Abstract
Background:
Nearly all surgeons have restrictive post-operative feeding protocols in place following primary cleft lip and cleft palate repairs. There are no standardized recommendations, potentially resulting in widely variable practices among cleft surgeons and teams. The purpose of this study was to examine current post-operative feeding practices for infants with cleft palate following lip and palate repairs.
Methods:
A survey of 50 questions was sent to members of the American Cleft Palate-Craniofacial Association (ACPA). Inclusion criteria included providers from North America that have either currently or previously served on a cleft palate team and reached the surgical question set within the survey.
Results:
64 respondents met inclusion criteria. The majority were in speech-language pathology (47%) or nursing (41%) disciplines, involved in feeding consultations frequently (84%), and working in an outpatient setting (69%). Following lip surgery, respondents recommended cleft-adapted bottle feeding (88%), spoon feeding (9%), cup feeding (13%), and syringe/squeeze bottle feeding (23%). The majority of respondents (69%) indicated infants could return to their pre-operative feeding modality immediately after lip surgery. Following palate surgery, respondents recommended cleft-adapted bottle feeding (55%), typical bottle feeding (3%), spoon feeding (36%), cup feeding (64%), and syringe/squeeze bottle feeding (30%). Infants could use a feeding system that required suction at an average of 20 days post-operatively and return to an age-appropriate diet at an average of 15 days post-operatively.
Conclusions:
The present study describes the wide variation of post-operative feeding guidelines used by cleft teams following lip and palate repairs.
Keywords: cleft palate, feeding, palatoplasty, cheiloplasty
INTRODUCTION
Most infants born with cleft palate with or without cleft lip will undergo surgical repairs while still in infancy. The goal of cleft lip repair, or cheiloplasty, is to restore the function of the orbicularis oris muscle and to achieve a favorable cosmetic outcome1. The primary goal of cleft palate repair, or primary palatoplasty, is to achieve adequate velopharyngeal closure for speech purposes2. One barrier to achieving these outcomes is wound healing complications, such as lip or palate dehiscence or development of a palatal fistula post-operatively. In order to prevent post-surgical wound complications, surgeons and associated cleft and craniofacial teams may implement restrictive feeding protocols and the use of arm restraints immediately after surgery.
For infants born with a cleft lip, cheiloplasty is commonly performed between 2–5 months of age with variations in timing stemming from the use of presurgical orthopedics and cleft type. Following lip repair, restrictive feeding protocols may include spoon or cup feeding only, even if spoon and cup feeding have not been previously introduced to the infant. Cohen and colleagues (1992) studied the difference between restrictive feeding, such as syringe or spoon feeding only, versus bottle-feeding in infants after cheiloplasty and found no association between unrestricted bottle feeding and lip dehiscence3–8. Similarly, Assuncao (2005) studied the difference between spoon feeding and unrestricted bottle feeding and found no difference in nutritional status between spoon and bottle feeding while the infant is healing9. Despite these findings in support of immediately returning to bottle feeds following surgery, restrictive feeding is still a common practice in the United States.
Regarding primary palatoplasty, age at surgery typically varies between 6–12 months for infants born in the United States. Common post-operative restrictions following palate repair include open cup-feeding, spoon feeding, and liquid-only diets. Cohen and colleagues (1992) studied syringe feeding versus bottle feeding after palatoplasty and found that returning to the bottle after palate repair does not result in increased post-operative complications, such as fistula formation3. Jigjinni et al. (1993) looked at 46 patients who returned to bottle feeding after palate repair10. Patients were randomized into two groups: using arm restraints versus no arm restraints. No significant difference was observed between groups regarding fistula formation, and all patients were bottle-fed. Another study found that infants who returned to bottle feeding versus cup or spoon feeding had higher volume intake by day 6 post-operation11. However, post-operative restrictions are still commonly implemented in clinical practice, and many times to a greater degree than after lip surgery. It is also unclear in the literature if bottle feeding after palate repair indicates a bottle that requires suction or a cleft-adapted bottle system that works via compression.
In addition to feeding restrictions, some providers also implement various restraints following lip and/or palate surgery. In a 2009 survey by Katzel and colleagues, it was reported that 85% of surgeons used arm restraints after palate repair12. The duration of arm restraint use following both types of repairs is reported to vary widely from 2–42 days, with a majority of surgeons recommending the use of arm restraints for 2 weeks12. Several studies show that the use of arm restraints following both lip and palate repair is not associated with wound complications or fistula formation4, 6, 10, 13–16. Further, no association has been found between thumb sucking (or fingers in the mouth) and fistula formation after palate repair15. The cost savings of eliminating arm restraints and the distress caused to both patients and caregivers has been called into question16.
Despite recent literature, nearly all surgeons have restrictive post-operative protocols in place12. However, there is no standard recommendation or protocol, resulting in practices that are widely variable among teams. The purpose of this study was to examine current practices in post-operative feeding care following cleft lip and palate repairs for infants with cleft palate from the perspective of feeding providers. These findings will then be contextualized within the current evidence base.
MATERIALS AND METHODS
Approval to conduct the research was granted by the University of Wyoming Institutional Review Board. Themes arising from semi-structured interviews with a small group of expert feeding providers for infants with cleft palate were explored in this survey17. The 50-question survey included 3 sections: (1) respondent demographics, (2) provider practice patterns, and (3) training and education within this area. The survey was piloted to ensure face and content validity, and the questions were revised accordingly. The Wyoming Survey and Analysis Center also reviewed survey questions to resolve any potential bias.
The survey, which included binary and multiple-choice questions, Likert-scale items, and open-ended responses, was assembled in Qualtrics XM Software, an online survey tool (Qualtrics XM, 2021, Provo, UT). Skip logic and forced-choice were employed to ensure that each question was relevant for each respondent, with the exception of open-ended response questions, which explored additional, less-prevalent feeding topics and allowed respondents to provide relevant information that could direct future recommendations. Since interdisciplinary healthcare professionals regularly involved in feeding infants with cleft palate were the target population for this survey, members of the American Cleft Palate-Craniofacial Association (ACPA) received a link to the consent form and 10-minute survey electronically either through the ACPA Online Community, a QR code at the ACPA 79th Annual Meeting, or via a direct email to the cleft team contact.
The data were imported from Qualtrics into SPPS Version 28.0 for data analysis. Descriptive statistics were used to identify the frequency of response to each relevant question. A one-way analysis of variance (ANOVA) was used to determine the relationship between provider demographics and practice patterns with post-operative restrictions.
RESULTS
Of the 87 respondents that consented to participate, 79 indicated they provided feeding services to infants with craniofacial differences as part of a cleft team (either currently or in the past). Due to the electronic distribution of the survey a response rate could not be calculated; however, respondents were judged to be a representative sample of practitioners that provide feeding services to infants with cleft palate. Exclusion criteria were then applied to control for availability of resources and dropout, which removed any providers outside of North America and those that did not complete at least the first surgically-related question of the survey. Thus, 64 healthcare providers were included in the analysis. This group of respondents can be categorized as experts within the area of cleft palate feeding, as the vast majority reported dedicating an average of 62.45% of their time to patients with cleft lip and palate and being involved in feeding consultations for infants with cleft lip and palate very frequently (58%, n=37) or somewhat frequently (27%, n=17).
Respondents in this analysis included speech-language pathologists (47%, n=30), nurses/nurse practitioners (41%, n=26), physician assistants (6%, n=4), occupational therapists (3%, n=2), a single dietitian, and a single dual certified lactation consultant/nurse. Respondents ranged in age from their 20s to 70s, specifically 20–29 years (11%, n=7), 30–39 years (28%, n=18), 40–49 years (23%, n=15), 50–59 years (13%, n=8), 60–69 years (24%, n=15), and 70–79 years (2%, n=1). Discipline-specific experience varied, and the survey included respondents that had varied experience both within their discipline and practicing in craniofacial care. Respondents reported practicing in their discipline for: <1 year (3%, n=2), 1–5 years (16%, n=10), 6–10 years (16%, n=10), 11–15 years (13%, n=8), 16–20 years (13%, n=8), and 21+ years (41%, n=26). Overall, providers had practiced in their discipline longer than they had practiced in craniofacial care. Years of experience in reported craniofacial-specific experience included: <1 year (6%, n=4), 1–5 years (30%, n=19), 6–10 years (16%, n=10), 11–15 years (11%, n=7), 16–20 years (16%, n=10), and 21+ years (22%, n=14) experience. The vast majority of respondents reported working in an outpatient (69%, n=44) or inpatient hospital setting (17%, n=11).
Practices Following Lip Repair
Variations in post-surgical recommendations were observed across respondents following lip surgery. Respondents recommended cleft-adapted bottle feeding or pre-operative system (88%, n=56), spoon feeding (9%, n=9), cup feeding (13%, n=8), and syringe/squeeze bottle feeding (23%, n=15) following lip surgery (Figure 1A). No one recommended a feeding obturator. While the majority of respondents (69%, n=44) indicated infants could return to their pre-operative feeding modality immediately (0 days) after lip surgery, feeding restrictions ranged from 0–30 days. The most common post-operative restrictions included no hard objects near the mouth (83%, n=53), arm restrains (75%, n=48), and/or no pacifiers (56%, n=36). A liquid diet (41%, n=26), mittens (11%, n=7), and soft diet (22%, n=14) were also recommended albeit less frequently (Figure 1B). No restrictions were noted by 3 respondents (5%), and 3 also noted other restrictions, such as using a CozeeCoo (swaddle blanket) or limited pacifier use.
Figure 1.
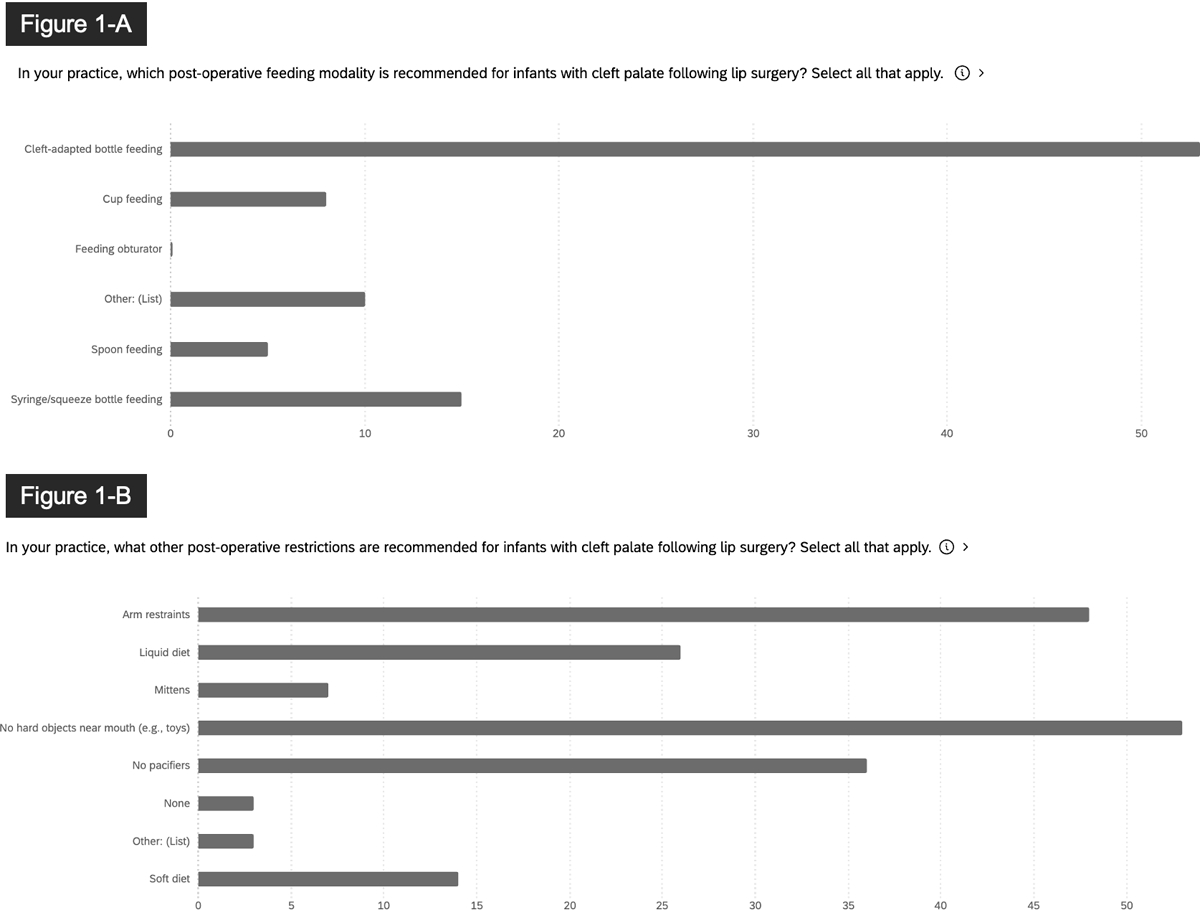
Participant responses to the questions (A) In your practice, which post-operative feeding modality is recommended for infants with cleft palate following lip surgery? (B) In your practice, what other post-operative restrictions are recommended for infants with cleft palate following lip surgery?
Practices Following Palate Repair
A greater number of restrictions with more inconsistency was reported post-palate repair. Following palate surgery, respondents recommended cleft-adapted bottle feeding or pre-operative system (55%, n=35), typical bottle feeding (3%, n=2), spoon feeding (36%, n=23), cup feeding (64%, n=41), and syringe/squeeze bottle feeding (30%, n=19) (Figure 2A). Other restrictions were noted by 8 respondents (13%), including pureed diet and use of a sippy cup (pouring, no straw). After palate repair, infants could use a feeding system that required suction at an average of 20 days (SD = 16 days) post-operatively, with responses ranging from 0–90 days. Infants could return to an age-appropriate diet following palate repair at an average of 15 days (SD = 13 days) post-operatively, with responses ranging from 0–42 days. Figure 3 includes boxplots demonstrating the variation in length of time for post-operative restrictions. Similar to lip repair recovery, the most common post-operative restrictions following palatoplasty included no hard objects near the mouth (92%, n=59), arm restrains (75%, n=48), and/or no pacifiers (73%, n=47). A soft diet (64, n=41%), a liquid diet (50%, n=32), and mittens (8%; n=5) were also recommend, although less frequently (Figure 2B). Nine respondents (14%) noted other restrictions, including CozeeCoo, pureed diet, no straws, or “nothing harder than a cooked noodle.” Pureed diet was mentioned by 6 respondents (9%). A one-way analysis of variance (ANOVA) revealed no significant associations between provider characteristics/practices and post-operative restrictions.
Figure 2.
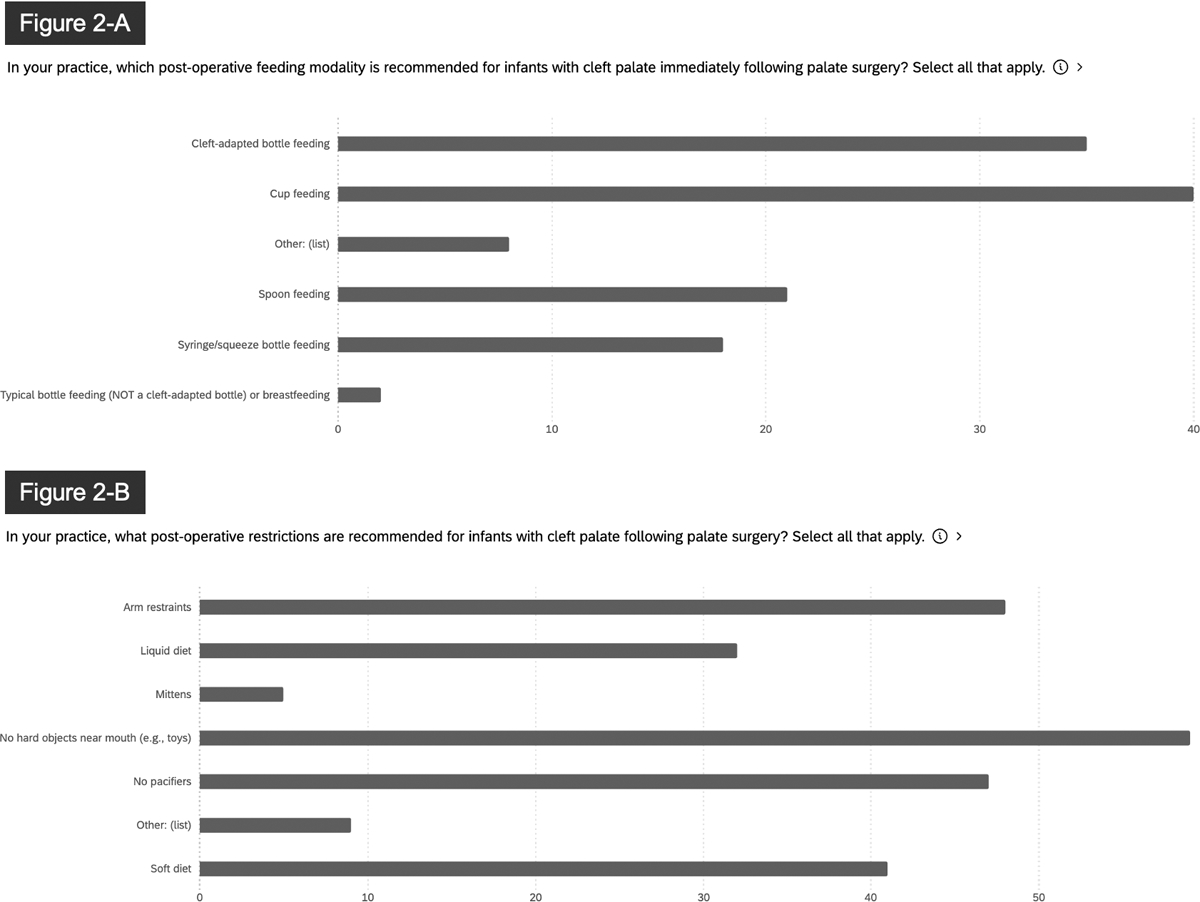
Participant responses to the questions: (A) In your practice, which post-operative feeding modality is recommended for infants with cleft palate immediately following palate surgery? (B) In your practice, what post-operative restrictions are recommended for infants with cleft palate following palate surgery?
Figure 3.
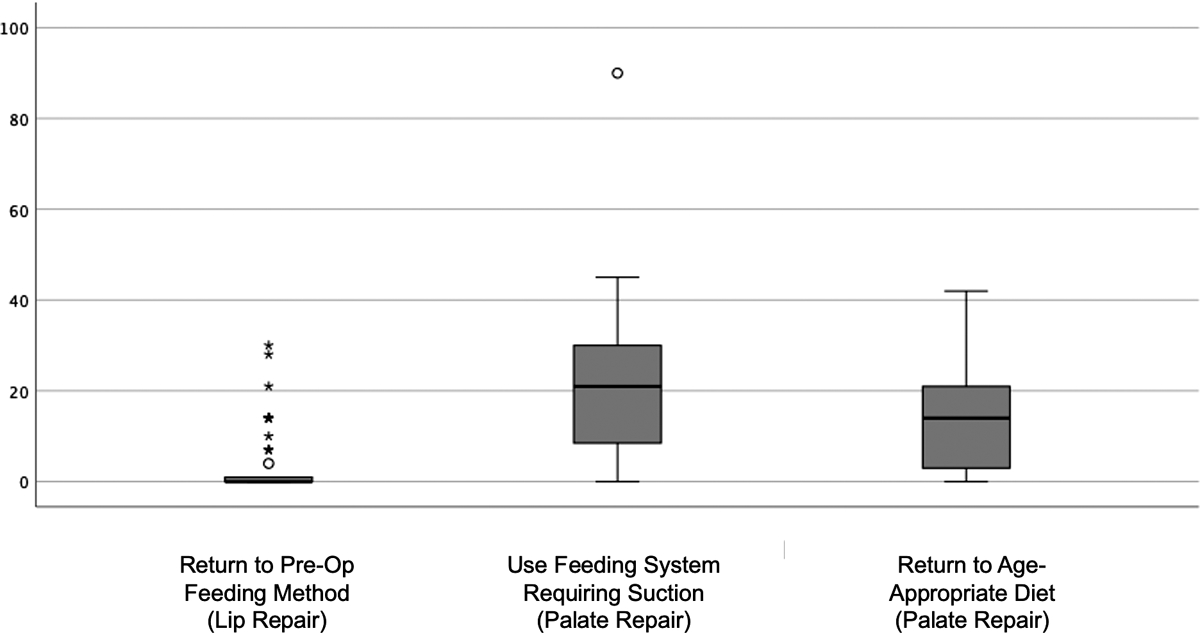
Boxplots showing frequency of responses related to post-surgical restrictions following lip or palate surgery.
DISCUSSION
The present study surveyed a group of 64 current feeding providers to determine which post-operative restrictions are utilized following both lip and palate surgery for infants born with cleft palate. The majority of these providers were speech-language pathologists or nurses that were involved in feeding consultations frequently and working in an outpatient setting. Following lip surgery, respondents recommended cleft-adapted bottle feeding most frequently, but some also recommended spoon feeding, cup feeding, or syringe/squeeze bottle feeding. Following palate surgery, respondents recommended cup feeding most commonly, but some also recommended cleft-adapted bottle feeding, typical bottle feeding, spoon feeding, or syringe/squeeze bottle feeding. Infants could use a suction-based system at an average of 20 days post-operatively and return to an age-appropriate diet at an average of 15 days post-operatively.
The present study reports that while 88% of feeding providers recommend returning to bottle feeding immediately after lip repair, bottle feeding after palate repair is less common (55%). Substantial evidence exists to support returning immediately to bottle feeds after lip and palate repairs3–11. Spoon feeding is a skill for which children have no prior knowledge when done at lip repair. Similarly, open cup feeding may not have been introduced to the infant unless discussed with the parents well before surgery. There appears to be consensus that immediate bottle feeding does not interfere with lip healing, but there still may be concern for fistula formation after palate repair. Research is also needed to examine weight gain and nutrition status post-operatively between infants on a liquid-only diet versus infants who are cleared to immediately return to purees or a soft-diet.
Other factors can play into the role of fistula formation outside of feeding modality and the use of post-operative arm restraints. Some authors have found an association between fistula formation and surgeon experience, with less experienced surgeons (such as medical residents) having a higher fistula rate than more senior surgeons18. Fistula formation may also be related to Veau type, width of the cleft palate18 and surgical technique.. It has also been documented that infants with reduced weight at the time of palatoplasty are at higher risk for fistula formation19. Despite evidence that bottle feeding does not cause fistula formation, results from this survey demonstrate many teams are still opting to implement restrictive post-operative feeding protocols. This discrepancy between the literature and practice may be due to members of cleft teams relying on clinical expertise rather than research when making decisions and forming protocols20. In light of existing literature showing no connection between bottle feeding and fistula rate3, 10–11, further research is needed to determine (a) which factors drive these post-operative feeding recommendations, (b) if there is a difference between using a bottle that requires suction versus only compression, and (c) how surgical integrity can be maintained with less restrictive protocols. It may be challenging for teams to update their protocols as new evidence emerges if their current incidence of fistulae is low.
Evidence is also lacking for the utility of arm restraints after both lip and palate repair. However, 86% of respondents stated they use mittens or arm restraints after lip repair, and 83% reported using arm restraints or mittens after palate repair. Swaddle blankets, such as the CozeeCoo, are also being utilized to restrict arm movement. When considering the whole child, putting hands to mouth is a developmentally appropriate milestone, with infants opening their hands at 3 months, putting objects to mouth at 4 months, and beginning to self-feed at 6 months of age21. Use of arm restraints can often coincide with the timeline these developmental milestones.
This study does not exist without its limitations. As expert feeding providers were targeted in this survey, the majority of respondents were speech-language pathologists and nurses who provide feeding services on cleft teams. One limitation is that respondents did not include all providers involved in the immediate post-operative period, such as surgeons who perform cleft repairs. While speech-language pathologists and nurses may not be determining the post-operative guidelines, they are often the disciplines providing the post-operative education to families. Future research should aim to investigate post-operative restrictions from an interdisciplinary perspective with all related disciplines involved. Another limitation of this work is the inclusion of only providers in North America. Information on cleft team size and geographic locations outside of North America may be beneficial to consider in future research.
CONCLUSIONS
There continues to be a consistent use of post-operative restrictions across cleft teams following lip and palate repairs for infants with cleft palate. A majority of infants are returning to bottle feeding immediately after lip repair. More variation was found related to post-operative feeding guidelines following palate repair. Only approximately half of infants are cleared to immediately return to bottle feeding after palate repair, and the time between palate repair and clearance to use suction and return to an age-appropriate diet also varied widely. Further evidence is needed to determine which factors drive post-operative recommendations and find the least restrictive protocol needed to maintain surgical integrity.
ACKNOWLEDGEMENTS
Research reported in this publication was supported by the National Institute of General Medical Sciences under award number P20GM103432. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health. We have no additional conflicts of interest to disclose. This study was approved by the University of Wyoming Institutional Review Board. The participants have given informed consent to this work. Authors have read the Helsinki Declaration and have followed the guidelines in this investigation. We would like to thank Dr. Mary Hardin-Jones for her contributions to this study, Dr. Bistra Anatchkova (Wyoming Survey and Analysis Center) for reviewing this survey prior to dissemination, and Dr. Nicole Kurnik for reviewing this manuscript prior to submission.
REFERENCES
- 1.Pujol G, Riera March A. Cleft Lip Repair. In: StatPearls. Treasure Island (FL): StatPearls Publishing; October 31, 2022. [PubMed] [Google Scholar]
- 2.Parameters for Evaluation and Treatment of Patients with Cleft Lip/Palate or Other Craniofacial Differences. American Cleft Palate-Craniofacial Association; 2018. [DOI] [PubMed] [Google Scholar]
- 3.Cohen M, Marschall MA, Schafer EM. Immediate unrestricted feeding of infants following cleft lip and palate repair. The Journal of Craniofacial Surgery. 1992;3(1):30–32. [DOI] [PubMed] [Google Scholar]
- 4.Darzi MA, Chowdri NA, Bhat AN. Beast feeding or spoon feeding after cleft lip repair: A prospective randomized study. Br J Plast Surg. 1996;49(1):24–26 [DOI] [PubMed] [Google Scholar]
- 5.Dhaiban M, Younas S, Channa JA, Akhtar N. Is restricted breast and bottle-feeding necessary following cleft lip repair? Pediatric Child Health. 2014;19(6):e77. [Google Scholar]
- 6.Ranzer M, Daniele E, Purnell CA. Perioperative management of cleft lip repair: A meta-analysis and clinical practice guideline. Cleft Palate-Craniofacial Journal. 2021;58(10):1217–1225. [DOI] [PubMed] [Google Scholar]
- 7.Skinner J, Arvedson JC, Jones G, Spinner C, Rockwood J. Post-operative feeding strategies for infants with cleft lip. Int J Pediatr Otorhinolaryngol. 1997;42(2):169–178. [DOI] [PubMed] [Google Scholar]
- 8.Weatherley-White RC, Kuehn DP, Mirett P, Gilman JI, Weatherley-White CC. Early repair and breast-feeding for infants with cleft lip. Plast Reconstr Surg. 1987;79(6):879–887. [DOI] [PubMed] [Google Scholar]
- 9.Assuncao AGA, Farha MA, Peres SPBA, TRistao, MRC. Immediate postoperative evaluation of the surgical wound and nutritional evolution after cheiloplasty. Cleft Palate-Craniofacial Journal. 2005;42(4):434–438. [DOI] [PubMed] [Google Scholar]
- 10.Jigjinni V, Kangesu T, Sommerlad BC. Do babies require arm splints after cleft palate repair? Br J Plast Surg. 1993;46(8):681–685. [DOI] [PubMed] [Google Scholar]
- 11.Kim EK, Lee EJ, Chae SW. Effect of unrestricted bottle-feeding on early postoperative course after cleft palate repair. J Cranio Surg. 2009; 20(8);1886–1888. [DOI] [PubMed] [Google Scholar]
- 12.Katzel EB, Basile P, Koltz PF, Marcus JR, Girotto JA. Current surgical practices in cleft care: Cleft palate repair techniques and postoperative care. Plastic and Reconstructive Surgery. 2009;124(3):899–906. [DOI] [PubMed] [Google Scholar]
- 13.Tokioka K, Park S, Sugawara Y, Nakatsuka T. Video recording study of infants undergoing primary cheiloplasty: Are arm restraints really needed? Cleft Palate Craniofac J. 2009;46(6):636–641. [DOI] [PubMed] [Google Scholar]
- 14.O’Riain S Cleft lip surgery without postoperative restraints. Br J Plast Surg. 1977;30(2):140–141. [DOI] [PubMed] [Google Scholar]
- 15.Huth J, Petersen JD, Lehman JA. The use of postoperative restraints in children after cleft lip or cleft palate repair: A preliminary report. ISRN Plastic Surgery. 2013. [Google Scholar]
- 16.Michelotti B, Ross LE, Leber D, Samson T, MacKay D. Should surgeons use arm restraints after cleft surgery? Annals of plastic surgery. 2012;69(4):387–388. [DOI] [PubMed] [Google Scholar]
- 17.Kotlarek K, Zarzycka A, Bush E. A qualitative study of current practice and training trends for feeding services in infants with cleft palate. Cleft Palate Craniofac J. 2022;59(4S):56. [Google Scholar]
- 18.Yong L, Bing S, Qian Z, Qinggang H, Zhiyong W. Incidence of palatal fistula after palatoplasty with levator veli palatini retropositioning according to Sommerlad. British J Oral and Maxillofacial Surg. 2010; 48: 6370640. [DOI] [PubMed] [Google Scholar]
- 19.Al-Nawas B, Wriedt S, Reinhard J, Keilmann A, Wehrbein H, Wagern W. Influence of patient age and experience of the surgeon on early complications after surgical closure of the cleft palate-A retrospective cohort study. J Cranio-Maxillo-Facial Surg. 2013; 41:135–139. [DOI] [PubMed] [Google Scholar]
- 20.Kotlarek KJ, Benson M, Williams JL. Current practice patterns and training pathways for feeding infants with cleft palate. Cleft Palate-Craniofacial Journal. 2023. January 23:1–9. doi: 10.1177/10556656231152358 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 21.Hall M Early recognition of developmental delays. The J for Nurse Practitioners. 2009;5(9):690–691. [Google Scholar]


