Abstract
Background and purpose
In patients around retirement age controversy exists as to whether to treat displaced femoral neck fracture (dFNF) with internal fixation (IF) or arthroplasty. An arthroplasty in this age group may need revision due to a long expected remaining lifetime. IF carries a higher risk of early failure but a maintained native hip if healing occurs. We aimed to determine the cumulative 5-year rate of conversion to arthroplasty after IF and implant revision after primary total hip arthroplasty (THA), respectively.
Patients and methods
In this longitudinal cohort study, patients aged 60–69 years registered with a dFNF in the Swedish Fracture Register (SFR) 2012–2018 were cross-referenced with available data from the Swedish Arthroplasty Register (SAR) until December 31, 2019. Conversion to arthroplasty or revision were analyzed utilizing competing risk, with death as competing event.
Results
At 5 years, the cumulative rate of conversion to arthroplasty after IF was 31% (95% confidence interval [CI] 26–37). For primary THA, the 5-year rate of revision was 4.0% (CI 2.8–5.8). The 5-year mortality did not differ, being 20% (CI 16–27) and 23% (CI 20–28) after IF and THA, respectively. Regression analyses did not identify any risk factors for conversion arthroplasty based on the variables in the register.
Conclusion
A follow-up of 5 years catches most reoperations after IF, resulting in a 31% conversion rate. The 4% revision rate at 5 years after primary THA should be seen as an intermediate result, as late complications may occur.
Hip arthroplasty is regarded as the gold standard for treatment of displaced femoral neck fractures (dFNF) in the elderly, whilst internal fixation (IF) is the preferred method for younger patients [1]. Traditionally, the Scandinavian countries have been more prone to treat with IF primarily and to perform secondary arthroplasty in case of failed fixation. Over the last decades, the age limit for arthroplasty as primary treatment for dFNF has gradually decreased in Scandinavia from around 70 to 60 years [2-4]. In Sweden, primary total hip arthroplasty (THA) is now the most common treatment choice in the current age group [5].
The potential benefits from preserving the femoral head after a fixed, healed fracture are weighted against the known high risk of reoperation due to healing disturbances [6], which might lead to pain and prolonged inactivity before the decision to reoperate is taken. In addition, a conversion arthroplasty may be associated with poorer results than THA as primary treatment [7]. Arthroplasty as primary treatment leads to significantly fewer major reoperations than IF, but poorer outcome than elective THA for osteoarthritis [8,9]. In younger age groups, an arthroplasty may need revision due to a long expected remaining lifetime [10]. In a previous study, we could not detect any differences between IF and THA as primary treatment in patients aged 60–69 years regarding crude mortality or patient satisfaction [11].
Arthroplasty as primary treatment for geriatric patients with dFNF is supported by several randomized controlled studies (RCTs) [12-14], but controversy still exists for patients around retirement age. IF can be defended, as more healthy and active individuals can better tolerate secondary surgery in the case of fixation failure. Successful fracture healing may give the patient the benefit from a maintained native hip joint, thus avoiding implant-related complications associated with arthroplasty.
We aimed to describe the cumulative rate of conversion/revision arthroplasty and mortality within 5 years after IF and primary THA, respectively but not to compare treatments as such. Secondarily, we analyzed risk factors for reoperations.
Patients and methods
Study design
This register-based cohort study was based on prospectively collected data from the Swedish Fracture Register (SFR) and the Swedish Arthroplasty Register (SAR). The STROBE guidelines were followed for reporting of the present study [15].
Setting
The SFR was initiated in 2011 [16], and over 810,000 fractures have been registered at the time of writing. The coverage has gradually improved due to a stepwise introduction and since 2021 all orthopedic departments in Sweden participate in the register, i.e., 100% coverage. During the study period 2012–2018, the completeness of hip fracture registrations in the SFR increased from 18% to 55% compared with the National Patient Register [17], due to the stepwise activation of more hospitals. The SFR has decided to continue with the 2007 AO/OTA classification, to maintain longitudinally homogeneous data. Thus, FNFs are classified accordingly as undisplaced or minimally displaced subcapital (31-B1), basicervical (31-B2), and displaced subcapital (31-B3) [18]. Each treating physician registers data on patient level for the injury, fracture classification, and treatment through a secure web-based portal. SAR is the national quality register for arthroplasty of the hip and knee in Sweden. The coverage of SAR is 100% of all departments performing hip arthroplasties, both public and private. For the study period, the completeness was 98% for THA and 92% regarding revisions of THA [19]. The registers are updated concerning date of death by regular co-processing every 24 hours with the population register (the Swedish Tax Agency).
Patients
Data for all patients aged 60–69 years at injury and registered with an FNF (defined by the ICD code S72.00) in SFR from 2012 to 2018 were extracted and cross-referenced with available data from SAR for each individual from the date of the index fracture until December 31, 2019. To provide trustable co-processing between registers regarding subsequent surgeries and/or death, the unique personal identity number given to each Swedish citizen was used. The dFNFs (AO/OTA 31-B3, Garden 3–4) were further examined for eligibility and other fracture types were excluded. Only the first registered hip fracture for each individual was included in the study; contralateral and subsequent ipsilateral fractures and duplicate registrations were excluded. Pathological, stress, and spontaneous fractures were identified by their ICD-10 diagnosis codes (M84.4, M84.8, M84.3) in the injury mechanism registration and excluded. Patients with treatment other than IF or primary THA, e.g., intramedullary nail, excision arthroplasty (Girdlestone procedure), and hemiarthroplasty, were also excluded from analysis. Based on the registered primary treatment, fractures treated with either IF (parallel pins/screws, sliding hip screw) or THA were identified and analyzed (Figure 1).
Figure 1.
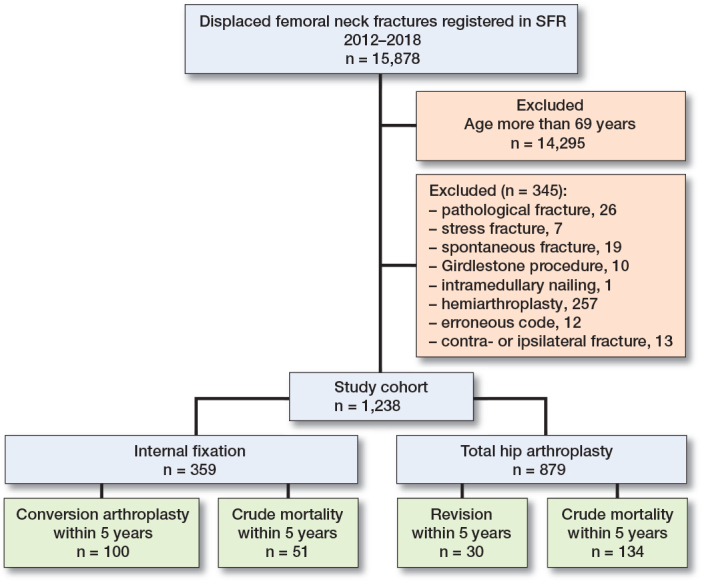
Flowchart of study cohort.
For patients treated with IF, the studied reoperations were limited to conversion arthroplasty. Screw extraction, which is a common (minor) reoperation after IF [12], was omitted here as such procedures also may be undertaken in cases of uneventful healing, due to local irritation. For arthroplasty, only revisions, i.e., exchange or extraction of any implant, were included.
Study variables
Basic demographic variables (age, sex, and trauma mechanism), data on the primary fracture treatment (surgeon experience defined as performed by either a resident or consultant orthopedic surgeon), and any date of death were extracted from the SFR. The SAR was sought for the occurrence of any conversion to arthroplasty after IF or primary THA revision. Length of follow-up was defined as time from injury date to date of death or end of study period on December 31, 2019.
Study outcomes
The main outcomes were either conversion to arthroplasty after IF or revision of a primary THA, both at 5 years. For primary THA, we used treatment codes indicating revision (NFU09, NFU19, NFCxx) in the SAR to identify major revisions. We also assessed mortality within a competing risk regression model.
Statistics
Patient characteristics were described using frequencies with proportions and interquartile range (IQR). We analyzed the time from IF to death, to conversion arthroplasty, or until end of study, whichever came first, and time from THA to death, to revision, or until end of study period, whichever came first. Patients who either died or who were still alive without any conversion arthroplasty/revision at the end of the study were censored.
Cox regression was utilized to explore associations between secondary surgery (conversion/revision) and risk factors available in the register data: sex (categorical), age (continuous), and treating surgeon (factorial—resident vs. consultant). Schoenfeld’s test for proportionality assumption was utilized.
Competing risk analysis was used to estimate conversion arthroplasty after IF, revision surgery after THA, and mortality in the two treatment groups respectively. Cumulative incidence functions (CIF) are presented with 95% confidence intervals (CI). Competing risk analysis was done utilizing the “cmprsk” package in R version 4.0.2 (R Foundation for Statistical Computing, Vienna, Austria).
Ethics, data sharing, funding, and disclosures
Ethical approval was granted from the Central Ethical Review Board in Gothenburg (ref. 830-17) and from the Swedish Ethical Review Authority (diary number 2019-05024, 2022-00972-02). To ensure confidentiality for patients included in this study, the dataset is not publicly available. This is a requirement for ethical approval and is also regulated by the law on public access and secrecy; Chapter 21, §7, Chapter 25, §1 (https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/offentlighets-och-sekretesslag-2009400_sfs-2009-400). Requests to access this data should go through the senior author and/or Lund University to ensure proper measures are taken in conjunction with the legislation as well as the ethical approval. Any sharing of data beyond what is presented in this paper will involve approval from the Swedish Ethical Review Authority.
Funding was received from the independent trusts Axel Linder Foundation and Greta & Johan Kock Foundation, and the Swedish Research Council funding for clinical research in medicine (ALF). Completed disclosure forms for this article following the ICMJE template are available on the article page, doi: 10.2340/17453674.2023.20284
Results
Patients
15,878 dFNFs were found in the SFR. After exclusion, 1,238 patients treated with either IF (n = 359) or THA (n = 879) were analyzed (Figure 1). Median age was slightly higher in patients treated with THA and this treatment was also more common in women. The fracture was caused by low-energy trauma in more than 9 out of 10 cases (Table 1).
Table 1.
Characteristics of patients included in the study. Values are count (%) unless otherwise specified
| Characteristics | Internal fixation (n = 359) | Total hip arthroplasty (n = 879) |
|---|---|---|
| Median age (IQR) | 64 (62–67) | 67 (64–68) |
| Women | 180 (50) | 563 (64) |
| Trauma type | ||
| High-energy trauma | 14 (4.0) | 20 (2.0) |
| Low-energy trauma | 319 (89) | 813 (92) |
| Missing data/unknown | 26 (7.0) | 46 (5.0) |
| Primary treatment | ||
| Parallel hook pins (2 pins) | 176 (49) | – |
| Parallel hook pins (> 2 pins) | 16 (4.5) | – |
| Wires or cerclage | 6 (1.7) | – |
| Parallel screws (2 screws) | 130 (36) | – |
| Parallel screws (> 2 screws) | 7 (1.9) | – |
| Sliding hip screw | 24 (6.7) | – |
| Uncemented THA | – | 33 (3.8) |
| Hybrid THA | – | 60 (6.8) |
| Cemented THA | – | 786 (89) |
IQR = interquartile range.
Conversion to arthroplasty after IF
The rate of conversion to arthroplasty after IF was 18% (CI 14–22) at 1 year (Figure 2, Table 2). The crude rate was 63 of 359 patients. At 5 years the cumulative rate increased to 31% (CI 26–37) with a crude rate of 100 of 359 patients.
Figure 2.

Competing risk analysis of conversion to arthroplasty after IF as primary treatment.
Table 2.
Conversion to arthroplasty and mortality after internal fixation (IF) as primary treatment
| Years | At risk | Conversion to arthroplasty after IF | Mortality | ||
|---|---|---|---|---|---|
| Cumulative events | CIF (CI) (%) | Cumulative events | CIF (CI) (%) | ||
| 1 | 274 | 63 | 18 (14–22) | 22 | 6.1 (4.1–9.2) |
| 2 | 189 | 88 | 25 (21–31) | 30 | 8.6 (6.1–12) |
| 3 | 143 | 95 | 28 (24–33) | 36 | 11 (7.9–15) |
| 4 | 91 | 98 | 30 (25–35) | 44 | 15 (11–20) |
| 5 | 46 | 100 | 31 (26–37) | 51 | 21 (16–27) |
CIF = cumulative incidence function.
Revision of primary THA
In the group treated with primary THA, the cumulative rate of revision was 2% (CI 1–3) at 1 year. The crude rate was 16 of 879 patients. At 5 years it increased to 4% (CI 3–6) with a crude rate of 30 of 879 patients (Figure 3, Table 3).
Figure 3.

Competing risk analysis of revision after THA as primary treatment.
Table 3.
Major revisions and mortality after total hip arthroplasty (THA) as primary treatment
| Years | At risk | Revision after THA | Mortality | ||
|---|---|---|---|---|---|
| Cumulative events | CIF (CI) (%) | Cumulative events | CIF (CI) (%) | ||
| 1 | 834 | 16 | 1.8 (1.1–3,0) | 28 | 3.2 (2.2–4.6) |
| 2 | 640 | 25 | 2.9 (2.0–4.3) | 63 | 7.5 (5.9–9.6) |
| 3 | 435 | 27 | 3.2 (2.2–4.7) | 97 | 13 (11–16) |
| 4 | 279 | 29 | 3.7 (2.6–5.4) | 120 | 18 (16–22) |
| 5 | 162 | 30 | 4.0 (2.8–5.8) | 134 | 23 (20–28) |
CIF = cumulative incidence functions.
Mortality
The 1- and 5-year mortality was 6% (CI 4–9) and 20% (CI 16–27) in the IF group and 3% (CI 2–5) and 23% (CI 20–28) in the THA group, respectively (Tables 2 and 3).
Risk factors for reoperation
Neither sex, age, nor surgeon experience interfered with the risk of secondary surgery in a Cox regression analysis (Table 4).
Table 4.
Cox regression with hazard ratios (HR) for conversion after internal fixation (IF) and revision after total hip arthroplasty (THA)
| IF HR (CI) | THA HR (CI) | |
|---|---|---|
| Age | 0.99 (0.98–1.1) | 1.0 (0.87–1.1) |
| Male sex | 0.71 (0.48–1.1) | 0.92 (0.43–2.0) |
| Specialist surgeon | 1.2 (0.81–1.9) | 0.64 (0.28–1.4) |
Discussion
We aimed to describe the cumulative rate of conversion/revision arthroplasty and mortality within 5 years after IF and primary THA. We found that, within 5 years, nearly one-third of the patients treated with IF underwent conversion to arthroplasty, whereas only 4% of those treated with primary THA underwent revision. Due to the different nature of the methods, the aim was not to compare them. IF may be a joint-preserving option with conversion arthroplasty as an established salvage procedure. However, from a patient’s point of view, the period leading up to any reoperation will be painful and disabling. THA as acute primary treatment will on the other hand sacrifice the joint, including in those whose fracture would have healed if treated with IF [12]. Within 5 years, most complications after IF are identified [12]. After THA, late complications such as aseptic loosening and late-presenting periprosthetic fractures, and dislocations due to wear may occur, and a follow-up of up to 20 years is warranted to establish a true revision rate [12].
When comparing literature on IF with our results, we found comparable conversion rates. Bartels et al. [3] reported conversion rates of 27% for patients treated with IF for dFNF within 5 years, also utilizing a competing risk analysis. A Danish register study reported a 19% reoperation rate after IF within 1 year [4]. In contrast, RCTs show higher 2-year reoperation rates of 37–51% [20,21]. The difference may represent a selection of patients or fractures more suitable for IF or THA in clinical practice reflected in the observational register studies.
Our results on THA as acute treatment align well with a Norwegian register study reporting 2.8% revisions within 5 years [3]. A systematic review found a pooled revision rate of 1.18 per 100 component years for THA in the hip fracture population [22]. Applied to our data this would predict close to 6% revisions within 5 years for patients treated with THA assuming linearity. In RCTs, the reoperation rate is reported as 4–9% at 2 years, with a somewhat wider definition of “major reoperations” [20,21].
The disadvantages of a conversion arthroplasty in terms of poorer surgical results than primary arthroplasty [7,23] is questioned by some studies [24-26]. Regardless, the main concern must be the loss of health-related quality-of-life during the period leading up to conversion arthroplasty [7].
From a clinical perspective, the fact that 2 out of 3 patients in this age group kept their native hip joint after 5 years could be interpreted as promising. We cannot assess their function or perceived pain based on our data, but in a previous study on the same age group we found no differences in patient-reported outcome between IF and primary THA [11].
So how should the risk of reoperation be weighed when initial treatment is chosen? Clinical variables such as comorbidity, activity, and the patient’s preferences play a role in determining whether he or she is a candidate for IF or not. The gradually lower age threshold for primary THA [5] may seem contradictory to longer life span and healthier older years. One can expect more retirees to perform sports and maintain a physically active lifestyle. Also, the focus on patient-centered care puts more emphasis on the surgeon being able to inform and share the treatment decision with the patient to best meet his or her expectations.
The age threshold for IF versus arthroplasty varies internationally. When designing this study, we conducted an informal survey sent to orthopedic trauma centers reporting to the SFR on how they allocate to the different treatments. Most of the 23 centers that answered used a mean age cut-off of 65 years for IF, whereby older patients would be treated with arthroplasty.
Regardless of surgical procedure, surgical skills are essential. As poor reduction quality is reported in recent studies [4,20], one can speculate in whether reduction and IF of a dFNF has become so rare a procedure that surgeons have lost their skills to handle it.
Strength and limitations
A strength of the study is that the surgical outcome is derived from a national register with high completeness and the excellent reliability of death dates.
A limitation is that the 5-year follow-up does not address the concerns of a poorer long-term prognosis for those treated with a primary THA [12]. Ideally, a comorbidity index and data on pre-fracture activity would have shed more light on how the 2 treatment methods were chosen, but such data is not available in the SFR. The initially low completeness of the SFR might lead to some bias, as not all Swedish trauma centers contributed during the first years. Nevertheless, the outcome was retrieved from the SAR, a register with a stable and high completeness and coverage.
As with all register-based data, the risk for residual confounding is apparent and when comparing implants and any differences in mortality should be interpreted more as a sign of residual confounding than an effect of the implant per se [27]. If the surgeon based the implant choice on patient factors like vitality or level of physical activity, this selection bias will overshadow inherent implant characteristics, interfering with the risk. Predictors available in our data such as sex, age, and surgeon experience have previously been associated with risk for reoperation and mortality. Also, there is a risk of selection and indication bias for who gets a conversion to arthroplasty, where frailer patients might be considered for minor reoperations or nonoperative treatment. However, in the current group, the young old, we believe this to be less of an issue than in older cohorts.
Conclusion
IF for dFNF carries a significant risk of complications even in the young old, around retirement age. In our study, one-third of patients needed conversion arthroplasty within 5 years. When patients received THA as primary treatment, 1 in 25 needed revision surgery in the same time span. Due to different surgical magnitude, the methods are not directly comparable, but the risk of secondary surgery should be considered when discussing treatment options with patients in this age group.
JL: author, study design, data acquisition, curation, and interpretation. SSR: author, data interpretation. OW: author, data interpretation. SM: author, data interpretation, study design. MM: author, draft manuscript preparation and project supervision. JN: data acquisition, statistics and interpretation of data. CR: author, study design, data acquisition, interpretation of data. project supervision.
The authors express their gratitude to Emma Nauclér for initial data curation. They would like to thank the SFR administrative staff, Monica Sjöholm and Karin Petterson, as well as all surgeons and other healthcare personnel who report to the SFR and SAR, and, finally, participating patients.
Handling co-editors: Bart Swierstra and Robin Christensen
Acta thanks JLC van Susante and Sarunas Tarasevicius for help with peer review of this manuscript.
References
- 1.Ftouh S, Morga A, Swift C, Guideline Development Group . Management of hip fracture in adults: summary of NICE guidance. BMJ 2011; 342: d3304. doi: 10.1136/bmj.d3304. [DOI] [PubMed] [Google Scholar]
- 2.Al-Ani A N, Neander G, Samuelsson B, Blomfeldt R, Ekstrom W, Hedstrom M. Risk factors for osteoporosis are common in young and middle-aged patients with femoral neck fractures regardless of trauma mechanism. Acta Orthop 2013; 84(1): 54-9. doi: 10.3109/17453674.2013.765639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bartels S, Gjertsen J E, Frihagen F, Rogmark C, Utvag S E. High failure rate after internal fixation and beneficial outcome after arthroplasty in treatment of displaced femoral neck fractures in patients between 55 and 70 years. Acta Orthop 2017: 1-6. doi: 10.1080/17453674.2017.1376514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nyholm A M, Palm H, Sandholdt H, Troelsen A, Gromov K, DFDB Collaborators . Risk of reoperation within 12 months following osteosynthesis of a displaced femoral neck fracture is linked mainly to initial fracture displacement while risk of death may be linked to bone quality: a cohort study from Danish Fracture Database. Acta Orthop 2020; 91(1): 1-75. doi: 10.1080/17453674.2019.1698503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Swedish Fracture Register Annual Report 2022 (in Swedish). Available from: https://registercentrum.blob.core.windows.net/sfr/r/-rsrapport-SFR-2022-By_ps8PU3.pdf.
- 6.Mahmoud S S, Pearse E O, Smith T O, Hing C B. Outcomes of total hip arthroplasty, as a salvage procedure, following failed internal fixation of intracapsular fractures of the femoral neck: a systematic review and meta-analysis. Bone Joint J 2016; 98-B(4): 452-60. doi: 10.1302/0301-620X.98B4.36922. [DOI] [PubMed] [Google Scholar]
- 7.Blomfeldt R, Tornkvist H, Ponzer S, Soderqvist A, Tidermark J. Displaced femoral neck fracture: comparison of primary total hip replacement with secondary replacement after failed internal fixation: a 2-year follow-up of 84 patients. Acta Orthop 2006; 77(4): 638-43. doi: 10.1080/17453670610012728. [DOI] [PubMed] [Google Scholar]
- 8.Le Manach Y, Collins G, Bhandari M, Bessissow A, Boddaert J, Khiami F, et al. Outcomes after hip fracture surgery compared with elective total hip replacement. JAMA 2015; 314(11): 1159-66. doi: 10.1001/jama.2015.10842. [DOI] [PubMed] [Google Scholar]
- 9.Qin C D, Helfrich M M, Fitz D W, Hardt K D, Beal M D, Manning D W. The Lawrence D. Dorr Surgical Techniques & Technologies Award: Differences in postoperative outcomes between total hip arthroplasty for fracture vs osteoarthritis. J Arthroplasty 2017; 32(9S): S3-S7. doi: 10.1016/j.arth.2017.01.049. [DOI] [PubMed] [Google Scholar]
- 10.Nugent M, Young S W, Frampton C M, Hooper G J. The lifetime risk of revision following total hip arthroplasty. Bone Joint J 2021; 103-B(3): 479-85. doi: 10.1302/0301-620X.103B3.BJJ-2020-0562.R2. [DOI] [PubMed] [Google Scholar]
- 11.Lagergren J, Möller M, Rogmark C. Displaced femoral neck fractures in patients 60–69 years old: treatment and patient reported outcomes in a register cohort. Injury 2020; 51(11): 2652-7. doi: 10.1016/j.injury.2020.08.004. [DOI] [PubMed] [Google Scholar]
- 12.Chammout G K, Mukka S S, Carlsson T, Neander G F, Stark A W, Skoldenberg O G. Total hip replacement versus open reduction and internal fixation of displaced femoral neck fractures: a randomized long-term follow-up study. J Bone Joint Surg Am 2012; 94(21): 1921-8. doi: 10.2106/JBJS.K.01615. [DOI] [PubMed] [Google Scholar]
- 13.Johansson T. Internal fixation compared with total hip replacement for displaced femoral neck fractures: a minimum fifteen-year follow-up study of a previously reported randomized trial. J Bone Joint Surg Am 2014; 96(6): e46. doi: 10.2106/JBJS.K.00244. [DOI] [PubMed] [Google Scholar]
- 14.Leonardsson O, Sernbo I, Carlsson A, Akesson K, Rogmark C. Long-term follow-up of replacement compared with internal fixation for displaced femoral neck fractures: results at ten years in a randomised study of 450 patients. J Bone Joint Surg Br 2010; 92(3): 406-12. doi: 10.1302/0301-620X.92B3.23036. [DOI] [PubMed] [Google Scholar]
- 15.von Elm E, Altman D G, Egger M, Pocock S J, Gotzsche P C, Vandenbroucke J P, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 2007; 370(9596): 1453-7. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 16.Moller M, Wolf O, Bergdahl C, Mukka S, Rydberg E M, Hailer N P, et al. The Swedish Fracture Register: ten years of experience and 600,000 fractures collected in a National Quality Register. BMC Musculoskelet Disord 2022; 23(1): 141. doi: 10.1186/s12891-022-05062-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bergdahl C, Nilsson F, Wennergren D, Ekholm C, Moller M. Completeness in the Swedish Fracture Register and the Swedish National Patient Register: an assessment of humeral fracture registrations. Clin Epidemiol 2021; 13: 325-33. doi: 10.2147/CLEP.S307762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marsh J L, Slongo T F, Agel J, Broderick J S, Creevey W, DeCoster T A, et al. Fracture and dislocation classification compendium—2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma 2007; 21(10 Suppl.): S1-133. doi: 10.1097/00005131-200711101-00001. [DOI] [PubMed] [Google Scholar]
- 19.W-Dahl A, Kärrholm J, Rogmark C, Nauclér E, Nåtman J, Bülow E, et al. The Swedish Arthroplasty Register: Annual report 2021. doi: 10.18158/SyZ333H5F. Available from: https://registercentrum.blob.core.windows.net/slr/r/SAR-Annual-Report-2021-SJlAFmlRl5.pdf. [DOI] [Google Scholar]
- 20.Bartels S, Kristensen T B, Gjertsen J E, Frihagen F, Rogmark C, Dolatowski F C, et al. Total hip arthroplasty leads to better results after low-energy displaced femoral neck fracture in patients aged 55 to 70 years: a randomized controlled multicenter trial comparing internal fixation and total hip arthroplasty. J Bone Joint Surg Am 2022; 104(15): 1341-51. doi: 10.2106/JBJS.21.01411. [DOI] [PubMed] [Google Scholar]
- 21.Keating J F, Grant A, Masson M, Scott N W, Forbes J F. Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty: treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Joint Surg Am 2006; 88(2): 249-60. doi: 10.2106/JBJS.E.00215. [DOI] [PubMed] [Google Scholar]
- 22.Hauer G, Heri A, Klim S, Puchwein P, Leithner A, Sadoghi P. Survival rate and application number of total hip arthroplasty in patients with femoral neck fracture: an analysis of clinical studies and national arthroplasty registers. J Arthroplasty 2020; 35(4): 1014-22. doi: 10.1016/j.arth.2019.11.033. [DOI] [PubMed] [Google Scholar]
- 23.McKinley J C, Robinson C M. Treatment of displaced intracapsular hip fractures with total hip arthroplasty: comparison of primary arthroplasty with early salvage arthroplasty after failed internal fixation. J Bone Joint Surg Am 2002; 84(11): 2010-15. doi: 10.2106/00004623-200211000-00016. [DOI] [PubMed] [Google Scholar]
- 24.van Leent E A P, Schmitz P P, de Jong L D, Zuurmond R G, Vos C J, van Susante J L C, et al. Complications and survival of conversion to total hip arthroplasty after failed primary osteosynthesis compared to primary total hip arthroplasty in femoral neck fractures. Injury 2022; 53(8): 2853-8. doi: 10.1016/j.injury.2022.02.033. [DOI] [PubMed] [Google Scholar]
- 25.Leonardsson O, Rogmark C, Kärrholm J, Åkesson K, Garellick G. Outcome after primary and secondary replacement for subcapital fracture of the hip in 10 264 patients. J Bone Joint Surg Br 2009; 91(5): 595-600. doi: 10.1302/0301-620X.91B5.22224. [DOI] [PubMed] [Google Scholar]
- 26.Schmitz P P, Hannink G, Somford M P, Schreurs B W, Van Susante J L C. Revision risk of salvage compared with acute total hip arthroplasty following femoral neck fracture: an analysis from the Dutch Arthroplasty Register. Acta Orthop 2023; 94:399-403. doi: 10.2340/17453674.2023.17743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hansson S, Bulow E, Garland A, Kärrholm J, Rogmark C. More hip complications after total hip arthroplasty than after hemi-arthroplasty as hip fracture treatment: analysis of 5,815 matched pairs in the Swedish Hip Arthroplasty Register. Acta Orthop 2020; 91(2): 133-8. doi: 10.1080/17453674.2019.1690339. [DOI] [PMC free article] [PubMed] [Google Scholar]


