Dear Editor,
Lichen planopilaris (LPP) is the most frequent primary lymphocytic cicatricial alopecia. 1 LPP has been divided into four variants: classic LPP, frontal fibrosing alopecia (FFA), Graham‐Little syndrome, and fibrosing alopecia in a pattern distribution (FAPD). 1 , 2 The annual incidence of biopsy‐proven LPP in four US tertiary hair centres was 1.15−7.59%. 2 In the classic form, typically, the vertex and parietal region are affected. Clinically in early lesions perifollicular erythema and keratotic follicular papules are visible. In some cases, the signs especially in early stage of the disease, may be very subtle, what makes the diagnosis challenging. 2 , 3 In further stages of the classic LPP lymphocytic inflammation resolves and it is replaced by scarring. In the late‐stage single or multiple scarring, alopecic patches are detectable. 1 , 2 , 3
Histopathological examination and trichoscopy plays an essential role in the diagnosing of LPP. 4 , 5 In early‐stage vacuolar interface changes with a moderately dense perifollicular lichenoid lymphocytic cell infiltrate are characteristic at the level of the infundibulum and isthmus. 4 Other typical signs include infundibular hyperkeratosis and hypergranulosis. In rare cases also a lichenoid infiltrate may be present in the interfollicular epidermis. 6 In advanced lesions, concentric lamellar perifollicular fibrosis embracing the infundibulum and separating the inflammatory infiltrate from the hair follicle is present. In the longstanding lesions, dilated blood vessels and clefts between the follicular epithelium and stroma may be visible. 4 , 6
Line‐field confocal optical coherence tomography (LC‐OCT) is a new imaging technique that was recently developed to perform in vivo biopsy of the skin and mucosa with a resolution close to the histopathology examination. 7 , 8 LC‐OCT combines the benefits of conventional optical coherence tomography (OCT) and reflectance confocal microscopy (RCM). It provides vertical images up to the depth of 5oo μm like conventional OCT. It has also excellent lateral and axial resolution at the level of 1 μm, which allows visualisation of the skin and mucosa with cellular details. LC‐OCT permits to provide two‐dimensional (2D) vertical and horizontal images as well as three‐dimensional (3D) reconstructions. 7 , 8 , 9
Recent studies investigated the potential usefulness of reflectance confocal microscopy as a helpful diagnostic tool in lichen planopilaris. 10 Herein, we describe for the first time LC‐OCT features of classic form of LPP. Six patients (four females and two males; mean age 47 [38‐55] years) with classic lichen planopilaris diagnosed by clinical presentation and trichoscopy were included in the study (Figure 1A, 1B, 2A, 2B). Non‐invasive examinations with LC‐OCT were performed in vertical, horizontal and 3D mode (DeepLive, DAMAE Medical) at the lesional skin and contralateral healthy sites.
FIGURE 1.
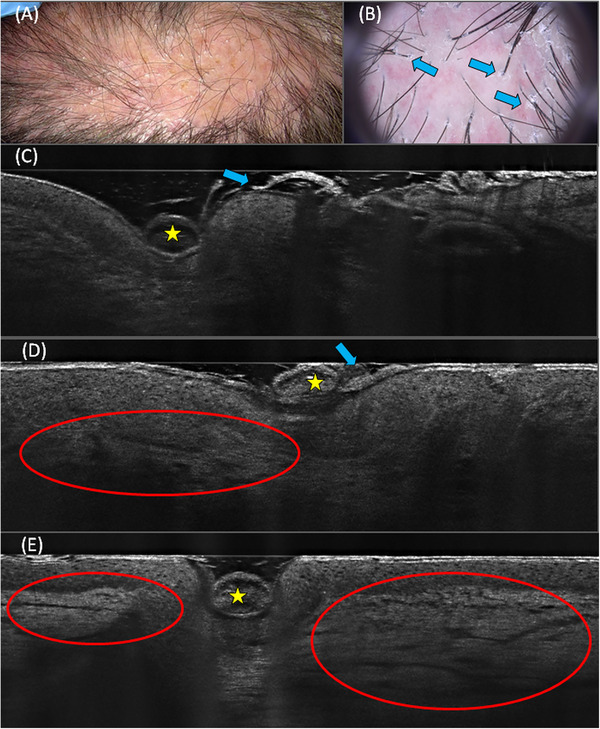
Clinical picture of patient with classic type of lichen planopilaris. Keratotic follicular papules are visible on the vertex of the scalp (A). Trichoscopy of patient with the classic LPP. Perifolicular scaling and elongated blood vessels (blue arrows) are visible (B). LC‐OCT image in a vertical mode showed hair shaft (yellow stars), perifollicular scaling (blue arrows) (C,D) and elongated blood vessels (red ovals) (D,E).
FIGURE 2.
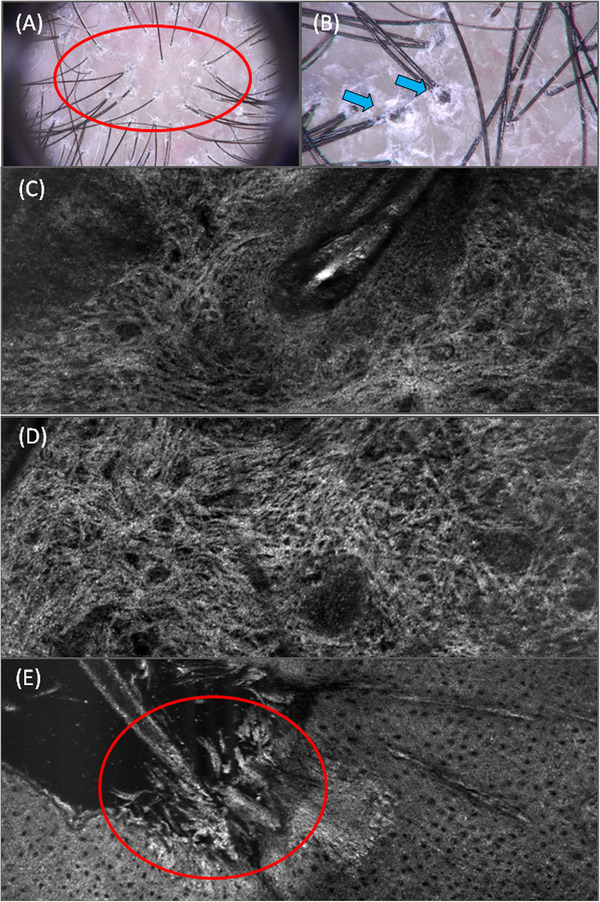
Trichoscopic image of patient with classic type of lichen planopilaris. Perifollicular scaling (20x magnification, red oval and 70x magnification blue arrows) is visible on trichoscopic picture (A,B). LC‐OCT image in a horizontal mode showed scarring around the hair follicle (C). LC‐OCT image in a horizontal mode revealed increased number of white, ill‐defined, coarse dermal fibres corresponding to the scarring (D). LC‐OCT image in a horizontal mode showed perifollicular hyperkeratosis (F).
Vertical 2D LC‐OCT images showed infundibular hyperkeratosis visible as whitish material filling the ostium of the hair follicle and surrounding the hair shaft (Figure 1C,D). Furthermore, dilated blood vessels were observed in the dermis as non‐reflective dark, longitudinal areas (Figure 1D,E). Horizontal 2D LC‐OCT images also showed infundibular hyperkeratosis (Figure 2E). Moderately dense perifollicular lichenoid cell infiltrate was present around the hair follicle within the dermis. Inflammatory cells were visible as small, hyperreflective roundish cells . Moreover, increased number of white, ill‐defined, coarse dermal fibres surrounding the hair follicle were also observed (Figure 2C). In the central part of patchy alopecia white, thick collagen bundles were present corresponding to the scarring (Figure 2D). 3D LC‐OCT images reveal, like the horizontal and vertical images, infundibular hyperkeratosis, perifollicular lichenoid cell infiltrate and coarse dermal fibres surrounding the hair follicle. In the contra‐lateral healthy sites, we did not observe above‐described abnormalities.
LC‐OCT enables the examination of scalp lesions in the vertical and horizontal planes with high cellular resolution. LC‐OCT brings many advantages compared with other non‐invasive diagnostic methods, such as a possibility of vertical and horizontal imaging along with the reproduction of a ‘virtual histology’ by applying 3D software rendering. 7 , 8 , 9 In addition, research is ongoing to develop a new automated method for precise, rapid, and direct assessment of skin matrix quality from in vivo LC‐OCT images. Future studies evaluating the application of this method in scarring alopecia could be conducted. 11
LC‐OCT appears to be an excellent diagnostic tool for in vivo examination of inflammatory skin diseases. As the preliminary study has shown, LC‐OCT appears to be a rapid and effective tool that can help distinguish between lichenoid papular diseases and their clinical simulators in patients during childhood and adolescence. 12 Another study showed that most of the characteristic features of lichen planus seen on histopathology are also visible on LC‐OCT images. 13
Summing up, this is the first study showing that LC‐OCT allows visualisation of major key diagnostic features of classic lichen planopilaris in the real time. Further investigations are needed to validate the present findings.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ETHICS STATEMENT
The patients in this manuscript have given written informed consent to the publication of their case details and images.
ACKNOWLEDGMENTS
None. The authors have nothing to report.
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.
REFERENCES
- 1. Kang H, Alzolibani AA, Otberg N, et al. Lichen planopilaris. Dermatol Ther. 2008;21(4):249‐256. [DOI] [PubMed] [Google Scholar]
- 2. Svigos K, Yin L, Fried L, et al. A practical approach to the diagnosis and management of classic lichen planopilaris. Am J Clin Dermatol. 2021;22(5):681‐692. [DOI] [PubMed] [Google Scholar]
- 3. Bolduc C, Sperling LC, Shapiro J. Primary cicatricial alopecia: Lymphocytic primary cicatricial alopecias, including chronic cutaneous lupus erythematosus, lichen planopilaris, frontal fibrosing alopecia, and Graham‐Little syndrome. J Am Acad Dermatol. 2016;75(6):1081‐1099. [DOI] [PubMed] [Google Scholar]
- 4. Stefanato CM. Histopathology of alopecia: a clinicopathological approach to diagnosis. Histopathology. 2010;56:24‐38. [DOI] [PubMed] [Google Scholar]
- 5. Starace M, Orlando G, Alessandrini A et al. Diffuse variants of scalp lichen planopilaris: Clinical, trichoscopic, and histopathologic features of 40 patients. J Am Acad Dermatol. 2020;83(6):1659‐1667. [DOI] [PubMed] [Google Scholar]
- 6. Gálvez‐Canseco A, Sperling L. Lichen planopilaris and frontal fi‐brosing alopecia cannot be differentiated by histopathology. J Cutan Pathol. 2018;45:313‐317. [DOI] [PubMed] [Google Scholar]
- 7. Ogien J, Daures A, Cazalas M, Perrot JL, Dubois A. Line‐field confocal optical coherencetomography for three‐dimensional skin imaging. Front Optoelectron. 2020;13:381‐392 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cinotti E, Bertello M, Cartocci A et al. Comparison of reflectance confocal microscopy and line‐field optical coherence tomography for the identification of keratinocyte skin tumours. Skin Res Technol. 2023;29:e13215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Chauvel‐Picard J, Bérot V, Tognetti L. et al. Line‐field confocal optical coherence tomography as a tool for three‐dimensional in vivo quantification of healthy epidermis: a pilot study. J Biophotonics. 2022;15:e202100236. [DOI] [PubMed] [Google Scholar]
- 10. Kurzeja M, Czuwara J, Walecka I et al. Features of classic lichen planopilaris and frontal fibrosing alopecia in reflectance confocal microscopy: a preliminary study. Skin Res Technol. 2021;27:266‐271. [DOI] [PubMed] [Google Scholar]
- 11. Breugnot J, Rouaud‐Tinguely P, Gilardeau S. Utilizing deep learning for dermal matrix quality assessment on in vivo line‐field confocal optical coherence tomography images. [DOI] [PMC free article] [PubMed]
- 12. Tognetti L, Carraro A, Cinotti E et al. Line‐field confocal optical coherence tomography for non‐invasive diagnosis of lichenoid dermatoses of the childhood: a case series. Skin Res Technol. 2021;27:1178‐1181. Skin Res Technol. 2023 e13221. [DOI] [PubMed] [Google Scholar]
- 13. Verzì AE, Broggi G, Micali G et al. Line‐field confocal optical coherence tomography of psoriasis, eczema and lichen planus: a case series with histopathological correlation. J. Eur. Acad. Dermatol. Venereol. 2022;36:1884‐1889. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data are not publicly available due to privacy or ethical restrictions.


