Abstract
Cholecystocutaneous fistulas (CCFs) are rare complications of gallbladder disease, wherein chronic inflammation leads the formation of an anomalous fistulous tract between the gallbladder and skin. Widespread availability of imaging modalities and timely access to surgical expertise has caused a marked decline in their incidence. Consequently, there is notable heterogeneity in management approaches to this disease entity, and guidance regarding the best, evidence-based treatment strategy is lacking. Most patients are definitively managed with cholecystectomy and en bloc excision of the adjoining fistula tract. However, there is no guidance on how to manage patients whose comorbidities preclude them from operative intervention. We provide the first report chronicling the stepwise development of a CCF in a 75-year-old woman, complete with pictorial documentation of its evolution. Furthermore, we present the inaugural account of a practical, safe approach to the long-term conservative management of CCFs in patients in whom surgical or endoscopic intervention is prohibitive.
INTRODUCTION
First described by Thelisus in 1670, a cholecystocutaneous fistula (CCF) denotes the exceptionally rare condition where extraperitoneal gallbladder perforation leads to an anomalous connection with the skin [1]. There has been a marked decline in the overall incidence of CCFs due, in large part, to the advent of widely available diagnostic imaging modalities and timely access to surgical or endoscopic interventions [1–4]. By comparison, intraperitoneal gallbladder perforation is much more common, with the formation of fistulous connections with the duodenum, colon, jejunum, common bile duct, and stomach all having been described [1].
CCFs typically complicate subclinical or untreated calculous cholecystitis, but may also occur secondary to an invasive gallbladder malignancy or acalculous cholecystitis [2–4]. They can also arise iatrogenically following percutaneous cholecystostomy or open subtotal cholecystectomy [2]. The pathogenesis is attributed to cystic duct obstruction by a gallstone, leading to increased intravesicular pressure and the subsequent sequelae of inflammation, ischaemia, infarction, gangrene, and perforation [3].
CCFs have a strong female preponderance and manifest mostly in those aged over 60 years old [2–4]. Most patients present with an abscess or a discharging sinus in the right hypochondrium, although other sites have also been reported to be involved, such as the umbilicus, anterior chest, and gluteal region [3–7]. Computer tomography (CT) scan with or without fistulogram and magnetic resonance cholangiopancreatography is the diagnostic imaging modality of choice for diagnosing and delineating the anatomy of a CCF [4].
Because of their rarity, the ideal management strategy of CCFs remains elusive and there is notable heterogeneity in the literature regarding treatment approaches [4]. When possible, the mainstay treatment strategy involves open or laparoscopic cholecystectomy with en bloc excision of the fistula tract [1–4].
We present a unique account of the formation of a CCF over time, complete with pictorial documentation of its progression at various stages of its development. To our knowledge, this is the first occasion in which the stepwise evolution of a CCF has ever been documented. Furthermore, we demonstrate the feasibility and safety of the long-term conservative management of this rare entity as a controlled fistula.
CASE REPORT
A 75-year-old woman from a nursing home presented to the emergency department with a 3-week history of a painful right-sided abdominal lump. She was otherwise systemically well. Her medical history was notable for end-stage chronic obstructive pulmonary disease requiring permanent home oxygen, lung cancer, and chronic cholecystitis. On presentation, all her vitals were normal. Examination revealed an indurated, tender, irreducible mass in the right hypochondrium with overlying cellulitis. Her white cell count was 9.3 mmol/L and C-reactive protein was 45 mg/L. CT scan revealed a complex collection in the right anterior abdominal wall, contiguous with a thickened gallbladder, consistent with an abdominal wall abscess complicating perforated acute-on-chronic cholecystitis (Fig. 1).
Figure 1.
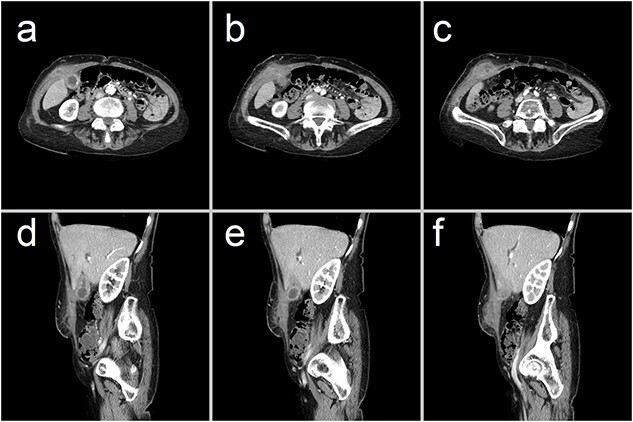
Representative CT images showing (a–c) axial and (d–f) sagittal views of a 47 × 23 × 66 mm complex collection within the right anterior abdominal wall, consisting of fluid and phlegmonous components. This collection is contiguous with a thick-walled gallbladder that contains calculi. These findings are consistent with an abdominal wall abscess complicating acute-on-chronic cholecystitis with extraperitoneal perforation.
Given her significant perioperative risks, the decision was made to incise and drain the abscess under sedation and local anaesthesia. The abscess cavity was confirmed to communicate with the gallbladder, as evidenced by the extrusion of gallstones. A Penrose drain was inserted, allowing for continuous drainage. She made an unremarkable postoperative recovery and was discharged on the 6th day of admission on oral antibiotics.
She represented 10 weeks later, complaining of pain at the previous surgical site. Remarkably, removal of the overlying wound dressing revealed a 20 mm gallstone lodged at the external opening of a CCF that had, by then, epithelialized along the previous drain tract (Figs 2 and 3). This obstructing gallstone and multiple others were removed from the visible fistula tract at the bedside using forceps.
Figure 2.
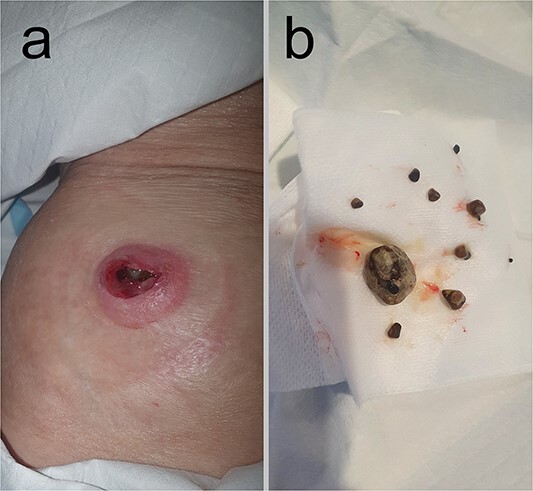
Clinical pictures taken at the time of representation 10 weeks following initial presentation and percutaneous drainage. (a) External opening of the CCF onto the skin of the right hypochondrium following removal of the obstructing gallstone from its orifice. (b) This obstructing 20 mm gallstone and multiple other gallstones, ranging in size from 2 to 7 mm, were retrieved from within the fistula tract.
Figure 3.
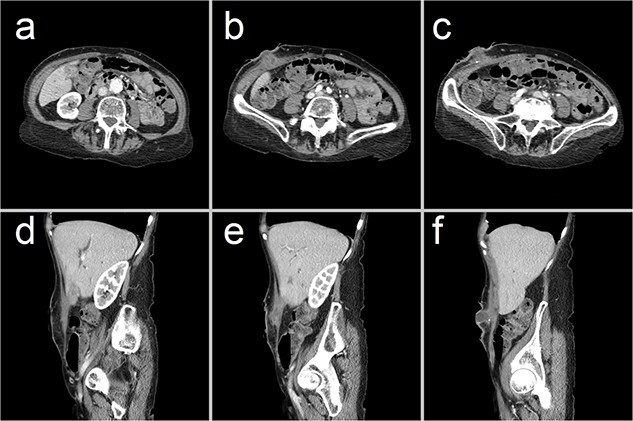
Representative CT images showing (a–c) axial and (d–f) sagittal views of the CCF, forming a communicating tract that extends from the gallbladder fundus, through the anterior abdominal wall and onto the skin. There has been interval collapse of the gallbladder, whose wall remains thickened with mucosal hyperenhancement, in keeping with chronic cholecystitis. Hyperenhancing gallstones are visible along this fistula tract.
She was discharged with a plan for continued conservative management with regular stoma bag changes and fistula output monitoring. On outpatient follow-up 2 months later, she remained well, and the fistula continued to drain freely.
DISCUSSION
To our knowledge, this is the first instance in which the long-term development, progression, and management of a CCF have ever been chronicled. As with most classic cases, our patient presented with a painful and inflamed lump in the right hypochondrium on a background of known chronic cholecystitis. Subsequent CT imaging confirmed this to be the result of extraperitoneal perforation of acute-on-chronic cholecystitis into the contiguous, overlying skin, forming a well-circumscribed subcutaneous abscess.
Our patient’s frailty and poor respiratory reserve precluded her from being able to withstand a general anaesthetic, so we tailored our management approach accordingly. In order to achieve source control, we incised and drained the abscess and explored the underlying fistula tract under local anaesthesia and sedation. Leaving a Penrose drain in situ allowed for indefinite, continuous drainage of the underlying fistulating gallbladder disease. However, our patient eventually represented acutely because the CCF, which had, by then, matured through epithelialisation along the previous drain tract, was obstructed by a large gallstone lodged at its cutaneous sinus. This was managed by bedside disimpaction of the offending gallstone from the skin opening. Numerous, smaller gallstones were also retrieved from within the fistula tract in this way, with immediate resolution of the patient’s symptoms. This phenomenon of extrusion of gallstones from a CCF has been previously documented [8, 9].
Given their scarcity, the ideal management strategy of CCFs remains elusive and there is notable heterogeneity in the literature regarding treatment approaches [4]. The overwhelming majority is managed definitively with open or laparoscopic cholecystectomy with fistulotomy, whereby the fistula tract and gallbladder are excised en bloc [3, 4] . However, as was the case for our patient, some individuals have comorbidities that preclude them from surgery, and the best treatment approach for such patients is even more ambiguous. Drainage with endoscopic retrograde cholangiopancreatography with or without stenting is a viable alternative in patients who are unable to undergo surgery [4, 5]. However, the sedation risks associated with this approach were also considered to be prohibitive in our patient because of her advanced chronic lung disease.
Interestingly, there have been reports of percutaneous cholecystostomy creating the substratum upon which a CCF later forms through presumed maturation and epithelialization along the drain tract [2, 8–10]. Our case is unique in that the patient’s CCF matured along the foundations of a Penrose drain that was left within the abscess cavity following surgical incision and drainage during her index presentation. This drain was dislodged 2 weeks after its initial insertion, and purulent bile continued to drain freely into an overlying stoma bag, which was being managed by the patient’s nurses in the nursing home where she resided.
In the report herein, we presented a unique account of the formation of a CCF following surgical percutaneous drainage of perforated cholecystitis, complete with pictorial documentation of its evolution at various stages of its development. To our knowledge, this is the first instance in which the stepwise progression of a CCF has ever been documented. Furthermore, we demonstrate the feasibility and safety of managing this rare entity long-term as a controlled fistula with drainage into an overlying stoma bag, akin to other gastrointestinal and renal tract stomas.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the patient whose case is discussed herein for allowing us to share her story in the spirit of contributing to medical literature regarding this rare disease entity. We would also like to thank our family and friends for their continued and unconditional support.
Contributor Information
Andrea J Naim, Department of Surgery, Wollongong Hospital, Loftus Street, Wollongong 2500, NSW, Australia; Department of Surgery, Shoalhaven District Memorial Hospital, Scenic Drive, Nowra 2541, NSW, Australia.
Marie Shella De Robles, Department of Surgery, Wollongong Hospital, Loftus Street, Wollongong 2500, NSW, Australia; Department of Surgery, Shoalhaven District Memorial Hospital, Scenic Drive, Nowra 2541, NSW, Australia; Graduate School of Medicine, University of Wollongong, Northfields Avenue, Keiraville 2500, NSW, Australia.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
This work did not receive any funding or sponsorship from any third-party agencies or institutions.
DATA AVAILABILITY
De-identified data is available upon request from the corresponding author.
ETHICAL APPROVAL
This work did not require any ethical approval.
CONSENT
Informed consent was obtained from the patient for publication of the article herein.
GUARANTORS
Dr Andrea J. Naim and Dr Marie S. De Robles.
References
- 1. Santos Seoane SM, Díaz Fernàndez V, Arenas García V. Cholecystocutaneous fistula. Rev Esp Enferm Dig 2019;111:407–8. [DOI] [PubMed] [Google Scholar]
- 2. Lofgren DH, Vasani S, Singzon V. Abdominal wall abscess secondary to cholecystocutaneous fistula via percutaneous cholecystostomy tract. Cureus 2019;11:e4444–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Rinzivillo NMA, Danna R, Leanza V, Lodato M, Marchese S, Basile F, et al. Case report: spontaneous cholecystocutaneous fistula, a rare cholelithiasis complication. F1000Research 2017;6:1768–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Alsaman MKB, Mazketly M, Ziadeh M, Aleter O, Ghazal A. Cholecystocutaneous fistula incidence, etiology, clinical manifestations, diagnosis and treatment. Annals of Medicine and Surgery 2020;59:180–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dixon S, Sharma M, Holtham S. Cholecystocutaneous fistula: an unusual complication of a para-umbilical hernia repair. BMJ Case Rep 2014;2014:bcr2013202417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nicholson T, Born MW, Garber E. Spontaneous cholecystocutaneous fistula presenting in the gluteal region. J Clin Gastroenterol 1999;28:276–7. [DOI] [PubMed] [Google Scholar]
- 7. Andersen P, Friis-Andersen H. Spontaneous cholecystocutaneous fistula presenting in the right breast. Ugeskr Laeger 2012;174:1235–6. [PubMed] [Google Scholar]
- 8. Gerrard A, Date R. Delayed spontaneous passage of gallstones via cholecystocutaneous fistula. ACG Case Rep J 2017;4:e102–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Hariharan D, Lobo DN. Spontaneous extrusion of gallstones after percutaneous drainage. Ann R Coll Surg Engl 2017;99:e1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pripotnev S, Petrakos A. Cholecystocutaneous fistula after percutaneous gallbladder drainage. Case Rep Gastroenterol 2014;8:119–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
De-identified data is available upon request from the corresponding author.


