary program area. However, 91% (95% CI 91%-92%) of the communicable disease workforce served in the COVID-19 response workforce, meaning they participated in COVID-19 pandemic response activities fully or partially at some point from March 2020 until survey completion (Table 2). All hazards is the program area with one of the smallest proportion of staff nationally (2%; 95% CI: 2%-2%) yet has the largest proportion serving in a COVID-19 response role (93%; 95% CI 90%-95%). The program area with the smallest proportion of the workforce serving in a COVID-19 response role was Maternal and Child Health (MCH), however, still more than half of the MCH workforce (55%; 95% CI 54%-57%) served in a COVID-19 response role. The specific programs that constitute each program area are shown in Appendix Table 1 (available at http://links.lww.com/JPHMP/B83).
TABLE 2. Proportion of the COVID-19 Response Workforce by (Non-COVID Response) Primary Program Area.
| Primary Program Area (Categories) | COVID-19 Response Workforce | Existing Services Workforce | Total % | ||
|---|---|---|---|---|---|
| %a | 95% CI | % | 95% CI | ||
| All Hazards | 93.0 | 90.2-95.0 | 7.0 | 5.0-9.8 | 100 |
| Communicable Disease | 91.2 | 90.6-91.9 | 8.8 | 8.1-9.4 | 100 |
| Other Health Care | 72.9 | 71.5-74.2 | 27.1 | 25.8-28.5 | 100 |
| Communications | 72.3 | 67.6-76.6 | 27.7 | 23.4-32.4 | 100 |
| Environmental Health | 68.8 | 67.0-70.6 | 31.2 | 29.4-33.0 | 100 |
| Chronic Disease & Injury | 68.5 | 65.9-71.0 | 31.5 | 29.0-34.1 | 100 |
| Assessment | 65.9 | 64.0-67.9 | 34.1 | 32.1-36.0 | 100 |
| Organizational Competencies | 65.1 | 63.7-66.4 | 34.9 | 33.6-36.3 | 100 |
| Other | 63.3 | 60.4-66.2 | 36.7 | 33.8-39.6 | 100 |
| Maternal and Child Health | 55.1 | 53.5-56.6 | 44.9 | 43.4-46.5 | 100 |
aTable is sorted from largest to smallest percent serving in a COVID-19 response role.
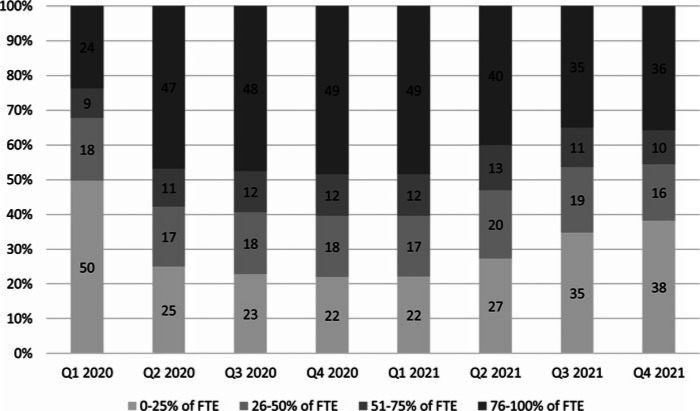
Time spent on COVID-19 pandemic response activities
From April 2020 to March 2021, nearly half of the workforce (47% Q2 2020; 48% Q3 2020; 49% Q4 2020; 49% Q1 2021) spent more than three-quarters of their time on COVID-19 pandemic response activities (Figure 1). The percent time devoted to COVID-19 pandemic response varied by program throughout 2020 and 2021, however, at all times during the COVID-19 pandemic, more than half of the workforce devoted at least one-quarter of their time to COVID-19 pandemic response activities.
FIGURE 1.
Distribution of Percentage of FTE Effort Devoted to COVID Response Across the COVID-19 Response Workforce (2020-2022) Abbreviation: FTE, full-time equivalent.
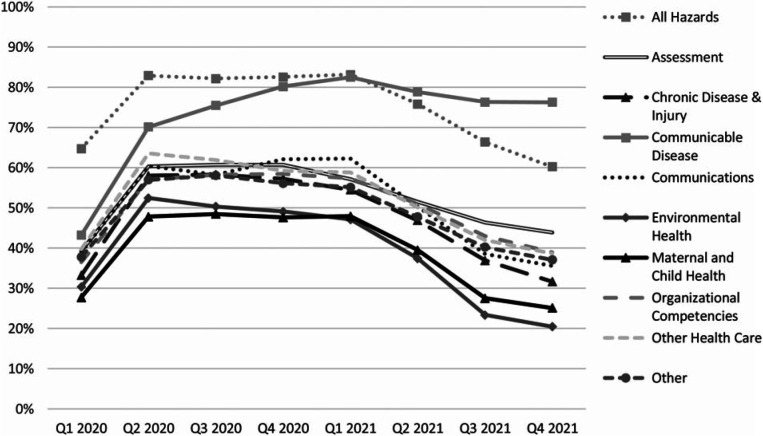
Percent time devoted to COVID-19 pandemic response activities per quarter by program area is shown in Figure 2. Those working in all hazards spent the largest percentage of time on COVID-19 pandemic response until Q1 2021 (January-March), after which time those working in communicable disease spent the largest percentage of time on COVID-19 pandemic response. Figure 2 also shows that employees working in all program areas devoted sizable percentages of FTE effort to COVID-19 pandemic response. Those working in MCH and environmental health generally devoted the least amount of time to COVID-19 pandemic response activities in every quarter, but devoted nearly half of their FTE effort to COVID from Q2 2020 through Q1 2021 and devoted more than 20% of their FTE effort to COVID during the entirety of the period surveyed.
FIGURE 2.
Percentage of Total Public Health Workforce FTE Effort Devoted to COVID-Response, by Program Area Abbreviation: FTE, full-time equivalent.
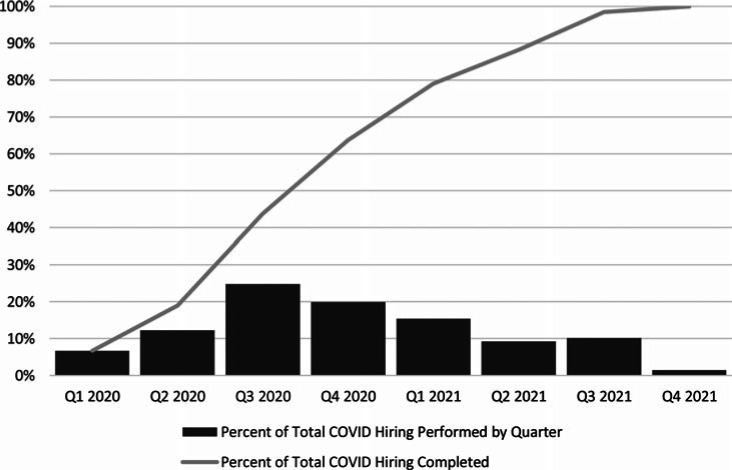
Staffing increases to fulfill COVID-19 pandemic response roles
July 2020 to September 2020 (Q3 2020) saw the highest number of new hires, with 25% (95% CI 24%-26%) of all new staff hired during that time (Figure 3). The proportion of new staff hired remained high through the beginning of 2021 with 20% (95% CI 19%-21%) of new staff hired between October 2020 and December 2020 and 15% (95% CI 14%-17%) of new staff hired in the first three months of 2021. By March 2021, about one year into the COVID-19 pandemic, about eighty percent of COVID-19 pandemic related hiring had been completed.
FIGURE 3.
State and Local Public Health Agency COVID-19–Related Hiring by Quarter
Discussion
This study is among the first to capture the experiences of the state and local public health workforce in terms of who contributed to the pandemic response, when, and to what extent. Our analysis makes use of a newly available data from a representative sample of individuals within agencies across the United States. This analysis finds that nearly three-fourths of the state and local governmental public health workforce across all foundational public health services, position types, and backgrounds participated in the COVID-19 pandemic response. Given existing public health workforce shortages, we believe that this demonstrates a major opportunity cost in terms of other core public health work that was not completing during this time.
We observed 2 main ways in which the state and local governmental public health workforce responded to the COVID-19 pandemic—hiring of additional staff and reallocating the workload and responsibilities of existing staff. With respect to the former of those, staffing up to respond to the COVID-19 pandemic was a large but not an instantaneous process. In total, thousands of additional workers were hired—as temporary workers, contractors, nonpermanent staff, or full-time permanent positions. However, this hiring process persisted across 2020 and 2021. Peak hiring occurred during the third quarter of 2020, several months after the initial onset of the pandemic, and large amounts of hiring continued well into the second half of 2021. By that point, the pandemic was well into its second year. Our finding that it took roughly a full year to complete 80% of all COVID-related hiring suggests that staffing up is not an immediate process. Indeed, large amounts of additional hiring was occurring at the same time at which the existing workforce was reporting high levels of burnout due to excessive workload seems especially important for public health practice and policy. Together, these 2 findings may suggest that the workers being hired well into the pandemic may have in fact been needed far earlier to meet emergent workloads, avert burnout, and avoid lost work when existing workforce turns attention away from prior responsibilities and to the COVID-19 pandemic.
In addition to hiring additional staff, we found clear evidence that the public health workforce also responded to the COVID-19 pandemic by reallocating the workload and responsibilities of the current workforce. The opportunity cost of workforce re-allocation may have serious implications for the public health system. Reallocation occurred across essentially every public health setting, program area, job classification, and demographic category analyzed. These results largely align with prior findings. A qualitative analysis from earlier in the COVID-19 pandemic found that all respondents reported reallocating existing workers from their usual roles into contact tracing roles.20
Reallocation means that, for example, individuals who had previously been responsible for everything from chronic disease to communications had less time to perform all other non-COVID-19 pandemic related work as a result of large COVID-19 pandemic response workload demands. This shift appeared to rapidly increase by the second quarter of 2020 and persist through the first quarter of 2021 before finally starting to tail off. But even by the last quarter of 2021, COVID-19 pandemic response work still accounted for 20% or more of the workload for each public health program area. At peak response levels, more than 80% of all communicable disease workload effort was devoted to COVID-19 pandemic response. That may in fact have been the appropriate amount of time and effort to respond to the COVID-19 pandemic, but it leaves open the question of whether the remaining 20% of communicable disease staff is sufficient for assessing and surveilling all other communicable diseases. If, as is reasonable to hypothesize, the remaining 20% of communicable disease staff is not sufficient for assessing and surveilling all other communicable diseases, there is considerable risk for public health workforce burnout and public health opportunity costs due to diseases and outbreaks that are not investigated.
On the one hand, this is important as it means that, to the extent to which public health departments and professionals are some of the most well-positioned and connected individuals within their communities, COVID-19 pandemic response work was undertaken by individuals well-positioned for this work. However, given that COVID-19 pandemic–related hiring persisted during and beyond these times, it is reasonable to suspect that there was an unmet need and additional work to be done elsewhere within the public health system. On the other hand, these undelivered services or unmet needs constitute the public health opportunity cost of our COVID-19 pandemic response. An opportunity cost is defined as the value of what we give up when we make one choice (over another).21 Our findings demonstrate that our collective COVID-19 pandemic response approach entailed reallocating the existing public health workforce away from existing services and priorities to COVID-19 pandemic response work and gradually backfilling through sustained additional hiring. Our findings therefore clearly suggest a considerable public health opportunity cost to the public health systems' large and prolonged COVID-19 pandemic response. An alternative scenario to envision would be one in which the nation's public health system does not face a workforce shortage of some 80 000 FTEs or has robust infrastructure in place for rapidly scaling the public health workforce as needed, including additional training pipelines or capacity enhancement mechanisms.
Future quantitative and qualitative research could help reveal the specific public health services that were paused or modified in order to accommodate the reductions in available workforce due to the COVID-19 response. This subsequent research could tie in with existing estimates of missed routine and preventive medical care,22,23 some of which may be related to the reduction in available public health workforce. For example, while 55% of the MCH workforce was at times working on COVID-19–related work, it is not clear from this study what happened to MCH services during this time. It is plausible that some MCH work would have been paused due to the pandemic itself or conversely may have been exacerbated by the pandemic, so it may or may not be the case that prepandemic staffing levels exactly equate to the COVID-19 response opportunity cost.
Our findings should be viewed in light of several limitations. First, in some states and localities, COVID-19 response may have been handled by a separate department or unit. In these cases, if the employee was not included on the staff roster provided by the health department, he or she was not invited to complete the survey. Therefore, our findings may better capture the impacts of the COVID-19 pandemic response to public health agencies rather than to state or local government as a whole. Second, although the PH WINS sample frame would capture workers who telecommute or work remotely from home, the sample frame may not capture all field-based employees or contractors. The assumption is that field-based workers are not bound to their computer as staff working at a desk may be. This contributes to lower response rates among field-based employees. This is an important limitation but one that maybe less relevant to our specific study of interest (COVID-19 response) due to the nature of work during this time and the individuals most heavily involved in the COVID-19 response. Third, although our data are the largest and most representative individual-level data on the public health workforce, there is a theoretical potential for response bias. Specifically, individuals who are especially busy or, conversely, especially uninterested in the survey topic areas may be more or less likely to respond. These potential biases, if any, are theoretical. We employed survey response weights to ensure that our estimates are representative of overall public health workforce demographics. Fourth, the survey was completed between September 2021 and January 2022. A respondents survey completion date has implications for the reported degree to which they served in their COVID-19 response role by quarter. For example, a respondent who completed the survey in September 2021 did not have an opportunity to share the degree to which they served in their COVID-19 response role during Q4 2021 (October-December). This may cause the reported average time spent on COVID-19 response to be lower than the actual for Q4 2021. In addition, new hires hired once the survey was well underway, unless specifically added by the participating department, did not receive the survey. This likely means that new hires hired between October and December 2021 are underrepresented. Finally, the data are self-reported by respondents. We were not able to independently verify reported workloads or position details. Although it is theoretically possible that reported workloads and topics would not match actual workloads and topics, this general approach—asking individuals to self-report workloads and topics—has been used extensively in past surveys and scholarly reports of the public health workforce.4,6,16,24
Implications for Policy & Practice
Staffing and hiring for the COVID-19 pandemic response was a large effort that spanned essentially all of 2020 and 2021, and even into 2022.
At all times during the pandemic, every single public health program area was spending 20% or more of workforce time on COVID-19 response efforts. At its peak (Q1 2021), the COVID-19 response took up between 48% of MCH time and 83% of communicable disease time.
Given that there was a preexisting workforce shortage and that COVID-19–related hiring persisted during and beyond peak response times, there is reason to suspect that there was unmet need and additional work to be done somewhere within the public health system.
There was likely a considerable public health opportunity cost to the public health systems' large and prolonged COVID-19 response.
Absent a larger workforce or process changes for much faster staffing up, it is reasonable to think that future pandemic responses may also have an opportunity cost to the public health system.
Supplementary Material
Footnotes
The authors declare no conflicts of interest.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (http://www.JPHMP.com).
Contributor Information
J. Mac McCullough, Email: MacMcCullough@boisestate.edu.
Moriah Robins, Email: gendelman@debeaumont.org.
References
- 1.Martin AB, Lassman D, Washington B, Catlin A. Growth in US health spending remained slow in 2010; health share of gross domestic product was unchanged from 2009. Health Aff. 2012;31(1):208–219. [DOI] [PubMed] [Google Scholar]
- 2.McCullough JM, Speer M, Magnan S, Fielding JE, Kindig D, Teutsch SM. Reduction in US health care spending required to meet the institute of medicine's 2030 target. Am J Public Health. 2020;110(12):1735–1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Alfonso YN, Leider JP, Resnick B, McCullough JM, Bishai D. US public health neglected: flat or declining spending left states ill equipped to respond to COVID-19. Health Aff. 2021;40(4):664–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.National Association of County & City Health Officials. NACCHO's 2019 Profile Study: changes in local health department workforce and finance capacity since 2008. https://www.naccho.org/uploads/downloadable-resources/2019-Profile-Workforce-and-Finance-Capacity.pdf. Published May 2020. Accessed August 17, 2022.
- 5.Association of State and Territorial Health Officials. Data from: Profile of State and Territorial Public Health. Washington, DC: Association of State and Territorial Health Officials; 2019. [Google Scholar]
- 6.National Association of County & City Health Officials. 2020 Forces of Change: The COVID-19 Edition. https://www.naccho.org/uploads/downloadable-resources/2020-Forces-of-Change-The-COVID-19-Edition.pdf?utm_campaign=2020+FOC+report. Published 2022. Accessed August 17, 2022.
- 7.Sterling P, Platt ML. Why deaths of despair are increasing in the US and not other industrial nations—insights from neuroscience and anthropology. JAMA Psychiatry. 2022;79(4):368–374. [DOI] [PubMed] [Google Scholar]
- 8.de Beaumont Foundation, Public Health National Center for Innovations. Staffing up: workforce levels needed to provide basic public health services for all Americans. https://debeaumont.org/wp-content/uploads/2021/10/Staffing-Up-FINAL.pdf. Published October 2021. Accessed August 17, 2022.
- 9.Public Health National Center for Innovations. Foundational Public Health Services. https://phnci.org/uploads/resource-files/FPHS-Factsheet-2022.pdf. Published February 2022. Accessed August 17, 2022.
- 10.de Beaumont Foundation. The impact of the COVID-19 pandemic: rising stress and burnout in public health. https://debeaumont.org/wp-content/uploads/dlm_uploads/2022/03/Stress-and-Burnout-Brief_final.pdf. Published 2022. Accessed August 17, 2022.
- 11.Levine H, Justice JB, Scorsone EA. Handbook of Local Government Fiscal Health. Burlington, MA: Jones & Bartlett; 2013. [Google Scholar]
- 12.Salge TO, Vera A. Small steps that matter: incremental learning, slack resources and organizational performance. Br J Manage. 2013;24(2):156–173. [Google Scholar]
- 13.Valdmanis VG, Rosko MD, Mutter RL. Hospital quality, efficiency, and input slack differentials. Health Serv Res. 2008;43(5, pt 2):1830–1848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mohr DC, Young GJ. Slack resources and quality of primary care. Med Care. 2012;50(3):203–209. [DOI] [PubMed] [Google Scholar]
- 15.Ng A, Wang WM. Slack resources and quality performance: case of a mega health care organization. Int J Qual Reliab Manage. 2018;35(5):1060–1074. [Google Scholar]
- 16.McCullough JM, Fowle N, Sylvester T, et al. Cost analysis of 3 concurrent public health response events: financial impact of measles outbreak, Super Bowl surveillance, and Ebola surveillance in Maricopa County. J Public Health Manag Pract. 2019;25(4):357–365. [DOI] [PubMed] [Google Scholar]
- 17.Robins M, Leider JP, Schaffer K, Gambatese M, Allen E, Hare Bork R. PH WINS 2021 methodology report. J Public Health Manag Pract. 2023;29(suppl 1):S35–S44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Meit M, Sellers K, Kronstadt J, et al. Governance typology: a consensus classification of state-local health department relationships. J Public Health Manag Pract. 2012;18(6):520–528. [DOI] [PubMed] [Google Scholar]
- 19.Leider JP, Pineau V, Bogaert K, Ma Q, Sellers K. The methods of PH WINS 2017: approaches to refreshing nationally representative state-level estimates and creating nationally representative local-level estimates of public health workforce interests and needs. J Public Health Manag Pract. 2019;25:S49–S57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clements L, Baum C. A qualitative analysis of local health departments' experiences with contact-tracing tools in response to COVID-19. J Public Health Manag Pract. 2022;28(1):101–103. [DOI] [PubMed] [Google Scholar]
- 21.McCullough JC, Zimmerman FJ, Fielding JE, Teutsch SM. A health dividend for America: the opportunity cost of excess medical expenditures. Am J Prev Med. 2012;43(6):650–654. [DOI] [PubMed] [Google Scholar]
- 22.Czeisler MÉ, Marynak K, Clarke KEN, et al. Delay or avoidance of medical care because of COVID-19–related concerns—United States, June 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1250–1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.World Health Organization. Pulse survey on continuity of essential health services during the COVID-19 pandemic. https://www.who.int/docs/default-source/coronaviruse/finalupdate_22-april-2021_summary-ppt_ehs-pulse-survey_second-round.pdf?sfvrsn=a965e121_8. Published April 16, 2021.
- 24.Dayan GH, Ortega-Sánchez IR, LeBaron CW, Quinlisk MP. The cost of containing one case of measles: the economic impact on the public health infrastructure—Iowa, 2004. Pediatrics. 2005;116(1):e1–4. [DOI] [PubMed] [Google Scholar]