Abstract
Objectives
To evaluate the efficacy of chewing gum on the intensity of pain in patients undergoing orthodontic treatment.
Materials and Methods
A search strategy that included both a manual search and a search of electronic databases was implemented; the electronic databases included PubMed, Cochrane Central Register of Controlled Trials (CENTRAL), ScienceDirect, Scopus, and EBSCO. Only randomized controlled trials were included in this study. All of the studies were assessed independently and in duplicate in accordance with the exclusion and inclusion criteria. The Cochrane risk of bias tool was used to evaluate the risk of bias within the included studies, and the GRADE approach was used to evaluate the certainty of evidence.
Results
Sixteen RCTs were included in the final analysis. The meta-analysis revealed that chewing gum significantly reduced pain intensity in comparison to pharmacologic agents (mean difference [MD] −0.50 [95% confidence interval {CI} −0.90 to −0.10], P = .01). When compared with a placebo, chewing gum significantly reduced pain intensity (MD −0.60 [95% CI −1.06 to −0.13], P = .01), while bite wafer and chewing gum groups had the same levels of reduction in pain intensity (MD −0.15 [95% CI −0.56 to 0.26], P = .48).
Conclusions
In patients undergoing fixed orthodontic treatment, chewing gum was significantly more effective than both pharmacologic agents and placebo in reducing orthodontic pain 24 hours after the initial placement of the archwire.
Keywords: Orthodontics, Orthodontic pain, Chewing gum, Pharmacologic interventions
INTRODUCTION
Orthodontic treatment often comprises long-lasting, painful, and expensive procedures. Pain is considered the main reason why patients interrupt their treatment, and it negatively influences their level of compliance.1,2 Different types of orthodontic procedures usually cause pain. These procedures include archwire activation,3 orthopedic appliances,4 and the placement of separators.5 Among patients undergoing fixed orthodontic treatment, 91% complained of pain at some stage of the treatment,6 and more than 30% of patients reported pain at each stage during the course of treatment.7 Pain was reported to be the main discouraging reason to discontinue treatment.2 Therefore, orthodontic pain is a major concern for both orthodontists and patients. It was shown that, in most patients, the peak intensity of pain occurred 1 day following the insertion of an archwire or separators and decreased gradually over the next 7 days.8 On the other hand, in some studies, it was reported that almost half of patients experienced orthodontic pain even 1 week after the insertion of an archwire.9
Orthodontic tooth movement is an inflammatory process that occurs following the application of orthodontic force. During this inflammatory process, several inflammatory mediators, including substance P, prostaglandin, bradykinin, serotonin, and histamine, are released after a series of biological events. In turn, these mediators induce pain by stimulating nerve endings.10,11 Ibuprofen, acetylsalicylic acid, and paracetamol are the analgesics most commonly prescribed by orthodontists to alleviate pain and discomfort caused by orthodontic treatment.12–14 On the other hand, these pain relievers may interfere with the inflammatory process responsible for inducing orthodontic tooth movement.15 In addition, these analgesics have negative side effects and contraindications.14,15
The repetitive chewing action performed while chewing gum can reduce orthodontic pain by reducing ischemia through the compression and decompression of the PDL.16 Thus, chewing sugar-free gum may be a promising nonpharmacologic intervention that reduces orthodontic pain. In addition, sugar-free gum has different uses in dentistry. It can be used as a salivary substitute to improve salivary flow and relieve the symptoms of dry mouth17; reduce plaque accumulation, gingivitis, and bleeding score18; and it can be used to evaluate chewing function in adults and the elderly.19,20 Also, several articles emphasized that chewing gum may enhance surgical recovery following postoperative ileus surgical interventions.21–23
The aim of this study was to synthesize evidence from the existing literature to explore fully the efficacy of chewing gum in reducing pain intensity in patients undergoing fixed orthodontic treatment, evaluate the quality of evidence of the existing literature and direct future research to develop an improved conclusion regarding the relationship between chewing gum and orthodontic pain.
MATERIALS AND METHODS
A well-structured design was implemented using the PICOS methodology:
Population: patients aged 12 years or older who were receiving fixed orthodontic treatment
Intervention: chewing gum
Comparison: patients receiving different intervention or no treatment
Outcome: reduction in reported pain intensity 24 hours after the activation of orthodontic force
Design: randomized clinical trials (RCTs)
Protocol and Registration
The systematic review was registered in Prospero (International Prospective Register of Systematic Reviews) with reference number CRD42019141501 and was reported in adherence to the Prisma checklist guidelines.
Information Sources and Search Strategy
In this systematic review, a comprehensive search strategy was used, which started in September 2021 and ended in September 2022 and incorporated both electronic and manual search methods. The electronic database search included PubMed, Cochrane Central Register of Controlled Trials (CENTRAL), Scopus, EBSCO, and ScienceDirect. In addition, a thorough manual search was performed to identify articles that were not indexed in databases and to eliminate any chance of excluding related articles.
Journals Manually Searched
The following journals were included in the manual search:
European Journal of Orthodontics (2010–2022)
Angle Orthodontist (2010–2022)
American Journal of Orthodontic and Dentofacial Orthopedics (2010–2022)
Journal of Orofacial Orthopedics/Fortschritte der Kieferorthopädie (2010–2022)
Eligibility Criteria
After the careful inspection of articles in accordance with the exclusion and inclusion criteria, only randomized controlled articles that involved patients who were (1) a minimum age of 12 years old, (2) receiving chewing gum as an intervention to control orthodontic pain, (3) undergoing fixed orthodontic treatment, (4) reporting pain 24 hours following the application of orthodontic force, (5) medically fit, (6) with no contraindication to use chewing gum or analgesics, and (7) currently not consuming analgesics or antibiotics, were considered in this study. Potential articles were assessed independently and in duplicate by two authors to determine their eligibility to meet the inclusion criteria; the titles, abstracts, and full texts of these articles were carefully assessed. In addition, the references of these articles were reviewed thoroughly to assess their eligibility to meet the inclusion criteria.
Primary Outcome Assessment
The intensity of orthodontic pain reported by patients 1 day after the insertion of an initial archwire was the primary outcome. A visual analog scale (VAS) reported on a 100-mm or a 10-cm scale and a numeric rating scale out of 10 points were used as the outcome assessment tool. In a recent article, the same method of combining these 10-point numerical scales into a single scale was used.24 VAS values reported from multiple functions (while fitting front teeth or back teeth together, while chewing, or when jaws were at rest) were combined into a single estimate using a formula to combine groups, as suggested in the Cochrane handbook of systematic reviews of interventions.25
Data Extraction and Meta-analysis
For the purpose of statistical analysis, two authors performed data extraction from each included study. The extracted data were later entered into Microsoft Excel 2016. The mean VAS reported by patients in each group 1 day after the insertion of the initial archwire, the sample size, and the standard deviation of the mean VAS represented the extracted data. The extracted data were entered into ReviewManager (Revman 5.4.1) software, which is a Cochrane collaboration software designed to run meta-analyses. The standardized mean difference (SMD), also known as effect size or Cohen’s d, was inspected, and the corresponding 95% confidence intervals were estimated for the effect sizes. The Q statistic was conducted to test for heterogeneity in this meta-analysis, and the between-study heterogeneity was assessed using the I2 statistic.
Risk of Bias in Individual Trials
To assess the level of bias among the studies included, two authors evaluated them thoroughly and independently using the Cochrane risk of bias tool.26 The overall quality of the evidence was assessed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach.27
RESULTS
Study Selection and Characteristics
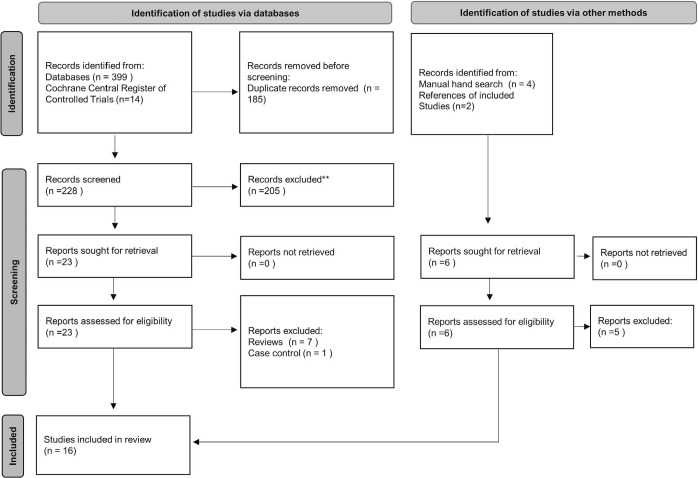
The flowchart in Figure 1 illustrates how many articles were excluded and included at different phases. The total number of studies assessed was 419, and of these, 413 studies were obtained from the electronic search, 4 from the manual search, and 2 by checking the reference lists of the studies included. Following the elimination of duplicates, 29 studies were assessed for possible inclusion in this review. A thorough review of the full texts of these articles led to the exclusion of 13 studies, including 1 case control and 12 reviews. As a result, 16 RCTs were considered in this review. The main characteristics of the studies are shown in Table 1.
Figure 1.
Flowchart showing the process of including and excluding studies at different phases.
Table 1.
Summarized Published Data of the Studies Included in the Systematic Review
|
Study ID |
Participants’ Size, Gender, Age (y), Dropout |
Interventions |
Instructions |
Method of Pain Assessment |
Author Conclusion |
| Basam et al. 202231 | N = 42 (only females); 2 dropouts | Group 1 Chewing gum Mean age = 19.6 y | Group 1 Chew sugar-free gum 10 to 12 min whenever you experience pain | VAS | There was no statistically significant difference between the two groups. Chewing gum was not inferior to tenoxicam. |
| Group 2 Tenoxicam Mean age = 20 y | Group 2 20 mg tenoxicam 1 h before archwire placement | ||||
| Celebi 202241 | N = 57 (27 males, 30 females); no dropouts | Group 1 Mechanical vibration Mean age = 14.1 y | Group 1 N/A | VAS | As compared with the chewing gum, the mechanical vibration has no clinically significant pain relief effect during orthodontic treatment. |
| Group 2 Chewing gum Mean age = 15.1 y | Group 2 Chew sugar-free gum for 20 min After initial wire placement, after 24 h and after 48 h | ||||
| Group 3 Control group Mean age=15.2 | Group 3 No intervention | ||||
| Rossi et al. 202236 | N = 102 (59 females, 30 male); 13 dropouts | Group 1 Placebo | Group 1 Capsules containing harmless material 1 h after initial wire placement and every 8 h | VAS | No difference between the three methods was observed. Chewing gum may be used adequately for orthodontic pain. |
| Group 2 Chewing gum | Group 2 Chew sugar-free gum for 10 min every 4 h | ||||
| Group 3 Ibuprofen | Group 3 400 mg of ibuprofen 1 h after initial wire placement and every 8 h | ||||
| Abdul-Aziz 202137 | N = 60 (24 males, 29 females); 7 dropouts | Group 1 Chewing gum Mean age = 21.8 y | Group 1 Chew sugar-free gum 10 min every 8 hours and immediately after separator placement. | VAS | Compared with the non–chewing gum group, chewing gum reduced pain significantly. |
| Group 2 No intervention Mean age = 22.3 y | Group 2 No intervention | ||||
| Celebi et al. 202140 | N = 63 (30 males, 33 females); no dropouts | Groups 1 Laser Mean age = 15.4 y | Group 1 N/A | VAS | There was no statistically significant difference between the three groups at any time of treatment. |
| Group 2 Chewing gum Mean age = 15.8 y | Group 2 Chew sugar-free gum 20 min three times per day. | ||||
| Control group 3 No intervention Mean age = 15.3 y | Group 3 Control group with no intervention | ||||
| da Silva Santos and Capelli 202135 | N = 106 (52 males, 54 females); 25 dropouts | Group 1 Chewing gum Mean age = 16.6 y | Group 1 Chew sugar-free gum 5 min every 6 h and immediately after archwire placement | VAS | Patients in the chewing gum group experienced less pain during biting and at rest compared with the ibuprofen group and less pain at biting when compared with control and acetaminophen groups. |
| Group 2 Ibuprofen Mean age = 19.2 y | Group 2 Ibuprofen 400 mg every 6 h and immediately after archwire placement | ||||
| Group 3 Acetaminophen Mean age = 19.5 y | Group 3 Acetaminophen 500 mg every 6 h and immediately after archwire placement | ||||
| Group 4 Control Mean age 18.5 | Group 4 Control group with no intervention | ||||
| Al Shayea et al. 202030 | N = 105 (90 females); 15 dropouts | Group 1 Ibuprofen Mean age = 24.7 y | Group 1 Ibuprofen 400 mg three times per day and immediately after archwire placement | VAS | The experience of pain between all groups was similar. Thus, chewing gum can be used to replace ibuprofen. |
| Group 2 Viscoelastic Bite wafer Mean age = 21.8 y | Group 2 Chew on viscoelastic bite wafer three times per day for 5 min Bite wafer | ||||
| Group 3 Chewing gum Mean age = 25.9 y | Group 3 Chew sugar-free gum for 5 min three times per day | ||||
| Delavarian and Imani 202038 | N = 66 (15 males, 35 females); 6 dropouts | Group 1 Placebo Mean age = 18.9 y | Group 1 Placebo 40 mg of vitamin B12 three times per day and immediately after archwire placement | NRS | Patients in the placebo group reported higher pain than those in the chewing gum or the ibuprofen groups. Chewing gum can be used as an alternative to ibuprofen. |
| Group 2 Ibuprofen Mean age = 20.25 y | Group 2 Ibuprofen 400 mg three times per day and immediately after archwire placement | ||||
| Group 3 Chewing gum Mean age = 19.8 y | Group 3 Chewing gum Chew sugar-free gum for 10 min three times per day | ||||
| Alqareer et al., 201929 | N = 75 patients (10 males, 25 females); 40 dropouts | Group 1 Chewing gum Mean age = 16.9 y | Group 1 Chew sugar-free chewing gum 5–10 min three times per day | VAS | Chewing gum does not significantly reduce orthodontic pain compared with placebo. |
| Group 2 Placebo Mean age = 16.1 y | Group 2 Rinse for 30 s with a fluoridated, alcohol-free mouth wash (Plax sensitive) three times per day | ||||
| Alshammari and Huggare 201933 | N = 60 patients (28 males, 32 females); 15 dropouts | Group 1 Chewing gum Mean age = 14.2 y | Group 1 Chew gum 10 minutes 3 times per day. | VAS | Chewing gum and paracetamol are equivalent in the reduction of orthodontic pain without having any negative effect on bracket loss. |
| Group 2 Paracetamol Mean age = 14.3 y | Group 2 Paracetamol 1000 mg or 500 mg three times per day if patient weighs less than 40 kg | ||||
| Azeem et al., 201839 | N = 120 (54 males, 66 females); no dropouts | Group 1 Chewing gum Mean age = 15.6 y | Group 1 Chew sugar-free gum 5 minutes three times per day and immediately after separator placement | VAS | Chewing gum can be recommended as a nonpharmacologic option instead of ibuprofen for orthodontic pain control associated with separator placement. |
| Group 2 Ibuprofen Mean age = 15.5 y | Group 2 Ibuprofen 400 mg four times per day and 1 h before separator placement | ||||
| Ireland et al., 201634 | N = 1000 (370 males, 630 females); 164 dropouts | Group 1 Chewing gum Mean age = 13.7 y | Group 1 Chew gum for pain relief if required and ibuprofen 250 mg if chewing gum is not effective | VAS | The use of sugar-free chewing gum after fixed appliance placement reduces the need for ibuprofen without having any significant effect on the bracket. |
| Control group 2 Ibuprofen Mean age = 13.6 y | Group 2 Ibuprofen 250 mg when required | ||||
| Ul-Hamid et al., 201642 | N = 250 (133 males, 117 females); mean age 14.03 y; no dropouts | Group 1 Chewing gum | Group 1 Chew a sugar-free gum (Orbit; The Wrigley Company) for 5 min immediately after this and repeated three times per day | VAS | Chewing gum was more effective in reducing orthodontic pain when compared with ibuprofen. This difference in the reduction in pain intensity was statistically significant. |
| Group 2 Ibuprofen | Group 2 400 mg ibuprofen immediately after first visit and repeated three times per day | ||||
| Nadeem et al., 201643 | N = 60 (29 males, 31 females); no dropouts | Group 1 Chewing gum | Group 1 Chew sugar-free gum twice daily for 10 min and after initial wire placement | VAS | A statistically significant reduction in orthodontic pain was reported in the chewing gum group. |
| Group 2 No intervention | Group 2 Control group with no intervention | ||||
| Farzanegan et al., 201228 | N = 50; 50 females; no dropouts | Group 1 Placebo | Group 1 B6 vitamin after archwire placement and three times per day for 1 wk | VAS | Both chewing gum and bite wafer can reduce pain intensity in orthodontic patients and can be used as nonpharmacologic substitutes for ibuprofen. |
| Group 2 Ibuprofen | Group 2 400 mg ibuprofen after archwire placement and three times per day for 1 wk if pain persisted | ||||
| Group 3 Chewing gum | Group 3 Chew a sugar-free gum (orbit) for 5 min after archwire placement and three times per day for 1 wk | ||||
| Group 4 Hard wafer | Group 4 and 5 Bite on wafer for 5 min three times per day | ||||
| Group 5 Soft wafer | |||||
| Benson et al., 201232 | N = 57 (31 males, 26 females); no dropouts | Group 1 Chewing gum Mean age = 13.8 y | Group 1 Chew sugar-free gum (Orbit Complete) when required at the bonding/separator appointments | VAS | Chewing gum reduced pain from fixed orthodontic appliances without causing appliance breakage. |
| Group 2 No chewing gum Mean age = 14.7 y | Group 2 Non–chewing gum group was specifically asked not to chew gum for the duration of the study |
Risk of Bias Within Studies
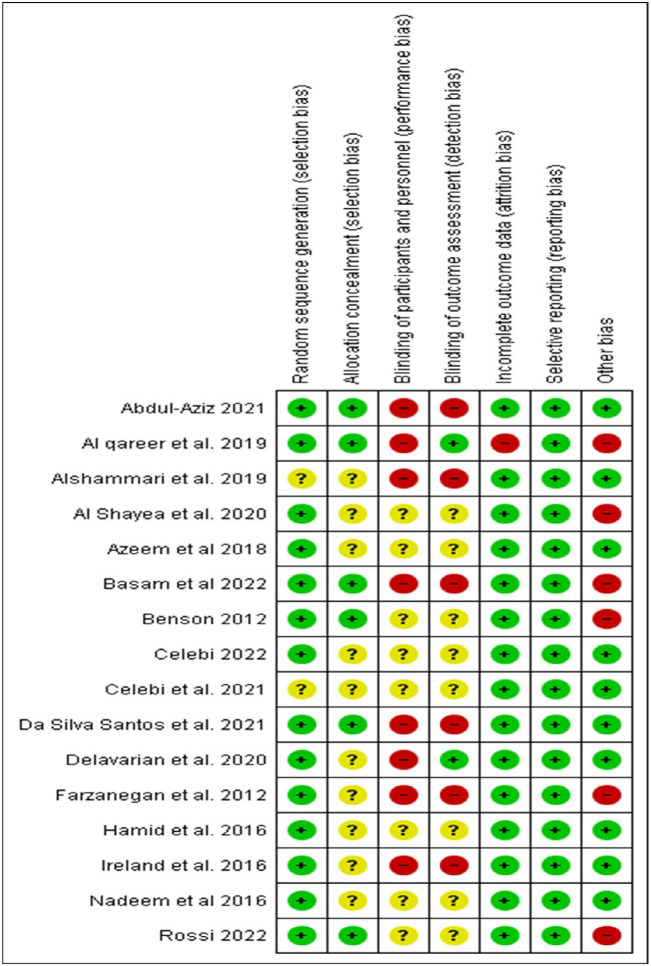
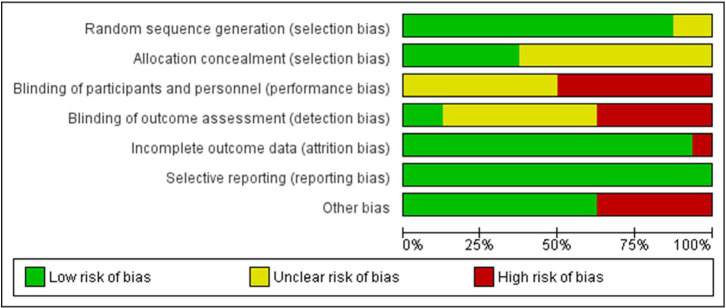
Figures 2 and 3 illustrate the results of the Cochrane risk of bias tool. According to the quality of the evidence, 10 articles were evaluated as having a high risk of bias,28–37 1 article was evaluated as having moderate risk of bias,38 and 5 articles were evaluated as having unclear risk of bias,39–43 either due to a lack of information regarding random sequence generation, randomization, allocation concealment, or blinding the outcome assessors and blinding the patients.
Figure 2.
Results of the Cochrane risk of bias tool for quality assessment.
Figure 3.
Results of the Cochrane risk of bias tool for quality assessment presented as percentages.
The quality of the evidence across studies was evaluated according to the GRADE approach, and it was found that there was a very low quality of evidence (Table 2).
Table 2.
Summary of Overall Quality of Evidence of Studies Included in Each Meta-analysis Using GRADE:
|
Certainty Assessment | ||||||||
|
Outcome |
Number of Studies |
Study Design |
Risk of Bias |
Inconsistency |
Indirectness |
Imprecision |
Others |
Certainty |
| Chewing gum vs pharmacological agents | 7 | RCTs | Seriousa | Seriousb | Seriousc | Not serious | Not serious | ⊕○○○ Very low |
| Chewing gum vs placebo | 4 | RCTs | Seriousa | Seriousd | Not serious | Seriouse | Not serious | ⊕○○○ Very low |
| Chewing gum vs hard bite wafer | 2 | RCTs | Seriousa | Seriousf | Not serious | Seriouse | Not serious | ⊕○○○ Very low |
Downgraded due to unclear or absence of blinding of both patients and outcome assessors.
Downgraded due to high heterogeneity (P < .00001); I2 = 88%.
Downgraded due to the inclusion of studies that reported mean pain at 24 h in females only.
Downgraded due to moderate level of heterogeneity; I2 = 44%.
Downgraded due to small sample size.
Downgraded due to small number of studies and imprecise I2.
Results of Individual Studies
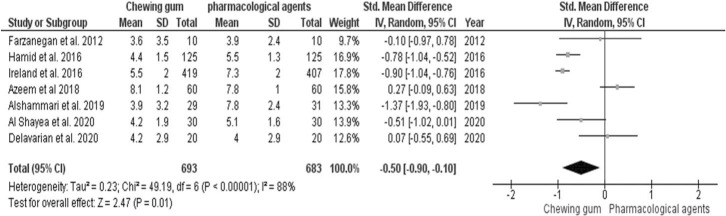
Chewing gum vs pharmacologic agents.
Seven randomized controlled trials28,30,33,34,38,39,42 compared the effect of chewing gum and pharmacologic agents (ibuprofen and paracetamol) on the reduction in pain 1 day after the insertion of an initial archwire, as seen in Figure 4. Statistically significant study heterogeneity was found (χ2 = 49.19, I2 = 88%; P < .00001). Therefore, the analysis was conducted using a random effect model. There was a statistically significant difference in the reduction in pain intensity between the chewing gum and the pharmacologic interventions. The SMD was −0.50 ([−0.90, −0.10], P = .01).
Figure 4.
A comparison between chewing gum and pharmacological interventions in decreasing pain intensity.
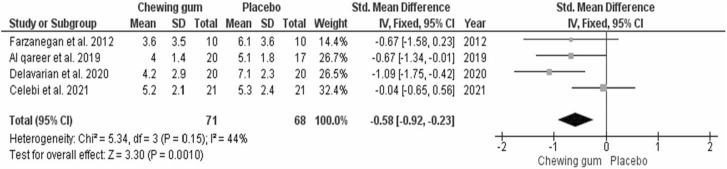
Chewing gum vs placebo.
Four randomized controlled trials28,29,38,40 compared the effect of chewing gum and a placebo on the reduction in pain 1 day after the insertion of an initial archwire, as seen in Figure 5. No statistically significant study heterogeneity was found (χ2 = 5.34, I2 = 44%; P = .15). Therefore, the analysis was conducted using a fixed effect model. There was a statistically significant difference in the reduction in pain intensity between the chewing gum and the placebo. The SMD was −0.60 ([−1.06, −0.13], P = .01).
Figure 5.
A comparison between chewing gum and placebo in decreasing pain intensity.
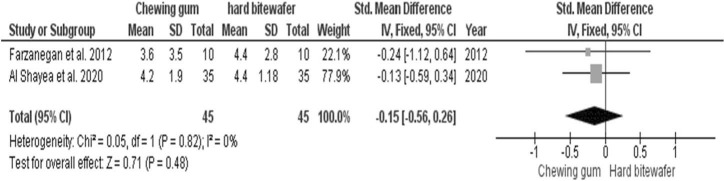
Chewing gum vs hard viscoelastic bite wafer.
Only two randomized controlled trials28,30 compared the effect of chewing gum and a hard viscoelastic bite wafer on the reduction in pain 1 day after the insertion of an initial archwire, as seen in Figure 6. No statistically significant study heterogeneity was found (χ2 = 0.05, I2 = 0%; P = .82). Therefore, the analysis was conducted using a fixed effect model. No statistically significant difference was found between the hard bite wafer and the chewing gum. The SMD was −0.15 ([−0.56, −0.26], P = .48).
Figure 6.
A comparison between chewing gum and viscoelastic bite wafer in decreasing pain intensity.
DISCUSSION
This was the first meta-analysis to directly investigate the role of chewing gum in the reduction in pain intensity during fixed orthodontic treatment.
Four studies reported median VAS pain scores but not the means. As a result, these studies were excluded from the quantitative analysis. Benson et al.32 compared patients who received chewing gum to those who did not receive any treatment. There was no statistically significant difference in the median VAS between the two groups.32 However, this study had an unequal gender distribution between the two groups, with more female participants in the non–chewing gum group and more male participants in the chewing gum group. In addition, the participants in the chewing gum group were instructed to chew only sugar-free gum if needed, and the patients in both groups were instructed to take painkillers if required.
Da Silva Santos and Capelli35 investigated the difference in pain intensity during different functions between patients who received chewing gum and those who received pharmacologic agents. The patients in the chewing gum group experienced less pain during biting and at rest compared with those who received ibuprofen and less pain when biting when compared with the control and acetaminophen groups.35
Basam et al.31 compared the pain intensity between patients who received chewing gum and those who received 20 mg of tenoxicam. Comparing the two groups 1 day after the placement of initial archwires, the patients in the chewing gum group experienced less pain when chewing, and the patients in the tenoxicam group experienced less pain when both biting and fitting their posterior teeth together. However, there was no statistically significant difference between the two groups.31
Celebi41 investigated the difference among mechanical vibration, chewing gum, and control groups. There was no statistically significant difference among the interventions at any time point during the treatment.41 The results of that study can be questioned due to the participants’ minimal exposure to the intervention during treatment as compared with other studies included in this review, as the patients were instructed to chew sugar-free gum for only 20 minutes at three time points.
According to Rossi et al.,36 the reduction in pain intensity during initial orthodontic treatment caused by ibuprofen, chewing gum, and the placebo was not statistically significant.
Nadeem et al.43 compared the reported pain intensity between patients in the chewing gum group and those who did not receive any intervention. In the chewing gum group, the median visual analog scale of the reported pain was significantly less after 24 hours and after 1 week of chewing sugar-free gum for 10 minutes twice a day over a period of 1 week.43 Similarly, patients who received sugar-free gum and were instructed to chew three times a day over a period of 1 week reported a statistically significant decrease in pain intensity compared with patients who received no intervention.37
The results of the current meta-analysis revealed a statistically significant reduction in pain intensity after 24 hours of the application of orthodontic force between chewing gum and the placebo as well as chewing gum and pharmacologic agents.
Wiedel et al.44 investigated the difference in the pain intensity experienced by patients undergoing fixed appliance treatment vs those undergoing removable appliance treatment. The results of that randomized controlled trial revealed that patients undergoing removable appliance therapy experienced less pain intensity in the first few days of treatment compared with those who received fixed appliance therapy.44 Therefore, patients undergoing fixed orthodontic treatment may benefit from chewing gum alone or in combination with analgesics by alleviating pain, improving quality of life, and reducing analgesic consumption.
In a few studies, the authors reported that pain was experienced by the participants when performing multiple jaws functions,28,33,36 and it is important to consider that the sensation of pain differs from function to function or when the jaws are at rest.33 Therefore, future studies should focus more on how chewing gum reduces the pain intensity during different functions in order to gain a better understanding of its role.
In this meta-analysis, the evidence was synthesized 24 hours following the activation of orthodontic force. This limitation can be attributed to differences in reporting the VAS at different time points among the included RCTs. Therefore, future studies regarding chewing gum should investigate the intensity of pain at similar and multiple time points. In addition, the results of the Cochrane risk of bias tool revealed a high risk of bias among the studies included, and the quality of evidence across the studies was graded according to the results of GRADE approach to be a very low quality of evidence, which belongs to the GRADE’s category stating that “we have very little confidence in the effect estimate; the true effect is likely to be substantially different from the estimate of effect.”
CONCLUSIONS
In patients undergoing fixed orthodontic therapy, chewing gum is an effective intervention for reducing orthodontic pain after 24 hours of initial wire placement.
Chewing gum may be considered a good substitute for pharmacologic interventions during fixed orthodontic treatment.
The results of the GRADE approach revealed a very low quality of evidence across the studies included and emphasized the need for better quality RCTs regarding the role of chewing gum in reducing orthodontic pain so that future practice can be based on scientific evidence.
REFERENCES
- 1. Jones ML. An investigation into the initial discomfort caused by placement of an archwire. Eur J Orthod. 1984;6:48–54. doi: 10.1093/ejo/6.1.48. [DOI] [PubMed] [Google Scholar]
- 2. Oliver RG, Knapman YM. Attitudes to orthodontic treatment. Br J Orthod. 1985;12:179–188. doi: 10.1179/bjo.12.4.179. [DOI] [PubMed] [Google Scholar]
- 3. Jones MCC. The pain and discomfort experienced during orthodontic treatment: a randomized controlled clinical trial of two aligning archwires. Am J Orthod Dentofacial Orthop. 1992;102:373–381. doi: 10.1016/0889-5406(92)70054-e. [DOI] [PubMed] [Google Scholar]
- 4. Needleman HLHCD, Allred E, Hertzberg J, Berde C. Reports of pain by children undergoing rapid palatal expansion. Pediatr Dent. 2000;22:221–226. [PubMed] [Google Scholar]
- 5. Bondemark L, Fredriksson K, Ilros S. Separation effect and perception of pain and discomfort from two types of orthodontic separators. World J Orthod. 2004;5:172–176. [PubMed] [Google Scholar]
- 6. Scheurer PA, Firestone AR, Bürgin WB. Perception of pain as a result of orthodontic treatment with fixed appliances. Eur J Orthod. 1996;18:349–357. doi: 10.1093/ejo/18.4.349. [DOI] [PubMed] [Google Scholar]
- 7. Lew KK. Attitudes and perceptions of adults towards orthodontic treatment in an Asian community. Community Dent Oral Epidemiol. 1993;21:31–35. doi: 10.1111/j.1600-0528.1993.tb00715.x. [DOI] [PubMed] [Google Scholar]
- 8. Wilson S, Ngan P, Kess B. Time course of the discomfort in young patients undergoing orthodontic treatment. Pediatr Dent. 1989;11:107–110. [PubMed] [Google Scholar]
- 9. Bergius M, Berggren U, Kiliaridis S. Experience of pain during and orthodontic procedure. Eur J Oral Sci. 2002;110:92–98. doi: 10.1034/j.1600-0722.2002.11193.x. [DOI] [PubMed] [Google Scholar]
- 10. Krishnan V, Davidovitch Z. Cellular, molecular, and tissue-level reactions to orthodontic force. Am J Orthod Dentofacial Orthop. 2006;129:469e1–e32. doi: 10.1016/j.ajodo.2005.10.007. [DOI] [PubMed] [Google Scholar]
- 11. Arias OR, Marquez-Orozco MC. Aspirin, acetaminophen, and ibuprofen: their effects on orthodontic tooth movement. Am J Orthod Dentofacial Orthop. 2006;130:364–370. doi: 10.1016/j.ajodo.2004.12.027. [DOI] [PubMed] [Google Scholar]
- 12. Bradley RL, Ellis PE, Thomas P, Bellis H, Ireland AJ, Sandy JR. A randomized clinical trial comparing the efficacy of ibuprofen and paracetamol in the control of orthodontic pain. Am J Orthod Dentofacial Orthop. 2007;132:511–517. doi: 10.1016/j.ajodo.2006.12.009. [DOI] [PubMed] [Google Scholar]
- 13. Bernhardt MK, Southard KA, Batterson KD, Logan HL, Baker KA, Jakobsen JR. The effect of preemptive and/or postoperative ibuprofen therapy for orthodontic pain. Am J Orthod Dentofacial Orthop. 2001;120:20–27. doi: 10.1067/mod.2001.115616. [DOI] [PubMed] [Google Scholar]
- 14. Karthi M, Anbuslevan GJ, Senthilkumar KP, Tamizharsi S, Raja S, Prabhakar K. NSAIDs in orthodontic tooth movement J Pharm Bioallied Sci 2012. 4 (suppl 2): S304 S306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. McAlinden RL, Ellis PE, Sandy JR. Report of an adverse incident in a randomized clinical trial. J Orthod. 2005;32:203–205. doi: 10.1179/146531205225021105. [DOI] [PubMed] [Google Scholar]
- 16.Proffit WR, Fields HW, Sarver DM. Contemporary Orthodontics. St. Louis, Mo: Mosby Elsevier; 2007. [Google Scholar]
- 17. Kaae JK, Stenfeldt L, Hyrup B, Brink C, Eriksen JG. A randomized phase III trial for alleviating radiation-induced xerostomia with chewing gum. Radiother Oncol. 2020;142:72–78. doi: 10.1016/j.radonc.2019.09.013. [DOI] [PubMed] [Google Scholar]
- 18. Aheer PA, Parmar P, Majid SA, Bashyam M, Kousalya PS, Marriette TM. Effect of sugar-free chewing gum on plaque and gingivitis among 14–15-year-old school children: a randomized controlled trial. Indian J Dent Res. 2019;30:61–66. doi: 10.4103/ijdr.IJDR_247_17. [DOI] [PubMed] [Google Scholar]
- 19. Ammut R, Trapani J, Deguara J, Ravasi V. The effect of gum chewing on postoperative ileus in open colorectal surgery patients: a review. J Perioper Pract. 2021;31:132–139. doi: 10.1177/1750458920917015. [DOI] [PubMed] [Google Scholar]
- 20. Arakawa I, Abou-Ayash S, Genton L, et al. Reliability and comparability of methods for assessing oral function: chewing, tongue pressure and lip force. J Oral Rehabil. 2020;47:862–871. doi: 10.1111/joor.12976. [DOI] [PubMed] [Google Scholar]
- 21. Kugimiya Y, Watanabe Y, Shirobe M, et al. A comparison of colorimetric and visual methods for the assessment of masticatory performance with color-changeable chewing gum in older persons. J Dent Sci. 2021;16:380–388. doi: 10.1016/j.jds.2020.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wallstrom A, Frisman GH. Facilitating early recovery of bowel motility after colorectal surgery: a systematic review. J Clin Nurs. 2014;23:24–44. doi: 10.1111/jocn.12258. [DOI] [PubMed] [Google Scholar]
- 23. Nelson G, Bakkum-Gamez J, Kalogera E, et al. Guidelines for perioperative care in gynecologic/oncology: Enhanced Recovery After Surgery (ERAS) Society recommendations-2019 update. Int J Gynecol Cancer. 2019;29:651–668. doi: 10.1136/ijgc-2019-000356. [DOI] [PubMed] [Google Scholar]
- 24. Mbizvo GK, Nolan SJ, Nurmikko TJ, Goebel A. Placebo responses in longstanding complex regional pain syndrome: a systematic review and meta-analysis. J Pain. 2015;16:99–115. doi: 10.1016/j.jpain.2014.11.008. [DOI] [PubMed] [Google Scholar]
- 25. Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions: Version 5.1.0 (updated March 2011). London, UK: Cochrane Collaboration; 2011. [Google Scholar]
- 26. Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomized trials. BMJ. 2011;343:d5928. doi: 10.1136/bmj.d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Balshem H, Helfand M, Schunemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64:401–406. doi: 10.1016/j.jclinepi.2010.07.015. [DOI] [PubMed] [Google Scholar]
- 28. Farzanegan F, Zebarjad SM, Alizadeh S, Ahrari F. Pain reduction after initial archwire placement in orthodontic patients: a randomized clinical trial. Am J Orthod Dentofacial Orthop. 2012;141:169–173. doi: 10.1016/j.ajodo.2011.06.042. [DOI] [PubMed] [Google Scholar]
- 29. Alqareer A, Alyahya A, Al-Anezi SA, AlAwadhi A, Al Qabandi S, Alyaseen M. Efficacy of chewing gum to reduce orthodontic pain compared to placebo: a blinded, parallel-group, preliminary clinical trial. J Oral Facial Pain Headache. 2019;33:301–307. doi: 10.11607/ofph.2192. [DOI] [PubMed] [Google Scholar]
- 30. Al Shayea EI. Comparative assessment between ibuprofen, chewing gum, and bite wafers in pain control following first archwire placement in orthodontic patients. J Contemp Dent Pract. 2020;21:416–420. [PubMed] [Google Scholar]
- 31. Basam LC, Singaraju GS, Obili S, et al. Orthodontic pain control following arch wire placement; a comparison between pre-emptive tenoxicam and chewing gum: a randomized clinical trial. J Dent Anesth Pain Med. 2022;22:107–116. doi: 10.17245/jdapm.2022.22.2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Benson PE, Razi RM, Al-Bloushi RJ. The effect of chewing gum on the impact, pain and breakages associated with fixed orthodontic appliances: a randomized clinical trial. Orthod Craniofac Res. 2012;15:178–187. doi: 10.1111/j.1601-6343.2012.01546.x. [DOI] [PubMed] [Google Scholar]
- 33. Alshammari AK, Huggare J. Pain relief after orthodontic archwire installation a comparison between intervention with paracetamol and chewing gum: a randomized controlled trial. Eur J Orthod. 2019;41:478–485. doi: 10.1093/ejo/cjy081. [DOI] [PubMed] [Google Scholar]
- 34. Ireland AJ, Ellis P, Jordan A, et al. Comparative assessment of chewing gum and ibuprofen in the management of orthodontic pain with fixed appliances: A pragmatic multicenter randomized controlled trial. Am J Orthod Dentofacial Orthop. 2016;150:220–227. doi: 10.1016/j.ajodo.2016.02.018. [DOI] [PubMed] [Google Scholar]
- 35. Da Silva Santos DJ, Capelli J., Jr. Chewing gum as a non-pharmacological alternative for orthodontic pain relief: a randomized clinical trial using an intention-to-treat analysis. Korean J Orthod. 2021;51:346–354. doi: 10.4041/kjod.2021.51.5.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Rossi S, Santamaria M, Junior, Venezian GC, et al. A double-blinded randomized clinical trial of pain perception during orthodontic treatment. Rev Odontol UNESP. 2022;51:e20220007. [Google Scholar]
- 37. Abdul-Aziz AI. Effect of chewing gum on pain following orthodontic elastomeric separators placement: a randomized controlled trial. Open Access Maced J Med Sci. 2021;9:134–138. [Google Scholar]
- 38. Delavarian M, Imani M. Comparison of chewing gum and ibuprofen in alleviating orthodontic pain: a single centre, randomised clinical trial. Aust Orthod J. 2020;36:38–44. [Google Scholar]
- 39. Azeem M, Khanb DI, Jamalb F, et al. Chewing gum for pain control following orthodontic separator placement. J World Fed Orthod. 2018;7((3)):102–105. [Google Scholar]
- 40. Celebi F, Bicakci AA, Kelesoglu U. Effectiveness of low-level laser therapy and chewing gum in reducing orthodontic pain: a randomized controlled trial. Korean J Orthod. 2021;51:313–320. doi: 10.4041/kjod.2021.51.5.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Çelebi F. Mechanical vibration and chewing gum methods in orthodontic pain relief. Turk J Orthod. 2022;35:133–138. doi: 10.5152/TurkJOrthod.2022.21091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Ul-Hamid MW, Ul-Haq A, Mahmoud HS, Muhammed A, Irfan S. Comparison between Ibuprofen and chewing gum for orthodontic control. Pakistan Oral Dent J. 2016;36:79–83. [Google Scholar]
- 43. Nadeem M, Tariq J, Kamran MA, et al. Effect of chewing gum on pain in fixed orthodontic treatment. 2016;21:94–99. [Google Scholar]
- 44. Wiedel A-P, Bondemark L. A randomized controlled trial of self-perceived pain, discomfort, and impairment of jaw function in children undergoing orthodontic treatment with fixed or removable appliances. Angle Orthod. 2016;86:324–330. doi: 10.2319/040215-219.1. [DOI] [PMC free article] [PubMed] [Google Scholar]