Abstract
Since the start of the COVID-19 pandemic, wastewater surveillance has emerged as a powerful tool used by public health authorities to track SARS-CoV-2 infections in communities. In May 2020, the Houston Health Department began working with a coalition of municipal and academic partners to develop a wastewater monitoring and reporting system for the city of Houston, Texas. Data collected from the system are integrated with other COVID-19 surveillance data and communicated through different channels to local authorities and the general public. This information is used to shape policies and inform actions to mitigate and prevent the spread of COVID-19 at municipal, institutional, and individual levels. Based on the success of this monitoring and reporting system to drive public health protection efforts, the wastewater surveillance program is likely to become a standard part of the public health toolkit for responding to infectious diseases and, potentially, other disease-causing outbreaks.
Keywords: wastewater, wastewater surveillance, SARS-CoV-2, COVID-19, public health interventions
Individuals infected with SARS-CoV-2, the virus that causes COVID-19, shed viral particles in their feces that can be detected in wastewater.1-5 During the COVID-19 pandemic, public health authorities worldwide began testing wastewater to monitor trends in SARS-CoV-2 viral levels and to use that information to develop interventions to slow or stop the spread of the virus.
Wastewater surveillance has several benefits. It is a passive method of detection that does not require any action from the public other than using the bathroom as they would normally. Because wastewater samples are pooled, results cannot be linked to a specific individual, thereby protecting privacy. Wastewater surveillance captures data on both symptomatic and asymptomatic COVID-19 infections6,7 and can provide insights into infection levels in communities where clinical diagnostic tests are underused or unavailable. 8 This ability to capture data on an entire population in a given community is increasingly relevant as the use of at-home tests becomes more widespread. The ability to monitor entire population groups in a given location allows public health authorities to collect data on racial and ethnic minority groups that might otherwise be difficult to obtain because of health disparities that create barriers to accessing the health care system 9 and to use that information to gear interventions toward populations that have been disproportionately affected by the COVID-19 pandemic. A recent study indicated that monitoring wastewater levels may precede changes in COVID-19–related hospitalizations by 1 to 2 weeks. 10 Wastewater data can also be useful for assessing the impact of public health interventions such as lockdowns and subsequent reopenings.9,11,12
In May 2020, the Houston Health Department (HHD) collaborated with academic and municipal partners to develop a SARS-CoV-2 wastewater surveillance and reporting system for Houston, Texas. Each week, 24-hour composite wastewater samples are collected from 39 wastewater treatment plants (WWTPs) and 32 lift stations, which provide information at the sewershed level. A 24-hour composite sample is collected using a refrigerated autosampler installed at the sample collection location. The autosampler collects an aliquot of wastewater (350 mL) once every hour for 24 hours. Thus, the final wastewater sample consists of a mixture of wastewater aliquots collected during a single day. Composite samples are more representative than grab samples (ie, single wastewater samples taken at a single point in time or a series of samples collected during a period that does not exceed 15 minutes) of the composition of wastewater across a day.13,14 Composite wastewater samples are also collected from 74 manholes across the city. These manhole samples include 24-hour composite samples from 21 congregate living facilities (11 shelters, 9 nursing homes, and 1 jail served by 2 manholes) and 6-hour composite samples from 52 schools. The entire system covers a population of more than 2.2 million people.
Replicate samples from all facilities are sent to 2 independent laboratories for analysis. The laboratories concentrate raw wastewater by using electronegative filtration and quantify the SARS-CoV-2 N1 and N2 gene targets by using either reverse transcription droplet digital polymerase chain reaction (RT-ddPCR) or reverse transcription quantitative polymerase chain reaction (RT-qPCR).10,15 The laboratories also screen for variants of concern by using targeted assays and targeted amplicon sequencing of the SARS-CoV-2 genome. 16
We developed a system of statistical models to analyze laboratory data derived from the wastewater collection system. One component analyzes data from the WWTPs. Using a flow-based normalization approach, we calculate the viral load at each WWTP by multiplying the measured viral RNA concentration by the average 24-hour flow rate for the corresponding WWTP. We use this information to generate a temporal analysis for each WWTP and a spatial–temporal analysis that combines data from all 39 WWTPs to obtain an estimated viral load for the entire city. The temporal analysis information is also used to generate estimates for temporal analyses at the zip code level, based on the percentage area of a zip code that is serviced by a WWTP. A second component of the statistical system analyzes data from lift stations and manholes and provides real-time, spatial visualizations of findings, which are classified as positive, inconclusive, or negative based on the levels of SARS-CoV-2 N1 and N2 gene targets detected in each sample.
The analysis system integrates information from other HHD COVID-19 surveillance systems (eg, clinical positivity, hospitalization, vaccination rates) and pertinent Houston demographic data (eg, race, ethnicity, socioeconomic status) to generate summary reports that are shared regularly with the mayor’s office, HHD leadership, various health authorities, and the general public. Each group uses this information in a distinct way to guide the development of public health policies and interventions to mitigate and prevent the spread of COVID-19 in communities throughout Houston.
Communication Outreach
Municipal and HHD Leadership
Houston is the fourth largest city in the United States, with an estimated population of >2.3 million residents (as of July 2021). 17 The Greater Houston area, which encompasses approximately 10 000 square miles, is one of the most racially and ethnically diverse in the nation. Houston is also home to the Texas Medical Center (TMC), the largest medical complex in the world. Effective communication of COVID-19–related public health data between HHD and the leaders of such a large, diverse, and complex metropolitan area has been crucial throughout the pandemic.
HHD is the central clearinghouse for public health information in Houston. Each week, wastewater data are combined with other COVID-19–related data and compiled in a detailed report that provides information about the status of SARS-CoV-2 viral loads at sewershed, zip code, and manhole levels. Every Monday, the wastewater data report is emailed to the mayor of Houston, the chief medical officer for the City of Houston (hereinafter, chief medical officer), the director and assistant directors of HHD, and leaders from HHD’s COVID-19 Response Team, which includes outreach, testing, vaccination, and reporting strike teams. The strike teams then forward facility-specific data to representatives from the Houston Independent School District (HISD) and congregate living facilities.
Information from the weekly report is also discussed at biweekly Data to Action meetings in HHD. The magnitude of and trends in wastewater viral load are used to prioritize zip codes for public health interventions, including site visits, telephone calls, emails, materials distribution (eg, door hangers, flyers, advertising related to COVID-19 education, testing, vaccination), door-to-door canvassing, workshops, and public health education classes. From August 13, 2020, through September 13, 2022, HHD’s community health education engagement activities and apartment canvasing team made contact with 161 190 people in 136 zip codes. In the zip codes most frequently prioritized for intervention, an average of 862 people received community health education outreach compared with an average of 137 people for the remainder of the city (email communication, F. Foreman-Hayes, DrPh, LVN, HHD, September 13, 2022). Priority zip codes were also targeted for the establishment of testing centers and vaccine clinics.
HHD also generates COVID-19 fact sheets, which are used internally to prioritize neighborhoods and schools with high COVID-19 positivity rates for further outreach and vaccination efforts. A fact sheet is a 1-page document that uses simple graphics and tables to convey information about vaccination rates (both in the zip code and citywide and broken down by race, ethnicity, and age), vaccination goals, and wastewater surveillance data for schools located in the zip code.
When a manhole’s wastewater sample tests positive for SARS-CoV-2, the appropriate strike team is activated. For congregate living facilities, contact is made with the facility’s director to determine if a new outbreak has occurred. If so, an HHD epidemiologist or subject matter expert conducts an on-site assessment and recommends a plan of action (eg, testing, lockdown, isolation). For schools, a member of the strike team assesses the school’s COVID-19 status and works with school leadership to coordinate contact tracing and testing and to provide isolation and quarantine letters as needed. The strike team maintains contact with the school for at least 10 days after being alerted to a positive manhole result or until wastewater samples from the manhole test negative. These assessment and follow-up actions have tapered off as staff at individual facilities have become more adept at responding to positive COVID-19 cases and have made adjustments to disease containment plans that improved mitigation in general.
Health Authorities
The chief medical officer also regularly disseminates summary information about wastewater data to various health authorities, including the presidents and chief executive officers of TMC facilities (hereinafter, TMC leadership), city and county health officials (hereinafter, local health authorities), and key infectious disease physicians and epidemiologists from health care organizations throughout TMC and the Greater Houston area. The primary method for wastewater data dissemination to the various health authorities is a COVID-19 conference call held by the chief medical officer, which initially occurred on a weekly basis starting in February 2020 and shifted to a biweekly basis in June 2022. By September 2021, conference call attendees included TMC leadership, local health authorities, and a team of infectious disease physicians and epidemiologists from the Memorial Hermann Hospital System (hereinafter, Memorial Hermann), Houston Methodist Hospital, Baylor St. Luke’s Medical Center, Texas Children’s Hospital, and the Harris Health System. These health authorities use the wastewater data communicated in the COVID-19 conference calls to shape policies and inform decision-making in response to changes in SARS-CoV-2 levels in Houston’s wastewater.
James J. McCarthy, MD, chief physician executive for Memorial Hermann and a COVID-19 conference call attendee, reported that wastewater data were the most reliable indicator for predicting upcoming needs related to COVID-19 hospitalizations (email communication, June 6, 2022). As an example, during the COVID-19 surge that took place in late 2021 and early 2022, Memorial Hermann found that trends in wastewater viral loads predated increases in hospital bed use by 2 weeks, giving the hospital time to prepare for additional hospitalizations by allocating space, adjusting staff levels, and scheduling delays for elective surgeries and procedures (email communication, June 6, 2022).
In 2020, Edward J. Septimus, MD, at the Department of Population Medicine at Harvard University in Boston, Massachusetts, began attending the COVID-19 conference calls. Dr. Septimus includes wastewater data from the conference calls in his weekly COVID-19 newsletter, which provides summaries of COVID-19–related publications and updates on local and national infection trends. The newsletter has a circulation of >1000 people and is archived by Memorial Hermann and the Gulf Coast Consortia for Quantitative Biomedical Sciences. According to Dr. Septimus, sharing wastewater data through the newsletter allows him to give health authorities advance notice about infection trends (email communication, September 6, 2022).
General Public
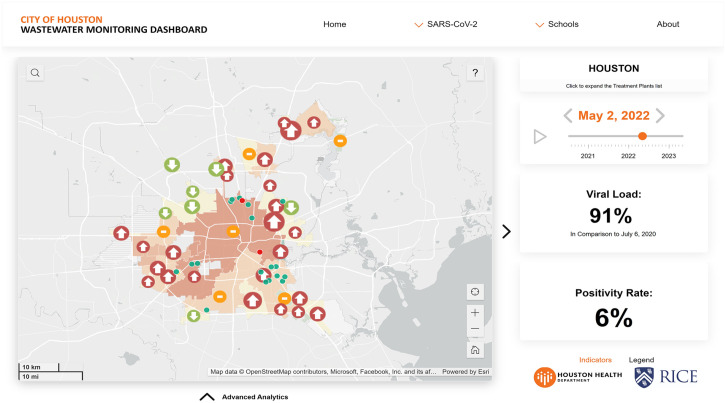
HHD has developed 2 primary methods for sharing wastewater data with the general public in Houston. In September 2021, HHD and the Spatial Studies Lab at Rice University launched an interactive dashboard on HHD’s public-facing website that displays levels of SARS-CoV-2 found in wastewater samples collected from the 39 WWTPs and 52 manholes in the wastewater surveillance system at HISD schools (Figure 1). 18 Facilities are depicted on maps of Houston and surrounding areas. Coverage areas for WWTPs are color coded according to the level of the viral load detected in each week’s wastewater samples and labeled with arrows to depict temporal trends in viral load levels. The bottom of the dashboard expands to display a historical plot of citywide viral load levels against positivity rates measured through diagnostic testing. Schools are color coded to indicate whether SARS-CoV-2 was detected in wastewater samples from their manholes. Historical testing data can be accessed by expanding the bottom of each school’s page. The dashboard also provides information about COVID-19 variants, vaccination rates, and the detection of influenza in school manholes.
Figure 1.
SARS-CoV-2 wastewater monitoring dashboard in Houston, Texas, 2022. The main page displays a map of Houston and the surrounding area with the coverage area of the 39 wastewater treatment plants (WWTPs) and the point location of schools. The dashboard is interactive. Data update as the user selects locations or scrolls through time. The menu button leads to other parts of the dashboard, including heat maps of viral load levels and trends, detection of influenza in schools, detection of SARS-CoV-2 variants, and a zip code map of estimated viral load. The map illustrates the benefits of geospatial analysis: the trend in northwest WWTPs is decreasing (indicated by down arrows), while trends in other WWTPs are increasing (indicated by up arrows) or have plateaued (indicated by dashes).
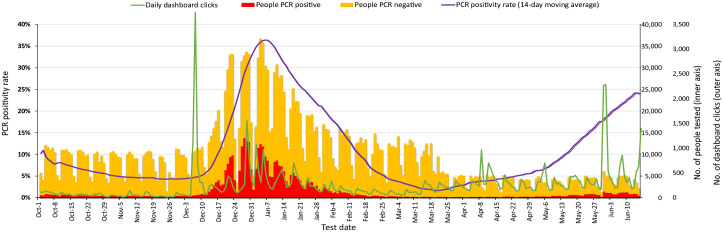
User engagement with the wastewater monitoring dashboard spikes at the start of COVID-19 surges. The dashboard recorded its highest number of clicks (>3000) on December 8, 2021, just prior to the outset of the Omicron surge (Figure 2). In addition, academic institutions such as Rice University and Baylor College of Medicine have referred to wastewater surveillance data or linked directly to the wastewater monitoring dashboard in informational emails sent to students and employees about rising COVID-19 levels in Houston.
Figure 2.
Use of SARS-CoV-2 wastewater monitoring dashboard, Houston, Texas, October 1, 2021, through June 10, 2022. The daily number of clicks on the dashboard is plotted alongside the City of Houston’s daily polymerase chain reaction (PCR)–positive case count, PCR-negative case count, and 14-day moving average PCR positivity rate. The daily number of dashboard clicks over time increases as the 14-day moving average PCR positivity rate increases, even if testing counts do not increase. This is seen in the Omicron wave of December 2021–February 2022 and again in May–June 2022.
The chief medical officer also engages in outreach efforts to educate the public about wastewater data and how the data can be used through lay and social media. Once the monitoring system was operational, the chief medical officer began including wastewater data in weekly press conferences. The information is now communicated to the news media via a weekly public health telephone conference. The wastewater surveillance system and the data it produces are frequently referenced in the Houston Chronicle.19-26 In March 2022, the chief medical officer recorded a 16-minute educational video that provides an overview of Houston’s wastewater surveillance system, the science of wastewater surveillance, and the public health benefits of the manhole testing program at schools. 27 The video was originally shared with HISD school nurses as part of an educational webinar but was subsequently posted on HHD’s website (via YouTube) and is now accessible to the general public. Several science teachers from HISD middle schools reported using the video to teach a unit on wastewater monitoring (email communication among seventh and eighth grade science teachers at a STEM magnet HISD school, school health program consultants from the Houston Health Foundation, and HHD, March 2022). Consultants from the Houston Health Foundation were working on a project as part of an ongoing partnership between HISD and HHD that was focused on using wastewater surveillance of COVID-19 in schools to improve communication and decision-making in the school setting.
Conclusion
The success of Houston’s wastewater monitoring and reporting system demonstrates that wastewater data can be used to guide public health interventions, particularly when communication strategies are tailored to the needs of various audiences. However, the widespread adoption of wastewater surveillance as a public health tool faces challenges. 28 Entities interested in developing their own wastewater surveillance systems will have upfront costs and may also encounter logistical difficulties when setting up wastewater sample collection and analysis processes, including supply chain issues (eg, shortages of wastewater autosamplers or laboratory supplies) and difficulty accessing 1 or more laboratories with the instruments and personnel required to perform RT-ddPCR or RT-qPCR quantification and genome sequencing or that conform to the Centers for Disease Control and Prevention’s (CDC’s) safety recommendations for working with SARS-CoV-2 specimens. 29 These obstacles can be offset by participation in CDC’s National Wastewater Surveillance System (NWSS), an initiative that provides financial support and resources for communities interested in conducting wastewater surveillance. 30 In addition, CDC has recognized the wastewater surveillance programs in Houston and Colorado (a collaboration between the Colorado Department of Health and the University of Denver) as NWSS Centers of Excellence, empowering them to share their expertise with and provide training, statistical support, office hours, and site visits to public health agencies across the United States.31,32
With these supports in place, wastewater surveillance has a future as an effective epidemiological tool in municipalities and other areas. The scope of Houston’s wastewater surveillance system is expanding to target other infectious diseases. As a result of HHD’s COVID-19 outreach and communication efforts, municipal leaders, health authorities, and the general public in Houston have found value in the information generated by wastewater surveillance, increasing the likelihood that wastewater data will play a vital role in responding to future public health emergencies.
Acknowledgments
The authors thank the following groups and professionals for their contributions to this project: Stadler Lab at Rice University; Houston Health Department (HHD) Bureau of Laboratory Services; Spatial Studies Lab at Rice University; TAILOR at Baylor College of Medicine; Houston Public Works; Deborah Banerjee, PhD (HHD); Coleen Boyle, PhD, MS Hyg, CDC Foundation; Kelsey Caton, MPH; Kendra Davis, MPH; Tanveer Farhad, MS; Juan Gonzalez, AA; Judy Harris, MBA; Courtney Hundley, MPH; Douglas Jennings, BS; Anthony Mulenga, MS; Jeremy Rangel, BS; Komal Sheth, MPH; Martha Stancil, MBA, RN, CNE-BCr; and Latreka Staten, MPH, MBA (HHD).
Footnotes
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the CDC Foundation (project no. 1085.46) and the Centers for Disease Control and Prevention (ELC-ED grant no. 6NU50CK000557-01-05 and ELC-CORE grant no. NU50CK000557).
ORCID iD: Loren Hopkins, PhD  https://orcid.org/0000-0003-0626-9775
https://orcid.org/0000-0003-0626-9775
References
- 1. Cai J, Xu J, Lin D, et al. A case series of children with 2019 novel coronavirus infection: clinical and epidemiological features. Clin Infect Dis. 2020;71(6):1547-1551. doi: 10.1093/cid/ciaa198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Holshue ML, Debolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929-936. doi: 10.1056/NEJMoa2001191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Tang A, Tong ZD, Wang HL, et al. Detection of novel coronavirus by RT-PCR in stool specimen from asymptomatic child, China. Emerg Infect Dis. 2020;26(6):1337-1339. doi: 10.3201/eid2606.200301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature. 2020;581(7809):465-469. doi: 10.1038/s41586-020-2196-x [DOI] [PubMed] [Google Scholar]
- 5. Xiao F, Tang M, Zheng X, Liu Y, Li X, Shan H. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology. 2020;158(6):1831-1833.e3. doi: 10.1053/j.gastro.2020.02.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chen Y, Chen L, Deng Q, et al. The presence of SARS-CoV-2 RNA in the feces of COVID-19 patients. J Med Virol. 2020;92(7):833-840. doi: 10.1002/jmv.25825 [DOI] [PubMed] [Google Scholar]
- 7. Weiss A, Jellingsø M, Sommer MOA. Spatial and temporal dynamics of SARS-CoV-2 in COVID-19 patients: a systematic review and meta-analysis. EBioMedicine. 2020;58:102916. doi: 10.1016/j.ebiom.2020.102916 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Medema G, Been F, Heijnen L, Petterson S. Implementation of environmental surveillance for SARS-CoV-2 virus to support public health decisions: opportunities and challenges. Curr Opin Environ Sci Health. 2020;17:49-71. doi: 10.1016/j.coesh.2020.09.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sharara N, Endo N, Duvallet C, et al. Wastewater network infrastructure in public health: applications and learnings from the COVID-19 pandemic. PLoS Glob Public Health. 2021;1(12):e0000061. doi: 10.1371/journal.pgph.0000061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hopkins L, Persse D, Caton K, et al. Citywide wastewater SARS-CoV-2 levels strongly correlated with multiple disease surveillance indicators and outcomes over three COVID-19 waves. Sci Total Environ. 2023;855:158967. doi: 10.1016/j.scitotenv.2022.158967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Hillary LS, Farkas K, Maher KH, et al. Monitoring SARS-CoV-2 in municipal wastewater to evaluate the success of lockdown measures for controlling COVID-19 in the UK. Water Res. 2021;200:117214. doi: 10.1016/j.watres.2021.117214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Stephens N, Béen F, Savic D. An analysis of SARS-CoV-2 in wastewater to evaluate the effectiveness of nonpharmaceutical interventions against COVID-19 in The Netherlands. ACS EST Water. 2022;2(11):2158-2166. doi: 10.1021/acsestwater.2c00071 [DOI] [PubMed] [Google Scholar]
- 13. Ahmed W, Bivins A, Bertsch PM, et al. Intraday variability of indicator and pathogenic viruses in 1-h and 24-h composite wastewater samples: implications for wastewater-based epidemiology. Environ Res. 2021;193:110531. doi: 10.1016/j.envres.2020.110531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. US Environmental Protection Agency, Science and Ecosystem Support Division. Operating procedure: wastewater sampling. Effective February 28, 2013. Accessed May 10, 2023. https://www.epa.gov/sites/default/files/2015-06/documents/Wastewater-Sampling.pdf
- 15. LaTurner ZW, Zong DM, Kalvapalle P, et al. Evaluating recovery, cost, and throughput of different concentration methods for SARS-CoV-2 wastewater-based epidemiology. Water Res. 2021;197:117043. doi: 10.1016/j.watres.2021.117043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Lou EG, Sapoval N, McCall C, et al. Direct comparison of RT-ddPCR and targeted amplicon sequencing for SARS-CoV-2 mutation monitoring in wastewater. Sci Total Environ. 2022;833:155059. doi: 10.1016/j.scitotenv.2022.155059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. US Census Bureau. Annual estimates of the resident population for incorporated places of 50,000 or more, ranked by July 1, 2021 population: April 1, 2020 to July 1, 2021. May 2022. Accessed May 10, 2023. https://www2.census.gov/programs-surveys/popest/tables/2020-2021/cities/totals/SUB-IP-EST2021-ANNRNK.xlsx
- 18. Houston Health Department and Rice University’s Ensor and Stadler Labs and Center for Research Computing’s Spatial Studies Lab. City of Houston Wastewater Monitoring Dashboard. September 2021. Updated October 3, 2022. Accessed October 14, 2022. https://covidwwtp.spatialstudieslab.org
- 19. Wu G. COVID infections are on the rise again in Houston. Will there be another surge? Houston Chronicle. July 16, 2021. Accessed September 17, 2022. https://www.houstonchronicle.com/news/houston-texas/health/article/COVID-infections-are-on-the-rise-again-in-16320085.php
- 20. McGuinness D. According to Houston’s wastewater, the surge of COVID-19 is only going to get worse. Houston Chronicle. August 4, 2021. Accessed September 17, 2022. https://www.houstonchronicle.com/news/houston-texas/houston/article/According-to-Houston-s-wastewater-the-surge-of-16364538.php
- 21. Hennes R. Houston testing wastewater for COVID Omicron variant. Houston Chronicle. December 1, 2021. Accessed September 17, 2022. https://www.houstonchronicle.com/coronavirus/article/Houston-testing-wastewater-for-COVID-omicron-16665798.php
- 22. McGuinness D. Omicron variant found in Houston wastewater, confirming spread of new strain locally. Houston Chronicle. December 7, 2021. Accessed September 17, 2022. https://www.houstonchronicle.com/news/houston-texas/health/article/omicron-variant-found-in-houston-waste-water-16681988.php
- 23. Foxhall E. COVID found in Houston wastewater spikes 285% in a week, reaching levels five times as high as first wave. Houston Chronicle. December 30, 2021. Accessed September 17, 2022. https://www.houstonchronicle.com/news/houston-texas/houston/article/COVID-found-in-Houston-wastewater-spikes-285-in-16739054.php
- 24. Mishanec N. Is Houston past the Omicron peak? With COVID transmission rates down, the worst may be over. Houston Chronicle. January 24, 2022. Accessed September 17, 2022. https://www.houstonchronicle.com/news/houston-texas/health/article/Is-Houston-past-the-omicron-peak-With-COVID-16800419.php
- 25. Mishanec N. Houston sewage workers finding less COVID-19 in wastewater. Houston Chronicle. February 3, 2022. Accessed September 17, 2022. https://www.houstonchronicle.com/news/houston-texas/health/article/Houston-sewage-workers-finding-less-COVID-19-in-16827716.php
- 26. Mishanec N. Houston’s COVID cases are climbing again, wastewater data shows. Houston Chronicle. May 31, 2022. Accessed September 17, 2022. https://www.houstonchronicle.com/coronavirus/article/Houston-sewage-workers-finding-more-COVID-19-in-17210263.php
- 27. Houston Health Department. HHD HISD Wastewater Testing Program. February 11, 2022. Accessed September 17, 2022. https://www.youtube.com/watch?v=Q-x5KOL7j9o
- 28. Safford HR, Shapiro K, Bischel HN. Wastewater analysis can be a powerful public health tool—if it’s done sensibly. Proc Natl Acad Sci U S A. 2022;119(6):e2119600119. doi: 10.1073/pnas.2119600119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Centers for Disease Control and Prevention. Interim laboratory biosafety guidelines for handling and processing specimens associated with coronavirus disease 2019 (COVID-19). Updated December 13, 2021. Accessed May 10, 2023. https://www.cdc.gov/coronavirus/2019-nCoV/lab/lab-biosafety-guidelines.html
- 30. Centers for Disease Control and Prevention. National Wastewater Surveillance System (NWSS). Updated March 14, 2023. Accessed May 10, 2023. https://www.cdc.gov/healthywater/surveillance/wastewater-surveillance/wastewater-surveillance.html
- 31. Centers for Disease Control and Prevention. Wastewater surveillance: progress in the United States. Last reviewed March 9, 2023. Accessed May 10, 2023. https://www.cdc.gov/nwss/progress.html
- 32. Houston Health Department. Houston Health Department earns CDC designation as Center of Excellence for wastewater epidemiology. August 3, 2022. Accessed May 10, 2023. https://www.houstonhealth.org/news/news-releases/houston-health-department-earns-cdc-designation-center-excellence-wastewater-epidemiology