Abstract
COVID-19 infection affects different organ systems with long-term sequelae, which has been termed as long COVID-19 syndrome. To the best of our knowledge, osteonecrosis of the knee as a part of long COVID-19 syndrome has not been documented. Corticosteroids are being used extensively in moderate and severe cases of COVID-19. We report two cases who developed osteonecrosis of the knee after being treated for COVID-19 infection. In our case series, the mean cumulative dose of prednisolone was 1156.5 mg (900–1413 mg), which is less than the cumulative dose reported in literature for osteonecrosis of the knee. In our case series, the patients developed symptomatic osteonecrosis at a mean interval of 73 days after initiation of steroid therapy, with the earliest presenting at 25 days. Early diagnosis of osteonecrosis of the knee on high clinical suspicion by MRI would help in early intervention with bisphosphonate therapy.
Keywords: COVID-19, Orthopaedics, Drugs: musculoskeletal and joint diseases
Background
The ongoing COVID-19 pandemic is caused by the novel SARS-CoV-2 virus. Increasing evidence suggests that COVID-19 affects multiple organ systems such as respiratory, cardiac, gastrointestinal and musculoskeletal systems as a part of ‘long COVID-19’ syndrome. Long-COVID-19 syndrome is a term used to describe the long-term effects of COVID-19 infection, including ongoing symptomatic COVID-19 infection (from 4 weeks to 12 weeks) and post-COVID-19 syndrome (≥12 weeks) after the onset of COVID-19 infection.1 Symptoms of long-COVID include fatigue, palpitations, chest tightness, cognitive impairment or ‘brain fog’, dizziness, peripheral neuropathy, nausea, diarrhoea, joint and muscle pains, tinnitus, skin rashes, etc.2 Given the short history of the pandemic, the long-term complications of COVID-19 infection are yet to be studied.
Even though many drugs have been tried to treat COVID-19 infection, corticosteroids have been proven to be life-saving. However, corticosteroids have been shown to be a predisposing factor for developing avascular necrosis (AVN).3 A resurgence in AVN cases following COVID-19 infection is likely due to the rampant use of corticosteroids.4 AVN of the femoral head has been reported in patients with COVID-19 infection treated with corticosteroids.5 However, osteonecrosis of the knee following COVID-19 infection has not been reported previously in the literature. An early diagnosis of osteonecrosis of the knee is important to prevent subsequent arthritis and the need for surgery. If diagnosed in the early stages, osteonecrosis of the knee responds well to bisphosphonate therapy.6
Here we report two cases of symptomatic osteonecrosis of the knee as part of the long-term complications of COVID-19 infection. This is the first case series of knee osteonecrosis reported worldwide as part of long COVID-19 syndrome.
Case presentation
Case 1
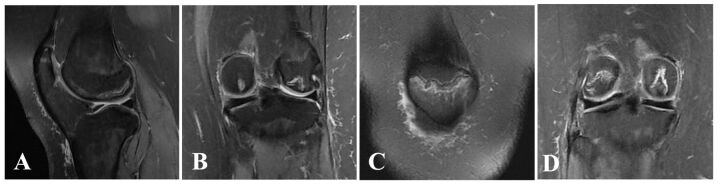
A woman in her 20s with no medical comorbidities was diagnosed with COVID-19 infection and managed at home. The patient was treated with oral methylprednisolone 16 mg three times a day for 15 days (cumulative steroid dose equivalent to 900 mg of prednisolone). She developed pain in both knees 25 days after diagnosis of COVID-19 infection, which did not settle on conservative management. On suspicion, an MRI of both knees was done, which confirmed bilateral osteonecrosis of femoral condyles and patella (figure 1). The patient was started on oral alendronate 70 mg/week in two divided doses along with a single dose of intravenous zoledronic acid 5 mg. This was supplemented with calcium, vitamin D and anti-inflammatory medications. On follow-up at 3 months, Pain Visual Analogue Score reduced from 8 to 2, and the patient was comfortable with no progression of the osteonecrosis on follow-up radiographs. The patient was able to resume her routine activities comfortably.
Figure 1.
MRI of a female patient in her 20s confirming osteonecrosis of both condyles and patella: (A,B) left knee and (C,D) right knee.
Case 2
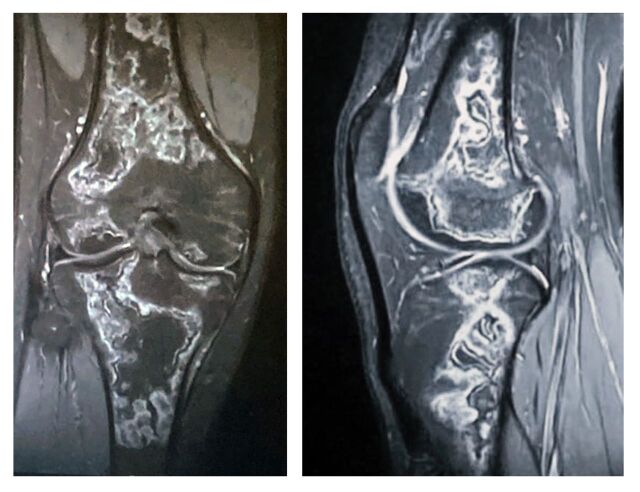
A male patient in his late teens presented to us with complaints of pain in the right knee and both hips. The patient had COVID-19 infection 4 months previously, for which he was admitted and treated with injection of methylprednisolone and dexamethasone tablet over 19 days with a dose equivalent to 1413 mg of prednisolone. MRI of the patient showed osteonecrosis of the right knee involving the distal femur and proximal tibia and Ficat-Arlet stage III AVN of both hips (figure 2). The patient was started on bisphosphonate therapy as per our protocol and was clinically better at 3 months of follow-up.
Figure 2.
MRI of a male patient in his late teens confirming osteonecrosis of the right knee involving distal femur and proximal tibia.
Outcome and follow-up
The cumulative prednisolone equivalent steroid taken by the patients in our case series ranged from 900 mg to 1413 mg with a mean of 1156.5 mg. The interval between initiation of corticosteroid therapy and development of symptomatic osteonecrosis was 25 days in the first case and 4 months in the second case, with a mean duration of 73 days. Both patients were started on oral alendronate 70 mg/week in two divided doses along with a single dose of intravenous zoledronic acid 5 mg. Both patients were clinically better on follow-up at 3 months with no progression of osteonecrosis on radiographs.
Discussion
Osteonecrosis most frequently affects the hips, followed by the knee.7 Osteonecrosis of the knee was first described by Ahlbäck et al in 19688 and can be classified as (1) spontaneous osteonecrosis of the knee (also called primary osteonecrosis) usually affects the elderly population and single condyle; (2) secondary osteonecrosis (also called atraumatic osteonecrosis) usually affects younger individuals and both condyles; it is usually associated with corticosteroid use, renal disease, haematological disorders, etc; and (3) post-arthroscopy usually affects a single condyle.9
Multiple classes of drugs have been studied for the management of moderate and severe COVID-19 infection. Among those, corticosteroids have been found to be life-saving in severe cases of COVID-19 infection.10 However, they are also known to be an independent risk factor for the development of osteonecrosis. The pathogenesis of osteonecrosis is not entirely understood but is believed to be multifactorial. Vascular occlusion, fat cell hypertrophy, fat emboli, hypercoagulability and vascular endothelial dysfunction are some of the mechanisms postulated in the pathogenesis of osteonecrosis.11 It is postulated that hypercoagulability, leucocyte aggregation and endothelial dysfunction, in addition to the use of corticosteroids in COVID-19 infection, can contribute to the development of osteonecrosis.12
Studies have shown that cumulative doses of steroids may be an important factor for osteonecrosis.13 However, there is no consensus regarding the exact dosage and duration of steroid usage, which can lead to the development of osteonecrosis. A review of literature showed reports of osteonecrosis of the knee with cumulative doses ranging from 1012 mg to 6562 mg of prednisolone.3 14–16 In our patients, the cumulative dose ranged from 900 mg to 1413 mg of prednisolone with a mean dose of 1156.5 mg.
After initiation of corticosteroid therapy, osteonecrosis can develop as early as within 1 year.13 Oinuma et al, in their case series, showed that osteonecrosis of the hips and the knee could be detected in 44% of patients with systemic lupus erythematous at an average of 3.1 months from corticosteroid therapy use.17 However, rare cases have been reported even within 1 month of initiation of corticosteroid therapy, as reported by Yildiz et al in a patient with idiopathic thrombocytopenic purpura.18 In the cases we report here, one of the patients developed symptomatic osteonecrosis of the knee very early (25 days after initiation of corticosteroid therapy) with an average onset at 73 days.
In our case series, one patient with knee osteonecrosis had concomitant AVN of the hips. Patients with osteonecrosis of the hip often present with referred pain in the thigh and knee owing to the sensory distribution of the obturator and femoral nerves.19 Therefore, a thorough clinical examination of the knee joint with high suspicion for the possibility of concomitant osteonecrosis of the knee is necessary for diagnosis and intervention.
The primary objective for treating osteonecrosis of the knee is to address pain, slow the disease progression and prevent bone collapse and joint arthritis. Multiple treatment options exist in the form of conservative, medical and surgical management; however, no standard therapeutic management protocols exist.20 Arthroplasty remains the mainstay of treatment of osteonecrosis once arthritis sets in. Agarwala et al showed that osteonecrosis of the knee responds well to medical management with combination bisphosphonate therapy in the early stages, but it is imperative to diagnose and intervene early.6 The protocol followed by the author was a single intravenous dose of 5 mg of zoledronic acid with 70 mg oral alendronate weekly divided into two doses. Jureus et al showed good outcome in 59% of patients with knee osteonecrosis treated with oral bisphosphonates in their study.21 Kraenzlin et al in their case series showed that patients treated with combination bisphosphonate therapy (intravenous pamidronate and oral alendronate) had rapid improvement in pain score and radiological consolidation of the area of osteonecrosis.22 Sixty-seven per cent of patients in their series showed complete resolution of bone marrow oedema in follow-up MRI at 2–3 months. Bisphosphonate therapy is now considered a standard option for the treatment of osteonecrosis with good clinical outcomes.23 Our patients were started on bisphosphonate combination therapy with good clinical response.
Learning points.
Corticosteroids have been proven to be life-saving in the present COVID-19 pandemic.
Patients seem to be more susceptible to osteonecrosis following COVID-19 infection, as witnessed by an increased incidence, at a lower dose of corticosteroids and early onset of symptomatic osteonecrosis.
In the early stages, osteonecrosis of the knee responds well to bisphosphonate therapy.
Early diagnosis by MRI on clinical suspicion would help in early intervention with bisphosphonate therapy in patients with knee joint complaints following COVID-19 infection.
Footnotes
Contributors: All authors contributed towards the conception and design of the article, planning, conduct, reporting, acquisition and interpretation of data.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1. The Lancet . Understanding long COVID: a modern medical challenge. Lancet 2021;398:725. 10.1016/S0140-6736(21)01900-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Overview | COVID-19 rapid guideline: managing the long-term effects of COVID-19 | guidance | NICE. Available: https://www.nice.org.uk/guidance/ng188 [Accessed 18 Oct 2021].
- 3. Powell C, Chang C, Naguwa SM, et al. Steroid induced osteonecrosis: an analysis of steroid dosing risk. Autoimmun Rev 2010;9:721–43. 10.1016/j.autrev.2010.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zhang S, Wang C, Shi L, et al. Beware of steroid-induced avascular necrosis of the femoral head in the treatment of COVID-19-Experience and lessons from the SARS epidemic. Drug Des Devel Ther 2021;15:983–95. 10.2147/DDDT.S298691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Agarwala SR, Vijayvargiya M, Pandey P. Avascular necrosis as a part of 'long COVID-19'. BMJ Case Rep 2021;14:e242101. 10.1136/bcr-2021-242101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Agarwala S, Sharoff L, Jagani N. Effect of zoledronic acid and alendronate on bone edema and pain in spontaneous osteonecrosis of the knee: a new paradigm in the medical management. Rev Bras Ortop 2020;55:543–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Assouline-Dayan Y, Chang C, Greenspan A, et al. Pathogenesis and natural history of osteonecrosis. Semin Arthritis Rheum 2002;32:94–124. 10.1053/sarh.2002.33724b [DOI] [PubMed] [Google Scholar]
- 8. Ahlbäck S, Bauer GC, Bohne WH. Spontaneous osteonecrosis of the knee. Arthritis Rheum 1968;11:705–33. 10.1002/art.1780110602 [DOI] [PubMed] [Google Scholar]
- 9. Karim AR, Cherian JJ, Jauregui JJ, et al. Osteonecrosis of the knee: review. Ann Transl Med 2015;3:6. 10.3978/j.issn.2305-5839.2014.11.13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Mouffak S, Shubbar Q, Saleh E, et al. Recent advances in management of COVID-19: a review. Biomed Pharmacother 2021;143:112107. 10.1016/j.biopha.2021.112107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kerachian MA, Séguin C, Harvey EJ. Glucocorticoids in osteonecrosis of the femoral head: a new understanding of the mechanisms of action. J Steroid Biochem Mol Biol 2009;114:121–8. 10.1016/j.jsbmb.2009.02.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Disser NP, De Micheli AJ, Schonk MM, et al. Musculoskeletal consequences of COVID-19. J Bone Joint Surg 2020;102:1197–204. 10.2106/JBJS.20.00847 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Chan KL, Mok CC. Glucocorticoid-Induced avascular bone necrosis: diagnosis and management. Open Orthop J 2012;6:449–57. 10.2174/1874325001206010449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Braverman DL, Lachmann EA, Nagler W. Avascular necrosis of bilateral knees secondary to corticosteroid enemas. Arch Phys Med Rehabil 1998;79:449–52. 10.1016/S0003-9993(98)90148-4 [DOI] [PubMed] [Google Scholar]
- 15. Takeda H, Nishise S, Fujishima S, et al. Osteonecrosis of the lateral femoral condyle in a patient with ulcerative colitis: report of a case. Clin J Gastroenterol 2008;1:93–6. 10.1007/s12328-008-0015-2 [DOI] [PubMed] [Google Scholar]
- 16. Hussain A, Young WB. Steroids and aseptic osteonecrosis (AON) in migraine patients. Headache J Head Face Pain 2006. [DOI] [PubMed] [Google Scholar]
- 17. Oinuma K, Harada Y, Nawata Y, et al. Osteonecrosis in patients with systemic lupus erythematosus develops very early after starting high dose corticosteroid treatment. Ann Rheum Dis 2001;60:1145–8. 10.1136/ard.60.12.1145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Yildiz N, Ardic F, Deniz S. Very early onset steroid-induced avascular necrosis of the hip and knee in a patient with idiopathic thrombocytopenic purpura. Intern Med 2008;47:1989–92. 10.2169/internalmedicine.47.1038 [DOI] [PubMed] [Google Scholar]
- 19. Sakamoto J, Morimoto Y, Ishii S, et al. Investigation and macroscopic anatomical study of referred pain in patients with hip disease. J Phys Ther Sci 2014;26:203–8. 10.1589/jpts.26.203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mont MA, Baumgarten KM, Rifai A, et al. Atraumatic osteonecrosis of the knee. J Bone Joint Surg Am 2000;82:1279–90. 10.2106/00004623-200009000-00008 [DOI] [PubMed] [Google Scholar]
- 21. Jureus J, Lindstrand A, Geijer M. Treatment of spontaneous osteonecrosis of the knee (SPONK) by a bisphosphonate: a prospective case series with 17 patients. Acta Orthop 2012;83:511–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Kraenzlin ME, Graf C, Meier C, et al. Possible beneficial effect of bisphosphonates in osteonecrosis of the knee. Knee Surg Sports Traumatol Arthrosc 2010;18:1638–44. 10.1007/s00167-010-1106-4 [DOI] [PubMed] [Google Scholar]
- 23. Agarwala S, Banavali SD, Vijayvargiya M. Bisphosphonate combination therapy in the management of Postchemotherapy avascular necrosis of the femoral head in adolescents and young adults: a retrospective study from India. J Glob Oncol 2018;4:1–11. 10.1200/JGO.17.00083 [DOI] [PMC free article] [PubMed] [Google Scholar]