Abstract
Despite evidence that pre-exposure prophylaxis (PrEP) reduces HIV risk, initiation and adherence remain low among vulnerable communities. Motivational interviewing (MI) can improve HIV prevention behaviors. However, limited research identifies how MI impacts PrEP uptake and adherence. This scoping review examines essential components of MI-based interventions that aimed to improve PrEP use, including the number and duration of sessions, counselor characteristics, and interview content. We searched four databases, PubMed, CINAHL Plus, Embase, and Web of Science, and reviewed 379 articles. Studies were considered if they (a) were published between 2012 and 2023, (b) used MI independently or part of a multi-component intervention strategy, and (c) focused on improving PrEP initiation or adherence. Seven articles met inclusion criteria. Regarding intervention components, the number of MI sessions varied and duration ranged between 15 and 60 min. MI counselors varied in credentialing and demographic characteristics. MI content included PrEP education, identifying initiation and adherence barriers, and strategizing ways to overcome barriers. MI is an important component of interventions that aim to improve PrEP initiation and adherence. However, the variability and limited details across studies hinder our ability to assess MI efficacy on PrEP initiation and adherence or replicate these approaches in future interventions.
Keywords: Prevention, Brief intervention, Men who have sex with men, Women, Sexual health
Introduction
Increased HIV pre-exposure prophylaxis (PrEP) initiation and adherence can help end the epidemic because it substantially reduces acquisition risk among vulnerable individuals (Anderson et al., 2012; Fauci et al., 2019; Mayer et al., 2020; Centers for Disease Control and Prevention [CDC], 2021). Specifically, PrEP adherence can reduce HIV acquisition risk by 99% when taken as prescribed (CDC, 2021). However, PrEP use remains suboptimal among individuals at greatest risk for HIV due to multi-level factors such as limited healthcare access, medication stigma, discomfort discussing sexual risk behaviors with clinicians, and low perceived HIV risk (Cahill et al., 2017; D’Angelo et al., 2020; Felsher et al., 2018). Disparities in PrEP uptake based on age, race, gender, and sexual orientation also exist (Kanny et al., 2019). Scalable and cost-effective interventions such as motivational interviewing (MI) (Bonacci & Holtgrave, 2017; Kelly, 2019) could circumvent barriers, reduce disparities, and improve PrEP initiation and adherence.
MI is a collaborative communication approach in which a counselor partners with clients to activate their motivations and resources to change unhealthy behaviors (Miller & Rollnick, 2012; Rollnick & Miller, 1995; Rollnick et al., 2010). MI facilitates progress through the transtheoretical model of change (Prochaska & DiClemente, 1982) and consists of the following core concepts: (1) engaging clients in collaboration with the counselor, (2) focusing on client goals, (3) evoking client motivations and barriers to behavior change, and (4) planning next steps toward the desired behavior(s) (Levensky et al., 2007; Miller & Rollnick, 2012). MI typically consists of one or two sessions ranging between 10 and 120 min (Hettema et al., 2005; Rubak et al., 2005) and can be conducted in a variety of settings such as clinics, community-based organizations, and via telephone (Hettema et al., 2005; Kahler et al., 2020; VanBuskirk & Wetherell, 2014). MI counselors can be trained paraprofessionals or clinicians who use open-ended interviewing and reflective listening to identify client ambivalence and barriers to behavior change (Naar-King et al., 2009; Palacio et al., 2016; Rollnick & Miller, 1995). MI approaches are often used in health promotion because of their cost-effectiveness, session brevity, adaptability, and use of client interests for behavior change. MI began with addiction counseling and has been applied as an intervention strategy globally to support effective behavior change for many health behaviors (Rubak et al., 2005), including dieting (Stallings & Schneider, 2018), exercise (Barnes & Cassidy, 2018), violence prevention (Soleymani et al., 2018), and medication adherence for chronic conditions (Ekong & Kavookjian, 2016).
MI can also be used to promote HIV prevention behaviors such as condom use, HIV testing, and PrEP use. Some biobehavioral HIV prevention interventions utilize “MI-consistent” or “MI-based” interviews because of its benefits (Carcone et al., 2022; MacDonell et al., 2022; Moitra et al., 2020). These interventions are useful to reduce barriers such as stigma and perceived HIV risk and could be effective at improving initiation and adherence. Research in other prevention domains has examined the influence of MI counselors’ personal characteristics, professional credentialing, and/or training on intervention efficacy (Gaume et al., 2009, 2014, 2016), highlighting the need for this inquiry among HIV prevention interventions. However, limited information is available regarding the specific components of MI-based interventions that aid in improving PrEP initiation and adherence. Few studies have clarified the credentials of interventionists, the intervention setting, discussion length, client goals, and conversation content in PrEP initiation and adherence interventions. Therefore, HIV prevention scientists’ understanding of how MI impacts PrEP use is limited. Additionally, optimizing and potentially standardizing MI-based interventions to improve PrEP initiation and adherence among individuals at greatest risk for HIV acquisition is challenging without details of effective key components.
The purpose of this scoping review is to examine the use of MI interventions that aimed to increase PrEP initiation and adherence and identify their components. Identifying the components of MI-based interventions (i.e., the counselor, setting, session duration, and content) is necessary to clarify the meaning of “MI-consistent” or “MI-based” approaches for implementing research protocols systematically. Inferences regarding the effects of MI-based interventions in PrEP interventions are difficult to make because details of MI components in the strategy are lacking. Replicating these PrEP promotion strategies is also difficult because details of their MI components are typically missing. Moreover, a better understanding of intervention components in PrEP interventions is needed to identify how contemporary strategies differ or deviate from original MI frameworks. Identifying components of MI-based protocols, including the counselor, number and duration of sessions, and content, is needed to establish a consistent MI-based approach among PrEP interventions and better evaluate the impact of MI on PrEP initiation and adherence. Findings will allow HIV prevention scientists (and clinicians) to implement more effective, reliable, and scalable interventions to increase PrEP initiation and adherence among vulnerable communities.
Methods
Search Strategy
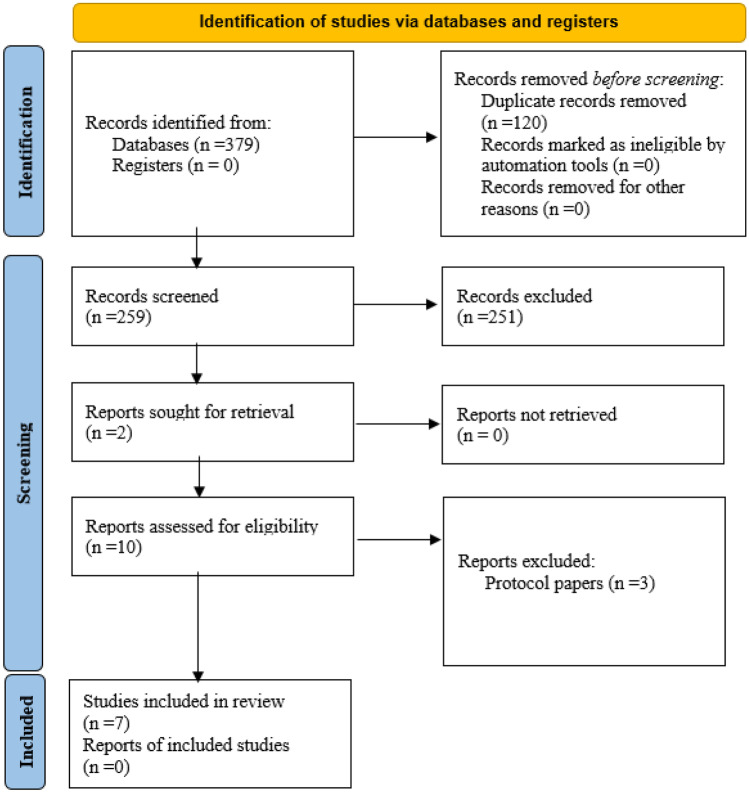
A targeted literature search guided by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist (Fig. 1) (Moher et al., 2009) was conducted between October 2020 and March 2023. To identify a range of relevant epidemiological, public health, and social science literature, we searched four databases: PubMed, Cumulative Index for Nursing and Allied Health Literature Plus, PsycINFO, and Embase. The literature search was conducted using the following search terms across all databases: “Human Immunodeficiency Virus OR HIV,” “HIV prevention,” “Pre-exposure Prophylaxis OR PrEP,” “Emtricitabine-Tenofovir Disoproxil Fumarate Drug Combination OR Truvada,” “Motivational Interviewing OR MI,” “Brief Intervention,” and “Descovy OR Emtricitabine/tenofovir alafenamide.”
Fig. 1.
PRISMA flow diagram (Page et al., 2021)
Study Selection
Studies were considered for inclusion if they (1) were published between 2012 and 2023, (2) used MI as an independent intervention, or (3) used MI as part of a multi-component strategy to improve PrEP initiation or adherence. Studies among all populations and in global settings were considered in order to identify and review the full scope of MI-related interventions among diverse groups in different cultural and geographic contexts. Dissertations, books, editorials, letters, and commentaries were excluded.
This strategy yielded a total of 379 studies after duplicates were removed. After initial review of titles and abstracts, ten full-text articles were assessed for inclusion, seven of which are included in this review. Three articles were excluded because they described intervention protocols without providing details regarding intervention effects on study outcomes (Fig. 1) (Page et al., 2021).
Data abstracted from the seven studies include the study sample, study design, MI setting, motivational interviewer, duration of sessions, theoretical framework, and MI content (Table 1). We used the Johns Hopkins Evidence-Based Practice Quality Guide (Dang & Dearholt, 2018) to identify the level of evidence and appraise the quality of the included studies in Table 2.
Table 1.
Characteristics of studies using motivational interviewing to increase PrEP initiation and/or adherence
| First author (year) | Sample | Study design | Theoretical framework | MI setting | Interviewer |
MI session Duration |
MI content | Intervention effect |
|---|---|---|---|---|---|---|---|---|
| Chan et al. (2021) | 86 SMM | RCT | MI theory |
STI clinic and telephone USA |
State-certified STI clinic counselors |
2 sessions 15–20 min |
Session 1: Build rapport, PrEP education, discuss HIV risk behaviors, identify and address barriers, PrEP pros and cons Session 2: Reinforce Session 1 and construct an action plan |
Yes |
| Dale (2020) | 10 Black women | Open pilot trial | Information, motivation, and behavioral skills model |
Unspecified clinical setting Miami, FL, USA |
Black female clinician | 2 sessions plus 1-month follow-up |
Session 1: PrEP information, enhancing motivation, work through ambivalence Session 2: Session 1 content plus questions regarding PrEP and potential access since Session 1 |
No |
| Mayer et al. (2017) | 50 SMM adults | RCT | Cognitive Behavior Theory |
Primary care clinic Boston, MA, USA |
Nurse counselors | 4 sessions plus 2 booster sessions (50 min) |
Session 1: PrEP education, MI exercise, exploring adherence schedule Session 2: Adherence check-in, PrEP experience, problem solving Session 3: Adherence check-in, identifying sexual risk behaviors, health behavior/HIV transmission education Session 4: PrEP adherence goals and plans for PrEP maintenance Booster sessions: PrEP adherence |
Yes |
| Moitra et al. (2020) | 19 SMM adults | Uncontrolled pilot trial MI intervention | Self-regulation theory | Publicly funded STD clinic Rhode Island, USA | Unspecified |
2 sessions 15–25 min |
Unspecified | No |
| Morris et al. (2022) | 255 transgender and non-binary adults | RCT | Theory of planned behavior | Telephone sessions, Southern California, USA | Research coordinators | Median 0–7 sessions, unspecified duration | Barriers and facilitators to adherence and adherence techniques | No |
| Psaros et al. (2014) | 168 HIV-negative men & women in serodiscordant relationships | Placebo-controlled efficacy trial | Cognitive behavioral theory | Clinical research sites Uganda | Lay counselors |
Varied, median 10 min (IQR 5, 16) 40 min (IQR 25, 30) |
Reviewing pros and cons of achieving high levels of PrEP adherence. Resolving ambivalence about adherence, moving participants to a higher level of readiness to adhere | Yes |
| Teixeira da Silva et al. (2021) | 136 Black SMM and transwomen | RCT | Information, motivation, behavioral skills model | Unspecific research site Chicago, USA | Social work interventionist | 60 min, 4 booster sessions | HIV and PrEP information, motivation to reduce HIV risk and engage in PrEP care, HIV risk reduction strategies, planning to enact change | Yes |
RCT randomized controlled trial, SMM sexual minority men, IQR interquartile range
Table 2.
Summary of level and quality of evidence
| First author (year) | Observable measures | Intervention effects | Study limitations | Level & quality of evidence |
|---|---|---|---|---|
| Chan et al. (2021) |
Scheduling a PrEP appointment with a clinician Attending clinical appointment Accepting PrEP prescription via self-report |
52.3% clinical appointment attendance and PrEP prescription for intervention group vs 27.9% in control group |
Small sample of mostly white and educated SMM Self-reported PrEP prescription acceptance |
Level I Grade B Good quality |
| Dale (2020) |
PrEP use motivation and readiness PrEP knowledge PrEP uptake via self-report PrEP adherence via self-report |
30% PrEP uptake |
Small sample size MI counselor credentials unavailable Conclusions regarding intervention impact on PrEP initiation/adherence cannot be drawn |
Level III Grade C Low quality |
| Mayer et al. (2017) |
PrEP adherence at 6 months via Wisepill Tenofovir plasma levels Sexual risk behaviors |
PrEP adherence high in both study groups, not statistically different |
Small sample of mostly high risk, white, educated SMM Conclusions regarding intervention impact on PrEP adherence cannot be determined |
Level I Grade B Good quality |
| Moitra et al. (2020) |
PrEP awareness and use Intervention acceptability |
High intervention acceptability 37% PrEP prescription after intervention |
Small sample size Information regarding intervention content not available Conclusions regarding intervention impact on PrEP adherence cannot be determined |
Level III Grade C Low quality |
| Morris et al. (2022) |
PrEP adherence via dried blood spot concentrations ≥ 1246 fmol/punch Self-reported adherence |
No statistically significant difference between the intervention and control arms (34.7% vs 38.3%; P = 0.60) or for the dried blood spot concentrations |
Details regarding the MI content not available Details regarding MI counselors limited Conclusions regarding how intervention impacted PrEP adherence cannot be determined |
Level I Grade B Good quality |
| Psaros et al. (2014) | PrEP adherence via pill count and micro-electromechanical system |
8% mean increase in PrEP adherence post-intervention ≥ 80% PrEP adherence after first session |
MI only used in the first session of intervention Large number and range of sessions Second session was couples-based Participants received different number of sessions |
Level I Grade B Good quality |
| Teixeira da Silva et al. (2021) | linkage to PrEP care where PrEP was discussed with a clinician (regardless of initiation) |
Greater proportion of intervention participants were linked to PrEP care within the linkage window (24% vs. 11%; p = 0.04) A significantly greater proportion of intervention participants initiated PrEP at 3-month follow-up (11% vs 25%; p = 0.05) |
Small sample of transwomen limits ability to specify intervention effects |
Level 1 Grade B Good quality |
Results
Study Population and Sample
Six of the seven studies were conducted in the USA; one study was conducted in Uganda. Four studies investigated MI with sexual minority men (SMM) (Chan et al., 2021; Mayer et al., 2017; Moitra et al., 2020; Teixeira da Silva et al., 2021). Four of the studies included non-SMM individuals, specifically U.S. Black women (Dale, 2020), transgender adults (Morris et al., 2022; Teixeira da Silva et al., 2021), and Ugandan men and women in serodiscordant relationships (Psaros et al., 2014). The sample size of these studies ranged from 10 to 255 (Table 1).
Theoretical Frameworks
All studies utilized theoretical frameworks that guided the intervention (MI approach). Specifically, two studies were guided by cognitive behavior theory (Mayer et al., 2017; Psaros et al., 2014), two were guided by the Information, Motivation, and Behavioral skills (IMB) model (Dale, 2020; Teixeira da Silva et al., 2021), one was guided by the Theory of Planned Behavior (Morris et al., 2022), and one was guided by Self-Regulation Theory, a framework for understanding motivation and goal attainment (Moitra et al., 2020). Chan et al. (2021) reported using unspecified “MI theory” in an intervention among SMM.
MI Intervention Setting
Six of the studies reported that their interventions were implemented in clinical settings, including sexually transmitted infection (STI) clinics (Chan et al., 2021; Moitra et al., 2020), primary care setting (Mayer et al., 2017), and unspecified clinical research sites (Dale, 2020; Psaros et al., 2014; Teixeira da Silva et al., 2021). One study included telephone-based MI sessions (Morris et al., 2022). Although most studies reported that the MI sessions were conducted in a traditional face-to-face format, three studies reported using telephone and/or video-based communication technology to deliver the intervention in a digital format (Chan et al., 2021; Morris et al., 2022; Teixeira da Silva et al., 2021).
Motivational Interviewers
Three studies reported that clinicians conducted MI (Chan et al., 2021; Dale, 2020; Mayer et al., 2017). In two of these studies, state-certified STI clinic counselors and nurse counselors served as motivational interviewers (Chan et al., 2021; Mayer et al., 2017). One study reported having a culturally congruent clinician who led MI sessions (Dale, 2020), while “lay counselors” (Psaros et al., 2014) and “research coordinators” (Morris et al., 2022) conducted MI-based sessions in two studies. One study utilized social workers as interventionists (Teixeira da Silva et al., 2021). Moitra et al. (2020) provided no details regarding the credentials, training, or demographic characteristics of the motivational interviewer.
Duration of Motivational Interview
Three studies reported conducting two MI-based sessions (Chan et al., 2021; Dale, 2020; Moitra et al., 2020), and two reported offering four sessions (Mayer et al., 2017; Teixeira da Silva et al., 2021). Two reported using an individualized approach with a median of 7–10 MI sessions per participant (Morris et al., 2022; Psaros et al., 2014). The duration of MI-based sessions ranged from 15 to 60 min across the studies. In Moitra’s study, the duration of the first MI session ranged from 15 to 25 min, and the median duration of the second session was 5 min (Moitra et al., 2020). Chan et al. (2021) reported 15–20-min sessions, and Mayer et al. reported their MI sessions lasting 50 min (2017). In the Psaros et al. (2014) study, the duration of MI was customized to the individual’s needs, with a median duration of 40 min (IQR 30,50) for the first session and median duration of 20 min (IQR 15, 30) by session 4. There were no reports of MI durations in two of the studies (Dale, 2020; Morris et al., 2022).
Motivational Interview Content
Most studies reported that the first MI-based session included a combination of providing PrEP education and identifying and alleviating barriers to PrEP use (Chan et al., 2021; Dale, 2020; Mayer et al., 2017; Morris et al., 2022; Psaros et al., 2014; Teixeira da Silva et al., 2021). Chan and colleagues (2021) explicitly mentioned building rapport with participants in the first session. Both the Dale (2020) and Moitra et al. (2020) studies reported 2 sessions, and the second visit reinforced the content presented in the first visit. However, unlike these two studies, Chan et al. (2021) used the second session to develop a PrEP action plan with participants. In one study that utilized 4 MI sessions (Mayer et al., 2017), the authors described how sessions built upon one another and focused on adherence checks, problem solving, risk assessments, and plans for PrEP maintenance. Moitra’s study did not provide any specifications on the MI content in the intervention (Moitra et al., 2020).
Intervention Effects
One study reported a statistically significant doubling in PrEP appointment attendance for those in the MI-based experimental arm (52.3%) compared to the control group (27.9%) (Chan et al., 2021). Four studies reported a pattern toward improvement in PrEP initiation and/or adherence, but the improvement was not statistically significant (Dale, 2020; Mayer et al., 2017; Moitra et al., 2020; Morris et al., 2022). Analysis of 3-month survey data in one study showed that a significantly greater proportion of participants who received the MI-based intervention initiated PrEP than control group participants (Teixeira da Silva et al., 2021).
Quality of Evidence
Despite the potential for rigor among the randomized/placebo-controlled trials (Chan et al., 2021; Mayer et al., 2017; Morris et al., 2022; Psaros et al., 2014; Teixeira da Silva et al., 2021), these studies were given “good” quality ratings (Dang & Dearholt, 2018). The randomized trials contained small sample sizes and limited or no information regarding the reliability of measurements, which reduced their ability to identify strong effects and generalizable results. However, they did contain some control with appropriate conclusions and reasonably consistent recommendations given their evidence. The quasi-experimental study by Moitra et al. (2020) was also given a “good” quality rating for similar reasons. The quasi-experimental study conducted by Dale (2020) was rated “low” quality due to a small sample size and reliance on qualitative findings to substantiate claims regarding intervention effects.
Discussion
This scoping review examined the use and components of MI in interventions aimed at improving PrEP initiation and adherence. Intervention components regarding the duration of MI sessions, MI counselor, and MI content differed across studies. Results from the studies’ small sample sizes and average quality provided inconclusive evidence regarding the relative effects of MI interventions on PrEP initiation and adherence. We were also unable to isolate the effect of MI from other components in the multi-component interventions. Complete details regarding MI components were not provided for all studies. Studies contained important similarities and differences to each other and to traditional MI approaches that require examination and discussion among prevention scientists who develop PrEP interventions and the clinicians and paraprofessionals who implement them.
Effective health promotion interventions are often guided by theories and/or conceptual frameworks whose interrelated concepts explain human behavior (Fishbein & Yzer, 2003; Glanz & Bishop, 2010). All interventions were guided by theoretical frameworks (e.g., social cognitive theory, IMB model), but most lacked clarity regarding how those frameworks guided their MI approach. Considering that MI was originally a standalone communication approach that leveraged client goals as the core intervention for behavior change (Hettema et al., 2005; Rollnick & Miller, 1995), contemporary interventions should explain how MI approaches meld with chosen theoretical constructs to achieve desired health outcomes (in this case PrEP initiation and/or adherence). Since the reviewed studies included multi-component interventions, it is unclear how MI fits into their theoretical frameworks and if the multi-component intervention model still adheres to the “spirit” of MI (Miller & Rollnick, 2012). For example, identifying and resolving ambivalence is key to MI (Miller & Rollnick, 2012; Rollnick & Miller, 1995). However, it is unclear how key constructs of the theoretical approaches used in these studies (e.g., self-efficacy or self-control) support or reinforce behavior change catalyzed by the MI approach in the studies. Additionally, studies in this review lacked key information regarding participants’ goals, their relative initial interests in PrEP initiation and/or adherence, and how theory informed the MI approaches used in session interviews.
Although using a range of trained professionals to conduct MI could be beneficial in clinical and community-based settings in which licensed clinicians are limited, the lack of information about counselors’ demographic characteristics or professional credentialing lessens our ability to make claims regarding interviewer impact on intervention outcomes. Some research suggests that cultural congruence, familiarity, patient-centered communication, and personal disclosures from clinicians improve adherence to clinical recommendations among subpopulations with elevated HIV risk, such as Black SMM (Dangerfield et al., 2021a, b; White et al., 2019). Therefore, we hypothesize that having MI counselors with clinical credentials, standard training in the MI approach, and in-group identity markers with potential PrEP clients (e.g., race/ethnicity, gender, and/or sexual or gender identity) could result in better engagement and collaboration, thereby strengthening the effects of MI on behavior change. Since PrEP initiation and adherence are partly impacted by medical mistrust and low perceived HIV risk (Biello et al., 2018; Gallagher et al., 2014), a trained, culturally congruent counselor with personal PrEP use experience could bridge the gap between participants (Dangerfield et al., 2021a). However, the inconsistency of demographic characteristics among the counselors identified in this review limits inferences on PrEP use effects.
Although MI sessions are generally described as brief and a number of sessions vary in health promotion interventions (Hettema et al., 2005; Palacio et al., 2016; Rubak et al., 2005), it is unclear how the range of sessions impacts intervention effects on PrEP initiation and/or adherence among the studies in this review. Potentially, the duration and number of sessions could be key to the relative impact of MI on PrEP use and to standardize this approach in clinical or community-based settings where resources are limited and patient engagement is often challenging (Emmons & Rollnick, 2001). In addition, interventions that effectively increase PrEP initiation and adherence in the shortest amount of time would reduce HIV risk among patients in a timelier manner.
There are limitations to this scoping review. The scope of the review was restricted to peer-reviewed articles printed in English and did not consider studies in other languages. Additionally, this scoping review did not measure the strength of associations between the interventions on PrEP initiation and adherence. Implications for specific populations cannot be drawn. Studies also did not discuss effects on contemporary PrEP modalities such as “on-demand PrEP” and the cabotegravir injectable, both of which could impact willingness, initiation, and adherence (Beymer et al., 2019; Meyers et al., 2018; Molina et al., 2017). Findings from this review will provide a foundation for future research on this important topic, such as conducting meta-analyses.
It was difficult to assess how the MI approaches were designed or how adherent they were to the “spirit of MI” (Miller & Rollnick, 2012) for several interventions. Since contemporary HIV prevention interventions have the ultimate goal of improving PrEP initiation and adherence among vulnerable individuals, the question posed in this scoping review is: are prevention scientists conducting MI or should “MI-consistent” interventions be reclassified as “MI-plus” or something else? Rollnick and Miller (1995, 2009) suggest that MI will not work well if dispatched as a cookbook approach or set of techniques applied to clients as opposed to with them, which may explain the variation in MI effects because PrEP interventions have an intrinsic goal to encourage initiation and/or adherence. Implementing an intervention to help individuals change unhealthy to healthy behaviors is different than encouraging people to use prophylactic medication for an absent condition because medication non-use may not necessarily be an “unhealthy behavior.” Additionally, encouraging specific behavior change in interventions with desired outcomes in mind (i.e., PrEP initiation and adherence) could deviate from the core element of focusing on client goals and desired behaviors, which could include other HIV prevention behaviors without using PrEP. Therefore, the premise of PrEP interventions that include MI components inherently differs from the “spirit of MI” (Miller & Rollnick, 2009) and should be reconsidered in prevention science.
Based upon the findings of this review, studies that include MI should provide details regarding their intervention components. Specifically, studies should detail (1) the theoretical framework guiding MI-based content and conversations; (2) demographic characteristics and professional qualifications of MI counselors; (3) MI counselor selection process; and (4) justification for location, number, and duration of MI sessions. These guidelines could improve researchers’ ability to standardize MI-based intervention approaches to potentially obtain stronger intervention effects and bring the strategies to scale. Developing a manual for an evidence-based MI intervention is feasible and can facilitate desired behavior change (Hurlocker et al., 2021), furthering the notion that at least some standardization in the MI approach is necessary for PrEP initiation and/or adherence interventions.
Conclusions
We found variability across studies in this review that makes it difficult to draw inferences about MI implementation in PrEP interventions. In the absence of detailed explanations of the components of MI in PrEP interventions, we are limited in our ability to assess the technique on PrEP outcomes. Substantial limitations regarding small sample sizes, self-reported outcomes, and inconclusive findings hinder our ability to establish standard protocols for MI implementation in PrEP interventions. No study earned an exemplar quality rating. Therefore, none of the studies in this scoping review can serve as a model for how MI can be used effectively in PrEP interventions. Consistent approaches are needed to identify the relative impact of MI on PrEP initiation and adherence to potentially standardize this approach in clinical and community-based settings. Future research should continue to identify the relative impact of MI approaches on PrEP initiation and adherence.
Funding
This research was supported in part by a National Institute of Mental Health Grant (no. K01MH11849 to PI DTD II). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Declarations
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Anderson, P. L., Glidden, D. V., Liu, A., Buchbinder, S., Lama, J. R., Guanira, J. V., McMahan, V., Bushman, L. R., Casapía, M., Montoya-Herrera, O., Veloso, V. G., Mayer, K. H., Chariyalertsak, S., Schechter, M., Bekker, L.-G., Kallás, E. G., Grant, R. M., & Team, F. the iPrEx S. (2012). Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Science Translational Medicine, 4(151), 151ra125–151ra125. 10.1126/scitranslmed.3004006 [DOI] [PMC free article] [PubMed]
- Barnes, M. S., & Cassidy, T. (2018). Diet, exercise and motivation in weight reduction: The role of psychological capital and stress: Diet, exercise and motivation in weight reduction. JOJ Nurse Health Care, 9(5), 1–6. 10.19080/JOJNHC.2018.09.555775
- Beymer MR, Holloway IW, Pulsipher C, Landovitz RJ. Current and future PrEP medications and modalities: On-demand, injectables, and topicals. Current HIV/AIDS Reports. 2019;16(4):349–358. doi: 10.1007/s11904-019-00450-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biello KB, Edeza A, Montgomery MC, Almonte A, Chan PA. Risk perception and interest in HIV pre-exposure prophylaxis among men who have sex with men with rectal gonorrhea and chlamydia infection. Archives of Sexual Behavior. 2018 doi: 10.1007/s10508-018-1260-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonacci, R. A., & Holtgrave, D. R. (2017). U.S. HIV incidence and transmission goals, 2020 and 2025. American Journal of Preventive Medicine, 53(3), 275–281. 10.1016/j.amepre.2017.03.012 [DOI] [PubMed]
- Cahill S, Taylor SW, Elsesser SA, Mena L, Hickson D, Mayer KH. Stigma, medical mistrust, and perceived racism may affect PrEP awareness and uptake in black compared to white gay and bisexual men in Jackson, Mississippi and Boston. Massachusetts. AIDS Care. 2017;29(11):1351–1358. doi: 10.1080/09540121.2017.1300633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carcone AI, Coyle K, Butame S, Harper GW, Aarons GA, Naar S. Using the Exploration-Preparation-Implementation-Sustainment (EPIS) Framework to prepare for the implementation of evidence-based practices into adolescent HIV settings. AIDS and Behavior. 2022;26(12):4093–4106. doi: 10.1007/s10461-022-03735-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan, P. A., Nunn, A., Van Den Berg, J. J., Cormier, K., Sowemimo-Coker, G., Napoleon, S. C., Arnold, T., & Moitra, E. (2021). A randomized trial of a brief behavioral intervention for PrEP uptake among men who have sex with men at increased risk for HIV infection. JAIDS Journal of Acquired Immune Deficiency Syndromes, Publish Ahead of Print. 10.1097/QAI.0000000000002671 [DOI] [PMC free article] [PubMed]
- D’Angelo AB, Lopez-Rios J, Flynn AWP, Holloway IW, Pantalone DW, Grov C. Insurance- and medical provider-related barriers and facilitators to staying on PrEP: Results from a qualitative study. Translational Behavioral Medicine. 2020 doi: 10.1093/tbm/ibz191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dale SK. Using motivational interviewing to increase PrEP uptake among Black women at risk for HIV: An open pilot trial of MI-PrEP. Journal of Racial and Ethnic Health Disparities. 2020;7(5):913–927. doi: 10.1007/s40615-020-00715-9. [DOI] [PubMed] [Google Scholar]
- Dang, D., & Dearholt, S. L. (2018). Johns Hopkins nursing evidence-based practice: Model & guidelines (3rd ed.). Sigma Theta Tau International.
- Dangerfield DT, II, Cooper J, Heidari O, Allen S, Winder TJA, Lucas GM. Nursing and health care preferences among opioid and stimulant using Black sexual minority men: An exploratory study. Journal of the Association of Nurses in AIDS Care. 2021;32(5):e30–e39. doi: 10.1097/JNC.0000000000000201. [DOI] [PubMed] [Google Scholar]
- Dangerfield II, D. T., Wylie, C., & Anderson, J. N. (2021b). Conducting virtual, synchronous focus groups among black sexual minority men: Qualitative study. JMIR Public Health and Surveillance, 7(2), e22980. 10.2196/22980 [DOI] [PMC free article] [PubMed]
- Ekong G, Kavookjian J. Motivational interviewing and outcomes in adults with type 2 diabetes: A systematic review. Patient Education and Counseling. 2016;99(6):944–952. doi: 10.1016/j.pec.2015.11.022. [DOI] [PubMed] [Google Scholar]
- Emmons KM, Rollnick S. Motivational interviewing in health care settings: Opportunities and limitations. American Journal of Preventive Medicine. 2001;20(1):68–74. doi: 10.1016/S0749-3797(00)00254-3. [DOI] [PubMed] [Google Scholar]
- Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV epidemic: A plan for the United States. JAMA. 2019;321(9):844. doi: 10.1001/jama.2019.1343. [DOI] [PubMed] [Google Scholar]
- Felsher M, Szep Z, Krakower D, Martinez-Donate A, Tran N, Roth AM. “I don’t need PrEP right now”: A qualitative exploration of the barriers to PrEP care engagement through the application of the health belief model. AIDS Education and Prevention. 2018;30(5):369–381. doi: 10.1521/aeap.2018.30.5.369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fishbein M, Yzer MC. Using theory to design effective health behavior interventions. Communication Theory. 2003;13(2):164–183. doi: 10.1111/j.1468-2885.2003.tb00287.x. [DOI] [Google Scholar]
- Gallagher T, Link L, Ramos M, Bottger E, Aberg J, Daskalakis D. Self-perception of HIV risk and candidacy for pre-exposure prophylaxis among men who have sex with men testing for HIV at commercial sex venues in New York City. LGBT Health. 2014;1(3):218–224. doi: 10.1089/lgbt.2013.0046. [DOI] [PubMed] [Google Scholar]
- Gaume J, Gmel G, Faouzi M, Daeppen J-B. Counselor skill influences outcomes of brief motivational interventions. Journal of Substance Abuse Treatment. 2009;37(2):151–159. doi: 10.1016/j.jsat.2008.12.001. [DOI] [PubMed] [Google Scholar]
- Gaume J, Longabaugh R, Magill M, Bertholet N, Gmel G, Daeppen J-B. Under what conditions? Therapist and client characteristics moderate the role of change talk in brief motivational intervention. Journal of Consulting and Clinical Psychology. 2016;84:211–220. doi: 10.1037/a0039918. [DOI] [PubMed] [Google Scholar]
- Gaume, J., Magill, M., Longabaugh, R., Bertholet, N., Gmel, G., & Daeppen, J.-B. (2014). Influence of counselor characteristics and behaviors on the efficacy of a brief motivational intervention for heavy drinking in young men—A randomized controlled trial. Alcohol: Clinical and Experimental Research, 38(7), 2138–2147. 10.1111/acer.12469 [DOI] [PubMed]
- Glanz K, Bishop DB. The role of behavioral science theory in development and implementation of public health interventions. Annual Review of Public Health. 2010;31(1):399–418. doi: 10.1146/annurev.publhealth.012809.103604. [DOI] [PubMed] [Google Scholar]
- Hettema J, Steele J, Miller WR. Motivational interviewing. Annual Review of Clinical Psychology. 2005;1(1):91–111. doi: 10.1146/annurev.clinpsy.1.102803.143833. [DOI] [PubMed] [Google Scholar]
- Hurlocker MC, Moyers TB, Houck J. Can a pure motivational interviewing intervention be manualized and still efficacious? A test of feasibility and initial efficacy. Psychotherapy. 2021;58(2):196–205. doi: 10.1037/pst0000309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahler, J., Heckman, T. G., Shen, Y., Huckans, M. S., Feldstein Ewing, S. W., Parsons, J. T., Phelps, A., Sutton, M., Holloway, J., & Lovejoy, T. I. (2020). Randomized controlled trial protocol for project BRIDGE: A telephone-administered motivational interviewing intervention targeting risky sexual behavior in older people living with HIV. Contemporary Clinical Trials, 95, 106047. 10.1016/j.cct.2020.106047 [DOI] [PMC free article] [PubMed]
- Kanny, D., Jeffries, W. L., Chapin-Bardales, J., Denning, P., Cha, S., Finlayson, T., Wejnert, C., Abrego, M., Al-Tayyib, A., Anderson, B., Barak, N., Beckford, J. M., Bolden, B., Brady, K. A., Brandt, M.-G., Brantley, M., Braunstein, S., Buyu, C., Cano, R., … Wortley, P. (2019). Racial/ethnic disparities in hiv preexposure prophylaxis among men who have sex with men—23 urban areas, 2017. Morbidity and Mortality Weekly Report, 68(37), 801–806. 10.15585/mmwr.mm6837a2 [DOI] [PMC free article] [PubMed]
- Kelly JA. Ten things we need to do to achieve the goals of the end the HIV epidemic plan for America. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2019;82:S94. doi: 10.1097/QAI.0000000000002166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levensky ER, Forcehimes A, O’Donohue WT, Beitz K. Motivational interviewing: An evidence-based approach to counseling helps patients follow treatment recommendations. AJN the American Journal of Nursing. 2007;107(10):50–58. doi: 10.1097/01.NAJ.0000292202.06571.24. [DOI] [PubMed] [Google Scholar]
- MacDonell, K. K., Wang, B., Phanuphak, N., Janamnuaysook, R., Srimanus, P., Rongkavilit, C., & Naar, S. (2022). Optimizing an mHealth intervention to improve uptake and adherence to HIV pre-exposure prophylaxis in young transgender women: Protocol for a multi-phase trial. JMIR Research Protocols, 11(5), e37659. 10.2196/37659 [DOI] [PMC free article] [PubMed]
- Mayer KH, Safren SA, Elsesser SA, Psaros C, Tinsley JP, Marzinke M, Clarke W, Hendrix C, Wade Taylor S, Haberer J, Mimiaga MJ. Optimizing pre-exposure antiretroviral prophylaxis adherence in men who have sex with men: Results of a pilot randomized controlled trial of “Life-Steps for PrEP”. AIDS and Behavior. 2017;21(5):1350–1360. doi: 10.1007/s10461-016-1606-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayer, K. H., Molina, J.-M., Thompson, M. A., Anderson, P. L., Mounzer, K. C., De Wet, J. J., DeJesus, E., Jessen, H., Grant, R. M., Ruane, P. J., Wong, P., Ebrahimi, R., Zhong, L., Mathias, A., Callebaut, C., Collins, S. E., Das, M., McCallister, S., Brainard, D. M., … Hare, C. B. (2020). Emtricitabine and tenofovir alafenamide vs emtricitabine and tenofovir disoproxil fumarate for HIV pre-exposure prophylaxis (DISCOVER): Primary results from a randomised, double-blind, multicentre, active-controlled, phase 3, non-inferiority trial. The Lancet, 396(10246), 239–254. 10.1016/S0140-6736(20)31065-5 [DOI] [PMC free article] [PubMed]
- Meyers, K., Wu, Y., Brill, A., Sandfort, T., & Golub, S. A. (2018). To switch or not to switch: Intentions to switch to injectable PrEP among gay and bisexual men with at least twelve months oral PrEP experience. PLOS ONE, 13(7), e0200296. 10.1371/journal.pone.0200296 [DOI] [PMC free article] [PubMed]
- Miller, W. R., & Rollnick, S. (2012). Motivational interviewing: Helping people change. Guilford Press.
- Miller WR, Rollnick S. Ten things that motivational interviewing is not. Behavioural and Cognitive Psychotherapy. 2009;37(2):129–140. doi: 10.1017/S1352465809005128. [DOI] [PubMed] [Google Scholar]
- Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA statement. Annals of Internal Medicine. 2009;151(4):264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Moitra E, van den Berg JJ, Sowemimo-Coker G, Chau S, Nunn A, Chan PA. Open pilot trial of a brief motivational interviewing-based HIV pre-exposure prophylaxis intervention for men who have sex with men: Preliminary effects, and evidence of feasibility and acceptability. AIDS Care. 2020;32(3):406–410. doi: 10.1080/09540121.2019.1622644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Molina, J.-M., Charreau, I., Spire, B., Cotte, L., Chas, J., Capitant, C., Tremblay, C., Rojas-Castro, D., Cua, E., Pasquet, A., Bernaud, C., Pintado, C., Delaugerre, C., Sagaon-Teyssier, L., Mestre, S. L., Chidiac, C., Pialoux, G., Ponscarme, D., Fonsart, J., … Rabian, C. (2017). Efficacy, safety, and effect on sexual behaviour of on-demand pre-exposure prophylaxis for HIV in men who have sex with men: An observational cohort study. The Lancet HIV, 4(9), e402–e410. 10.1016/S2352-3018(17)30089-9 [DOI] [PubMed]
- Morris SR, Jain S, Blumenthal J, Bolan R, Dubé MP, Henderson P, Corado K, Sun S, He F, Chow K, Burke L, Anderson PL, Moore DJ. Randomized trial of individualized texting for adherence building (iTAB) plus motivational interviewing for PrEP adherence in transgender individuals: The iM-PrEPT study. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2022;91(5):453–459. doi: 10.1097/QAI.0000000000003091. [DOI] [PubMed] [Google Scholar]
- Naar-King S, Outlaw A, Green-Jones M, Wright K, Parsons JT. Motivational interviewing by peer outreach workers: A pilot randomized clinical trial to retain adolescents and young adults in HIV care. AIDS Care. 2009;21(7):868–873. doi: 10.1080/09540120802612824. [DOI] [PubMed] [Google Scholar]
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed]
- Palacio A, Garay D, Langer B, Taylor J, Wood BA, Tamariz L. Motivational interviewing improves medication adherence: A systematic review and meta-analysis. Journal of General Internal Medicine. 2016;31(8):929–940. doi: 10.1007/s11606-016-3685-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PrEP Effectiveness | PrEP | HIV Basics | HIV/AIDS | CDC. (2021, May 13). https://www.cdc.gov/hiv/basics/prep/prep-effectiveness.html
- Prochaska, J. O., & DiClemente, C. C. (1982). Transtheoretical therapy: Toward a more integrative model of change. Psychotherapy: Theory, Research & Practice, 19(3), 276–288. 10.1037/h0088437
- Psaros, C., Haberer, J. E., Katabira, E., Ronald, A., Tumwesigye, E., Campbell, J. D., Wangisi, J., Mugwanya, K., Kintu, A., Enyakoit, M., Thomas, K. K., Donnell, D., Krows, M., Kidoguchi, L., Ware, N., Baeten, J. M., Celum, C., Bangsberg, D. R., & Safren, S. A. (2014). An intervention to support HIV pre-exposure prophylaxis (PrEP) adherence in HIV serodiscordant couples in Uganda. Journal of Acquired Immune Deficiency Syndromes (1999), 66(5), 522–529. 10.1097/QAI.0000000000000212 [DOI] [PMC free article] [PubMed]
- Rollnick, S., Butler, C. C., Kinnersley, P., Gregory, J., & Mash, B. (2010). Motivational interviewing. BMJ, 340, c1900. 10.1136/bmj.c1900 [DOI] [PubMed]
- Rollnick S, Miller WR. What is motivational interviewing? Behavioural and Cognitive Psychotherapy. 1995;23(4):325–334. doi: 10.1017/S135246580001643X. [DOI] [PubMed] [Google Scholar]
- Rubak S, Sandbæk A, Lauritzen T, Christensen B. Motivational interviewing: A systematic review and meta-analysis. The British Journal of General Practice. 2005;55(513):305–312. [PMC free article] [PubMed] [Google Scholar]
- Soleymani S, Britt E, Wallace-Bell M. Motivational interviewing for enhancing engagement in intimate partner violence (IPV) treatment: A review of the literature. Aggression and Violent Behavior. 2018;40:119–127. doi: 10.1016/j.avb.2018.05.005. [DOI] [Google Scholar]
- Stallings DT, Schneider JK. Motivational interviewing and fat consumption in older adults: A meta-analysis. Journal of Gerontological Nursing. 2018;44(11):33–43. doi: 10.3928/00989134-20180817-01. [DOI] [PubMed] [Google Scholar]
- Teixeira da Silva D, Bouris A, Ramachandran A, Blocker O, Davis B, Harris J, Pyra M, Rusie LK, Brewer R, Pagkas-Bather J, Hotton A, Ridgway JP, McNulty M, Bhatia R, Schneider JA. Embedding a linkage to preexposure prophylaxis care intervention in social network strategy and partner notification services: Results from a pilot randomized controlled trial. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2021;86(2):191. doi: 10.1097/QAI.0000000000002548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- VanBuskirk KA, Wetherell JL. Motivational interviewing with primary care populations: A systematic review and meta-analysis. Journal of Behavioral Medicine. 2014;37(4):768–780. doi: 10.1007/s10865-013-9527-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White JJ, Dangerfield DT, II, Grieb SM. Methodological considerations for conducting focus groups in HIV prevention research among Black men who have sex with men. Public Health Nursing. 2019;36(3):439–445. doi: 10.1111/phn.12592. [DOI] [PMC free article] [PubMed] [Google Scholar]