Abstract
A 59-year-old man presented to the emergency department with recent onset biphasic stridor, dyspnoea and increased work of breathing on the background of prolonged intubation for the novel COVID-19 2 months previously. Flexible laryngoscopy revealed bilateral vocal fold immobility with a soft tissue mass in the interarytenoid region. The patient’s symptoms improved with oxygen therapy, nebulised epinephrine (5 mL; 1:10 000) and intravenous dexamethasone (3.3 mg). The following morning, the patient was taken to theatre, underwent suspension microlaryngoscopy and found to have bilateral fixation of the cricoarytenoid joints and a large granuloma in the interarytenoid area. He underwent cold steel resection of the granuloma and balloon dilatation between the arytenoids, with the hope of mobilising the joints. This failed and CO2 laser arytenoidectomy was performed on the left side. The stridor had resolved postoperatively, with normalisation of work of breathing and the patient was discharged home on the first postoperative day.
Keywords: ear, nose and throat/otolaryngology, adult intensive care, otolaryngology / ENT
Background
On 11 March 2020, COVID-19 was declared as a worldwide pandemic1 with never before seen numbers of patients requiring mechanical ventilation and threatening to overwhelm the most well-resourced health systems in the world.2
During the pandemic, duration of endotracheal intubation prior to tracheostomy insertion in these patients was considerably prolonged beyond the typical 7–14 days.3 Reasons for delaying tracheostomy insertion are multivariate, including need for high ventilation pressures, cardiovascular instability and need for nursing in the prone position. Due to the high viral concentration in the upper aerodigestive tract,4 5 delays also occurred due to the concern of cross-infection of healthcare professionals both performing a tracheostomy and those looking after it. The British Laryngological Association also recommended that patients have two negative viral PCR swabs 48 hours apart prior to surgical tracheostomy insertion.6 Thus, many of these patients experienced periods of endotracheal intubation up to 3 weeks or 4 weeks and a large increase in presentations of iatrogenic airway injury is expected in the coming months.3
We report a case of COVID-19-related airway stenosis in a patient intubated during the pandemic. Laryngotracheal stenosis, including webs, granulomas and tracheal necrosis, are well-recognised iatrogenic sequelae of prolonged intubation,7 though bilateral vocal fold fixation is less common. We highlight a safe and effective surgical procedure to relieve airway obstruction from bilateral cricoarytenoid fixation that would ordinarily have required tracheostomy insertion. We hope to highlight the expected surge of airway injuries over the short to medium term and increase appreciation of this rarer complication as well as a safe and effective alternative to tracheostomy insertion.
Case presentation
A 59-year-old man presented to the emergency department with biphasic stridor, dyspnoea and increased work of breathing on the background of prolonged intubation for COVID-19 2 months previously. The patient had been intubated with a size seven endotracheal tube for 17 days and been intermittently nursed in the prone position before being successfully extubated and discharged home after a 42-day inpatient hospital stay. Observations on arrival included O2 saturations of 99% on room air, respiratory rate of 16 RPM, heart rate of 100 beats/minute and blood pressure of 152/86 mm Hg. The patient had moderate increased work of breathing and biphasic stridor at rest. Flexible laryngoscopy revealed bilateral vocal fold immobility with the cords fixed in the paramedian position and a soft tissue mass in the interarytenoid region. The patient’s symptoms improved with oxygen therapy via face mask, nebulised epinephrine(5 mL; 1:10,000) and intravenous dexamethasone (3.3 mg).
Treatment
The following morning, the patient was taken to theatre and underwent suspension microlaryngoscopy. Personal protective equipment was used for all staff in the theatre consisting off visors, FFP3 masks, long-sleeved gowns and gloves. Intravenous propofol was used to induce general anaesthesia intravenously following which atracurium was administered as muscle relaxant. A laryngeal mask airway (LMA) was placed through which positive pressure ventilation was delivered. The LMA was removed by the operating surgeon immediately prior to direct laryngoscopy using a Dedo-Pilling laryngoscope (Pilling Weck Teleflex, Morrisville, North Carolina, USA). The larynx was suspended using a Pilling Laryngoscope Holder mounted on a board above the patient’s chest. High frequency automated supraglottic jet ventilation (Monsoon 3, Acuatronic, Switzerland) was used to maintain ventilation throughout the procedure lasting 25 min.
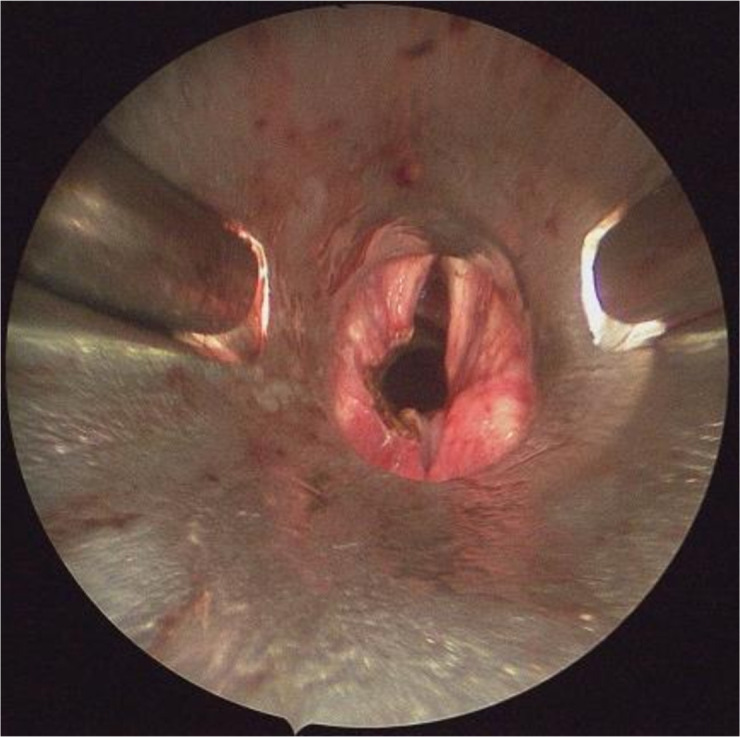
Direct laryngoscopy was performed using a Hopkins Rod (Karl Storz SE & Co KG, Germany) and bilateral cricoarytenoid joint fixation was confirmed through palpation. An interarytenoid granuloma was also diagnosed (figure 1). The subglottis and distal airway were not involved (figure 2). The granuloma was resected using cold steel. Balloon dilation to 19 mm was next performed using a CRE Balloon Dilation Catheter (Boston Scientific, Marlborough, Massachusetts, USA) for 60 s. This did not achieve mobile joints. A partial left-sided arytenoidectomy was performed using the CO2 laser (Lumenis (UK) Ltd, Manchester, UK) at 10 W and superpulse mode. Resection was carried out until a smooth longitudinal path was formed through the arytenoid and into the subglottis, thus allowing laminar flow of air through the glottis (figure 3).
Figure 1.

Preoperative image showing vocal folds in paramedian position and interarytenoid granuloma.
Figure 2.

Distal airway not involved.
Figure 3.
Postoperative image showing partial arytenoidectomy on the left side.
The procedure duration was 38 min. At the end of the operation, the laryngoscope was removed and the LMA was again used to secure a supraglottic airway. Paralysis was monitored throughout the procedure with train-of-four ulnar nerve stimulation, and was reversed with 2.5 mg of neostigmine and 500 mcg of glycopyrrolate (Robinul-Neostigmine Injection, Anpharm, Tipperary, Ireland) at the end of the procedure to optimise re-establishment of spontaneous ventilation. The patient was ventilated until the now-unencumbered spontaneous breathing was re-established.
Outcome and follow-up
Postoperatively, the stridor had resolved and the work of breathing returned to normal. The patient was transferred to the Ear, Nose and Throat ward. Later that day, he underwent fiberoptic endoscopic evaluation of swallowing, which revealed no evidence of penetration or aspiration. The patient was observed overnight and discharged home on the first postoperative day. Arrangements were made for the patient to have airway clinic review in 2 weeks time for fiberoptic assessment of the glottis and subglottis and thereafter will be followed via telephone clinic on a 6–12 weekly basis. Histopathology samples taken during the procedure confirmed a posterior commissure granuloma.
Discussion
Published in June 2020, the ‘Call to Action’ of the European Laryngological Society3 highlights an expected unprecedented increase in iatrogenic airway stenoses in the coming months. Patients requiring mechanical ventilation for COVID-19 suffered prolonged endotracheal intubation due to the need for high ventilation pressures, nursing in the prone position (higher risk of decannulation) and high viral concentration in the upper aerodigestive tract leading to possible infection of healthcare providers during and after tracheostomy insertion.
Common symptoms of laryngotracheal stenosis include dry cough, hoarseness, swallow dysfunction and at a more advanced stage, stridor. Early diagnosis and treatment of these cases have been shown to yield superior therapeutic outcomes7 and prevent long-term sequelae. A study of 62 patients from our institution showed that endoscopic surgery can be an effective strategy for definitively treating postintubation tracheal stenosis in most patients.8 Rigid bronchoscopic intervention is a cogent alternative in cases of subglottic and tracheal stenoses,9 though would be unsuitable for glottic pathology as in this case. Suspension laryngoscopy allowed CO2 laser arytenoidectomy, which created a patent airway in the posterior third of the glottis thus avoiding a tracheostomy.
Patients with long-term airway stenosis are often misdiagnosed with respiratory conditions such as asthma and thus suffer delays in initiation of diagnostic and therapeutic interventions. It is important to promote a high index of suspicion among general practitioners, emergency medicine and respiratory physicians in order to facilitate early diagnosis and maximise patient outcomes.
To the best of our knowledge, this is the first case report of iatrogenic laryngotracheal stenosis published in the scientific literature. Laser arytenoidectomy was used to obviate the need for tracheostomy insertion. The patient experienced rapid relief of their symptoms and a foreshortened inpatient stay.
Learning points.
Patients with COVID-19 are at a high risk of airway stenosis due to remaining intubated much longer than standard due to the need for high ventilation pressures, nursing in the prone position and cross-infection issues. We expect a large volume of COVID-19-related airway stenosis in the next 3–6 months and sharing of experience is essential.
In this case, laser arytenoidectomy was used to obviate the need for tracheostomy insertion. The patient experienced rapid relief of their symptoms and significant reduction in morbidity and inpatient hospital stay.
Endoscopic management of airway stenosis can be performed safely using jet ventilation and CO2 laser as described, as long as infection control and personal protective equipment guidelines are followed.
Footnotes
Contributors: GT and HL were involved in drafting the manuscript. GT, CAY and GSS were involved in revisions.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.World Health Organization . Rolling updates on coronavirus disease (COVID-19). Available: https://www%20.who.int/emergencies/diseases/novel-coronavirus-2019/eventsas-they-happen [Accessed 17 Apr 2020].
- 2.Kowalski LP, Sanabria A, Ridge JA, et al. COVID-19 pandemic: effects and evidence-based recommendations for otolaryngology and head and neck surgery practice. Head Neck 2020;42:1259–67. 10.1002/hed.26164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Piazza C, Filauro M, Dikkers FG, et al. Long-Term intubation and high rate of tracheostomy in COVID-19 patients might determine an unprecedented increase of airway stenoses: a call to action from the European Laryngological Society. Eur Arch Otorhinolaryngol 2020:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.To KK-W, Tsang OT-Y, Leung W-S, et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: an observational cohort study. Lancet Infect Dis 2020;20:565–74. 10.1016/S1473-3099(20)30196-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheng X, Liu J, Li N, et al. Otolaryngology providers must be alert for patients with mild and asymptomatic COVID-19. Otolaryngol Head Neck Surg 2020;162:809–10. 10.1177/0194599820920649 [DOI] [PubMed] [Google Scholar]
- 6.. Available: https://www.entuk.org/sites/default/files/BLA%20Tracheostomy%20guideline%20-BLA%20April%202020%20final.pdf
- 7.Mehel DM, Özdemir D, Çelebi M, et al. Classification of laryngeal injury in patients with prolonged intubation and to determine the factors that cause the injury. Am J Otolaryngol 2020;41:102432. 10.1016/j.amjoto.2020.102432 [DOI] [PubMed] [Google Scholar]
- 8.Nouraei SAR, Ghufoor K, Patel A, et al. Outcome of endoscopic treatment of adult postintubation tracheal stenosis. Laryngoscope 2007;117:1073–9. 10.1097/MLG.0b013e318050ca12 [DOI] [PubMed] [Google Scholar]
- 9.Madan K, Agarwal R, Aggarwal AN, et al. Utility of rigid bronchoscopic dilatation and mitomycin C application in the management of postintubation tracheal stenosis: case series and systematic review of literature. J Bronchology Interv Pulmonol 2012;19:304–10. 10.1097/LBR.0b013e3182721290 [DOI] [PubMed] [Google Scholar]


