Abstract
Background
Immune checkpoint inhibitors (ICI) substantially improve outcome for patients with cancer. However, the majority of patients develops immune-related adverse events (irAEs), which can be persistent and significantly reduce quality of life. Neurological irAEs occur in 1–5% of patients and can induce severe, permanent sequelae or even be fatal. In order to improve the diagnosis and treatment of neurological irAEs and to better understand their pathogenesis, we assessed whether previous neurotropic infections are associated with neurological irAEs.
Methods
Neurotropic infections that might predispose to ICI-induced neurological irAEs were analyzed in 61 melanoma patients from 3 countries, the Netherlands, Australia and Germany, including 24 patients with neurotoxicity and 37 control patients. In total, 14 viral, 6 bacterial, and 1 protozoal infections previously reported to trigger neurological pathologies were assessed using routine serology testing. The Dutch and Australian cohorts (NL) included pre-treatment plasma samples of patients treated with neoadjuvant ICI therapy (OpACIN-neo and PRADO trials; NCT02977052). In the Dutch/Australian cohort a total of 11 patients with neurological irAEs were compared to 27 control patients (patients without neurological irAEs). The German cohort (LMU) consisted of serum samples of 13 patients with neurological irAE and 10 control patients without any documented irAE under ICI therapy.
Results
The association of neurological irAEs with 21 possible preceding infections was assessed by measuring specific antibodies against investigated agents. The seroprevalence of all the tested viral (cytomegalovirus, Epstein-Barr-Virus, varicella-zoster virus, measles, rubella, influenza A and B, human herpes virus 6 and 7, herpes simplex virus 1 and 2, parvovirus B19, hepatitis A and E and human T-lymphotropic virus type 1 and 2), bacterial (Borrelia burgdorferi sensu lato, Campylobacter jejuni, Mycoplasma pneumoniae, Coxiella burnetti, Helicobacter pylori, Yersinia enterocolitica and Y. pseudotuberculosis) and protozoal (Toxoplasma gondii) infections was similar for patients who developed neurological irAEs as compared to control patients. Thus, the analysis provided no evidence for an association of described agents tested for seroprevalence with ICI induced neurotoxicity.
Conclusion
Previous viral, bacterial and protozoal neurotropic infections appear not to be associated with the development of neurological irAEs in melanoma patients who underwent therapy with ICI across 3 countries. Further efforts are needed to unravel the factors underlying neurological irAEs in order to identify risk factors for these toxicities, especially with the increasing use of ICI in earlier stage disease.
Keywords: Checkpoint-inhibitor, Side effect, Serology, Melanoma
Introduction
Immune checkpoint inhibitors (ICI) have proven efficacy across multiple malignancies, significantly improving outcomes for many cancer patients [1]. As immune checkpoints are involved in self-tolerance and limiting of autoimmunity, ICI therapy can induce immune-related adverse events (irAEs) mimicking autoimmune disease. Severe irAEs, classified as grade 3–5 according to the Common Terminology Criteria for Adverse events (CTCAE), can be observed in 20–59% of patients [2]. Although any organ system can be affected, neurological toxicities are highly relevant irAEs due to their morbidity and mortality as well as permanent consequences. Neurological irAEs are observed in 1–5% [2] of patients, and can involve the central (CNS) as well as the peripheral nervous system (PNS) and the neuromuscular junction [3–7].
Reported neurological irAEs include immune neuropathies, like de novo manifestations or exacerbations of pre-existing immune-mediated neurological diseases such as Guillain–Barré like syndrome (GBS) [5], demyelinating polyneuropathy [4], enteric neuropathy [5], myasthenia gravis (MG) [5, 6, 8], multiple sclerosis (MS), or (vasculitic) neuropathies [9], but also posterior reversible encephalopathy syndrome, aseptic meningitis, (transverse) myelitis, and immune encephalitis [4, 5, 10]. Furthermore, cranial nerve involvement of optical and vestibulocochlear nerve can lead to vision impairment, hearing loss and vertigo [11]. Persistent irAEs after cessation of ICI therapy have been shown to severely reduce quality of life for cancer survivors [12], thus it would be of utmost importance to detect patients with a high risk of therapy-induced sequelae before starting ICI [13]. Additionally, since ICI are applied in earlier tumor stages, there is a dire need to carefully weigh risks and benefits [14]. So far the efforts to identify predictive markers for severe or life-threatening irAEs have been less fruitful than anticipated [15]. For neurological side effects this attempt is especially pressing since they are associated with a mortality rate of up to 21% [4], often require intensive care with e.g. in 27–37% of cases of ICI-induced encephalitis [10], and result in permanent sequelae in 11% of cases [4].
ICI-induced neurological irAEs behave differently from their autoimmune counterparts with a lower frequency of autoantibodies [7, 16], and different response to therapy. However, both conditions can be triggered by distinct organ-specific antigens. Peripheral neuropathies can be caused by immunological cross-reactivity in which an immune response to an environmental agent (e.g. infectious agent or vaccine) targets self-antigens from the nervous system [17, 18]. Even though the research field is hampered by latency, unknown interactions with the microbiota, and other environmental factors, molecular mimicry can play a role in autoimmune reactions [19]. GBS has been linked to autoantibody production after Campylobacter jejuni infection via molecular mimicry [17, 18]. In analogy to these autoimmune diseases, preceding infections could predispose to ICI-induced toxicity, especially neurological irAEs potentially associated with infectious agents reported to be causative for autoimmune neurological diseases [4, 18, 19]. Activation or re-activation of such previous immune responses by ICI therapy might trigger neurological irAEs by molecular mimicry.
Therefore, we tested whether exposure to a neurotropic infection is associated with the development of an ICI induced neurological irAE. This study analyzed 61 cancer patients for serological evidence of 21 infectious agents and their possible association with the occurrence of neurological irAE following ICI.
Methods
Patient population
Plasma and serum samples of patients treated with ICI were identified from three cancer centers (Netherlands Cancer Institute (NKI), Melanoma Institute Australia (MIA) and Ludwig–Maximilians-University (LMU), Germany) (Fig. 1). This cohort included pre-treatment plasma samples of patients of the OpACIN-neo (n = 32) and PRADO trials (n = 6; NCT02977052) and serum samples of the LMU (n = 23).
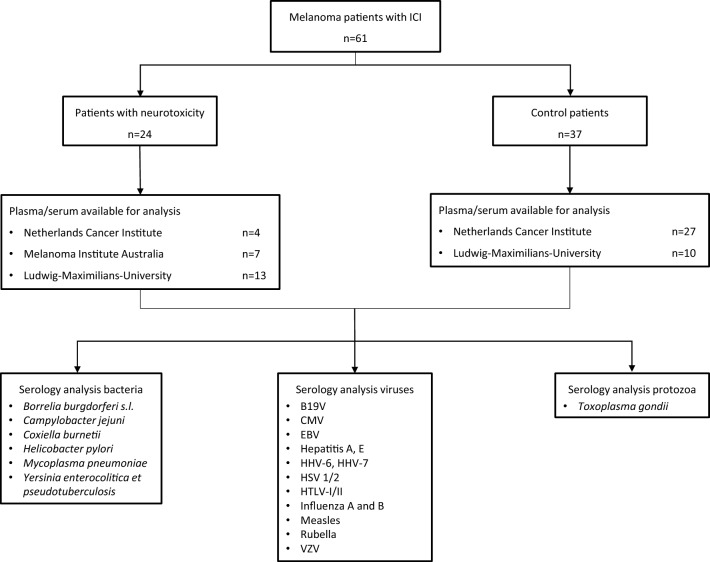
Fig. 1.
Study overview. Analysis of melanoma patients treated with immune checkpoint inhibitor (ICI) (n = 61). The samples of the Netherlands Cancer Institute (NKI) and Melanoma Institute Australia (MIA) were plasma samples (NL) and the samples of the Ludwig–Maximilians University (LMU) were serum samples. A total of 24 patients with neurological irAEs was compared to 37 patients without neurotoxicity. Patients mainly received ipilimumab plus nivolumab combination therapy (all NL, part of LMU), and the percentage receiving monotherapy and combination therapy was balanced (Table 2). Abbreviations: sensu lato (s.l.), parvovirus B19 (B19V), cytomegalovirus (CMV), Epstein-Barr virus (EBV), human herpesvirus (HHV), herpes simplex virus (HSV), human T-lymphotropic virus (HTLV), varicella-zoster virus (VZV)
In the OpACIN-neo and PRADO trials (NCT02977052), summarized as Dutch cohort (NL), melanoma patients were treated with different doses of neoadjuvant ipilimumab and nivolumab [20–22]. At baseline all 38 patients were stage III according to AJCC 2017. Out of this cohort, 11 patients developed neurological irAEs, ranging from grade 1 to 5 CTCAE (Table 1). Patients treated at the NKI within the OpACIN-neo trial who did not experience neurological irAEs were selected as control cohort (n = 27). The NL control cohort included patients who experienced other types of irAEs such as gastrointestinal irAEs, irArthritis, irHepatitis or irDermatitis, of which 10 demonstrated CTCAE grade 3 or 4 irAEs.
Table 1.
Methods of investigated infectiological agents
| Infectiological agents | Method | Details [unit] | Cut-off range |
|---|---|---|---|
| Virological agents | |||
| CMV IgG | CLIA | Quantitative [U/ml] | 12–14 |
| EBV-EA IgG | CLIA | Quantitative [U/ml] | 10–40 |
| EBV-EBNA IgG | 20–40 | ||
| EBV-VCA IgG | 20 | ||
| Hepatitis A IgG | CMIA | Semiquantitative | 0.8–1.1 |
| Hepatitis E IgG |
ELISA and CLIA |
Semiquantitative Quantitative [AU/ml] |
0.8–1.1 |
| HHV-6 IgG | ELISA | Semiquantitative | 0.9–1.1 |
| HHV-7 IgG | IFT | Semiquantitative | 1:8 |
| HSV 1/2 IgG | CMIA | Semiquantitative | 0.9–1.1 |
| HTLV-I/II IgG | CMIA | Semiquantitative | 1 |
| Influenza A IgG | ELISA | Semiquantitative | 0.8–1.1 |
| Influenza B IgG | ELISA | Semiquantitative | 0.8–1.1 |
| Measles IgG | CLIA | Quantitative [AU/ml] | 13.5–16.5 |
| B19V IgG | CLIA | Semiquantitative | 0.9–1.1 |
| Rubella IgG | CLIA | Quantitative [IU/ml] | 7–10 |
| VZV IgG | CLIA | Quantitative [mIU/ml] | 50–100 |
| Bacteriological and protozoal agents | |||
| Coxiella burnetii IgG | CLIA | Semiquantitative | 0.9–1.1 |
| Coxiella burnetii IgM | 0.9–1.1 | ||
| Borrelia burgdorferi s.l. IgG | ELISA | Quantitative [AU/ml] | 16–22 |
| Borrelia burgdorferi s.l. IgM | 16–22 | ||
| Campylobacter jejuni IgG | ELISA | Quantitative [AU/ml] | 16–22 |
| Campylobacter jejuni IgA | Semiquantitative | 0.8–1.1 | |
| Helicobacter pylori IgG | ELISA | Semiquantitative | 0.8–1.1 |
| Helicobacter pylori IgA | 0.8–1.1 | ||
| Mycoplasma pneumoniae IgG | ELISA | Quantitative [AU/ml] | 16–22 |
| Mycoplasma pneumoniae IgA | Semiquantitative | 0.8–1.1 | |
| Mycoplasma pneumoniae IgM | Semiquantitative | 0.8–1.1 | |
| Toxoplasma gondii IgG | ELISA | Quantitative [IU/ml] | 8–11 |
| Toxoplasma gondii IgM | Semiquantitative | 0.8–1.1 | |
| Yersinia p.e. IgG | Immunoblot | Qualitative | – |
| Yersinia p.e. IgA | |||
| Yersinia p.e. IgM | |||
Virological and bacteriological/protozoal agents are given in alphabetical order. Virological agents: Immunoglobulin G (IgG) antibodies measured using chemiluminescent immunoassay (CLIA) are indicated in arbitrary units per milliliter [AU/ml] as well as international units per milliliter [IU/ml] and units per milliliter [U/ml]. HHV-7 was detected by indirect immunofluorescence technique (IFT), classified as negative if the titer was below 1:8.Other methods: enzyme-linked immunosorbent assay (ELISA) and chemiluminescence microparticle immunoassay (CMIA). Bacteriological and protozoal agents: Immunoglobulins A, G, M (IgA, IgG, IgM) were semiquantitatively and quantitatively measured using CLIA and ELISA. Immunoglobulins against Yersinia enterocolitica and pseudotuberculosis (Yersinia p.e.) were detected by immunoblot, in which case they were only either detected or not detected (positive/negative). Anti-phase-II-Coxiella burnetii immunoglobulins were measured, testing for phase-II-antigen, which is more likely in an acute than in a chronic infection. Cut-off range: values in the displayed range were classified as inconclusive, seroprevalence below and above cut-off points was considered as negative and positive. If only one cut-off point is displayed, values below were classified as negative
The LMU cohort consisted of 23 melanoma patients receiving ipilimumab plus nivolumab or ICI monotherapy (nivolumab, pembrolizumab or ipilimumab) including longitudinal blood samples (Table 2). Out of these, 13 patients developed neurological irAEs and 10 served as control patients. 30 samples were collected for the irAE group, including 6 baseline (bl), 12 under ICI therapy (cxp) and 12 at the time of the adverse event (ae). Either cxp or ae or both were at least obtained from every irAE patient. The LMU control cohort included 10 patients who did not develop any kind of irAE, with one sample per patient, split into 1 at bl and 9 at cxp time point. Due to differing serum volumes for each timepoint, some parameters could not be measured in all samples.
Table 2.
Baseline characteristics of study cohort treated with ICI
| Baseline characteristics | Control cohort | Neurological irAE | Total cohort | |||
|---|---|---|---|---|---|---|
| NL | LMU | NL | LMU | irAE | Control | |
| n | 27 | 10 | 11 | 13 | 24 | 37 |
| Age (years) | 53 (27–78) | 69 (31–80) | 58 (24–70) | 58 (42–74) | 58 (24–74) | 57 (27–80) |
| Gender: female—male: n (%) | 13—14 (48%—52%) | 2—8 (20%—80%) | 8—3 (73%—27%) | 6—7 (46%—54%) | 14—10 (58%—42%) | 15—22 (41%—59%) |
| Primary tumor stage | ||||||
| T1a/b | 8 (30%) | 0 (0%) | 4 (36%) | 2 (15%) | 6 (25%) | 8 (22%) |
| T2a/b | 4 (15%) | 3 (30%) | 0 (0%) | 1 (8%) | 1 (4%) | 7 (19%) |
| T3a/b | 5 (19%) | 2 (20%) | 2 (18%) | 1 (8%) | 3 (12%) | 7 (19%) |
| T4a/b | 2 (7%) | 1 (10%) | 2 (18%) | 4 (31%) | 6 (25%) | 3 (8%) |
| Tx | 8 (30%) | 0 (0%) | 1 (9%) | 2 (15%) | 3 (12%) | 8 (22%) |
| Unknown primary | 0 (0%) | 4 (40%) | 2 (18%) | 3 (23%) | 5 (21%) | 4 (11%) |
| Primary AJCC stage | ||||||
| I | 0 (0%) | 1 (10%) | 0 (0%) | 1 (8%) | 1 (4%) | 1 (3%) |
| II | 0 (0%) | 3 (30%) | 0 (0%) | 1 (8%) | 1 (4%) | 3 (8%) |
| III B/C | 27 (100%) | 2 (20%) | 11 (100%) | 1 (8%) | 12 (50%) | 29 (78%) |
| IV | 0 (0%) | 4 (40%) | 0 (0%) | 10 (77%) | 10 (42%) | 4 (11%) |
| Therapy regimen ICI | ||||||
| Pembrolizumab/Nivolumab | 0 (0%) | 6 (60%) | 0 (0%) | 2 (15%) | 2 (8%) | 6 (16%) |
| Ipilimumab | 0 (0%) | 0 (0%) | 0 (0%) | 3 (23%) | 3 (12%) | 0 (0%) |
| Ipilimumab + Nivolumab | 27 (100%) | 4 (40%) | 11 (100%) | 8 (62%) | 19 (79%) | 31 (84%) |
| Prior therapy | ||||||
| Chemotherapy | 0 (0%) | 0 (0%) | 0 (0%) | 5 (38%) | 5 (21%) | 0 (0%) |
| Radiotherapy | 0 (0%) | 1 (10%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (3%) |
| IFN-α | 0 (0%) | 1 (10%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (3%) |
| BRAF-/MEK-inhibitor | 0 (0%) | 0 (0%) | 0 (0%) | 5 (38%) | 5 (21%) | 0 (0%) |
Percentages may not sum up to 100 due to rounding. Age: median displayed with range in brackets. NL cohort included OpACIN-neo and PRADO trial patients from the Netherlands and Australia, LMU included German patients from the MelAutim study. Primary AJCC 2017 stage and prior therapy before initiation of ICI displayed
Clinical data was obtained from eCRFs and electronic patients files. Ethical consent was obtained within the OpACIN-neo and PRADO studies (NL) and the MelAutim study (LMU) (No. 20-1122) from the respective institutional review boards. Patients gave written informed consent before inclusion. Adverse events were graded using CTCAE version 5.0 [23].
Infectiological analyses
A total of 14 viral, 6 bacteriological and one protozoal agents was investigated for seroprevalence. Due to different available sample volumes for each patient, a priorization was established, taking different variables into account such as needed amount of volume and interest in the parameter. For this reason, the numbers of investigated samples slightly vary for single parameters. Selected infections were based on possible associations with neurologic symptoms. Previously described associations with ICI were also taken into account, such as human T-lymphotropic virus (HTLV) [24], Helicobacter pylori [25], Toxoplasma gondii [26], influenza [27], cytomegalovirus (CMV) [28], Campylobacter jejuni [29] or Epstein–Barr virus (EBV) [30] to finally come up with the curated list of interest of potentially neurotropic infectious agents.
Viral serology
Seroprevalence was assessed using chemiluminescent immunoassay (CLIA), chemiluminescence microparticle immunoassay (CMIA), enzyme-linked immunosorbent assay (ELISA) and indirect immunofluorescence technique (IFT). These assays provide quantitative or semiquantitative readouts, respectively (Table 1).
Antibodies against CMV, EBV, measles, parvovirus B19 (B19V), rubella and varicella-zoster virus (VZV) were measured using CLIA. For EBV, three different parameters were measured including antibodies against early antigen (EA), Epstein-Barr nuclear antigen (EBNA) and viral capsid antigen (VCA), respectively, each related to a different stage of this viral infection. Specific antibodies against hepatitis A, herpes simplex virus (HSV 1/2), as well as HTLV type I/II were detected using CMIA, whereas antibodies against hepatitis E, human herpesvirus 6 (HHV-6), influenza A and B were quantified using ELISA. Measurement of hepatitis E-antibodies was first performed using ELISA but was switched to CLIA. Lastly, IFT was applied to measure antibodies against human herpesvirus 7 (HHV-7).
Bacterial and protozoal serology
For investigated bacterial and protozoal agents, quantitative, semiquantitative and qualitative methods were applied, using ELISA, CLIA and immunoblotting (Table 1). In comparison to the viral serology, where only IgG's were quantified, bacteriological agents were additionally measured as IgM and/ or IgA. Antibodies against phase-II-antigens of Coxiella burnetii were investigated using CLIA, antibodies against Yersinia enterocolitica and Y. pseudotuberculosis (summarized as Yersinia p.e.) by using immunoblotting, whereas the other parameters were measured by ELISA (Borrelia burgdorferi sensu lato (s.l.), Campylobacter jejuni, Helicobacter pylori, Mycoplasma pneumoniae and the protozoa Toxoplasma gondii).
Statistical analysis
The NL cohort and the LMU cohort were analyzed separately as well as combined, considering possible differences such as center effects. Analyses were performed using GraphPad Prism 9.3.1 (GraphPad Software, Inc. San Diego, California, USA), graphs were generated using GraphPad Prism 9.3.1 and Microsoft PowerPoint 2016. Comparisons were made using Mann–Whitney-U-tests and/or Kruskal–Wallis-tests with a significance level of p ≤ 0.05.
For all measured parameters, the neurotoxicity group was compared to the control group. Additionally, since irHypophysitis has been classified as neurological or endocrine irAE, cases of the neurotoxicity group with irHypophysitis were analyzed separately in comparison to the control group to unravel possible effects of this type of irAE on the results. The quantitative parameters were visualized as scatter dot plots, displayed with median and 95% confidence intervals (CI). Semiquantitative and qualitative parameters were visualized as stacked bar graphs.
Results
Patient population
Melanoma patients receiving ICI therapy were included for seroprevalence analyses of 21 bacterial, viral and protozoal agents described in the context of neurological pathologies (Table 1). Samples were collected from three different countries (Netherlands, Australia, Germany) with plasma samples before initiation of ICI therapy in the trial patients (NL) or serum samples of at least one of three possible time points in patients treated in Germany (LMU).
In the NL cohort 11 patients reported neurological irAEs (Table 2), such as meningitis, encephalitis, transverse myelitis, ataxia and different neuropathies, including a bilateral ulnar neuropathy, autonomic neuropathy (gastroparesis), bilateral Bell's palsy, and polyradiculoneuropathy (Table 3). The control cohort consisted of 27 patients without neurological irAEs. All included NL patients received neoadjuvant ipilimumab plus nivolumab without any prior systemic therapy or radiotherapy.
Table 3.
Neurological adverse events in investigated cohorts of melanoma patients under ICI treatment
| Neurological irAE | NL | LMU | Total cohort | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | 11 patients, 12 diagnoses | 13 patients, 14 diagnoses | 24 patients, 26 diagnoses | ||||||||||
| CTCAE grade | 1–2 | 3 | 4 | 5 | 1–2 | 3 | 4–5 | Unknown | 1–2 | 3 | 4 | 5 | Unknown |
| n (%) | 4 (33) | 6 (50) | 1 (8.3) | 1 (8.3) | 5 (36) | 8 (57) | 0 (0) | 1 (7) | 9 (35) | 14 (54) | 1 (4) | 1 (4) | 1 (4) |
| Ataxia | 1 | 1 | |||||||||||
| Bell’s palsy | 1 | 1 | |||||||||||
| Encephalitis | 1 | 1 | 1 | 1 | |||||||||
| Gastroparesis | 1 | 1 | |||||||||||
| Hypophysitis | 5 | 4 | 1 | 5 | 4 | 1 | |||||||
| Meningitis | 1 | 2 | 1 | 2 | |||||||||
| Myelitis | 1 | 1 | |||||||||||
| Neuritis* | 1 | 1 | |||||||||||
| Neuropathy | 1 | 1 | 1 | 1 | 1 | 1 | |||||||
| Radiculitis | 1 | 1 | |||||||||||
| Transverse myelitis-like syndrome | 1 | 1 | |||||||||||
| Vestibulopathy | 1 | 1 | |||||||||||
Numbers of cases displayed (percentages in brackets). Alphabetical order of neurological irAEs. In our case the specific differentiation of ataxia as a symptom for i.e. polyneuropathy was not possible. Percentages may not sum up to 100 due to rounding. *Neuritis case could potentially have polyneuropathy, whereas neuritis was more probable. One patient in each cohort appears twice because of two leading diagnoses of one patient. Common Terminology Criteria for Adverse events (CTCAE v 5.0) used for grading of irAEs
LMU patients received ICI combination therapy with ipilimumab plus nivolumab (62% of irAE group, 40% of controls) or ICI monotherapy with pembrolizumab, nivolumab or ipilimumab (38% or irAE, 60% of control group) (Table 2).
The LMU cohort contained 13 patients with neurological irAEs such as neuritis, myelitis, encephalitis or vestibulopathy (Table 3). Of these, 10 patients had received a prior systemic therapy with chemotherapy (38%) or BRAF-/MEK-inhibitors before initiation of ICI (38%). The LMU control group included 10 patients who received ICI therapy but did not develop any kind of irAE (Table 2). A part of these had received radiotherapy (10%) or interferon (IFN)-alpha therapy (10%) before ICI. For further details of patients’ characteristics, see Tables 2 and 3.
Virological results
Quantitative parameters
Seroprevalence of viral pathogens described to potentially induce neurological pathologies were investigated for the cohorts of melanoma patients under ICI (Table 1). Samples were analyzed for the quantitative measurement of antibodies against cytomegalovirus (CMV), Epstein-Barr-virus (EBV), varicella-zoster virus (VZV), measles virus and rubella virus (Fig. 2).
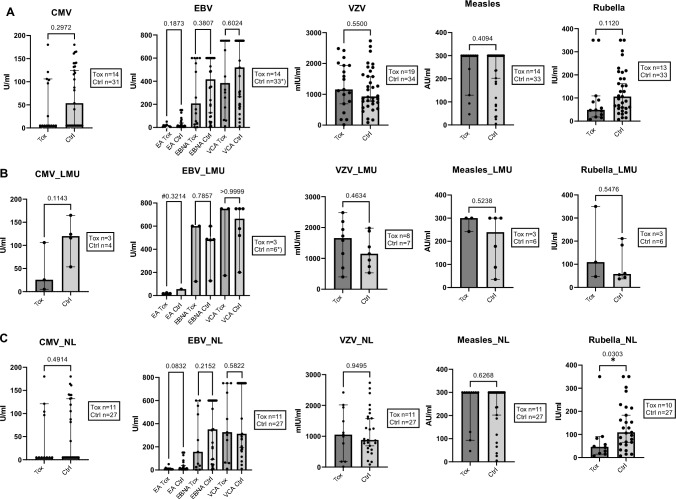
Fig. 2.
No association of quantitative agents for viral infections with neurological irAEs compared to controls without neurological irAE. Melanoma patients treated with ICI with (Tox) and without (Ctrl) neurological irAEs. Values of IgG antibodies against each virus measured. Combined (A) and separate analyses of LMU (B) and NL (C) cohorts. EBV *): differing n of Ctrl, (A) Ctrl n = 28 for EA, n = 32 for EBNA, n = 33 for VCA; (B) EBNA Ctrl n = 5. (C) Rubella virus antibodies statistically significant in NL cohort, Ctrl > Tox, p = 0.0303. (B) EBV EA #: no value comparison possible (Tox n = 3, Ctrl n = 1), p of pos/neg comparison displayed with Tox n = 3 and Ctrl n = 6. (A) CMV: In the Tox group 8/14 (57%) (1 from LMU (B) and 7 from NL (C)) were classified negative, in the Ctrl group this was the case for 14/31 (45%) (all NL (C)) cases. P values displayed. Boxes show the numbers of measured samples for each agent. Control group consisted of patients without neurological irAEs (NL) and of patients without any ICI-induced irAE (LMU). Mann–Whitney-U tests. Median with 95% CI displayed. For reference cut-off points see Table 1. Serum (LMU, B) and plasma (NL, C) analyses
For EBV, antibodies against early antigen (EA), Epstein-Barr-nuclear antigen (EBNA) and viral capsid antigen (VCA) were measured. For described quantitative viral agents, patients who developed neurological irAEs after initiation of ICI therapy (Tox) did not have significantly higher specific IgG levels compared to the control cohorts (Ctrl), considering combined (Fig. 2A) and separate analyses of the LMU (Fig. 2B) and NL cohort (Fig. 2C). Investigating the NL cohorts separately, significantly higher specific IgG levels of antibodies against rubella virus were found in the control group compared to patients that developed neurological irAEs (Fig. 2C).
In addition, irHypophysitis was analyzed separately for VZV (LMU), in comparison to other neurological irAEs and controls (Kruskal–Wallis-test). There was no significant difference for VZV (p = 0.4407). No irHypophysitis only case was included in other quantitative viral measurements due to priorization and available amounts of volume.
Semiquantitative parameters
In addition to quantitative parameters, we determined antibodies against virological parameters semiquantitatively, against influenza A and B, HHV6 and HHV7, HSV 1/2, B19V, hepatitis A and E and HLTV-I/II (Fig. 3A–C).
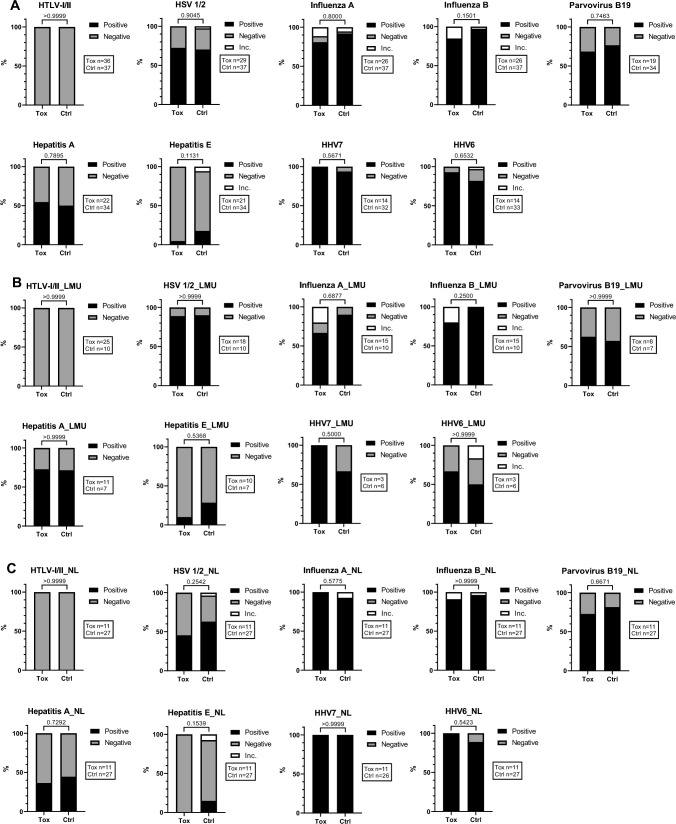
Fig. 3.
Semiquantitative virological agents are not associated with neurological irAEs. Melanoma patients treated with ICI with (Tox) and without (Ctrl) neurological irAEs. Combined (A) and separate analyses of LMU (B) and NL (C) cohorts. Evaluation of positive, negative or inconclusive (Inc.) values for each semiquantitative parameter. P values displayed. Boxes show the number of measured samples for each agent. Control group consisted of patients without neurological irAEs (NL) and of patients without any ICI-induced irAEs (LMU). Mann–Whitney-U tests. For reference cut-off points see Table 1. Serum (LMU) and plasma (NL) analyses compared
The majority of patients tested positive for influenza A and B viruses, HSV 1/2, HHV6, HHV7 and B19V, whereas most tested negative for hepatitis E and all patients tested negative for HLTV-I/II.
There was no significant association between these semiquantitative virological agents and neurological irAEs when comparing to the control patients, in combined (Fig. 3A) as well as separate analyses of the cohorts (Fig. 3B, C).
As described for the quantitative viral parameters, no significant difference was observed comparing irHypophysitis cases to other neurological irAEs and to the controls (LMU), conducted for the semiquantitative virological parameters HSV 1/2 (p = 0.4066), influenza virus A (p = 0.4204) and B (p = 0.1699), B19V (p > 0.9999) as well as for hepatitis virus A (p = 0.2386) and E (p = 0.7838). Also for other semiquantitative virological parameters, no irHypophysitis case was measured (HHV6 and 7) or all investigated samples were negative (HTLV-I/II).
The data implicate that there is no association between the tested quantitatively and semiquantitatively assessed virus-specific antibodies (Table 1) and the development of neurological irAEs under ICI therapy in our cohorts (Figs. 2 and 3).
Bacteriological and protozoan results
Quantitative parameters
Melanoma patients treated with ICI were analyzed for neurotropic infections with several bacterial and protozoal pathogens (Table 1). Antibodies against Toxoplasma gondii (IgG), Borrelia burgdorferi s.l. (IgG and IgM), Campylobacter jejuni (IgG) and Mycoplasma pneumoniae (IgG) were determined by quantitative assays (Fig. 4). Samples were either pre-treatment plasma samples (NL) or serum samples (LMU), analyzed combined (Fig. 4A) and separately (Fig. 4B, C).
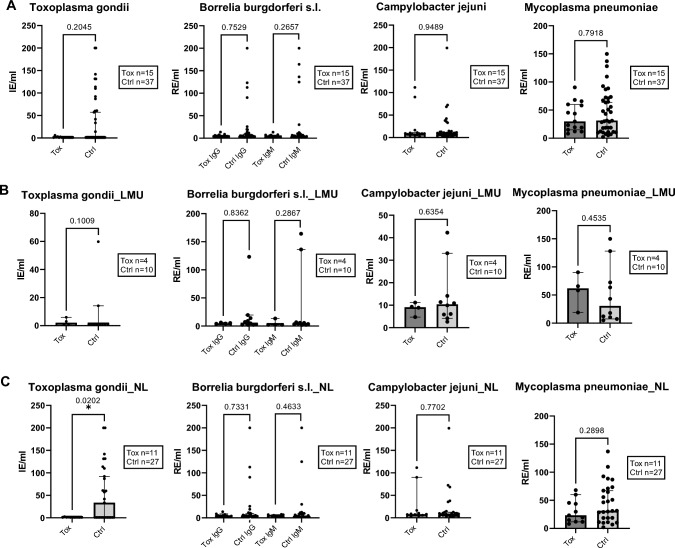
Fig. 4.
Bacteriological and protozoal quantitative agents are not associated with neurological irAEs. Values of antibodies against each bacterial/protozoal parameter. (A) Combined analysis of NL and LMU cohorts. Separate analyses of LMU (B) and NL (C) cohorts. Toxoplasma gondii EIA IgG, statistically higher values of Ctrl compared to Tox in NL cohort only. Borrelia EIA IgG and IgM. Campylobacter jejuni EIA IgG. Mycoplasma pneumoniae EIA IgG. P values displayed. Boxes show the numbers of measured samples for each agent. Comparison of patients with neurological irAE (Tox) under ICI vs. controls (Ctrl). Control group consisted of patients without neurological irAEs (NL) and of patients without any ICI induced irAEs (LMU). Mann–Whitney-U tests. Median with 95% CI displayed. For reference cut-off points see Table 1. Plasma (NL) and serum (LMU) analyses. Antibody concentrations per mililiter (ml): Internationale Einheit = international unit (IE), relative Einheiten = relative units (RE)
Patients developing neurological irAEs under ICI therapy (Tox) did not have significantly higher specific IgG levels compared to the control patients without neurological irAEs (Ctrl). In the NL cohort alone, significantly higher IgG levels against Toxoplasma gondii were observed for control patients (p = 0.0202) (Fig. 4C), but all patients were determined to be IgM negative (Fig. 5C).
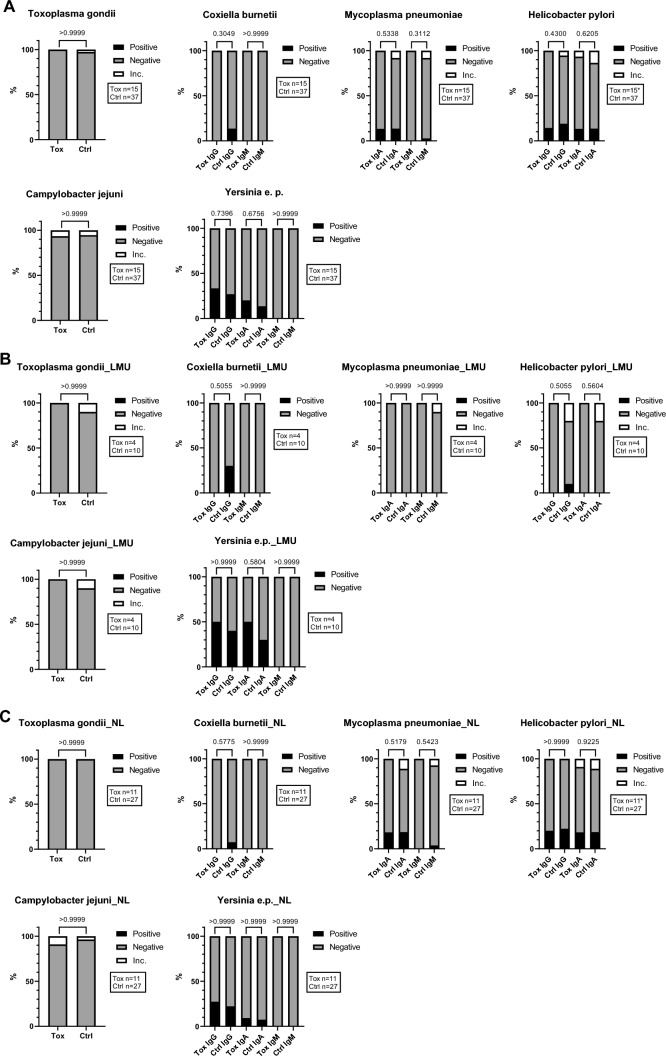
Fig. 5.
Bacteriological and protozoal semiquantitative and qualitative agents showed no association with neurological irAE. Melanoma patients with neurological irAE under ICI (Tox) versus control (Ctrl). Semiquantitative examination of antibodies against each bacterial/protozoal parameter. Combined (A) and separate analysis of NL (C) and LMU (B) cohorts. Toxoplasma gondii EIA IgM. Helicobacter pylori IgG and IgA, (A)*: for IgG Tox n = 14, (C) *: for IgG Tox n = 10. Campylobacter jejuni IgA. P values displayed. Boxes show the numbers of measured samples for each agent. Comparison of patients with neurological irAE (Tox) under ICI vs. controls (Ctrl). Control group included patients without neurological ICI induced irAEs (NL) and patients without any ICI induced irAEs (LMU). Mann–Whitney-U tests. For reference cut-off points see Table 1. Plasma (NL) and serum (LMU) analyses
A separate analysis of irHypophysitis cases in comparison to other neurological irAEs and to controls was not conducted since only one case of isolated irHypophysitis was investigated regarding the quantitative bacteriological and protozoal parameters.
Semiquantitative parameters
Regarding semiquantitative and qualitative analyses of anti-bacterial antibodies and anti-Toxoplasmosis IgM antibodies, the majority of patients tested negative for Campylobacter jejuni IgA and for Mycoplasma pneumoniae IgA and IgM, in both the combined (Fig. 5A) and separate analysis of the cohorts (Fig. 5B, C). In addition, most patients were negative for antibodies against Coxiella burnetii (IgG and IgM), Helicobacter pylori (IgG and IgA) and Yersinia e.p. (IgG, IgA and IgM). No significant difference between patients with or without neurological irAEs was observed (Fig. 5). A separate analysis of irHypophysitis in comparison to other neurological irAEs and controls was not performed, since only one case was included in the semiquantitative measurement of anti-bacteriologal and anti-protozoal antibodies.
Together, this implicates that in our patient cohorts, there was no association between the development of neurological irAEs under ICI therapy and serological signs of previous or current neurotropic bacterial and protozoal infections with the tested pathogens (Table 1, Fig. 4, 5).
Discussion
Treatment with ICI is increasingly common and irAEs constitute a considerable obstacle for safe administration, especially in the case of the life-threatening and irreversible neurological irAEs. Therefore, a deeper understanding of the aetiology and risk factors of neurological irAEs is of great importance. Immunological cross-reactivity of T-cells in response to infectious agents and host antigens from the nervous system could predispose patients to develop neurological irAEs under ICI due to molecular mimicry.
In this study, 61 melanoma patients under ICI therapy with (24 patients) and without (37 patients) neurological irAEs were tested for seroprevalence of 21 infections (14 viral, 6 bacterial and 1 protozoal), which have been previously described to trigger neurological pathologies potentially by molecular mimicry [17–19]. In two independent cohorts, there was no serological evidence for a higher incidence of preceding neurotropic infections in patients who developed neurological irAEs compared to patients without neurological irAEs. While this data suggests the absence of an association between neurotropic infections and development of neurological irAEs under ICI treatment, there are some limitations to our study. One limitation is that for some investigated parameters we observed a high serum prevalence in the control group as well as in the neurological irAE group, including influenza A and B, HSV 1/2 and parvovirus B19. This is in line with the general population, for which high incidences of these infections are known [31–33]. As only a minority of subjects infected with those pathogens may experience autoimmunity, we cannot rule out a participation of infections with these pathogens in the induction of neurological side effects either by molecular mimicry or by immune activation due to replication in the nervous system.
Since neurological irAEs are rare, and there is a large variety of types of neurological irAEs, it has previously been called for to join forces in the investigation of rare side effects to increase the number of patients per subtype [34], as it has been done for myocarditis [35]. Thus, maximizing collaboration efforts such as the side effect registry immune-oncology (www.serio-registry.org) [34] are needed especially in view of the high mortality rate reaching 21% for neurological irAEs. Additionally, irHypophysitis has been discussed controversially to be classified as a neurological or an endocrine irAE, whereas a strict classification is hardly possible [36, 37]. However, even when analysing irHypophysitis separately in comparison to the other investigated neurological irAEs or to the controls, no differences were observed. Nevertheless, by increasing the number of patients with a specific type of neurological irAEs, for example, irGBS [17], correlations with specific infections like Campylobacter jejuni infection or with specific HLA types might appear. This remains challenging due to the rarity of events. Taking the low incidence of neurological irAEs into consideration, this study analyzed a relatively high number of patients compared to previous studies [4, 5, 7, 10].
Few predictive markers for irAEs have shown an increased risk for irAEs in smokers, patients under 60 years of age, patients with a higher body mass index, and with severe lung, heart or kidney disease, whereas unspecific biomarkers such as cytokines or HLA genotypes have shown minor predictive evidence [15]. Increased inflammatory markers including c-reactive protein (CRP) and interleukin-6 are known to precede irAEs [38] and shifts in immune profiles occur early in the course of ICI treatment [13, 15]. For irThyreoiditis, baseline autoantibodies might be a risk factor [16]. Helicobacter pylori positivity has been demonstrated to be associated with decreased survival in ICI-treated patients [39], whereas only 4.3% of irGastritis cases under ICI are Helicobacter pylori and CMV positive [40]. This points out the relevance but also difficulty associated with the establishment of predictive markers for irAEs.
Importantly, our results were independent of investigated material, country and cohort with similar results for plasma and serum samples from the Netherlands (NL) and the German cohorts (LMU). We showed that there was no significant difference of the described viral, bacterial or protozoal pathogens with neurological irAEs across two different cohorts and three countries as well as no difference dependent on the tested material.
Significantly higher values of rubella IgG and Toxoplasma gondii IgG occurred in the NL control cohort compared to the NL neurological irAE cohort in contrast to the combined analysis (NL + LMU) or the LMU cohort alone. Retrospectively, it would have been of interest to query possible factors that may have an influence on the infectious parameters in the investigated cohorts. Since we were not able to survey these factors due to the already closed trials (OpACIN-neo and PRADO), we suppose a coincidentally occurring larger number of cat owners in the control group (NL) compared to the neurological irAE group could be causative for the observation regarding Toxoplasma gondii [41]. The higher levels of rubella IgG in the control group (NL) could be potentially explained by a higher number of participants with incomplete vaccination status or by a higher frequency of patients with contact to young children in this group, since infants of 0–4 years of age were observed to have the highest incidence in relation to age [42]. Therefore, we assume the results of these two parameters are of minor importance and occurred by coincidence. Also other tested agents might have been influenced by confounding factors and possibly appeared as false negative results. Therefore, we recommend the inclusion of a survey for unravelling the vaccination status and other potential influencing factors related to patients’ lives in future studies.
Even though no association was found in our cohorts to rule out mechanisms in the aetiology of neurological irAEs, antibodies or T cell clones directed against previously reported immunodominant epitopes have to be better characterized [18, 19]. Especially pre- and post-neurological symptom samples would be of interest for dynamics, particularly to investigate the development of serological IgM levels possibly indicative for a reactivation or a new infection. As an alternative to pre-existing infectious molecular mimicry, other possible underlying mechanisms could potentially trigger neurological irAEs. Autoreactive T and B cells to healthy tissue are thought to be a prime factor in the development of irAEs [19]. These autoreactive T cells could be pre-existing and perturbation of self-tolerance by ICI therapy could lead to reactivation, potentially due to genetic pre-disposition [43, 44]. In addition, a de novo autoreactive immune response could be generated through epitope spreading [19, 45]. These potential mechanisms are not mutually exclusive and could both contribute to (neurological) irAEs.
In conclusion, we did not find an association between the serologic prevalence for previous neurotropic infections in patients with melanoma and the development of neurological irAEs under ICI therapy. Given that neurological irAEs form a major obstacle for safely administering ICI in cancer patients, further efforts to unravel the underlying causes and predictive biomarkers of these toxicities are needed so as to identify patients at risk for irAEs induced by ICI treatment.
Acknowledgements
We thank all patients and their relatives. We thank Irene L. M. Reijers from the Netherlands Cancer Institute, Martin Eberhardt from the Department of Dermatology, Uniklinikum Erlangen and Friedrich-Alexander-Universität (FAU) Erlangen-Nürnberg, and Karl Dichtl from the Max von Pettenkofer Institute Munich, who advised us at the initiation of the project. RAS is supported by an National Health and Medical Research Council of Australia (NHMRC) Investigator Grant (APP2018514). GVL is supported by an NHMRC Investigator Grant and the University of Sydney Medical Foundation. AMM is supported by a NHMRC Investigator Grant, Nicholas and Helen Moore, and Melanoma Institute Australia.
Author contributions
Conceptualization, CS, EH, NK, AC, CB, LH; Methodology, CS, EH, CB, LH; Validation, all authors; Formal Analysis, CS, EH, CK, NK, CB, LH; Investigation, all authors; Resources, LH, CB; Data Curation, all authors; Writing—Original Draft Preparation, CS, EH, CB, LH; Writing—Review & Editing, all authors; Visualization, CS, EH, TF, CK, LH; Supervision, CB, LH; Project Administration, CB, LH; Funding Acquisition, CB, LH.
Funding
Open Access funding enabled and organized by Projekt DEAL. Funding was approved by BMBF (Bundesministerium für Bildung und Forschung) (grant no. 01ZX1905E) for our project MelAutim and by Bristol Myers Squibb foundation for SERIO (Side Effect Registry Immuno-Oncology).
Declarations
Conflict of interest
GVL is consultant advisor for Agenus, Amgen, Array Biopharma, AstraZeneca, Boehringer Ingelheim, Bristol Myers Squibb, Evaxion, Hexal AG (Sandoz Company), Highlight Therapeutics S.L., Innovent Biologics USA, Merck Sharpe & Dohme, Novartis, OncoSec, PHMR Ltd, Pierre Fabre, Provectus, Qbiotics, Regeneron. RAS has received fees for professional services from MetaOptima Technology Inc., F. Hoffmann-La Roche Ltd, Evaxion, Provectus Biopharmaceuticals Australia, Qbiotics, Novartis, Merck Sharp & Dohme, NeraCare, AMGEN Inc., Bristol-Myers Squibb, Myriad Genetics, GlaxoSmithKline. LH has received speaker and consultancy fees from Amgen, BiomeDx, BMS, Curevac, Kyowa Kirin, Merck, MSD, Myoncare, Novartis, Pierre-Fabre, Roche, Sanofi, SUN and Therakos. The LMU received research grants or clinical study grants from Agenus, AstraZeneca Inc., BMS, Hoffmann-La Roche AG, Huya Bioscience, Immunocore, IO Biotech, Merck, Merck Sharp & Dome GmbH, Miltenyi Biomedicine GmbH, Novartis, Pfizer, Pierre Fabre, Regeneron, Replimune, and Sanofi Aventis. The cantonal hospital St. Gallen (TH) received speaker and consultation fees from NovoCure, Amicus therapeutics, Sanofi Genzyme and Bayer AG and an unrestricted research grant from Bayer AG. AMM has served on advisory boards for BMS, MSD, Novartis, Roche, Pierre-Fabre and QBiotics. All remaining authors have declared no conflicts of interest.
Ethical approval
The study was approved by the local ethics committee of the Ludwig Maximilian University Munich, Netherlands Cancer Institute and Melanoma Institute of Australia. All centers were acting according to their regulatory requirements.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shared first author: C. Schmitt and E. P. Hoefsmit.
Shared senior author: C. U. Blank and L. M. Heinzerling.
References
- 1.Hodi FS, Chiarion-Sileni V, Gonzalez R, et al. Nivolumab plus ipilimumab or nivolumab alone versus ipilimumab alone in advanced melanoma (CheckMate 067): 4-year outcomes of a multicentre, randomised, phase 3 trial. Lancet Oncol. 2018;19(11):1480–1492. doi: 10.1016/s1470-2045(18)30700-9. [DOI] [PubMed] [Google Scholar]
- 2.Heinzerling L, de Toni EN, Schett G, Hundorfean G, Zimmer L. Checkpoint inhibitors. Dtsch Arztebl Int. 2019;116(8):119–126. doi: 10.3238/arztebl.2019.0119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spain L, Walls G, Julve M, et al. Neurotoxicity from immune-checkpoint inhibition in the treatment of melanoma: a single centre experience and review of the literature. Ann Oncol. 2017;28(2):377–385. doi: 10.1093/annonc/mdw558. [DOI] [PubMed] [Google Scholar]
- 4.Cuzzubbo S, Carpentier AF. Neurological adverse events of immune checkpoint blockade: from pathophysiology to treatment. Curr Opin Neurol. 2022;35(6):814–822. doi: 10.1097/wco.0000000000001113. [DOI] [PubMed] [Google Scholar]
- 5.Zimmer L, Goldinger SM, Hofmann L, et al. Neurological, respiratory, musculoskeletal, cardiac and ocular side-effects of anti-PD-1 therapy. Eur J Cancer. 2016;60:210–225. doi: 10.1016/j.ejca.2016.02.024. [DOI] [PubMed] [Google Scholar]
- 6.Voskens CJ, Goldinger SM, Loquai C, et al. The price of tumor control: an analysis of rare side effects of anti-CTLA-4 therapy in metastatic melanoma from the ipilimumab network. PLoS ONE. 2013;8(1):e53745. doi: 10.1371/journal.pone.0053745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Knauss S, Ginesta Roque L, Hühnchen P, Heinzerling L, Böhmerle W, Endres M. Neurological side effects of checkpoint inhibitors. Nervenarzt. 2019;90(2):138–147. doi: 10.1007/s00115-018-0571-8. [DOI] [PubMed] [Google Scholar]
- 8.Moreira A, Loquai C, Pföhler C, et al. Myositis and neuromuscular side-effects induced by immune checkpoint inhibitors. Eur J Cancer. 2019;106:12–23. doi: 10.1016/j.ejca.2018.09.033. [DOI] [PubMed] [Google Scholar]
- 9.Baldauf MC, Kapauer M, Joerger M, et al. Pembrolizumab-associated CD8(+) vasculitic mononeuritis multiplex in a patient with mesothelioma. Neurol Neuroimmunol Neuroinflamm. 2021 doi: 10.1212/nxi.0000000000000993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Müller-Jensen L, Zierold S, Versluis JM, et al. Characteristics of immune checkpoint inhibitor-induced encephalitis and comparison with HSV-1 and anti-LGI1 encephalitis: a retrospective multicentre cohort study. Eur J Cancer. 2022;175:224–235. doi: 10.1016/j.ejca.2022.08.009. [DOI] [PubMed] [Google Scholar]
- 11.Voskens C, Cavallaro A, Erdmann M, et al. Anti-cytotoxic T-cell lymphocyte antigen-4-induced regression of spinal cord metastases in association with renal failure, atypical pneumonia, vision loss, and hearing loss. J Clin Oncol. 2012;30(33):e356–e357. doi: 10.1200/jco.2011.41.4359. [DOI] [PubMed] [Google Scholar]
- 12.Schulz TU, Zierold S, Sachse MM, et al. Persistent immune-related adverse events after cessation of checkpoint inhibitor therapy: prevalence and impact on patients' health-related quality of life. Eur J Cancer. 2022;176:88–99. doi: 10.1016/j.ejca.2022.08.029. [DOI] [PubMed] [Google Scholar]
- 13.Nuñez NG, Berner F, Friebel E, et al. Immune signatures predict development of autoimmune toxicity in patients with cancer treated with immune checkpoint inhibitors. Med (N Y) 2023;4(2):113–129.e7. doi: 10.1016/j.medj.2022.12.007. [DOI] [PubMed] [Google Scholar]
- 14.Weiss J, Kirchberger MC, Heinzerling L. Therapy preferences in melanoma treatment-Willingness to pay and preference of quality versus length of life of patients, physicians, healthy individuals and physicians with oncological disease. Cancer Med. 2020;9(17):6132–6140. doi: 10.1002/cam4.3191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chennamadhavuni A, Abushahin L, Jin N, Presley CJ, Manne A. Risk factors and biomarkers for immune-related adverse events: a practical guide to identifying high-risk patients and rechallenging immune checkpoint inhibitors. Front Immunol. 2022;13:779691. doi: 10.3389/fimmu.2022.779691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muir CA, Clifton-Bligh RJ, Long GV, et al. Thyroid immune-related adverse events following immune checkpoint inhibitor treatment. J Clin Endocrinol Metab. 2021;106(9):e3704–e3713. doi: 10.1210/clinem/dgab263. [DOI] [PubMed] [Google Scholar]
- 17.Rodríguez Y, Rojas M, Pacheco Y, et al. Guillain–Barré syndrome, transverse myelitis and infectious diseases. Cell Mol Immunol. 2018;15(6):547–562. doi: 10.1038/cmi.2017.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lee S, Levin MC. Molecular mimicry in neurological disease: what is the evidence? Cell Mol Life Sci. 2008;65(7–8):1161–1175. doi: 10.1007/s00018-007-7312-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rojas M, Restrepo-Jiménez P, Monsalve DM, et al. Molecular mimicry and autoimmunity. J Autoimmun. 2018;95:100–123. doi: 10.1016/j.jaut.2018.10.012. [DOI] [PubMed] [Google Scholar]
- 20.Rozeman EA, Menzies AM, van Akkooi AC, et al. Identification of the optimal combination dosing schedule of neoadjuvant ipilimumab plus nivolumab in macroscopic stage III melanoma (OpACIN-neo): a multicentre, phase 2, randomised, controlled trial. Lancet Oncol. 2019;20(7):948–960. doi: 10.1016/S1470-2045(19)30151-2. [DOI] [PubMed] [Google Scholar]
- 21.Rozeman E, Hoefsmit E, Reijers I, et al. Survival and biomarker analyses from the OpACIN-neo and OpACIN neoadjuvant immunotherapy trials in stage III melanoma. Nat Med. 2021;27(2):256–263. doi: 10.1038/s41591-020-01211-7. [DOI] [PubMed] [Google Scholar]
- 22.Reijers IL, Menzies AM, van Akkooi AC, et al. Personalized response-directed surgery and adjuvant therapy after neoadjuvant ipilimumab and nivolumab in high-risk stage III melanoma: the PRADO trial. Nat Med. 2022;28:1178–1188. doi: 10.1038/s41591-022-01851-x. [DOI] [PubMed] [Google Scholar]
- 23.U.S. Department of Health and Human Services (2017) Common terminology criteria for adverse events (CTCAE) Version 5.0. Available: https://ctep.cancer.gov/protocoldevelopment/electronic_applications/ctc.htm
- 24.Clements DM, Crumley B, Chew GM, et al. Phenotypic and functional analyses guiding combination immune checkpoint immunotherapeutic strategies in HTLV-1 infection. Front Immunol. 2021;12:608890. doi: 10.3389/fimmu.2021.608890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shi Y, Zheng H, Wang M, Ding S. Influence of Helicobacter pylori infection on PD-1/PD-L1 blockade therapy needs more attention. Helicobacter. 2022;27(2):e12878. doi: 10.1111/hel.12878. [DOI] [PubMed] [Google Scholar]
- 26.Zhu YC, Elsheikha HM, Wang JH, et al. Synergy between Toxoplasma gondii type I ΔGRA17 immunotherapy and PD-L1 checkpoint inhibition triggers the regression of targeted and distal tumors. J Immunother Cancer. 2021 doi: 10.1136/jitc-2021-002970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Spagnolo F, Boutros A, Croce E, et al. Influenza vaccination in cancer patients receiving immune checkpoint inhibitors: a systematic review. Eur J Clin Invest. 2021;51(7):e13604. doi: 10.1111/eci.13604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lankes K, Hundorfean G, Harrer T, et al. Anti-TNF-refractory colitis after checkpoint inhibitor therapy: possible role of CMV-mediated immunopathogenesis. Oncoimmunology. 2016;5(6):e1128611. doi: 10.1080/2162402x.2015.1128611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lee KA, Shaw H, Bataille V, Nathan P. Campylobacteriosis following immunosuppression for immune checkpoint inhibitor-related toxicity. J Immunother Cancer. 2020 doi: 10.1136/jitc-2020-000577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bai Y, Xie T, Wang Z, et al. Efficacy and predictive biomarkers of immunotherapy in Epstein–Barr virus-associated gastric cancer. J Immunother Cancer. 2022 doi: 10.1136/jitc-2021-004080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Malainou C, Herold S. Influenza. Internist (Berl) 2019;60(11):1127–1135. doi: 10.1007/s00108-019-00670-6. [DOI] [PubMed] [Google Scholar]
- 32.Arshad Z, Alturkistani A, Brindley D, Lam C, Foley K, Meinert E. Tools for the diagnosis of herpes simplex virus 1/2: systematic review of studies published between 2012 and 2018. JMIR Public Health Surveill. 2019;5(2):e14216. doi: 10.2196/14216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jain A, Jain P, Kumar A, Prakash S, Khan DN, Kant R. Incidence and progression of Parvovirus B19 infection and molecular changes in circulating B19V strains in children with haematological malignancy: a follow up study. Infect Genet Evol. 2018;57:177–184. doi: 10.1016/j.meegid.2017.11.021. [DOI] [PubMed] [Google Scholar]
- 34.Heinzerling L, Ascierto PA, Dummer R, et al. Adverse events 2.0-Let us get SERIOs: new reporting for adverse event outcomes needed in the era of immunooncology. Eur J Cancer. 2019;112:29–31. doi: 10.1016/j.ejca.2019.01.015. [DOI] [PubMed] [Google Scholar]
- 35.Mahmood SS, Fradley MG, Cohen JV, et al. Myocarditis in patients treated with immune checkpoint inhibitors. J Am Coll Cardiol. 2018;71(16):1755–1764. doi: 10.1016/j.jacc.2018.02.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bot I, Blank CU, Boogerd W, Brandsma D. Neurological immune-related adverse events of ipilimumab. Pract Neurol. 2013;13(4):278–280. doi: 10.1136/practneurol-2012-000447. [DOI] [PubMed] [Google Scholar]
- 37.Wright JJ, Powers AC, Johnson DB. Endocrine toxicities of immune checkpoint inhibitors. Nat Rev Endocrinol. 2021;17(7):389–399. doi: 10.1038/s41574-021-00484-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Husain B, Kirchberger MC, Erdmann M, et al. Inflammatory markers in autoimmunity induced by checkpoint inhibitors. J Cancer Res Clin Oncol. 2021;147(6):1623–1630. doi: 10.1007/s00432-021-03550-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Oster P, Vaillant L, Riva E, et al. Helicobacter pylori infection has a detrimental impact on the efficacy of cancer immunotherapies. Gut. 2022;71(3):457–466. doi: 10.1136/gutjnl-2020-323392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Obeidat A, Silangcruz K, Kozai L, Wien E, Fujiwara Y, Nishimura Y. Clinical characteristics and outcomes of gastritis associated with immune checkpoint inhibitors: scoping review. J Immunother. 2022;45(8):363–369. doi: 10.1097/cji.0000000000000435. [DOI] [PubMed] [Google Scholar]
- 41.Brennan A, Hawley J, Dhand N, et al. Seroprevalence and risk factors for toxoplasma gondii infection in owned domestic cats in Australia. Vector Borne Zoonotic Dis. 2020;20(4):275–280. doi: 10.1089/vbz.2019.2520. [DOI] [PubMed] [Google Scholar]
- 42.Bogusz J, Augustynowicz E, Paradowska-Stankiewicz I. Rubella in Poland in 2019. Przegl Epidemiol. 2021;75(4):588–596. doi: 10.32394/pe.75.55. [DOI] [PubMed] [Google Scholar]
- 43.Hoefsmit EP, Rozeman EA, Haanen JB, Blank CU. Susceptible loci associated with autoimmune disease as potential biomarkers for checkpoint inhibitor-induced immune-related adverse events. ESMO open. 2019;4(4):e000472. doi: 10.1136/esmoopen-2018-000472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cappelli LC, Dorak MT, Bettinotti MP, Bingham CO, III, Shah AA. Association of HLA-DRB1 shared epitope alleles and immune checkpoint inhibitor-induced inflammatory arthritis. Rheumatology. 2019;58(3):476–480. doi: 10.1093/rheumatology/key358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.June CH, Warshauer JT, Bluestone JA. Is autoimmunity the Achilles' heel of cancer immunotherapy? Nat Med. 2017;23(5):540–547. doi: 10.1038/nm.4321. [DOI] [PubMed] [Google Scholar]