Description
A 71-year-old man presented to our emergency department with reports of sudden onset breathlessness for 2 days and two episodes of frank blood in stools in the last 24 hours. Prior to these symptoms, the patient gave history of pain in the lower back region, which was present for the last 10 days along with swelling of both feet that was noticed around the same time. The patient was recently diagnosed to have severe COVID-19 infection and was treated for the same with intravenous steroid, low-molecular weight heparin (LMWH) and remdesivir. Initial d-dimer at the time of admission was 2.27 mg/L fibrinogen equivalent units (FEU). He was discharged 15 days before the onset of the current symptoms without any oral anticoagulant, d-dimer at discharge was 1.92 mg/L FEU.
On initial assessment, blood pressure was 120/90 mm Hg, pulse rate was 114 bpm, respiratory rate was 24 cycles/min and room air oxygen saturation was 89%. Clinical examination of the cardiovascular, respiratory and gastrointestinal (GI) systems was otherwise found to be normal.
Blood investigations revealed haemoglobin 61.2 g/L, packed cell volume 19.4% and platelet count 90x109/L. Coagulation profile done showed International Normalised Ratio (INR) 1.36, partial thromboplastin time 35.5 s (control 26.3 s), fibrinogen 373 mg/dL and d-dimer 14.72 mg/L FEU. Renal function test revealed a prerenal pattern acute kidney injury (blood urea nitrogen 24 mg/dL and creatinine 1.3 mg/dL). ECG showed sinus tachycardia with no ST-T changes.
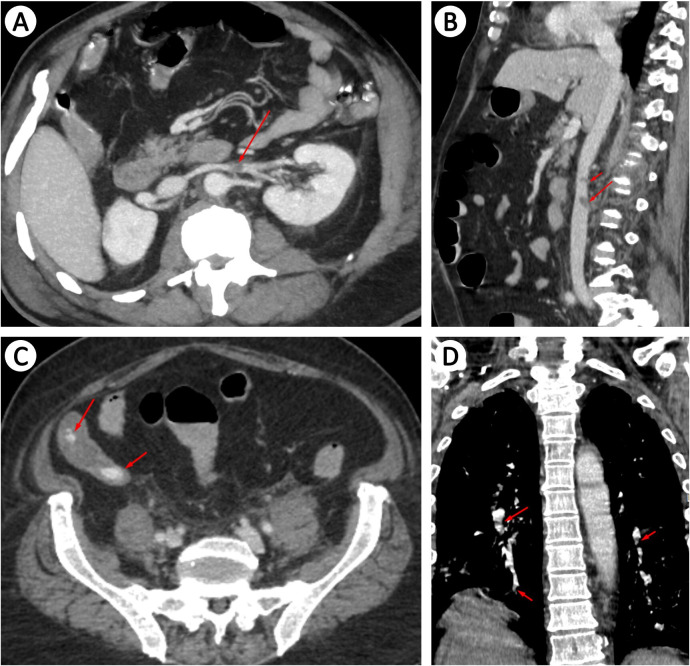
CT for pulmonary angiogram was done, which showed acute pulmonary thromboembolism involving the segmental and subsegmental branches of bilateral lower lobes. Abdominal angiogram showed a small thrombus of 9.6 mm is seen in the left renal vein and a small thrombus (9×8 mm) in the inferior vena cava. Postcontrast images revealed progressive accumulation of contrast material in the dependent portion of the terminal ileum suggestion an active bleed. Bilateral lower limb venous doppler ruled out the presence of deep vein thrombosis (figure 1).
Figure 1.
CT angiogram showing: (A) left renal vein thrombus (red arrow), (B) inferior vena caval thrombus (red arrow), (C) contrast leak seen in the ileum (red arrow) and (D) segmental and subsegmental pulmonary thromboembolism (red arrow).
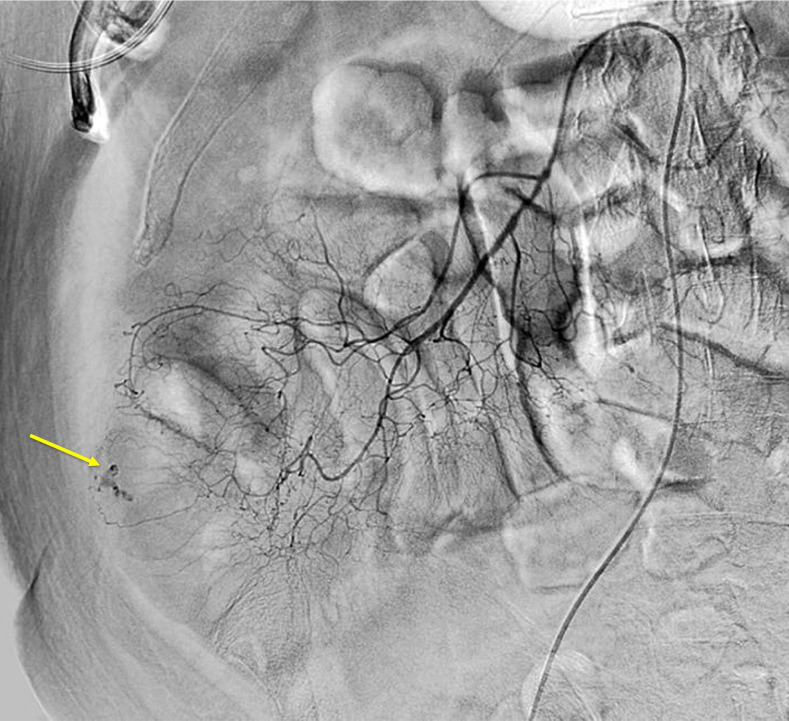
In view of venous thromboembolism (VTE) with concomitant lower GI bleeding, the interventional radiology team was involved. Patient underwent digital subtraction angiogram, which revealed active leak in the right ileac fossa supplied by the marginal branches of ileocecal artery. Poly-vinyl alcohol and gel foam embolisation were done and haemostasis was achieved (figure 2).
Figure 2.
Digital subtraction angiography showing bleed from the ileocecal artery (yellow arrow).
Patient was then initiated on anticoagulation with LMWH and was monitored in the intensive care unit. There was clinical recovery and no further episodes of haematochezia.
COVID-19 infection is associated with hypercoagulability.1 Increased risk of developing deep vein thrombosis and pulmonary thromboembolism (cumulative incidence of 2.5%) has been noted in patients who have recovered from COVID-19.2 It has been advised to prescribe patients with oral anticoagulant for 30 days in those who have an increased risk for VTE.3 Our patient happens to be the first case to be reported in the clinical literature to have presented with both VTE and ongoing bleed while not on prophylactic anticoagulation. The exact pathology that resulted in the GI bleed was not evaluated for as the patient did not consent for a colonoscopy. Nevertheless, the incidence of clinically significant bleeding in patients who have recovered from COVID-19 (not receiving prophylactic anticoagulation) was found to be 0.7%.2 Our patient manifested with features resultant of both pulmonary thromboembolism and volume depletion secondary to GI blood loss. Treatment is a challenge in such patients, given the presentation of venous thrombosis with ongoing haemorrhage.
Learning points.
COVID-19 infection leads to a hypercoagulable state.
Patients who have recovered from COVID-19 infection require appropriate follow-up postdischarge for a period of at least 30 days.
Patients at higher risk for thrombosis require prolonged anticoagulation following discharge while being monitoring for presence of bleeding manifestations.
Footnotes
Contributors: MAK: writing—original draft; MK—conceptualisation, writing—review and editing, supervision; JNA—conceptualisation, writing—review & editing.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Panigada M, Bottino N, Tagliabue P, et al. Hypercoagulability of COVID-19 patients in intensive care unit: a report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost 2020;18:1738–42. 10.1111/jth.14850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Patell R, Bogue T, Koshy A, et al. Postdischarge thrombosis and hemorrhage in patients with COVID-19. Blood 2020;136:1342–6. 10.1182/blood.2020007938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bikdeli B, Madhavan MV, Jimenez D, et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol 2020;75:2950–73. 10.1016/j.jacc.2020.04.031 [DOI] [PMC free article] [PubMed] [Google Scholar]