Abstract
Objective
This study aimed to investigate the association of reproductive hormones with primary dysmenorrhea in Chinese women.
Methods
A case–control study was conducted and patients with primary dysmenorrhea and non-dysmenorrhea participants were recruited. Oxytocin, PGF2α, vasopressin, estriol and estradiol were respectively measured in plasma collected three to five days after menstruation. Restricted cubic spline and multiple logistic regression models were adopted to analyze the association between hormones and primary dysmenorrhea.
Results
There were 604 participants enrolled in our study including 300 patients with primary dysmenorrhea. After adjustment for the potential confounders, oxytocin levels (Q3: OR (95% CI) = 0.50 (0.27~0.95) (p=0.035); Q4: 0.34 (0.17~0.66) (p=0.001)) and PGF2α levels (Q3: 0.45 (0.24~0.87) (p=0.017); Q4: 0.43 (0.22~0.84) (p=0.013)) were respectively associated with an decreased risk of primary dysmenorrhea, but estradiol (Q2: 2.18 (1.13~4.19) (p=0.020); Q3: 2.17 (1.12~4.19) (p=0.022)) and vasopressin (Q3: 2.88 (1.48~5.63) (p=0.002); Q4: 3.20 (1.65~6.22) (p<0.001)) with an increased risk of primary dysmenorrhea, respectively. Among patients with primary dysmenorrhea, the higher estriol level was associated with higher frequent dysmenorrhea (Q2: 3.12 (1.32~7.34) (p=0.009); Q3: 4.97 (2.08~11.85) (p<0.001)) and always dysmenorrhea (Q2: 2.51 (1.03~6.11) (p=0.041); Q3: 3.10 (1.25~7.73) (p=0.015)). Similarly, high estriol levels were associated with the higher degree of pain significantly only when hormone levels were at a high level (Q3: 2.06 (1.03~4.18) (p=0.043)).
Conclusion
Higher serum vasopressin and estradiol concentrations as well as lower oxytocin and PGF2α levels were associated with higher risk of primary dysmenorrhea. Estrogen showed a reverse U-shape association on the frequency and degree of pain among patients with primary dysmenorrhea.
Keywords: primary dysmenorrhea, reproductive hormone, restricted cubic spline
Introduction
Primary dysmenorrhea is defined as one type of dysmenorrhea without organic lesions in female reproductive organs.1 Menstrual pain mainly occurs in the lower abdomen, and the main symptoms are spasmodic pain possibly followed by abdominal distention, fatigue, headache, nausea, etc.2 Moderate and severe dysmenorrhea has even become a major reason for work absence and physical activity limitation in young women. The prevalence of dysmenorrhea in young women ranges from 45.0% to 94.0% in countries worldwide.3–6 The prevalence reported among college women in China is approximately from 41.7% to 90.9%,7,8 while it was lower in married women.9
The occurrence of primary dysmenorrhea is influenced by many factors such as diet, exercise,10 emotion,11 genetics, hormones, and so on, while adverse life behaviors as well as mental conditions will lead to increase frequency and severity of diseases.12,13 Some lifestyles and complementary therapies can decrease the pain level.14,15 As for reproductive hormones, the development of dysmenorrhea was affected by prostaglandin, estrogen, oxytocin, vasopressin, etc. Many studies reported that primary dysmenorrhea was the result of increased prostaglandin, especially prostaglandin F2α (PGF2α) and prostaglandin E2 (PGE2) which produced the effect through the cyclooxygenase pathway, and further led to uterine ischemia hypoxia.16,17 Oxytocin secretion also stimulated uterine smooth muscle contraction by a biochemical pathway to aggravate dysmenorrhea and promoted to secrete prostaglandin synthase which resulted in primary dysmenorrhea exacerbation and hyperalgesia.18 However, other recent studies supported that compared to healthy women, patients with dysmenorrhea had lower serum oxytocin concentrations.19,20 On the other hand, some studies considered that vasopressin might be onset of dysmenorrhea by the uterine muscle contraction and promote prostaglandin synthesis the same as oxytocin.21 Estrogen including estriol and estradiol was considered to be related to endometriosis as well as secondary dysmenorrhea, although the conclusion was still contradictory.22,23 Nevertheless, the relationship between reproductive hormones and primary dysmenorrhea was not completely clear. Hence, this study aims to investigate the association of oxytocin, PGF2α, vasopressin and estrogen with primary dysmenorrhea.
Methods
Study Population
This study was a case–control study, and patients with primary dysmenorrhea and non-dysmenorrhea who visited the gynecological clinic in Yiwu Maternity and Children Hospital in Zhejiang, China from March 2019 to February 2020 were recruited. In our study, the inclusion criteria of the case group (patients with primary dysmenorrhea) were: (1) agreed to participate in this study and signed the informed consents; (2) aged from 18 to 40 years; (3) not menopausal yet; (4) accorded with the diagnostic criteria of primary dysmenorrhea ((i) onset within 1~2 years after menarche; (ii) pain occurs at or hours before menstrual blood with less than 48~72 hours pain time; (iii) spasmodic pain or similar to labor pain; (iV) bimanual examination or rectal examination negative; and (v) no organic lesions in pelvic cavity); (5) history of recurrent dysmenorrhea; and (6) visiting the clinic at three to five days after menstruation occurrence. The exclusion criteria of the case group were: (1) serious primary diseases of cardiovascular, liver, kidney, and hemopoietic system, or mental disease and other patients unable to cooperate with treatment; (2) patients under hormone therapy, chemotherapy or radiotherapy; (3) any history of pelvic surgery; (4) secondary dysmenorrhea; (5) females with Mullerian anomaly or any congenital condition; and (6) reproductive tract anomalies. The inclusion criteria of the control group were: (1) agreed to participate in this study and signed the informed consents; (2) aged from 18 to 40 years; (3) without primary dysmenorrhea; and (4) visiting clinic at three to five days after menstruation occurrence. The exclusion criteria of control group were the same as those of the case group.
Information and Blood Sample Collection
The information of participants was collected by a well-trained nurse with a questionnaire including the following three parts: (1) information about dysmenorrhea including occurrence of dysmenorrhea, frequency, degree and type of pain, and menstrual related symptoms; (2) basic information of participants including age, menarche age, menstrual duration, menstrual cycles, sanitary pad consumption; and (3) lifestyle including diet and sleeping habits, physical activity, mental conditions and dysmenorrhea history of mother. In addition, 5 mL fasting venous blood of participants would be collected at three to five days after menstruation occurrence, while the plasma and leukocytes were separated and saved under −80 °C until use.
Measurement of Plasma Hormones
In plasma, oxytocin, estriol, PGF2α and vasopressin were measured by ELISA (Miblo, Shanghai, China) while estradiol was measured by automatic immune analyzer (Beckman Coulter, Danaher Corporation, Brea, CA, USA) through competitive binding enzyme immunochemiluminescence. All plasma hormone concentrations were reported in pg/mL. Both coefficients of variation of hormone detection between-group and within-group were less than 5%.
Variable Definition
The primary dysmenorrhea frequency was divided into three levels (Occasional: ≤6 times/year; Frequent: 7~11 times/year; Always: ≥12 times/year). The degree of pain was divided into three types (Low: pain did not influence daily life and did not need painkillers; Moderate: pain influenced daily life slightly and needed painkillers; High: general pain with poor analgesic effect). Considering the abnormal distributions of hormone (oxytocin, PGF2α, vasopressin, estriol and estradiol) concentrations, the hormone levels were categorized into four groups by quartile (Q1~Q4). The mental conditions including life/work mental stress, angry, worried, anxiety, irritability and depression were defined as the frequency of mental stress in daily life among participants. Sleep quality was defined as the condition of insomnia or other sleep disorders. Dysmenorrhea history of mother was defined as the dysmenorrhea condition of mothers in their youth.
Statistical Analysis
Data were input and processed by EpiData. Mean and standard deviation (mean ± SD) were used to present continuous variables (medium and quartile for non-normal distributed variables) while frequency and percentage (%) were used for categorical variables for describing social demographic data of participants. Continuous and categorical variables were analyzed by Student’s t-test (Wilcoxon rank-sum test for non-normal distribution data instead) and chi-square test, respectively. To assess the non-linear relationship between five different hormones and primary dysmenorrhea as well as the degree of pain, we used restricted cubic spline (RCS) analysis with predefined knots at the 25th, 50th and 75th percentiles of hormones. The multiple logistic regression model was adopted to detect the association of five reproductive hormones (quartile) with the risk of primary dysmenorrhea after adjustment for age, raw or cold food consumption, tea, coffee or wine consumption, cold bathing, sleep quality, vigorous sports during menstrual period, angry, anxiety, and dysmenorrhea history of mother. Additionally, the multiple logistic regression model was adopted to detect the association of five reproductive hormones (quartile) with the frequency and degree of pain of primary dysmenorrhea after adjustment for the following covariates: age, raw or cold food consumption, tea, coffee or wine consumption, cold bathing, sleep quality, vigorous sports during menstrual period, angry, anxiety, and dysmenorrhea history of mother. Considering the very few patients with a high degree of pain, we combined high and moderate into one group in the logistic regression analysis. Furthermore, all of the statistical analysis was conducted by program package using R software (version 3.5.1). The P value less than 0.05 was considered as statistical significance.
Results
The Association of Reproductive Hormones with the Risk of Primary Dysmenorrhea
In our study, we enrolled 604 women finally, including 300 cases and 304 controls. The basic demographic characteristics of participants are exhibited in the Table 1. The average ages were 27.11 ± 6.78 years, while the case group was younger than the control group (P<0.001). However, the menarche age, menstrual duration, menstrual cycles and sanitary pad consumption showed no statistical difference between case and control groups (all P>0.05). Compared with the control group, women with primary dysmenorrhea suffered more from worse negative emotions, such as high life/work mental stress, angry, worried, anxiety, irritability and depression (all P<0.001). For life behavior and dietary habits, the case group consumed more raw or cold food, spicy food, vegetables and fruit; less tea, coffee or wine; and suffered more from staying up late, poor sleep quality and sedentary; compared with the control group (all P<0.01). Additionally, the mothers of the case group had higher dysmenorrhea history than those of the control group (P<0.001). However, regular diet habit, cold water shampoo, vigorous sports during menstrual period and physical activity showed no statistical difference between two groups.
Table 1.
Basic Demographic Characteristics of Study Participants
| Variables | Primary Dysmenorrhea | P | |||
|---|---|---|---|---|---|
| Participants (n=604) | Control (n=304) | Case (n=300) | |||
| Mean ± SD | |||||
| Age, years | 27.11 ± 6.78 | 29.73 ± 7.02 | 24.46 ± 5.36 | <0.001 | |
| Median (Q1, Q3) | |||||
| Menarche age, years | 13 (12, 14) | 13 (12, 15) | 13 (12, 14) | 0.649 | |
| Menstrual duration, day | 5 (4, 7) | 5 (4, 7) | 5 (4, 7) | 0.552 | |
| N (%) | |||||
| Menstrual cycle, days | 0.212 | ||||
| <21 | 46 (7.6) | 18 (5.9) | 28 (9.3) | ||
| 21~38 | 501 (82.9) | 254 (83.6) | 247 (82.3) | ||
| >38 | 57 (9.4) | 32 (10.5) | 25 (8.3) | ||
| Sanitary pad consumption, packs | 0.066 | ||||
| <=1/2 | 26 (4.3) | 12 (3.9) | 14 (4.7) | ||
| <1 | 170 (28.1) | 91 (29.9) | 79 (26.3) | ||
| 1~2 | 307 (50.8) | 152 (50.0) | 155 (51.7) | ||
| >2 | 72 (11.9) | 28 (9.2) | 44 (14.7) | ||
| Irregular | 29 (4.8) | 21 (6.9) | 8 (2.7) | ||
| Life/work mental stress | <0.001 | ||||
| Low | 42 (7.0) | 30 (9.9) | 12 (4.0) | ||
| Moderate | 506 (83.8) | 258 (84.9) | 248 (82.7) | ||
| High | 56 (9.3) | 16 (5.3) | 40 (13.3) | ||
| Angry | <0.001 | ||||
| Never | 61 (10.1) | 48 (15.8) | 13 (4.3) | ||
| Occasional | 432 (71.5) | 225 (74.0) | 207 (69.0) | ||
| Often | 111 (18.4) | 31 (10.2) | 80 (26.7) | ||
| Worried | <0.001 | ||||
| Never | 87 (14.4) | 58 (19.1) | 29 (9.7) | ||
| Occasional | 393 (65.1) | 213 (70.1) | 180 (60.0) | ||
| Often | 124 (20.5) | 33 (10.9) | 91 (30.3) | ||
| Anxiety | <0.001 | ||||
| Never | 95 (15.7) | 71 (23.4) | 24 (8.0) | ||
| Occasional | 426 (70.5) | 207 (68.1) | 219 (73.0) | ||
| Often | 83 (13.7) | 26 (8.6) | 57 (19.0) | ||
| Irritability | <0.001 | ||||
| Never | 101 (16.7) | 67 (22.0) | 34 (11.3) | ||
| Occasional | 405 (67.1) | 202 (66.4) | 203 (67.7) | ||
| Often | 98 (16.2) | 35 (11.5) | 63 (21.0) | ||
| Depression | <0.001 | ||||
| Never | 85 (14.1) | 65 (21.4) | 20 (6.7) | ||
| Occasional | 465 (77.0) | 221 (72.7) | 244 (81.3) | ||
| Often | 54 (8.9) | 18 (5.9) | 36 (12.0) | ||
| Raw or cold food consumption | <0.001 | ||||
| Never | 67 (11.1) | 55 (18.1) | 12 (4.0) | ||
| Occasional | 414 (68.5) | 206 (67.8) | 208 (69.3) | ||
| Often | 123 (20.4) | 43 (14.1) | 80 (26.7) | ||
| Spicy food consumption | <0.001 | ||||
| Never | 53 (8.8) | 40 (13.2) | 13 (4.3) | ||
| Occasional | 364 (60.3) | 196 (64.5) | 168 (56.0) | ||
| Often | 187 (31.0) | 68 (22.4) | 119 (39.7) | ||
| Tea, coffee or wine consumption | 0.007 | ||||
| Never | 235 (38.9) | 122 (40.1) | 113 (37.7) | ||
| Occasional | 329 (54.5) | 153 (50.3) | 176 (58.7) | ||
| Often | 40 (6.6) | 29 (9.5) | 11 (3.7) | ||
| Regular diet | 0.059 | ||||
| Never | 68 (11.3) | 32 (10.5) | 36 (12.0) | ||
| Occasional | 331 (54.8) | 155 (51.0) | 176 (58.7) | ||
| Often | 205 (33.9) | 117 (38.5) | 88 (29.3) | ||
| Vegetable and fruit consumption | <0.001 | ||||
| Never | 24 (4.0) | 18 (5.9) | 6 (2.0) | ||
| Occasional | 233 (38.6) | 135 (44.4) | 98 (32.7) | ||
| Often | 347 (57.5) | 151 (49.7) | 196 (65.3) | ||
| Cold bathing | 0.001 | ||||
| Never | 319 (52.8) | 153 (50.3) | 166 (55.3) | ||
| Occasional | 257 (42.5) | 127 (41.8) | 130 (43.3) | ||
| Often | 28 (4.6) | 24 (7.9) | 4 (1.3) | ||
| Cold water shampoo | 0.649 | ||||
| Never | 318 (52.6) | 155 (51.0) | 163 (54.3) | ||
| Occasional | 259 (42.9) | 136 (44.7) | 123 (41.0) | ||
| Often | 27 (4.5) | 13 (4.3) | 14 (4.7) | ||
| Staying up late | <0.001 | ||||
| Never | 106 (17.5) | 82 (27.0) | 24 (8.0) | ||
| Occasional | 348 (57.6) | 172 (56.6) | 176 (58.7) | ||
| Often | 150 (24.8) | 50 (16.4) | 100 (33.3) | ||
| Sleep quality | <0.001 | ||||
| Good | 117 (19.4) | 76 (25.0) | 41 (13.7) | ||
| Fair | 370 (61.3) | 199 (65.5) | 171 (57.0) | ||
| Poor | 117 (19.4) | 29 (9.5) | 88 (29.3) | ||
| Vigorous sports during menstrual period | 0.087 | ||||
| Never | 216 (35.8) | 107 (35.2) | 109 (36.3) | ||
| Occasional | 358 (59.3) | 176 (57.9) | 182 (60.7) | ||
| Often | 30 (5.0) | 21 (6.9) | 9 (3.0) | ||
| Physical activity | 0.326 | ||||
| Never | 125 (20.7) | 68 (22.4) | 57 (19.0) | ||
| Occasional | 420 (69.5) | 203 (66.8) | 217 (72.3) | ||
| Often | 59 (9.8) | 33 (10.9) | 26 (8.7) | ||
| Sedentary | <0.001 | ||||
| Never | 66 (10.9) | 49 (16.1) | 17 (5.7) | ||
| Occasional | 352 (58.3) | 176 (57.9) | 176 (58.7) | ||
| Often | 186 (30.8) | 79 (26.0) | 107 (35.7) | ||
| Dysmenorrhea history of mother | <0.001 | ||||
| Never | 379 (62.7) | 283 (93.1) | 96 (32.0) | ||
| Occasional | 186 (30.8) | 20 (6.6) | 166 (55.3) | ||
| Often | 39 (6.5) | 1 (0.3) | 38 (12.7) | ||
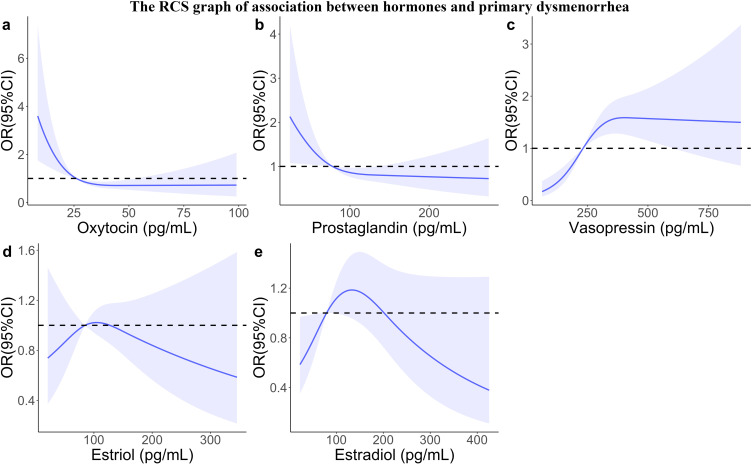
We compared the concentrations of five reproductive hormones between the two groups (Table 2), the concentrations of oxytocin (median (Q1, Q3): 29.15 (22.67, 39.32) vs 24.30 (17.70, 32.88) pg/mL) and PGF2α (86.10 (62.32, 113.62) vs 74.10 (54.30, 99.87) pg/mL) in the case group were significantly lower than those in the control group (all P<0.01), while the concentration of vasopressin in the case group was higher than that in the control group (216.20 (160.38, 295.97) vs 266.90 (197.70, 363.97) pg/mL, P<0.001). But estradiol and estriol concentrations showed no statistical significance. Besides, the RCS was used for describing the association of reproductive hormones with the risk of primary dysmenorrhea (Figure 1). The risk of primary dysmenorrhea decreased rapidly below around 30 pg/mL of oxytocin and then changed to a flat trend (Figure 1a). The relationship between PGF2α and risk of primary dysmenorrhea emerged the similar pattern of oxytocin and the inflection point was around 110 pg/mL (Figure 1b). Regarding vasopressin, the risk presented an increased trend within the lower range of levels of vasopressin, which reached the peak at 375 pg/mL and then kept a relatively steady trend with the rise of the hormone (Figure 1c). The risk with estriol (Figure 1d) as well as estradiol (Figure 1e) presented a reverse U shape. Thirdly, we further divided hormone levels into four categories (quartile) and then the association of quartile of five reproductive hormones with the risk of primary dysmenorrhea was performed respectively, after adjustment for potential confounders (Table 3). Women with higher oxytocin (Q2: OR=0.69, 95% CI: 0.36~1.33; Q3: 0.50, 0.27~0.95; Q4: 0.34, 0.17~0.66) as well as PGF2α (Q2: OR=0.85, 95% CI: 0.45~1.58; Q3: 0.45, 0.24~0.87; Q4: 0.43, 0.22~0.84) levels had lower risk of primary dysmenorrhea, compared to those with low hormone levels (Q1). On the contrary, vasopressin (Q3: OR=2.88, 95% CI: 1.48~5.63; Q4: 3.20, 1.65~6.22) showed a positive correlation between hormone levels and risk of disease; the reverse U shape was observed between the estradiol (Q2: OR=2.18, 95% CI: 1.13~4.19; Q3: 2.17, 1.12~4.19; Q4: 1.55, 0.80~3.00), estriol and the risk of disease; however, estriol was not significantly associated with the risk of disease.
Table 2.
Reproductive Hormones (pg/mL) Distribution of Study Participants
| Variables | Primary Dysmenorrhea | P | ||
|---|---|---|---|---|
| Participants (n=604) | Control (n=304) | Case (n=300) | ||
| Median (Q1, Q3) | ||||
| Estriol | 86.90 (59.27, 117.03) | 88.15 (60.08, 119.25) | 85.40 (58.72, 115.27) | 0.321 |
| Oxytocin | 26.70 (20.30, 36.32) | 29.15 (22.67, 39.32) | 24.30 (17.70, 32.88) | <0.001 |
| PGF2α | 80.90 (57.88, 108.45) | 86.10 (62.32, 113.62) | 74.10 (54.30, 99.87) | 0.001 |
| Vasopressin | 237.25 (175.38, 329.02) | 216.20 (160.38, 295.97) | 266.90 (197.70, 363.97) | <0.001 |
| Estradiol | 79.17 (44.57, 137.88) | 75.67 (40.86, 143.95) | 79.98 (47.93, 137.15) | 0.492 |
Figure 1.
Restricted cubic spline graph showing the association between five different hormones and the occurrence of primary dysmenorrhea. Blue-shaded area indicates 95% confidence interval. (a) Association of oxytocin with primary dysmenorrhea; (b) association of PGF2α with primary dysmenorrhea; (c) association of vasopressin with primary dysmenorrhea; (d) association of estriol with primary dysmenorrhea; (e) association of estradiol with primary dysmenorrhea.
Table 3.
Adjusted Association Between Reproductive Hormones and Primary Dysmenorrhea
| Variables§ | Control, n (%) | Case, n (%) | OR (95% CI) | |
|---|---|---|---|---|
| Model 1† | Model 2‡ | |||
| Oxytocin | ||||
| Q1 | 50 (16.4) | 100 (33.3) | Ref. | Ref. |
| Q2 | 75 (24.6) | 75 (25.0) | 0.50 (0.31~0.80)* | 0.69 (0.36~1.33) |
| Q3 | 87 (28.6) | 66 (22.0) | 0.38 (0.24~0.60)* | 0.50 (0.27~0.95)* |
| Q4 | 92 (30.4) | 59 (19.7) | 0.32 (0.20~0.51)* | 0.34 (0.17~0.66)* |
| PGF2α | ||||
| Q1 | 61 (20.0) | 90 (30.0) | Ref. | Ref. |
| Q2 | 69 (22.7) | 81 (27.0) | 0.80 (0.50~1.26) | 0.85 (0.45~1.58) |
| Q3 | 83 (27.3) | 69 (23.0) | 0.56 (0.36~0.89)* | 0.45 (0.24~0.87)* |
| Q4 | 91 (30.0) | 60 (20.0) | 0.45 (0.28~0.71)* | 0.43 (0.22~0.84)* |
| Estriol | ||||
| Q1 | 74 (24.3) | 77 (25.7) | Ref. | Ref. |
| Q2 | 72 (23.7) | 79 (26.3) | 1.05 (0.67~1.66) | 1.42 (0.75~2.71) |
| Q3 | 76 (25.0) | 75 (25.0) | 0.95 (0.60~1.49) | 1.18 (0.62~2.23) |
| Q4 | 82 (27.0) | 69 (23.0) | 0.81 (0.51~1.27) | 0.90 (0.47~1.71) |
| Estradiol | ||||
| Q1 | 90 (29.6) | 61 (20.3) | Ref. | Ref. |
| Q2 | 65 (21.4) | 86 (28.7) | 1.95 (1.24~3.08)* | 2.18 (1.13~4.19)* |
| Q3 | 71 (23.4) | 80 (26.7) | 1.66 (1.05~2.62)* | 2.17 (1.12~4.19)* |
| Q4 | 78 (25.6) | 73 (24.3) | 1.38 (0.88~2.18) | 1.55 (0.80~3.00) |
| Vasopressin | ||||
| Q1 | 99 (32.6) | 52 (17.3) | Ref. | Ref. |
| Q2 | 83 (27.3) | 68 (22.7) | 1.56 (0.98~2.48) | 1.08 (0.55~2.14) |
| Q3 | 59 (19.4) | 92 (30.7) | 2.97 (1.86~4.74)* | 2.88 (1.48~5.63)* |
| Q4 | 63 (20.7) | 88 (29.3) | 2.66 (1.67~4.24)* | 3.20 (1.65~6.22)* |
Notes: §The hormone levels were categorized into four groups by quartile (Q1~Q4). †Model 1 was the crude model. ‡Model 2 was adjusted for age, raw or cold food consumption, tea, coffee or wine consumption, cold bathing, sleep quality, vigorous sports during menstrual period, angry, anxiety, and dysmenorrhea history of mother. *P<0.05.
The Association of Reproductive Hormones with Frequency and Degree of Pain Among the Women with Primary Dysmenorrhea
The pain-related variables' characteristics among patients with primary dysmenorrhea are presented in Table 4. Among 300 patients, 107 (35.7%), 113 (37.7%) and 80 (26.7%) patients occasionally, frequently and always underwent the primary dysmenorrhea, respectively. Over half of the patients stated the dysmenorrhea emergence from menarche or 1–2 years after menarche. As for degree of pain, 56.7% of patients felt low degree of pain and 40.0% moderate pain as well, only 3.3% a high degree of pain. Regarding pain symptoms, dull pain and distending pain were the major types, with 43.0% and 52.0% of patients, respectively; meanwhile, other pain types included colicky pain, falling pain and throbbing pain. Furthermore, there were menstrual related symptoms among the patients with primary dysmenorrhea; and backache (58.3%), breast distention (43.3%), abdomen distention (37.0%), weakness (34.0%) and feeling cold (32.7%) were common; other low frequent symptoms included muscle pain, breast pain, poor sleep quality, somnolence, indigestion, nausea, diarrhea and feeling cold.
Table 4.
Pain-Related Variables’ Characteristics Among Patients with Primary Dysmenorrhea
| Variables | N (%) | Variables | N (%) |
|---|---|---|---|
| Frequency | Menstrual-related symptom | ||
| Occasional | 107 (35.7) | Abdominal distention | |
| Frequent | 113 (37.7) | No | 189 (63.0) |
| Always | 80 (26.7) | Yes | 111 (37.0) |
| Emergence time | Breast distention | ||
| Menarche | 106 (35.3) | No | 170 (56.7) |
| 1–2 years after menarche | 103 (34.3) | Yes | 130 (43.3) |
| 3–5 years after menarche | 62 (20.7) | Breast pain | |
| In college | 29 (9.7) | No | 253 (84.3) |
| Degree of pain | Yes | 47 (15.7) | |
| Low | 170 (56.7) | Poor sleep quality | |
| Moderate | 120 (40.0) | No | 254 (84.7) |
| High | 10 (3.3) | Yes | 46 (15.3) |
| Pain type | Somnolence | ||
| Dull pain | No | 244 (81.3) | |
| No | 171 (57.0) | Yes | 56 (18.7) |
| Yes | 129 (43.0) | Weakness | |
| Distending pain | No | 198 (66.0) | |
| No | 144 (48.0) | Yes | 102 (34.0) |
| Yes | 156 (52.0) | Indigestion | |
| Colicky pain | No | 281 (93.7) | |
| No | 226 (75.3) | Yes | 19 (6.3) |
| Yes | 74 (24.7) | Nausea | |
| Falling pain | No | 276 (92.0) | |
| No | 212 (70.7) | Yes | 24 (8.0) |
| Yes | 88 (29.3) | Diarrhea | |
| Throbbing pain | No | 249 (83.0) | |
| No | 280 (93.3) | Yes | 51 (17.0) |
| Yes | 20 (6.7) | Feeling cold | |
| Menstrual-related symptom | No | 202 (67.3) | |
| Backache | Yes | 98 (32.7) | |
| No | 125 (41.7) | ||
| Yes | 175 (58.3) | ||
| Muscle pain | |||
| No | 271 (90.3) | ||
| Yes | 29 (9.7) |
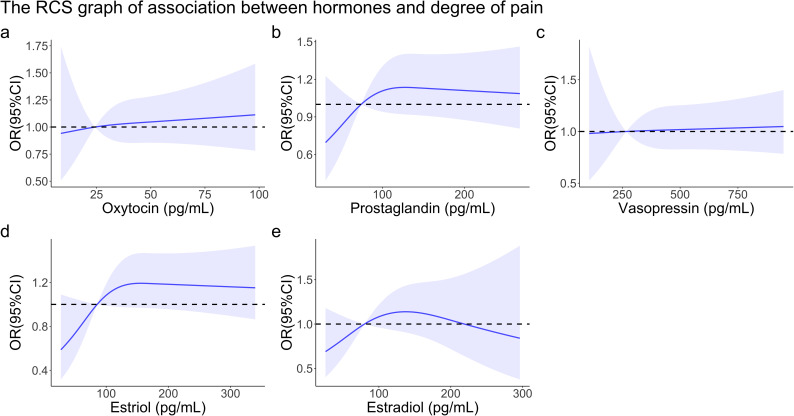
We also explored the association of five reproductive hormones (quartile) with frequency as well as degree of pain of primary dysmenorrhea among the patients. With regard to frequency (Table 5), compared to Q1 estriol, Q2 estriol (frequent: OR=3.12, 95% CI: 1.32~7.34; always: OR=2.51, 95% CI: 1.03~6.11) and Q3 estriol (frequent: OR=4.97, 95% CI: 2.08~11.85; always: OR=3.10, 95% CI: 1.25~7.73) were associated with higher frequency and always primary dysmenorrhea after adjustment for potential confounders. Similarly, estradiol also emerged with a similar effect on pain frequency (Q3: always: OR=2.62, 95% CI: 1.03~6.64). Besides, the RCS was also used for describing the association of hormones with the degree of pain among patients with primary dysmenorrhea (Figure 2). The degree of pain presented slight increased trend in oxytocin (Figure 2a) and vasopressin (Figure 2c), while diagrams increased rapidly below around 100 pg/mL of PGF2α as well as 150 pg/mL of estriol and then showed a flat trend in Figure 2b and 2d. And similar to Figure 1e, estradiol showed the similar U-reverse trends (Figure 2e). As for the degree of pain in logistic regression model (Table 6), only higher estriol (Q3: OR=2.06, 95% CI: 1.03~4.18) presented significant association with higher degree of pain, compared to Q1 estriol.
Table 5.
Adjusted Association Between Reproductive Hormones and Frequency Among Patients with Primary Dysmenorrhea
| Variables§ | OR (95% CI) | |||
|---|---|---|---|---|
| Model 1† | Model 2‡ | |||
| Frequent | Always | Frequent | Always | |
| Oxytocin | ||||
| Q1 | Ref. | Ref | Ref. | Ref. |
| Q2 | 0.45 (0.21~0.96) | 0.9 (0.39~2.11) | 0.47 (0.20~1.08) | 0.90 (0.36~2.24) |
| Q3 | 0.73 (0.34~1.53) | 1.06 (0.44~2.52) | 0.68 (0.29~1.56) | 0.97 (0.38~2.48) |
| Q4 | 0.58 (0.27~1.25) | 1.17 (0.5~2.74) | 0.58 (0.25~1.34) | 1.22 (0.49~3.07) |
| PGF2α | ||||
| Q1 | Ref. | Ref. | Ref. | Ref. |
| Q2 | 0.49 (0.23~1.04) | 1.27 (0.54~2.97) | 0.63 (0.27~1.43) | 1.59 (0.64~3.98) |
| Q3 | 0.72 (0.35~1.5) | 1.32 (0.55~3.17) | 0.78 (0.35~1.73) | 1.23 (0.48~3.12) |
| Q4 | 0.78 (0.37~1.65) | 1.79 (0.75~4.24) | 1.07 (0.47~2.43) | 2.15 (0.85~5.43) |
| Estriol | ||||
| Q1 | Ref. | Ref. | Ref. | Ref. |
| Q2 | 3.21 (1.47~6.99)* | 2.56 (1.12~5.86)* | 3.12(1.32~7.34)* | 2.51 (1.03~6.11)* |
| Q3 | 4.43 (2.00~9.80)* | 3.13 (1.34~7.32)* | 4.97 (2.08~11.85)* | 3.10 (1.25~7.73)* |
| Q4 | 2.54 (1.18~5.47)* | 1.97 (0.87~4.48) | 2.18 (0.94~5.06) | 1.64 (0.68~3.97) |
| Estradiol | ||||
| Q1 | Ref. | Ref. | Ref. | Ref. |
| Q2 | 1.10 (0.53~2.31) | 1.74 (0.76~4.00) | 1.10 (0.48~2.51) | 1.82 (0.74~4.47) |
| Q3 | 1.98 (0.93~4.24) | 2.58 (1.09~6.12)* | 1.97 (0.85~4.56) | 2.62 (1.03~6.64)* |
| Q4 | 1.02 (0.49~2.13) | 1.47 (0.64~3.40) | 1.3 7(0.61~3.06) | 1.82 (0.74~4.46) |
| Vasopressin | ||||
| Q1 | Ref. | Ref. | Ref. | Ref. |
| Q2 | 1.36 (0.64~2.89) | 1.56 (0.69~3.51) | 1.34 (0.58~3.07) | 1.60 (0.66~3.84) |
| Q3 | 1.63 (0.78~3.43) | 1.54 (0.67~3.51) | 1.75 (0.77~3.95) | 1.52 (0.63~3.69) |
| Q4 | 2.34 (1.09~5.01)* | 2.20 (0.95~5.10) | 1.79 (0.77~4.14) | 2.23 (0.89~5.57) |
Notes: §The hormone levels were categorized into four groups by quartile (Q1~Q4). †Model 1 was the crude model. ‡Model 2 was adjusted for age, raw or cold food consumption, tea, coffee or wine consumption, cold bathing, sleep quality, vigorous sports during menstrual period, angry, anxiety, and dysmenorrhea history of mother. *P<0.05.
Figure 2.
Restricted cubic spline graph showing the association between five different hormones and the degree of pain among patients with primary dysmenorrhea. Blue-shaded area indicates 95% confidence interval. (a) Association of oxytocin with degree of pain; (b) association of PGF2α with degree of pain; (c) association of vasopressin with degree of pain; (d) association of estriol with degree of pain; (e) association of estradiol with degree of pain.
Table 6.
Adjusted Association Between Reproductive Hormones and Degree of Pain Among Patients with Primary Dysmenorrhea
| Variables§ | Low, n (%) | Moderate/high, n (%) | OR (95% CI) | |
|---|---|---|---|---|
| Model 1† | Model 2‡ | |||
| Oxytocin | ||||
| Q1 | 42 (24.7) | 31 (23.8) | Ref. | Ref. |
| Q2 | 43 (25.3) | 33 (25.4) | 1.04 (0.54~1.99) | 1.02 (0.51~2.04) |
| Q3 | 47 (27.6) | 29 (22.3) | 0.84 (0.43~1.61) | 0.80 (0.39~1.61) |
| Q4 | 38 (22.3) | 37 (28.5) | 1.32 (0.69~2.52) | 1.18 (0.59~2.36) |
| PGF2α | ||||
| Q1 | 46 (27.0) | 29 (22.3) | Ref. | Ref. |
| Q2 | 46 (27.0) | 29 (22.3) | 1.00 (0.52~1.93) | 1.10 (0.55~2.22) |
| Q3 | 40 (23.5) | 35 (26.9) | 1.39 (0.72~2.66) | 1.15 (0.58~2.3) |
| Q4 | 38 (22.5) | 37 (28.5) | 1.54 (0.81~2.95) | 1.48 (0.73~2.97) |
| Estriol | ||||
| Q1 | 50 (29.4) | 25 (19.2) | Ref. | Ref. |
| Q2 | 42 (24.7) | 33 (25.4) | 1.57 (0.81~3.05) | 1.57 (0.78~3.21) |
| Q3 | 37 (21.8) | 38 (29.2) | 2.05 (1.06~3.97)* | 2.06 (1.03~4.18)* |
| Q4 | 41 (24.1) | 34 (26.2) | 1.66 (0.86~3.21) | 1.52 (0.75~3.09) |
| Estradiol | ||||
| Q1 | 46 (27.0) | 29 (22.3) | Ref. | Ref. |
| Q2 | 42 (24.7) | 33 (25.4) | 1.25 (0.65~2.39) | 1.25 (0.62~2.52) |
| Q3 | 36 (21.2) | 39 (30.0) | 1.72 (0.90~3.29) | 1.77 (0.87~3.59) |
| Q4 | 46 (27.1) | 29 (22.3) | 1.00 (0.52~1.93) | 1.11 (0.56~2.24) |
| Vasopressin | ||||
| Q1 | 42 (24.7) | 33 (25.4) | Ref. | Ref. |
| Q2 | 44 (25.9) | 30 (23.1) | 0.87 (0.45~1.66) | 0.81 (0.40~1.62) |
| Q3 | 44 (25.9) | 32 (24.6) | 0.93 (0.49~1.76) | 0.73 (0.37~1.46) |
| Q4 | 40 (23.5) | 35 (26.9) | 1.11 (0.59~2.12) | 0.90 (0.45~1.82) |
Notes: §The hormone levels were categorized into four groups by quartile (Q1~Q4). †Model 1 was the crude model. ‡Model 2 was adjusted for age, raw or cold food consumption, tea, coffee or wine consumption, cold bathing, sleep quality, vigorous sports during menstrual period, angry, anxiety, and dysmenorrhea history of mother. *P<0.05.
Discussion
Our study found that serum PGF2α and oxytocin concentrations presented negative association with the risk of primary dysmenorrhea, while vasopressin levels showed positive association with the risk of primary dysmenorrhea, but the reverse U-shape association between estradiol and risk of primary dysmenorrhea was observed. As for degree and frequency of pain, estriol showed a positive correlation with degree and frequency of pain among patients with primary dysmenorrhea.
As for dysmenorrhea patients, our study showed that most patients had pain symptoms from menarche or 1–2 years after menarche (69.6%), while few patients had symptoms in college, which indicated that most patients got illness in the early period and suffered a long time. On the other side, although the great majority of patients suffered from the low or moderate pain (96.7%) rather than a high degree of pain, almost all of the patients reported themselves with dull pain, distending pain, accompanied by backache, breast distention and other menstrual related symptoms, which might influence daily life and work severely.24
With regard to the effect of hormones to the risk of primary dysmenorrhea, the majority of research studies considered that increased prostaglandin was the major cause of primary dysmenorrhea. Prostaglandins included several classes while PGF2α and PGE2 contributed the most in the onset of primary dysmenorrhea.25 Some studies indicated that the increased PGF2α by the way of the cyclooxygenase pathway led to increased uterine tone as well as spastic contraction,5 then promoted the occurrence of dysmenorrhea.26,27 Contrary to PGF2α, PGE2 played the reverse role in primary dysmenorrhea including inhibition of uterine smooth muscle contraction and reduction of spontaneous uterine activity. In our study, we detected the serum PGF2α concentration of participants; however, compared to participants with lower PGF2α levels, participants with higher PGF2α levels had decreased risk of primary dysmenorrhea after adjustment for the potential compounds, which was also shown in the RCS graph. Another associated hormone which showed a similar effect on primary dysmenorrhea in our study was oxytocin, and some recent studies supported our results that compared to non-dysmenorrhea women, patients of dysmenorrhea had lower serum oxytocin concentrations.19,20 Same as PGF2α, the RCS graph of oxytocin also presented a negative association. Furthermore, the finding of another study was that the endometrial concentration of oxytocin receptor mRNA in patients was lower than that in non-dysmenorrhea women.28 Hence, oxytocin could be the negative correlation with primary dysmenorrhea during the menstrual period. However, the pathway of oxytocin affecting dysmenorrhea is vague or strongly disputed currently. One study demonstrated that oxytocin receptor was also presented in myometrium of non-pregnant women, and was bound with oxytocin for uterine contractions.17 In another previous study, oxytocin was considered as a hormone which could exert an analgesic effect by a spinal circuit when suffering from endogenous or exogenous pain, and the serum oxytocin concentration among patients with pain such as backache and stomach ache was higher than that in healthy people.29 On the other hand, oxytocin was also involved in influencing prostaglandin synthesis, that stimulated smooth muscle contraction and aggravated dysmenorrhea.30 Hence, some studies considered that oxytocin levels in patients were higher than that in healthy controls and synergized prostaglandin to aggravated dysmenorrhea.28,31 Nevertheless, considering the result of oxytocin as well as prostaglandin on primary dysmenorrhea in our study and other studies of oxytocin for decreasing the onset of dysmenorrhea, the synergism of oxytocin and prostaglandin in primary dysmenorrhea needs more research to explore.32
As for vasopressin, our results showed that the serum vasopressin concentration was associated with an increased risk of primary dysmenorrhea, which was consistent with the results reported in some other studies in addition.27,33 One previous research result presented that the pain rating described by the patients with primary dysmenorrhea decreased visibly when treated with arginine vasopressin antagonists (atosiban) while patients of the placebo group reported no difference about pain rating and diagrams after treatment.34 Vasopressin, considered as a powerful uterotonic, could cause myometrial small vessel contraction through vasopressin receptors and reduce uterine blood flow, which at last lead to dysmenorrhea. Another study indicated that vasopressin receptors were associated with pain control and predominantly expressed in the endometrium which could widely affect the occurrence of dysmenorrhea.35 Hence, high serum vasopressin level could be the risk factor for the primary dysmenorrhea during menstrual periods.
In the RCS graphs of two different estrogens, the plots both reflected a reverse U shape, but 95% CI and P values presented no significant difference. As for the results of association between estradiol as well as estriol and primary dysmenorrhea, the former similarly showed no statistical significance with less related studies, while the latter indicated the correlation with primary dysmenorrhea. However, compared to the estradiol Q1 level, the results with significance only when estradiol levels were Q2 and Q3, and the statistical association disappeared when estradiol reached the highest level (Q4). Current studies considered that similar to vasopressin, estradiol also could lead to uterine spastic contraction and ischemia, and the pain symptom could be effectively relieved among patients with dysmenorrhea when the patients were treated by gonadotropin-releasing hormone antagonist.36,37 Furthermore, another study showed that estrogen receptor alpha (ESR1) was associated with primary dysmenorrhea when producing effect through binding with estrogen.38 Our study and relevant mechanism could suggest that estradiol within a medium level was positively correlated with the risk of primary dysmenorrhea and the effect disappeared when estradiol reached a higher level, which needs more related research to verify.
Regarding the frequency and degree of pain, prostaglandin levels presented a positive correlation with frequency and degree of pain about primary dysmenorrhea although the difference showed no statistical significance. Prostaglandin F2α could decrease the pain threshold by affecting nerve receptors, which could explain the high frequency and degree of pain with the high serum PGF2α concentration. One previous study also showed that the intensity of pain in primary dysmenorrhea and related symptoms were proportional to the PGF2α levels during the menstrual phase.25 Another risk factor for the degree and frequency of pain was estriol. Our study showed that middle-level estriol was associated with more frequent dysmenorrhea and more severe pain and the statistical significance also disappeared when estriol reached a peak level. Estriol was formed from estrone, considered as pregnancy estrogens compared with estradiol as a major estrogen, and could be converted from estradiol in the liver.39,40 Similar to estradiol, estriol could produce effect through decrease of the pain threshold which led to pain exacerbation. However, the studies concentrating on the association between estriol and degree of pain and frequency about primary dysmenorrhea were few. Hence, more non-pregnancy studies are needed to demonstrate the correlation between estrogen and primary dysmenorrhea and support our results.
Strengths and Limitations
There are several strengths in our study. Initially, we analyzed five different relative reproductive hormones at the same time in order to explore the association with primary dysmenorrhea. Moreover, the relationship between hormones and the degree as well as frequency of pain in patients was considered in addition; furthermore, the potential confounders were adjusted. There were some limitations in this study. First, due to being a case–control study, recalled bias would be introduced in the associations, while the case–control study could only reflect the casual association between the reproductive hormones and the relevant outcomes. Second, some socio-demographic information was lacking, and the potential confounding effect from them was not adjusted. Third, we only detected the reproductive hormone levels of patients during the menstrual period while the data of hormone concentration before the menstrual period were not collected, which could not reflect individual reproductive hormone levels comprehensively.
Conclusion
Higher serum vasopressin and estradiol concentrations as well as lower oxytocin and PGF2α levels were associated with higher risk of primary dysmenorrhea. Estrogen showed a reverse U-shape association on the degree of pain and frequency of primary dysmenorrhea among patients with primary dysmenorrhea.
Acknowledgments
The authors thank the support from faculties and staff in Yiwu Maternity and Children Hospital and all the participants in this study.
Funding Statement
Science and Technology Research Plan of Jinhua (2019-4-142), Chinese National Natural Science Foundation (81973055), National Key Research and Development Programme of China (2021YFC2701901), Major research and development projects of Zhejiang Science and Technology Department (2018C03010), Key Laboratory of Intelligent Preventive Medicine of Zhejiang Province (2020E10004) and Leading Innovative and Entrepreneur Team Introduction Program of Zhejiang (2019R01007).
Data Sharing Statement
The data and materials used and analyzed in our study available from the corresponding author with reasonable request.
Ethics Approval and Consent to Participate
The study was approved by the Medical Ethics Committee of Yiwu Maternity and Children Hospital.
Author Contributions
J.J. and Y.Z. conceived and designed this paper. S.S, H.C, X.A, M.M. and H.Z. collected the data together. H.L. and Y.Y. revised the manuscript. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors declare that they have no competing interest in this work.
References
- 1.Iacovides S, Avidon I, Baker FC. What we know about primary dysmenorrhea today: a critical review. Hum Reprod Update. 2015;21(6):762–778. doi: 10.1093/humupd/dmv039 [DOI] [PubMed] [Google Scholar]
- 2.Kho KA, Shields JK. Diagnosis and management of primary dysmenorrhea. JAMA. 2020;323(3):268–269. doi: 10.1001/jama.2019.16921 [DOI] [PubMed] [Google Scholar]
- 3.Abu Helwa HA, Mitaeb AA, Al-Hamshri S, Sweileh WM. Prevalence of dysmenorrhea and predictors of its pain intensity among Palestinian female university students. BMC Women's Health. 2018;18(1):18. doi: 10.1186/s12905-018-0516-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ameade EPK, Amalba A, Mohammed BS. Prevalence of dysmenorrhea among University students in Northern Ghana; its impact and management strategies. BMC Women's Health. 2018;18(1):39. doi: 10.1186/s12905-018-0532-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barcikowska Z, Wójcik-Bilkiewicz K, Sobierajska-Rek A, Grzybowska ME, Wąż P, Zorena K. Dysmenorrhea and associated factors among Polish women: a cross-sectional study. Pain Res Manag. 2020;2020:6161536. doi: 10.1155/2020/6161536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Durand H, Monahan K, McGuire BE. Prevalence and impact of dysmenorrhea among university students in Ireland. Pain Med. 2021;22(12):2835. doi: 10.1093/pm/pnab122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chen L, Tang L, Guo S, Kaminga AC, Xu H. Primary dysmenorrhea and self-care strategies among Chinese college girls: a cross-sectional study. BMJ Open. 2019;9(9):e026813. doi: 10.1136/bmjopen-2018-026813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wong CL, Ip WY, Lam LW. Self-care strategies among Chinese adolescent girls with dysmenorrhea: a qualitative study. Pain Manag Nurs. 2016;17(4):262–271. doi: 10.1016/j.pmn.2016.04.001 [DOI] [PubMed] [Google Scholar]
- 9.Jiang W, Hua X-G, Hu C-Y, Li F-L, Huang K, Zhang X-J. The prevalence and risk factors of menstrual pain of married women in Anhui Province, China. Eur J Obstet Gynecol Reprod Biol. 2018;229:190–194. doi: 10.1016/j.ejogrb.2018.09.002 [DOI] [PubMed] [Google Scholar]
- 10.Muluneh AA, Nigussie TS, Gebreslasie KZ, Anteneh KT, Kassa ZY. Prevalence and associated factors of dysmenorrhea among secondary and preparatory school students in Debremarkos town, North-West Ethiopia. BMC Women's Health. 2018;18(1):57. doi: 10.1186/s12905-018-0552-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bajalan Z, Moafi F, MoradiBaglooei M, Alimoradi Z. Mental health and primary dysmenorrhea: a systematic review. J Psychosom Obstet Gynaecol. 2019;40(3):185–194. doi: 10.1080/0167482X.2018.1470619 [DOI] [PubMed] [Google Scholar]
- 12.Ferries-Rowe E, Corey E, Archer JS. Primary dysmenorrhea: diagnosis and therapy. Obstet Gynecol. 2020;136(5):1047–1058. doi: 10.1097/AOG.0000000000004096 [DOI] [PubMed] [Google Scholar]
- 13.Hailemeskel S, Demissie A, Assefa N. Primary dysmenorrhea magnitude, associated risk factors, and its effect on academic performance: evidence from female university students in Ethiopia. Int J Women's Health. 2016;8:489–496. doi: 10.2147/IJWH.S112768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Doğan H, Eroğlu S, Akbayrak T. The effect of kinesio taping and lifestyle changes on pain, body awareness and quality of life in primary dysmenorrhea. Complement Ther Clin Pract. 2020;39:101120. doi: 10.1016/j.ctcp.2020.101120 [DOI] [PubMed] [Google Scholar]
- 15.Hanife Doğan MDÇ. Approaches of dealing with primary dysmenorrhea and relationship between Kinesiophobia and pain severity. Konuralp Med J. 2020;12(3):1. [Google Scholar]
- 16.Chan WY, Hill JC. Determination of menstrual prostaglandin levels in non-dysmenorrheic and dysmenorrheic subjects. Prostaglandins. 1978;15(2):365–375. doi: 10.1016/0090-6980(78)90176-4 [DOI] [PubMed] [Google Scholar]
- 17.Coco AS. Primary dysmenorrhea. Am Fam Physician. 1999;60(2):489–496. [PubMed] [Google Scholar]
- 18.Bossmar T, Akerlund M, Szamatowicz J, Laudanski T, Fantoni G, Maggi M. Receptor-mediated uterine effects of vasopressin and oxytocin in nonpregnant women. Br J Obstet Gynaecol. 1995;102(11):907–912. doi: 10.1111/j.1471-0528.1995.tb10880.x [DOI] [PubMed] [Google Scholar]
- 19.Oladosu FA, Tu FF, Garfield LB, et al. Low serum oxytocin concentrations are associated with painful menstruation. Reprod Sci. 2020;27(2):668–674. doi: 10.1007/s43032-019-00071-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salonia A, Nappi RE, Pontillo M, et al. Menstrual cycle-related changes in plasma oxytocin are relevant to normal sexual function in healthy women. Horm Behav. 2005;47(2):164–169. doi: 10.1016/j.yhbeh.2004.10.002 [DOI] [PubMed] [Google Scholar]
- 21.French L. Dysmenorrhea. Am Fam Physician. 2005;71(2):285–291. [PubMed] [Google Scholar]
- 22.Strömberg P, Forsling ML, Akerlund M. Effects of prostaglandin inhibition on vasopressin levels in women with primary dysmenorrhea. Obstet Gynecol. 1981;58(2):206–208. [PubMed] [Google Scholar]
- 23.Taylor HS, Giudice LC, Lessey BA, et al. Treatment of endometriosis-associated pain with elagolix, an oral GnRH antagonist. N Engl J Med. 2017;377(1):28–40. doi: 10.1056/NEJMoa1700089 [DOI] [PubMed] [Google Scholar]
- 24.Hu Z, Tang L, Chen L, Kaminga AC, Xu H. Prevalence and risk factors associated with primary dysmenorrhea among Chinese female university students: a cross-sectional study. J Pediatr Adolesc Gynecol. 2020;33(1):15–22. doi: 10.1016/j.jpag.2019.09.004 [DOI] [PubMed] [Google Scholar]
- 25.Dawood MY. Primary dysmenorrhea: advances in pathogenesis and management. Obstet Gynecol. 2006;108(2):428–441. doi: 10.1097/01.AOG.0000230214.26638.0c [DOI] [PubMed] [Google Scholar]
- 26.Lundström V, Gréen K. Endogenous levels of prostaglandin F2alpha and its main metabolites in plasma and endometrium of normal and dysmenorrheic women. Am J Obstet Gynecol. 1978;130(6):640–646. doi: 10.1016/0002-9378(78)90320-4 [DOI] [PubMed] [Google Scholar]
- 27.Strömberg P, Akerlund M, Forsling ML, Granström E, Kindahl H. Vasopressin and prostaglandins in premenstrual pain and primary dysmenorrhea. Acta Obstet Gynecol Scand. 1984;63(6):533–538. doi: 10.3109/00016348409156715 [DOI] [PubMed] [Google Scholar]
- 28.Liedman R, Hansson SR, Howe D, Igidbashian S, Russell RJ, Akerlund M. Endometrial expression of vasopressin, oxytocin and their receptors in patients with primary dysmenorrhoea and healthy volunteers at ovulation. Eur J Obstet Gynecol Reprod Biol. 2008;137(2):189–192. doi: 10.1016/j.ejogrb.2007.10.015 [DOI] [PubMed] [Google Scholar]
- 29.Xin Q, Bai B, Liu W. The analgesic effects of oxytocin in the peripheral and central nervous system. Neurochem Int. 2017;103:57–64. doi: 10.1016/j.neuint.2016.12.021 [DOI] [PubMed] [Google Scholar]
- 30.Makino S, Zaragoza DB, Mitchell BF, Yonemoto H, Olson DM. Decidual activation: abundance and localization of prostaglandin F2alpha receptor (FP) mRNA and protein and uterine activation proteins in human decidua at preterm birth and term birth. Placenta. 2007;28(5–6):557–565. doi: 10.1016/j.placenta.2006.06.010 [DOI] [PubMed] [Google Scholar]
- 31.Liedman R, Hansson SR, Howe D, et al. Reproductive hormones in plasma over the menstrual cycle in primary dysmenorrhea compared with healthy subjects. Gynecol Endocrinol. 2008;24(9):508–513. doi: 10.1080/09513590802306218 [DOI] [PubMed] [Google Scholar]
- 32.Engel S, Klusmann H, Ditzen B, Knaevelsrud C, Schumacher S. Menstrual cycle-related fluctuations in oxytocin concentrations: a systematic review and meta-analysis. Front Neuroendocrinol. 2019;52:144–155. doi: 10.1016/j.yfrne.2018.11.002 [DOI] [PubMed] [Google Scholar]
- 33.Akerlund M.Involvement of oxytocin and vasopressin in the pathophysiology of preterm labor and primary dysmenorrhea. Prog Brain Res. 2002;139:359–365. [DOI] [PubMed] [Google Scholar]
- 34.Liedman R, Grant L, Igidbashian S, et al. Intrauterine pressure, ischemia markers, and experienced pain during administration of a vasopressin V1a receptor antagonist in spontaneous and vasopressin-induced dysmenorrhea. Acta Obstet Gynecol Scand. 2006;85(2):207–211. doi: 10.1080/00016340500495082 [DOI] [PubMed] [Google Scholar]
- 35.Akerlund M. Vasopressin and oxytocin in normal reproduction and in the pathophysiology of preterm labour and primary dysmenorrhoea. Development of receptor antagonists for therapeutic use in these conditions. Rocz Akad Med Bialymst. 2004;49:18–21. [PubMed] [Google Scholar]
- 36.Donnez J, Taylor HS, Taylor RN, et al. Treatment of endometriosis-associated pain with linzagolix, an oral gonadotropin-releasing hormone-antagonist: a randomized clinical trial. Fertil Steril. 2020;114(1):44–55. doi: 10.1016/j.fertnstert.2020.02.114 [DOI] [PubMed] [Google Scholar]
- 37.Giudice LC, As-Sanie S, Arjona Ferreira JC, et al. Once daily oral relugolix combination therapy versus placebo in patients with endometriosis-associated pain: two replicate Phase 3, randomised, double-blind, studies (SPIRIT 1 and 2). Lancet. 2022;399(10343):2267–2279. doi: 10.1016/S0140-6736(22)00622-5 [DOI] [PubMed] [Google Scholar]
- 38.Ozsoy AZ, Karakus N, Yigit S, Cakmak B, Nacar MC, Ylmaz Dogru H. The evaluation of IL6 and ESR1 gene polymorphisms in primary dysmenorrhea. Immunol Invest. 2016;45(1):75–86. doi: 10.3109/08820139.2015.1113426 [DOI] [PubMed] [Google Scholar]
- 39.Guerami A, MacDonald PC, Casey ML. Variation in the fractional conversion of plasma estrone to estriol among women and men. J Clin Endocrinol Metab. 1984;58(6):1148–1152. doi: 10.1210/jcem-58-6-1148 [DOI] [PubMed] [Google Scholar]
- 40.Ali ES, Mangold C, Peiris AN. Estriol: emerging clinical benefits. Menopause. 2017;24(9):1081–1085. doi: 10.1097/GME.0000000000000855 [DOI] [PubMed] [Google Scholar]