Abstract
Objectives:
Autism spectrum disorder (autism) is a heterogeneous condition that poses challenges in describing the needs of individuals with autism and making prognoses about future outcomes. We applied a newly proposed definition of profound autism to surveillance data to estimate the percentage of children with autism who have profound autism and describe their sociodemographic and clinical characteristics.
Methods:
We analyzed population-based surveillance data from the Autism and Developmental Disabilities Monitoring Network for 20 135 children aged 8 years with autism during 2000-2016. Children were classified as having profound autism if they were nonverbal, were minimally verbal, or had an intelligence quotient <50.
Results:
The percentage of 8-year-old children with profound autism among those with autism was 26.7%. Compared with children with non–profound autism, children with profound autism were more likely to be female, from racial and ethnic minority groups, of low socioeconomic status, born preterm or with low birth weight; have self-injurious behaviors; have seizure disorders; and have lower adaptive scores. In 2016, the prevalence of profound autism was 4.6 per 1000 8-year-olds. The prevalence ratio (PR) of profound autism was higher among non-Hispanic Asian/Native Hawaiian/Other Pacific Islander (PR = 1.55; 95 CI, 1.38-1.73), non-Hispanic Black (PR = 1.76; 95% CI, 1.67-1.86), and Hispanic (PR = 1.50; 95% CI, 0.88-1.26) children than among non-Hispanic White children.
Conclusions:
As the population of children with autism continues to change, describing and quantifying the population with profound autism is important for planning. Policies and programs could consider the needs of people with profound autism across the life span to ensure their needs are met.
Keywords: autism, surveillance, public health
Autism spectrum disorder (ASD; autism) is a developmental disability that manifests during childhood, affects multiple areas of development, and usually lasts throughout a person’s life. 1 Autism varies in presentation and can be associated with a wide range of social, communication, and behavioral problems and outcomes. This heterogeneity poses challenges in describing the needs of people with autism and making prognoses about future outcomes.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) introduced severity levels for people with autism in the domains of social communication and restricted and repetitive behaviors to indicate the degree of support needed, 2 but they lack validation and their application might not be consistent.3,4 Increasing efforts have been made in scientific and family advocacy communities to define people with autism who will likely have the greatest need for supports and services. 5 A recent Lancet commission defined “profound autism” as having autism with an overall or subdomain intelligence quotient (IQ) score <50 or being nonverbal or minimally verbal. 6 The commission indicated that children with profound autism were also more likely to have self-injurious behavior or epilepsy and require around-the-clock supervision than children without profound autism. 6
As a result of this new and highly debated definition, there is a need for population-based information about the prevalence and characteristics of people who meet the criteria for profound autism. This information is critical for developing effective public health policies and programs to provide support across the life span. For example, one autism advocacy group is primarily focused on recognition and policy solutions for forms of autism that “by virtue of any combination of cognitive and functional impairments, necessitate continuous or near-continuous supervision, services and supports over the lifespan. Individuals in this category are often nonverbal or have limited use of language, are intellectually disabled, and, in a subset, exhibit challenging behaviors that interfere with safety and well-being.” 7 This new definition of profound autism may help to quantify the population with high levels of need in these areas. In this article, we applied the newly recognized definition of profound autism to population-based surveillance data in selected US communities to (1) estimate the percentage of children with profound autism and compare their sociodemographic and clinical characteristics with those of children who have non–profound autism and (2) estimate the population prevalence for both groups across time.
Methods
Study Design and Population
The Autism and Developmental Disabilities Monitoring (ADDM) Network has conducted population-based surveillance of 8-year-old children with autism at selected US sites in even-numbered years since 2000 to estimate the prevalence of autism. The ADDM Network uses records-based surveillance methodology in which staff review records from medical, education, and service providers, as previously described. 8 Children were classified as having autism after record review by clinicians who applied a standard case definition of ASD based on behavioral criteria for ASD described in the DSM-IV (2000-2014) 9 and DSM-5 (2016). 2 Sites linked children’s records to birth certificate information from their states to identify additional birth, maternal, and demographic characteristics. We obtained population denominators from the National Center for Health Statistics vintage 2018 bridged-race postcensal population estimates. 10 For study areas comprising subcounty school districts, we implemented a standardization process using public school enrollment counts to adjust the population estimates. 8 The Centers for Disease Control and Prevention determined this was a public health surveillance activity, deemed not to be research, and, therefore, exempt from institutional review board review.
We excluded 2 sites (Missouri and Pennsylvania) from this analysis because of a lack of access to educational records in which cognitive functioning data are typically included. We analyzed data from 15 sites (Alabama, Arkansas, Arizona, Colorado, Florida, Georgia, Maryland, Minnesota, North Carolina, New Jersey, South Carolina, Tennessee, Utah, Wisconsin, and West Virginia). We also excluded 2 ADDM surveillance years (2012 and 2014) because data on verbal status were not captured during these years.
Sociodemographic information collected included state of residence, sex (male, female), race and ethnicity (non-Hispanic Black [hereinafter, Black], non-Hispanic White [hereinafter, White], non-Hispanic Asian/Native Hawaiian/Other Pacific Islander [hereinafter, API], non-Hispanic American Indian/Alaska Native [hereinafter, AI/AN], or Hispanic), and highest maternal educational attainment (high school diploma, bachelor’s degree, or >bachelor’s degree). We also included census tract–level socioeconomic indicator rank values: (1) education: percentage of the population aged ≥25 years with ≥high school diploma or General Educational Development (GED), (2) poverty: percentage of families with children aged <19 years living below the federal poverty level, and (3) median annual household income: percentile rank for census tract. Birth characteristics collected included birthweight <2500 g (low birthweight; yes or no) and gestational age <37 weeks (preterm; yes or no). Clinical and educational characteristics collected included cognitive functioning scores, adaptive functioning composite scores, verbal status, self-injurious behavior, aggressive behavior, staring spells or seizure-like activity, and special education eligibility category.
Profound Autism Criteria
We categorized children as having profound autism if they were either nonverbal or minimally verbal or had an IQ <50. 6 We considered children to be nonverbal or minimally verbal if any of the following were identified in the records: (1) most recent evaluation at ≥48 months of age describing a child as nonverbal (median [IQR], 79 [65-93] months) or child determined to be nonverbal (no spontaneous words or word approximations) by clinician record review, (2) language classified primarily as echolalia or jargon by clinician review, or (3) being administered an Autism Diagnostic Observation Scale Module 1 (a gold standard observational measure appropriate for nonverbal or minimally verbal children) at age ≥48 months (median [IQR], 60 [53-70] months). 11 A sensitivity analysis increasing the age cutoff to ≥60 months minimally lowered (by <1 percentage point) the overall percentage of children with profound autism; thus, we kept the ≥48 months cutoff to capture children who may not have had a more recent language assessment recorded. If none of these indicators were identified, we categorized the child as being verbal.
We categorized children as having an IQ <50 if the most recent standard score results of an IQ test for either the overall IQ score or IQ subdomain score was <50. IQ data were not available for 19% (n = 3894) of children and were imputed.
Statistical Analyses
To impute missing data, we used the multivariate imputation by chained equations approach with 20 imputed datasets. 12 We used a separate imputation model for each variable: logistic regression for binary data (self-injurious behavior, aggressive behavior, IQ <50, preterm birth, and low birthweight) and polytomous logistic regression for categorical data (census-tract socioeconomic level, maternal education level, and adaptive score level). We created a descriptive summary of the percentage of the population with profound autism and prevalence ratios (PRs) among autism cases and 95% CIs comparing characteristics of children with profound autism with children with non–profound autism on the complete case (ie, nonimputed) and multiply imputed (imputed) datasets. We also calculated the median and IQR of age of first autism diagnosis among children with an age of diagnosis (age of diagnosis was not included in the imputation models because some children who met the ADDM autism case definition never had a documented clinical diagnosis) for the profound autism and non–profound autism groups. We further described characteristics of the profound autism and non–profound autism populations in the multiply imputed dataset.
For the 2016 surveillance year, we calculated the overall, sex-specific, race and ethnicity–specific, and site-specific population prevalence estimates of children with profound and non–profound autism per 1000 children aged 8 years and associated PRs to compare prevalence estimates between groups within the profound and non–profound autism populations, respectively. For study years 2000-2010, we calculated the overall population prevalence estimates by year to examine changes in the prevalence of profound and non–profound autism over time. We used Stata release 17 (StataCorp LLC) and R version 4.1.2 (R Foundation for Statistical Computing) for data management and analyses.
Results
The final sample included 20 135 children aged 8 years identified as having autism across 7 surveillance years and 15 sites (eTable 1 in Supplemental Material). Of these children, 26.7% (Table 1) had profound autism in the imputed data compared with 29.4% of children in the nonimputed data (eTable 2 in Supplemental Material); we imputed the IQ level of approximately 8% of all cases of profound autism.
Table 1.
Characteristics of children aged 8 years with autism (N = 20 135), by profound autism status—ADDM Network, 15 sites, United States, 2000-2016 a
| Characteristic | Total, b no. (%) | Non–profound autism, c % (n = 14 755) | Profound autism, d % (n = 5380) | Prevalence ratio (95% CI) |
|---|---|---|---|---|
| Total | 20 135 (100.0) | 73.3 | 26.7 | |
| Sex | ||||
| Male | 16 524 (82.1) | 74.4 | 25.6 | 1 [Reference] |
| Female | 3611 (17.9) | 68.1 | 31.9 | 1.25 (1.18-1.32) |
| Race and ethnicity | ||||
| Non-Hispanic White | 11 643 (57.8) | 78.7 | 21.3 | 1 [Reference] |
| Non-Hispanic Asian/Native Hawaiian/Other Pacific Islander | 764 (3.8) | 67.1 | 32.9 | 1.55 (1.38-1.73) |
| Non-Hispanic American Indian/Alaska Native | 110 (0.5) | 71.8 | 28.2 | 1.33 (0.97-1.82) |
| Non-Hispanic Black | 4312 (21.4) | 62.6 | 37.4 | 1.76 (1.67-1.86) |
| Hispanic | 2829 (14.1) | 68.1 | 31.9 | 1.50 (1.40-1.61) |
| Non-Hispanic multiple races/other | 479 (2.4) | 77.6 | 22.4 | 1.05 (0.88-1.26) |
| ADDM study year | ||||
| 2000 | 1246 (6.2) | 59.5 | 40.5 | 1 [Reference] |
| 2002 | 2366 (11.8) | 73.1 | 26.9 | 0.67 (0.60-0.74) |
| 2004 | 1151 (5.7) | 74.5 | 25.5 | 0.63 (0.55-0.72) |
| 2006 | 2286 (11.4) | 72.1 | 27.9 | 0.69 (0.62-0.76) |
| 2008 | 3216 (16.0) | 72.8 | 27.2 | 0.67 (0.61-0.74) |
| 2010 | 4975 (24.7) | 75.0 | 25.0 | 0.62 (0.57-0.68) |
| 2016 | 4895 (24.3) | 75.7 | 24.3 | 0.60 (0.55-0.66) |
| Site | ||||
| Colorado | 1130 (5.6) | 79.0 | 21.0 | 1 [Reference] |
| Utah | 683 (3.4) | 78.7 | 21.3 | 1.01 (0.83-1.23) |
| Maryland | 1722 (8.6) | 77.9 | 22.1 | 1.05 (0.90-1.23) |
| Minnesota | 313 (1.6) | 77.7 | 22.3 | 1.06 (0.83-1.35) |
| New Jersey | 2486 (12.3) | 76.8 | 23.2 | 1.10 (0.96-1.27) |
| Arizona | 2530 (12.6) | 75.4 | 24.6 | 1.17 (1.02-1.34) |
| Tennessee | 405 (2.0) | 74.8 | 25.2 | 1.20 (0.97-1.48) |
| North Carolina | 2209 (11.0) | 72.8 | 27.2 | 1.30 (1.13-1.49) |
| West Virginia | 257 (1.3) | 72.2 | 27.8 | 1.33 (1.03-1.70) |
| Wisconsin | 1702 (8.5) | 71.5 | 28.5 | 1.36 (1.17-1.57) |
| Arkansas | 1514 (7.5) | 70.5 | 29.5 | 1.41 (1.22-1.63) |
| Georgia | 3306 (16.4) | 70.2 | 29.8 | 1.42 (1.24-1.62) |
| Alabama | 678 (3.4) | 68.6 | 31.4 | 1.50 (1.26-1.77) |
| Florida | 327 (1.6) | 66.3 | 33.7 | 1.60 (1.31-1.97) |
| South Carolina | 873 (4.3) | 61.7 | 38.3 | 1.82 (1.57-2.12) |
| Associated behavioral and clinical features | ||||
| Self-injurious behaviors | ||||
| No | 14 491 (72.0) | 76.4 | 23.6 | 1 [Reference] |
| Yes | 5645 (28.0) | 65.2 | 34.8 | 1.48 (1.41-1.55) |
| Aggressive behaviors | ||||
| No | 9722 (48.3) | 73.8 | 26.2 | 1 [Reference] |
| Yes | 10 413 (51.7) | 72.8 | 27.2 | 1.04 (0.99-1.09) |
| Seizure or seizure-like behaviors | ||||
| No | 15 058 (74.8) | 75.3 | 24.7 | 1 [Reference] |
| Yes | 5077 (25.2) | 67.2 | 32.8 | 1.33 (1.26-1.40) |
| Adaptive functioning score | ||||
| ≤70 | 11 015 (54.7) | 61.2 | 38.8 | 1 [Reference] |
| 71-85 | 6155 (30.6) | 85.8 | 14.2 | 0.37 (0.34-0.40) |
| >85 | 2965 (14.7) | 92.0 | 8.0 | 0.21 (0.18-0.24) |
| Socioeconomic status e | ||||
| Education, tertile | ||||
| Lowest | 5259 (26.1) | 66.0 | 34.0 | 1 [Reference] |
| Middle | 7170 (35.6) | 73.0 | 27.0 | 0.79 (0.75-0.84) |
| Highest | 7705 (38.3) | 78.5 | 21.5 | 0.63 (0.60-0.67) |
| Poverty, tertile | ||||
| Highest | 5487 (27.3) | 65.9 | 34.1 | 1 [Reference] |
| Middle | 7071 (35.1) | 73.1 | 26.9 | 0.79 (0.75-0.84) |
| Lowest | 7578 (37.6) | 78.8 | 21.2 | 0.62 (0.58-0.66) |
| Median annual household income, tertile | ||||
| Lowest | 5365 (26.6) | 65.8 | 34.2 | 1 [Reference] |
| Middle | 6980 (34.7) | 72.6 | 27.4 | 0.80 (0.76-0.85) |
| Highest | 7790 (38.7) | 79.1 | 20.9 | 0.61 (0.57-0.65) |
| Maternal education status | ||||
| ≤High school diploma | 8711 (43.3) | 69.2 | 30.8 | 1 [Reference] |
| ≤Bachelor’s degree | 9106 (45.2) | 75.6 | 24.4 | 0.79 (0.75-0.84) |
| >Bachelor’s degree | 2319 (11.5) | 79.7 | 20.3 | 0.66 (0.59-0.74) |
| Birth characteristics | ||||
| Preterm f | ||||
| No | 16 986 (84.4) | 73.8 | 26.2 | 1 [Reference] |
| Yes | 3149 (15.6) | 70.7 | 29.3 | 1.12 (1.02-1.22) |
| Low birth weight g | ||||
| No | 17 730 (88.1) | 74.2 | 25.8 | 1 [Reference] |
| Yes | 2406 (11.9) | 66.5 | 33.5 | 1.30 (1.20-1.41) |
| Special education eligibility h | ||||
| Autism | 8452 (42.0) | 69.8 | 30.2 | 1 [Reference] |
| Developmental delay/preschool | 634 (3.1) | 74.1 | 25.9 | 0.86 (0.75-0.99) |
| Emotional disturbance | 502 (2.5) | 94.1 | 5.9 | 0.19 (0.14-0.28) |
| Hearing or visual impairments | 35 (0.2) | 63.4 | 36.6 | 1.21 (0.76-1.91) |
| Intellectual disability | 1025 (5.1) | 43.3 | 56.7 | 1.88 (1.76-2.00) |
| Multiple disabilities | 478 (2.4) | 50.6 | 49.4 | 1.63 (1.47-1.81) |
| Orthopedic impairments | 71 (0.4) | 79.0 | 21.0 | 0.69 (0.43-1.11) |
| Unknown/other i | 6739 (33.5) | 76.7 | 23.3 | 0.77 (0.73-0.82) |
| Other health impairments | 1271 (6.3) | 91.1 | 8.9 | 0.29 (0.25-0.35) |
| Specific learning disabilities | 916 (4.5) | 89.9 | 10.1 | 0.33 (0.27-0.41) |
| Traumatic brain injury | 12 (0.1) | 37.5 | 62.5 | 2.06 (1.30-3.28) |
Data source: Autism and Developmental Disabilities Monitoring (ADDM) Network. 8
Sample sizes may not sum to 20 135 because of rounding the average number in each group for the 20 imputed datasets.
Non–profound autism was defined as children with autism who did not meet the profound autism criteria.
Profound autism was defined as children with autism who were either nonverbal or minimally verbal or had an (intelligence quotient) IQ <50.
Socioeconomic status was based on census tract–level indicator rank values. Within each site, census tracts were ranked among all other census tracts in the study population and divided into tertiles, so an approximately equal proportion of the population was categorized into each tertile. The 3 socioeconomic indicators were (1) education: percentage of population aged ≥25 years with ≥high school diploma or General Educational Development (GED); (2) poverty: percentage of families with children aged <19 years living below the federal poverty level; and (3) median annual household income: percentile rank for census tract.
Born at <37 weeks gestation.
Born weighing <2500 g.
Special education categories were based on the most recent special education eligibility classification; if a child was served under >1 eligibility, the child would be classified as having “multiple disabilities.”
Other/unknown means either Individualized Educational Program eligibility information was not collected or the eligibility listed was not one of the choices.
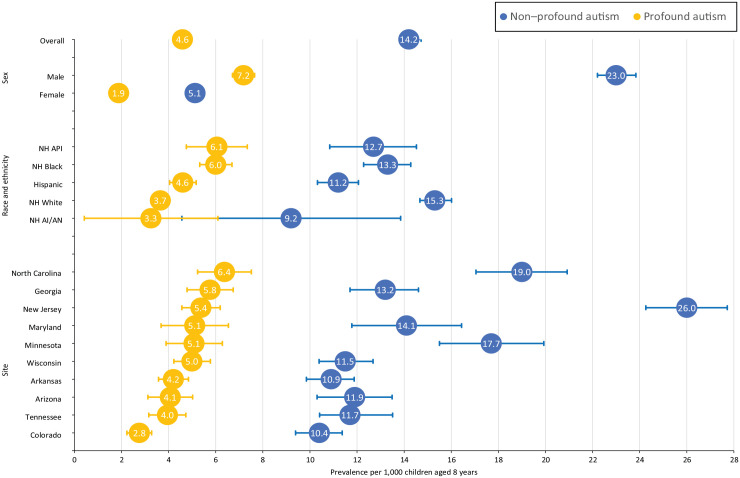
The prevalence of profound autism in 2016 was 4.59 (95% CI, 4.31-4.85) cases per 1000 8-year-old children (Figure 1 and Table 2) with a ratio of 3.1 non–profound autism cases for every 1 profound autism case. Prevalence estimates of profound autism per 1000 8-year-old children were highest among API (6.05; 95% CI, 4.75-7.34) and Black (6.00; 95% CI, 5.32-6.69) children and lowest among White children (3.65; 95% CI, 3.31-3.98). In contrast, White children had the highest prevalence of non–profound autism (15.34; 95% CI, 14.67-16.01) compared with all other racial and ethnic groups. The prevalence of profound autism varied by site, ranging from 2.76 (95% CI, 2.23-3.28) in Colorado to 6.37 (95% CI, 5.23-7.51) in North Carolina. New Jersey had the highest prevalence of non–profound autism (25.99; 95% CI, 24.26-27.72).
Figure 1.
Prevalence of profound and non–profound autism among children aged 8 years, by sex, race and ethnicity, and site, Autism and Developmental Disabilities Monitoring Network, 10 sites, United States, 2016. Error bars indicate 95% CIs. Data source: Autism and Developmental Disabilities Monitoring Network. 8 Abbreviations: AI/AN, American Indian/Alaska Native; API, Asian/Native Hawaiian/Other Pacific Islander; NH, non-Hispanic.
Table 2.
Prevalence of profound and non–profound autism among children aged 8 years, by sex, race and ethnicity, and site (N = 4895), ADDM Network, 10 sites, United States, 2016 a
| Characteristic | Profound autism | Non–profound autism | ||
|---|---|---|---|---|
| Prevalence b (95% CI) | Prevalence ratio (95% CI) | Prevalence b (95% CI) | Prevalence ratio (95% CI) | |
| Overall | 4.59 (4.31-4.85) | 14.26 (13.80-14.72) | ||
| Sex | ||||
| Female | 1.88 (1.62-2.13) | 1 [Reference] | 5.12 (4.72-5.52) | 1 [Reference] |
| Male | 7.18 (6.71-7.65) | 3.83 (3.30-4.44) | 23.03 (22.21-23.84) | 4.50 (4.13-4.90) |
| Race and ethnicity | ||||
| Non-Hispanic White | 3.65 (3.31-3.98) | 1 [Reference] | 15.34 (14.67-16.01) | 1 [Reference] |
| Non-Hispanic Asian/Native Hawaiian/Other Pacific Islander | 6.05 (4.75-7.34) | 1.66 (1.31-2.09) | 12.68 (10.84-14.52) | 0.83 (0.71-0.96) |
| Non-Hispanic American Indian/Alaska Native | 3.25 (0.42-6.09) | 0.89 (0.37-2.13) | 9.20 (4.56-13.85) | 0.60 (0.36-1.00) |
| Non-Hispanic Black | 6.00 (5.32-6.69) | 1.65 (1.42-1.91) | 13.28 (12.28-14.28) | 0.87 (0.79-0.94) |
| Hispanic | 4.60 (4.04-5.17) | 1.26 (1.08-1.47) | 11.19 (10.32-12.06) | 0.73 (0.67-0.80) |
| Site c | ||||
| Colorado | 2.76 (2.23-3.28) | 1 [Reference] | 10.38 (9.39-11.37) | 1 [Reference] |
| Tennessee | 3.95 (3.16-4.73) | 1.43 (1.09-1.88) | 11.73 (10.41-13.51) | 1.13 (0.98-1.31) |
| Arizona | 4.07 (3.12-5.02) | 1.48 (1.09-1.99) | 11.90 (10.30-13.49) | 1.15 (0.97-1.35) |
| Arkansas | 4.20 (3.57-4.84) | 1.52 (1.20-1.94) | 10.86 (9.85-11.88) | 1.05 (0.92-1.20) |
| Wisconsin | 4.99 (4.22-5.77) | 1.81 (1.42-2.31) | 11.53 (10.39-12.68) | 1.11 (0.97-1.27) |
| Minnesota | 5.08 (3.89-6.28) | 1.84 (1.36-2.50) | 17.72 (15.50-19.93) | 1.71 (1.46-2.00) |
| Maryland | 5.11 (3.68-6.54) | 1.85 (1.32-2.60) | 14.10 (11.78-16.44) | 1.36 (1.12-1.65) |
| New Jersey | 5.37 (4.56-6.19) | 1.95 (1.53-2.48) | 25.99 (24.26-27.72) | 2.50 (2.23-2.81) |
| Georgia | 5.76 (4.78-6.74) | 2.09 (1.62-2.69) | 13.15 (11.70-14.61) | 1.27 (1.10-1.47) |
| North Carolina | 6.37 (5.23-7.51) | 2.31 (1.78-3.00) | 18.98 (17.05-20.92) | 1.83 (1.59-2.10) |
Profound autism was defined as children with autism who were either nonverbal or minimally verbal or had an (intelligence quotient) IQ <50. Non–profound autism was defined as children with autism who did not meet the profound autism criteria. Data source: Autism and Developmental Disabilities Monitoring (ADDM) Network. 8
Prevalence per 1000 children aged 8 years.
Five sites did not participate and contribute data to the 2016 surveillance year and were excluded.
During 2000-2016, the prevalence of non–profound autism increased from 3.94 to 14.26 cases per 1000 children aged 8 years; the prevalence of profound autism increased from 2.68 to 4.59 cases per 1000 children aged 8 years (Figure 2).
Figure 2.
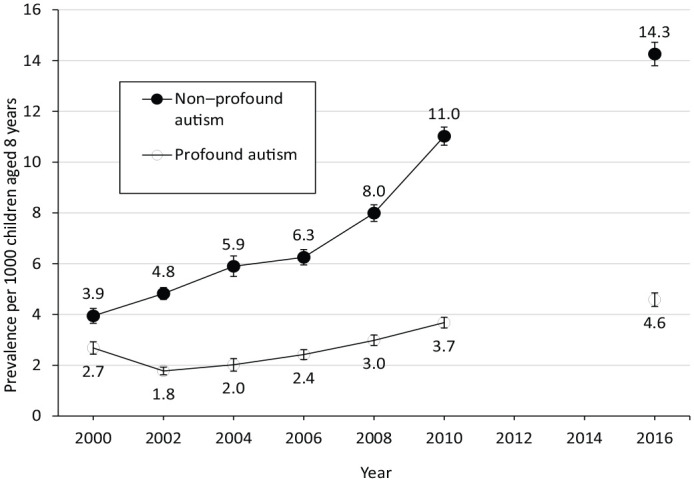
Prevalence of profound and non–profound autism among children aged 8 years, by year, Autism and Developmental Disabilities Monitoring Network, 15 sites, United States, 2016. Data from 2012 and 2014 were unavailable and were excluded from analyses. Error bars indicate 95% CIs. Data source: Autism and Developmental Disabilities Monitoring Network. 8
Profound autism was more common among girls than among boys (31.9% vs 25.6%; PR = 1.25; 95% CI, 1.18-1.32) (Table 1). Profound autism was also more common among Black (PR = 1.76; 95% CI, 1.67-1.86), API (PR = 1.55; 95% CI, 1.38-1.73), and Hispanic (PR = 1.50; 95% CI, 1.40-1.61) children than among White children. Apart from study year 2000, when the highest percentage of children with profound autism was observed (40.5%), the percentage of children with autism who had profound autism was similar across study years (2002-2016 range, 24.3%-27.9%). The lowest percentage of children with profound autism was observed in the most recently included study year, 2016 (24.3%). Sites varied in the percentage of their autism population who had profound autism, ranging from 21.0% in Colorado to 38.3% in South Carolina. Profound autism was more common among children who had documented self-injurious behaviors (PR = 1.48; 95% CI, 1.41-1.55) or seizure-like behaviors (PR = 1.33; 95% CI, 1.26-1.40) than among children without these behaviors. A higher percentage of children with an adaptive score ≤70 had profound autism (38.8%) than children with scores of 71-85 (14.2%) and >85 (8.0%). Lower community-level socioeconomic status and maternal education levels were associated with a higher percentage of profound autism. Children with autism who were born preterm or had a low birthweight were more likely to have profound autism than children with autism who were not born preterm (PR = 1.12; 95% CI, 1.02-1.22) or with a low birthweight (PR = 1.30; 95% CI, 1.20-1.41). The percentage of children with profound autism being served in an autism special education eligibility category was 30.2%. Among children with a known age of diagnosis (74.2% for profound autism and 65.5% for non–profound autism), the median (IQR) age of diagnosis was 46 (34-62) months among children with profound autism and 57 (38-76) months among children with non–profound autism.
Among children with profound autism, most met the case definition of profound autism through only 1 of the criteria: 42.7% had met only the IQ score <50 criterion and 38.1% met only the nonverbal/minimally verbal criterion; 19.3% met both criteria (Table 3). Most children with profound autism had aggressive behavior (52.7%) and an adaptive functioning score ≤70 (79.4%); 36.5% had self-injurious behavior, and 31.0% had seizures or seizure-like behaviors.
Table 3.
Characteristics of children aged 8 years with profound autism and non–profound autism among children with autism spectrum disorder (N = 20 135), ADDM Network, 15 sites, United States, 2000-2016 a
| Characteristic | Non–profound autism, no. b (%) (n = 14 755) | Profound autism, no. c (%) (n = 5380) |
|---|---|---|
| Profound autism case criteria | ||
| Intelligence quotient (IQ) <50 only | — | 2295 (42.7) |
| Nonverbal/minimally verbal only | — | 2049 (38.1) |
| IQ <50 AND nonverbal/minimally verbal | — | 1036 (19.3) |
| Associated behavioral and clinical features | ||
| Self-injurious behaviors | ||
| No | 11 077 (75.1) | 3414 (63.5) |
| Yes | 3678 (24.9) | 1966 (36.5) |
| Aggressive behaviors | ||
| No | 7178 (48.6) | 2546 (47.3) |
| Yes | 7577 (51.4) | 2834 (52.7) |
| Seizure or seizure-like behaviors | ||
| No | 11 343 (76.9) | 3715 (69.1) |
| Yes | 3412 (23.1) | 1665 (31.0) |
| Adaptive functioning score d | ||
| ≤70 | 6745 (45.7) | 4271 (79.4) |
| 71-85 | 5283 (35.8) | 871 (16.2) |
| >85 | 2727 (18.5) | 237 (4.4) |
Profound autism was defined as children with autism who were either nonverbal or minimally verbal or had an intelligence quotient (IQ) <50. Non–profound autism was defined as children with autism who did not meet the profound autism criteria. Data source: Autism and Developmental Disabilities Monitoring (ADDM) Network. 8
Sample sizes may not sum to 14 755 because of rounding the average number in each group for the 20 imputed datasets.
Sample sizes may not sum to 5380 because of rounding the average number in each group for the 20 imputed datasets.
Among those who met the definition of profound autism by verbal status alone (ie, IQ >50), 64% had an adaptive score of ≤70, 27% had an adaptive score of 71-85, and 9% had an adaptive score of >85.
Discussion
Among the 20 135 children aged 8 years with autism in the 2000-2016 surveillance years, approximately 27% overall met the case definition of profound autism. In 2016, the most recent surveillance year, the prevalence of profound autism was 1 in 218 children aged 8 years. To our knowledge, this study is the first US population-based study quantifying the prevalence and describing the characteristics of the population with profound autism. This analysis used data from a long-running surveillance system for autism in the United States, allowing profound autism to be quantified in a well-described cohort of school-aged children. It is important to identify these children because they are underrepresented in autism research and intervention studies and generally have the greatest need for services and supports.13,14 Children with profound autism may have considerable medical complexity and likely may not be able to live independently or perform tasks of daily living as they age.15,16 It is essential that policies, programs, and resources are tailored to the profound autism population across the life span to ensure their needs are met.17,18
While the prevalence of both profound and non–profound autism increased over time (2000-2016), the increase was greater for non–profound autism (from 1 in 254 to 1 in 70 children aged 8 years) than for profound autism (from 1 in 373 to 1 in 218 children aged 8 years); while attenuated, this trend remained when we used the 2002 study year as the starting reference point. This finding suggests that the composition of the identified autism population changed as the overall identified autism prevalence increased. 17 Because the profound autism population has lower proportional representation among all autism cases compared with earlier years, it is critical to support policy and programming that are focused on the unique support needs of people with profound autism.19-21
Variation across sites in the prevalence of autism per 1000 children aged 8 years in 2016 was greater for non–profound autism (site range, 10.4-26.0) than for profound autism (site range, 2.8-6.4). The difference in autism prevalence estimates by site within a study year could reflect geographic differences in identification and access to services, especially given the wide range of prevalence estimates of non–profound autism.
The overall Black to White PR of 1.0 in 2016 from a previously published report masks differences in prevalence by profound autism status. 8 The prevalence of profound autism among Black children was higher than among White children, while the prevalence of non–profound autism was higher among White children than among Black children. We found similar prevalence differences for the other racial and ethnic minority groups compared with White children. One possibility is that children of racial and ethnic minority groups with non–profound autism are less likely than White children with non–profound autism to be identified in the community. 22 The higher prevalence of profound autism in these racial and ethnic minority populations may also be due, in part, to a higher overall prevalence of intellectual disability compared with White children. 23 Additional research is needed to better understand the relationship of race and ethnicity and associated structural discrimination with profound autism status.
While boys were significantly more likely than girls to have autism, among autism cases, girls had 1.25 times the prevalence of profound autism as boys. This finding is consistent with preliminary characterization of the profound autism population. 6 One explanation for this finding is that girls with non–profound autism may be underidentified because they compensate more than boys for social deficits. 24 Alternatively, clinicians may be less likely to identify autism in girls than in boys because of differences by sex or gender in diagnostic procedures. 25 Genetic analyses have also shown a higher frequency of deleterious mutations among girls with autism compared with boys with autism, which could contribute to a higher prevalence of profound autism among girls than among boys. 26
The finding that self-injurious behavior was associated with profound autism is consistent with previous studies. 27 One explanation may be that this behavior is a form of communication when cognitive and communication functions are impaired. Aggression was not associated with profound autism, in contrast to previous findings that showed a relationship between aggression and lower cognitive and language measures. 28 Further research is needed to better understand clinical and behavioral characteristics among those with profound autism.
Limitations
This study had several limitations. First, ADDM Network sites changed across study years and may not be representative of their entire state or the United States, although they are representative of large, geographically defined populations and less subject to selection bias than clinical samples. Second, data on nonverbal status were not captured during the 2012 and 2014 study years, resulting in a gap in our longitudinal analytic data. Third, we used 48 months as a lower bound to assess nonverbal/minimally verbal status to allow time for verbal ability to develop, while balancing inclusion of an adequate number of years to capture more recent evaluations of verbal ability in surveillance records; children who were classified as nonverbal/minimally verbal may have become verbal at later ages. 29 In contrast, we classified children as verbal if they had no verbal ability information in their records, which might have led to underascertainment of nonverbal/minimally verbal status; furthermore, the ADDM case definition for nonverbal was stricter than the case definition for minimally verbal from other research.30,31 As is true for data from the entire ADDM Network, it may be harder to distinguish the presence of autism for children with lower IQ levels than for children with average or above-average IQ levels. 32 Next, 3 of the socioeconomic variables were based on census tract–level data versus family-level data and, thus, may not reflect the status of a child’s family; however, similar findings were observed for the single family-level socioeconomic variable (maternal education status). Lastly, the definition of profound autism originally defined by the Lancet Commission is relatively new, and additional studies are needed to further characterize this population and understand how profiles can inform decision-making for supports and services in addition to prognostic utility; with further exploration, the definition of profound autism may evolve.
Conclusions
Overall, more than one-quarter of 8-year-old children with autism met the criteria for profound autism. As the population of children with autism continues to change, describing and quantifying the profound autism population is critical for planning to ensure this group receives the services and supports needed during the life course and is appropriately represented in research and intervention studies. Further research on the barriers children with profound autism may face as they transition to adolescence and to adulthood will be important to ensure they are included in overall ASD services planning.
Supplemental Material
Supplemental material, sj-docx-1-phr-10.1177_00333549231163551 for The Prevalence and Characteristics of Children With Profound Autism, 15 Sites, United States, 2000-2016 by Michelle M. Hughes, Kelly A. Shaw, Monica DiRienzo, Maureen S. Durkin, Amy Esler, Jennifer Hall-Lande, Lisa Wiggins, Walter Zahorodny, Alison Singer and Matthew J. Maenner in Public Health Reports
Footnotes
Disclaimer: The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Centers for Disease Control and Prevention, National Center on Birth Defects and Developmental Disabilities (CDC-RFA-DD19-1901).
ORCID iDs: Michelle M. Hughes, PhD  https://orcid.org/0000-0002-4436-2236
https://orcid.org/0000-0002-4436-2236
Kelly A. Shaw, PhD  https://orcid.org/0000-0003-2964-8946
https://orcid.org/0000-0003-2964-8946
Supplemental Material: Supplemental material for this article is available online. The authors have provided these supplemental materials to give readers additional information about their work. These materials have not been edited or formatted by Public Health Reports’s scientific editors and, thus, may not conform to the guidelines of the AMA Manual of Style, 11th Edition.
References
- 1. Shaw KA, McArthur D, Hughes MM, et al. Progress and disparities in early identification of autism spectrum disorder: Autism and Developmental Disabilities Monitoring Network, 2002-2016. J Am Acad Child Adolesc Psychiatry. 2022;61(7):905-914. doi: 10.1016/j.jaac.2021.11.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. American Psychiatric Association; 2013. [Google Scholar]
- 3. Weitlauf AS, Gotham KO, Vehorn AC, Warren ZE. Brief report: DSM-5 “levels of support:” a comment on discrepant conceptualizations of severity in ASD. J Autism Dev Disord. 2014;44(2):471-476. doi: 10.1007/s10803-013-1882-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rosen NE, Lord C, Volkmar FR. The diagnosis of autism: from Kanner to DSM-III to DSM-5 and beyond. J Autism Dev Disord. 2021;51(12):4253-4270. doi: 10.1007/s10803-021-04904-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Singer A. “Profound autism” is the term we need to provide critical specificity to a broad spectrum. Autism Spectrum News. January 6, 2021. Accessed July 14, 2021. https://autismspectrumnews.org/profound-autism-is-the-term-we-need-to-provide-critical-specificity-to-a-broad-spectrum
- 6. Lord C, Charman T, Havdahl A, et al. The Lancet Commission on the future of care and clinical research in autism. Lancet. 2022;399(10321):271-334. doi: 10.1016/S0140-6736(21)01541-5 [DOI] [PubMed] [Google Scholar]
- 7. National Council on Severe Autism. Frequently asked questions. Accessed July 14, 2021. https://www.ncsautism.org/faqs
- 8. Maenner MJ, Shaw KA, Baio J, et al. Prevalence of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2016. MMWR Surveill Summ. 2020;69(4):1-12. doi: 10.15585/mmwr.ss6904a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Association; 2000. [Google Scholar]
- 10. National Center for Health Statistics. Vintage 2018 postcensal estimates of the resident population of the United States (April 1, 2010, July 1, 2010–July 1, 2018), by year, county, single-year of age (0, 1, 2, .., 85 years and over), bridged race, Hispanic origin, and sex. 2020. Prepared under a collaborative arrangement with the US Census Bureau. Accessed June 25, 2019. http://www.cdc.gov/nchs/nvss/bridged_race.htm [Google Scholar]
- 11. Lord C, Rutter M, DiLavore PC, Risi S, Gotham K, Bishop S. Autism Diagnostic Observation Schedule. 2nd ed (ADOS-2). Western Psychological Services; 2012. [Google Scholar]
- 12. van Buuren S, Groothuis-Oudshoorn K. Mice: multivariate imputation by chained equations in R. J Stat Softw. 2011;45(3):1-67. doi: 10.18637/jss.v045.i03 [DOI] [Google Scholar]
- 13. Russell G, Mandy W, Elliott D, White R, Pittwood T, Ford T. Selection bias on intellectual ability in autism research: a cross-sectional review and meta-analysis. Mol Autism. 2019;10:9. doi: 10.1186/s13229-019-0260-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Stedman A, Taylor B, Erard M, Peura C, Siegel M. Are children severely affected by autism spectrum disorder underrepresented in treatment studies? An analysis of the literature. J Autism Dev Disord. 2019;49(4):1378-1390. doi: 10.1007/s10803-018-3844-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Kirby AV, Baranek GT, Fox L. Longitudinal predictors of outcomes for adults with autism spectrum disorder. OTJR (Thorofare N J). 2016;36(2):55-64. doi: 10.1177/1539449216650182 [DOI] [PubMed] [Google Scholar]
- 16. Doshi-Velez F, Ge Y, Kohane I. Comorbidity clusters in autism spectrum disorders: an electronic health record time-series analysis. Pediatrics. 2014;133(1):e54-e63. doi: 10.1542/peds.2013-0819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ishler KJ, Biegel DE, Wang F, et al. Service use among transition-age youth with autism spectrum disorder. J Autism Dev Disord. 2022;52(3):1051-1065. doi: 10.1007/s10803-021-04999-6 [DOI] [PubMed] [Google Scholar]
- 18. Turcotte P, Mathew M, Shea LL, Brusilovskiy E, Nonnemacher SL. Service needs across the lifespan for individuals with autism. J Autism Dev Disord. 2016;46(7):2480-2489. doi: 10.1007/s10803-016-2787-4 [DOI] [PubMed] [Google Scholar]
- 19. Lundström S, Taylor M, Larsson H, Lichtenstein P, Kuja-Halkola R, Gillberg C. Perceived child impairment and the ‘autism epidemic’. J Child Psychol Psychiatry. 2022;63(5):591-598. doi: 10.1111/jcpp.13497 [DOI] [PubMed] [Google Scholar]
- 20. McCoy MS, Liu EY, Lutz ASF, Sisti D. Ethical advocacy across the autism spectrum: beyond partial representation. Am J Bioeth. 2020;20(4):13-24. doi: 10.1080/15265161.2020.1730482 [DOI] [PubMed] [Google Scholar]
- 21. Elster N, Parsi K. Like autism, representation falls on a spectrum. Am J Bioeth. 2020;20(4):4-5. doi: 10.1080/15265161.2020.1735871 [DOI] [PubMed] [Google Scholar]
- 22. Mandell DS, Wiggins LD, Carpenter LA, et al. Racial/ethnic disparities in the identification of children with autism spectrum disorders. Am J Public Health. 2009;99(3):493-498. doi: 10.2105/AJPH.2007.131243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Patrick ME, Shaw KA, Dietz PM, et al. Prevalence of intellectual disability among eight-year-old children from selected communities in the United States, 2014. Disabil Health J. 2021;14(2):101023. doi: 10.1016/j.dhjo.2020.101023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hull L, Petrides KV, Mandy W. The female autism phenotype and camouflaging: a narrative review. Rev J Autism Dev Disord. 2020;7(4):306-317. doi: 10.1007/s40489-020-00197-9 [DOI] [Google Scholar]
- 25. Ratto AB, Kenworthy L, Yerys BE, et al. What about the girls? Sex-based differences in autistic traits and adaptive skills. J Autism Dev Disord. 2018;48(5):1698-1711. doi: 10.1007/s10803-017-3413-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Jacquemont S, Coe BP, Hersch M, et al. A higher mutational burden in females supports a “female protective model” in neurodevelopmental disorders. Am J Hum Genet. 2014;94(3):415-425. doi: 10.1016/j.ajhg.2014.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Soke GN, Rosenberg SA, Hamman RF, et al. Brief report: prevalence of self-injurious behaviors among children with autism spectrum disorder—a population-based study. J Autism Dev Disord. 2016;46(11):3607-3614. doi: 10.1007/s10803-016-2879-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Dominick KC, Davis NO, Lainhart J, Tager-Flusberg H, Folstein S. Atypical behaviors in children with autism and children with a history of language impairment. Res Dev Disabil. 2007;28(2):145-162. doi: 10.1016/j.ridd.2006.02.003 [DOI] [PubMed] [Google Scholar]
- 29. Wodka EL, Mathy P, Kalb L. Predictors of phrase and fluent speech in children with autism and severe language delay. Pediatrics. 2013;131(4):e1128-e1134. doi: 10.1542/peds.2012-2221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Koegel LK, Bryan KM, Su PL, Vaidya M, Camarata S. Definitions of nonverbal and minimally verbal in research for autism: a sytematic review of the literature. J Autism Dev Disord. 2020;50(8):2957-2972. doi: 10.1007/s10803-020-04402-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Kasari C, Brady N, Lord C, Tager-Flusberg H. Assessing the minimally verbal school-aged child with autism spectrum disorder. Autism Res. 2013;6(6):479-493. doi: 10.1002/aur.1334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Thurm A, Farmer C, Salzman E, Lord C, Bishop S. State of the field: differentiating intellectual disability from autism spectrum disorder. Front Psychiatry. 2019;10:526. doi: 10.3389/fpsyt.2019.00526 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-phr-10.1177_00333549231163551 for The Prevalence and Characteristics of Children With Profound Autism, 15 Sites, United States, 2000-2016 by Michelle M. Hughes, Kelly A. Shaw, Monica DiRienzo, Maureen S. Durkin, Amy Esler, Jennifer Hall-Lande, Lisa Wiggins, Walter Zahorodny, Alison Singer and Matthew J. Maenner in Public Health Reports