Abstract
Sarcina ventriculi is an anaerobic gram-positive bacterium capable of surviving in the acidic environment of the stomach and causing gastrointestinal symptoms. We report the case of a 51-year-old patient with no notable medical history who presented with abdominal distension, nausea, and vomiting. Initial endoscopic evaluation revealed a distended stomach in stasis with pyloric stenosis. Biopsies revealed the presence of Helicobacter pylori and S. ventriculi. A therapeutic protocol was administered, but no symptomatic relief was observed. Subsequently, the patient was referred to our institution, where computed tomography imaging of the abdomen was performed. The results corroborated a presentation suggestive of a high obstruction attributable to a right anterior para-duodenal internal hernia. Ultimately, surgery was undertaken, ruling out the diagnosis of right para-duodenal internal hernia and resulting in gastroenteric anastomosis with satisfactory improvement in clinical symptoms.
Keywords: gastroenteric anastomosis, gastroparesis, gastric pyloric obstruction, Sarcina ventriculi, Helicobacter pylori
Introduction
Belonging to the Clostridiaceae family, this pathogen derives its name from the Latin term ‘Sarcina’, which evokes the notion of ‘bundle’. Patients with Sarcina ventriculi present a wide range of gastrointestinal symptoms [1]. It was first described in 1842 by John Goodsir, and since then, only a handful of cases have been documented. S. ventriculi, a gram-positive anaerobic coccus, is resilient to the extremely low pH conditions of the stomach [2]. In 1872, anatomist and microbiologist David Ferrier observed the presence of the bacterium in blood samples from patients suffering from enteric fever [3]. Endoscopy revealed signs of food residue accumulation, gastric ulcers, inflammation, and erosions [4]. We present here a case of S. ventriculi characterized by a long history of gastrointestinal symptoms that required surgical intervention following failure of medical treatment.
Case presentation
A 51-year-old patient with no significant medical history. He was admitted to the emergency department with abdominal distension, persistent vomiting, intolerance to solid foods, he could consume only small amounts of liquid. Clinical examination of the abdomen revealed diffuse tenderness in all quadrants, accompanied by severe abdominal distension. Prior to his consultation at our institution, he had undergone oesophagogastroduodenoscopy, revealing a dilated stomach and narrowing of the pyloric ring. Biopsies revealed the presence of H. pylori and S. ventriculi. (Fig. 1). He was put on conservative treatment for a duration of ~4 weeks, but no significant improvement was noted. On admission to our clinic, he underwent a computed tomography (CT) scan of the abdomen (Fig. 2), which revealed marked dilatation of the stomach, as well as an upright arrangement of the entire jejunal coves, suggesting the presence of a high occlusion due to a right anterior para-duodenal internal hernia. While a more comprehensive non-operative management approach could have been contemplated in the absence of hernia-related concerns, the clinical deterioration and the refractory nature of symptoms to medical therapy served to underscore the appropriateness of the surgical approach. During surgery, the hypothesis of a para-duodenal internal hernia was ruled out after a duodeno-pancreatic detachment using the KOCHER maneuver, thus facilitating exposure of the entire duodenum and also allowing individualization of the transition zone located at the level of the pylorus (Fig. 3), thus justifying the performance of gastroenteric anastomosis (Fig. 4). Post-operatively, the diet was progressively advanced and well tolerated. On discharge, the patient was in satisfactory condition.
Figure 1.
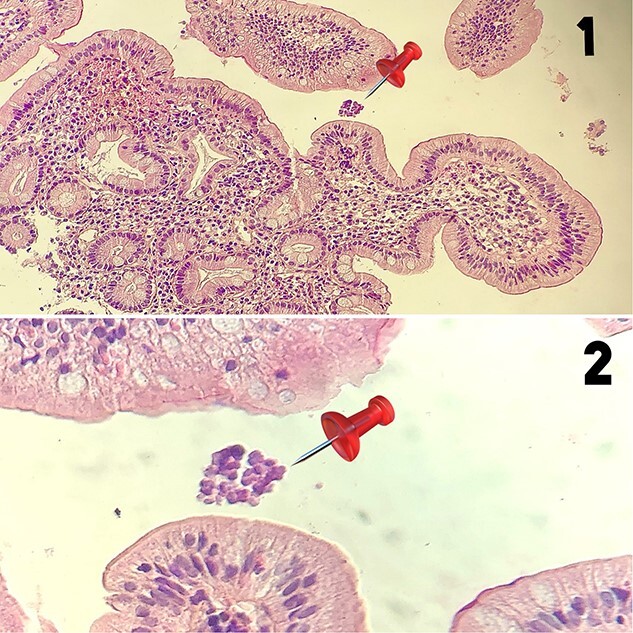
1-Low magnification histological section (HE ×40) showing a bulbous mucosa housing in surface the Sarcina ventriculi germ (pin) 2-High magnification microphotograph (HE ×400) revealing the presence of cuboid-shaped germs arranged in tetrads, corresponding to Sarcina ventriculi (pin).
Figure 2.

CT scan of the abdomen, which revealed marked dilatation of the stomach.
Figure 3.

Individualization of the transition zone located at the level of the pylorus.
Figure 4.

Gastroenteric anastomosis.
Discussion
The bacterium’s natural habitat is soil, but it can also be found in water and air in the form of spores [5]. Infection in humans and animals is generally caused by food contamination. In addition, it has been shown that there is a link between the consumption of a vegetarian diet and the presence of the bacterium in feces [6]. Several studies have established a correlation between this organism and delayed gastric emptying. According to Canale et al. [7], the growth of S. ventriculi in the human gastrointestinal tract is the result of delayed gastric emptying caused by conditions such as diabetic gastroparesis, gastric reconstructive surgery, scarring, and pyloric stenosis. However, although the pathogenicity of S. ventriculi in humans remains unclear, some authors support the theory that this organism directly affects the healthy stomach [8]. Since 2003, few cases have been reported in the literature. In 2022, a systematic review by Tartaglia et al. [9] identified 65 cases from 55 articles, with a median age of 51 years at diagnosis and the diagnosis made primarily by histopathological examination of endoscopic biopsies taken from the stomach. The predominant location for bacterial identification is the stomach, followed by the esophagus and duodenum. Bacteria have also been reported in blood and urine [3, 10]. On upper gastrointestinal endoscopic examination, the most frequent finding is food retention or bezoar formation. In their study, Haroon Al Rasheed and colleagues [11] reported a case where the bacterium was identified in a gastric ulcer after treatment and eradication of H. pylori. It is important to note that the two bacteria can coexist, as pointed out by Sauter and colleagues [12]. Although direct evidence substantiating a causal relationship between the bacterium and gastric outlet obstruction is limited, the available evidence within the literature does suggest an association between S. ventriculi and delayed gastric emptying. This temporal delay can potentially result from a combination of factors, including pre-existing mucosal lesions and delayed emptying, which together contribute to the symptomatic manifestation of obstruction. Furthermore, the fermentative metabolism of carbohydrates by S. ventriculi, culminating in the production of acetaldehyde and ethanol, could conceivably exacerbate symptoms of gastric distension and gastroparesis [5]. To improve symptoms of gastric distension and gastroparesis in patients with S. ventriculi, the use of proton pump inhibitors and prokinetics has been recommended, fasting appears to contribute to clinical improvement by eliminating the carbohydrate source for the bacteria, and antibiotic regimens are varied and can be used orally or intravenously [2]. The main antibiotics used to treat this infection are metronidazole alone or in combination with ciprofloxacin [4]. Other antibiotics, such as vancomycin and piperacillin-tazobactam, have been shown to be effective in eradicating this organism [13]. To date, however, no consensus has been reached on a standard treatment regimen or duration for S. ventriculi infection [4]. When symptomatic treatment and antibiotics fail to bring about improvement, surgery has been reported as the ultimate intervention in many cases of S. ventriculi [14–15].
Conclusion
S. ventriculi, a bacterium closely associated with gastrointestinal complications, such as stomach distension and pyloric obstruction, is attracting particular attention. Although medical treatments are generally preferred as first-line treatments, surgery is an effective alternative in cases where symptoms persist. However, further research is needed to gain a better understanding of the pathogenic nature of this bacterium and to develop standardized treatment protocols that will optimize therapeutic outcomes.
Contributor Information
Tarik Deflaoui, Department of General Surgery, Mohammed VI University Hospital, BP 4806 Oujda Universite 60049 Oujda, Oujda, Morocco.
Mohamed Y Mabrouk, Department of General Surgery, Mohammed VI University Hospital, BP 4806 Oujda Universite 60049 Oujda, Oujda, Morocco.
Anas Derkaoui, Department of General Surgery, Mohammed VI University Hospital, BP 4806 Oujda Universite 60049 Oujda, Oujda, Morocco.
Slimi Younes, Department of General Surgery, Mohammed VI University Hospital, BP 4806 Oujda Universite 60049 Oujda, Oujda, Morocco.
Yassir Akil, Department of General Surgery, Mohammed VI University Hospital, BP 4806 Oujda Universite 60049 Oujda, Oujda, Morocco.
Rihab Amara, Department of Medicine, Mohammed VI University Hospital, Faculty of Medicine and Pharmacy, Mohammed I University, BP 4806 Oujda Universite 60049 Oujda, Oujda, Morocco.
Nada Akouh, Department of Pathology, Mohammed VI University Hospital, BP 4806 Oujda Universite 60049 Oujda, Oujda, Morocco.
Benani Amal, Department of Pathology, Mohammed VI University Hospital, BP 4806 Oujda Universite 60049 Oujda, Oujda, Morocco.
Rachid Jabi, Department of General Surgery, Mohammed VI University Hospital, BP 4806 Oujda Universite 60049 Oujda, Oujda, Morocco; Laboratory of Anatomy, Microsurgery and Surgery Experimental and Medical Simulation (LAMCESM), Faculty of Medicine and Pharmacy, Mohammed Ist University, BP 4806 Oujda Universite 60049 Oujda, Oujda, Morocco.
Mohammed Bouziane, Department of General Surgery, Mohammed VI University Hospital, BP 4806 Oujda Universite 60049 Oujda, Oujda, Morocco; Laboratory of Anatomy, Microsurgery and Surgery Experimental and Medical Simulation (LAMCESM), Faculty of Medicine and Pharmacy, Mohammed Ist University, BP 4806 Oujda Universite 60049 Oujda, Oujda, Morocco.
References
- 1. Lam-Himlin D, Tsiatis AC, Montgomery E, et al. Sarcina organisms in the gastrointestinal tract: a clinicopathologic and molecular study. Am J Surg Pathol 2011;35:1700–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Al Rasheed MR, Senseng CG. Sarcina ventriculi: revue de la littérature. Arch Pathol Lab Med 2016;140:1441–5. [DOI] [PubMed] [Google Scholar]
- 3. Ferrier D. The constant occurrence of Sarcina ventriculi (Goodsir) in the blood of man and the lower animals: with remarks on the nature of sarcinous vomiting. BMJ 1872;1:98–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Al Rasheed MR, Senseng CG. Sarcina ventriculi : review of the literature. Arch Pathol Lab Med 2016;140:1441–5. [DOI] [PubMed] [Google Scholar]
- 5. Lowe SE, Pankratz HS, Zeikus JG. Influence of pH extremes on sporulation and ultrastructure of Sarcina ventriculi. J Bacteriol 1989;171:3775–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Crowther JS. Sarcina ventriculi in human faeces. J Med Microbiol 1971;4:343–50. [DOI] [PubMed] [Google Scholar]
- 7. Canale-Parola E. Biology of the sugar-fermenting Sarcinae. Bacteriol Rev 1970;34:82–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ali MA, Arnold CA, Singhi AD, Voltaggio L. Clues to uncommon and easily overlooked infectious diagnoses affecting the GI tract and distinction from their clinicopathologic mimics. Gastrointest Endosc 2014;80:689–706. [DOI] [PubMed] [Google Scholar]
- 9. Tartaglia D, Coccolini F, Mazzoni A, et al. Sarcina ventriculi infection: a rare but fearsome event. A systematic review of the literature. Int J Infect Dis 2022;115:48–61. [DOI] [PubMed] [Google Scholar]
- 10. Bortolotti P, Kipnis E, Faure E, et al. Bactériémie à Clostridium ventriculi après pseudo-obstruction colique aiguë : à propos d'un cas. Anaerobe 2019;59:32–4. [DOI] [PubMed] [Google Scholar]
- 11. Haroon Al Rasheed MR, Kim GJ, Senseng C. Un cas rare de Sarcina ventriculi de l'estomac chez un patient asymptomatique. Int J Surg Pathol 2016;24:142–5. [DOI] [PubMed] [Google Scholar]
- 12. Sauter JL, Nayar SK, Anders PD, D'Amico M, Butnor KJ, Wilcox RL. Coexistence des organismes Sarcina et de la gastrite/duodénite à Helicobacter pylori chez les frères et sœurs pédiatriques. J Clin Anat Pathol (JCAP) 2013;1:103. [PMC free article] [PubMed] [Google Scholar]
- 13. Singh K. Emphysematous gastritis associated with Sarcina ventriculi. Case Rep Gastroenterol 2019;13:207–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Liu L, Gopal P. Sarcina ventriculi in a patient with slipped gastric band and gastric distention. Clin Gastroenterol Hepatol 2018;16:0–6. [DOI] [PubMed] [Google Scholar]
- 15. Dumitru A, Alius C, Nica AE, Antoniac I, Gheorghita D, Gradinaru S, et al. Fatal outcome of gastric perforation due to infection with Sarcina spp. a case report. IDCases 2020;19:e00711. 10.1016/j.idcr.2020.e00711. [DOI] [PMC free article] [PubMed] [Google Scholar]


