Abstract
Six days after a normal delivery, a 24-year-old woman with atraumatic lumbosacral pain radiating to the left groin was referred to the orthopaedic surgeon due to worsening pain and impossible load bearing on the left lower limb. Standard pelvic radiographs revealed an unstable displaced left neck of femur (NOF) fracture. A CT scanner and MRI showed diffuse osteopaenia of the left proximal femur and the corresponding acetabulum. A diagnosis of transient osteoporosis of the hip (TOH) complicated by a pathological displaced subcapital NOF fracture was established. The patient underwent total hip arthroplasty without complication and recovered excellent function after rehabilitation. Awareness of the differential diagnosis of TOH in pregnancy, a high index of suspicion and early MRI to make an early diagnosis and to prevent devastating fracture complications are mandatory.
Keywords: hip prosthesis implantation, pregnancy, osteoporosis
Background
Transient osteoporosis of the hip (TOH) during pregnancy is a well-known disease occurring most of the time in the third trimester.1–4 The exact cause remains unknown but is considered multifactorial.1 2 The typical complaints are groin pain and loss of function without notion of trauma.1 Under adapted limb discharge the disease is most often benign with progressive relief of symptoms,1 5 6 but it has the potential to lead to a severe complication of an unstable neck of femur (NOF) fracture requiring arthroplasty at young age. Atraumatic pelvic or groin pain is not uncommon in pregnancy.7 Therefore, it must raise a high index of suspicion of TOH and must be followed by a thorough clinical examination. To make a definitive diagnosis of TOH, MRI is the best method.3 7 Once diagnosed, we are at ease to implement efficient prophylactic measures and prevent a pathological fracture. We report a case of undiagnosed TOH which was complicated by a pathological NOF fracture with indication for total hip arthroplasty (THA) in a young patient. This case highlights that general practitioners, gynaecologists/obstetricians, midwives and orthopaedic surgeons must be aware of TOH and its potential complications and the need for early MRI in case of a clinical suspicion.
Case presentation
A 24-year-old Caucasian patient, gravida 1, para 0, pregnant in her third trimester, presented to the emergency room in January 2019 with progressive left lower back pain radiating to the ipsilateral groin and knee. Symptoms began about 4 weeks prior and the patient had already consulted her gynaecologist, her general practitioner as well as an osteopath with transitory pain relief. She had also consulted a neurologist who investigated the lumbar spine exclusively with an MRI scan showing a small herniated disc without signs of nerve compression. Her personal and familial history did not reveal any specific immunological, rheumatological or osteoarticular disorder. She described having caries in childhood. Previous tobacco and alcohol consumption was occasional and she did not have any treatment with cortisone or other steroids in the past.
Clinical examination showed an increased body mass index of 40 and general joint hyperlaxity of the elbows and fingers without skin laxity. Pain was reproduced during left paralumbar palpation and during passive rotation of the hip without limitation in the range of motion (ROM). With the known diagnosis of disc herniation and in the absence of a neurological deficit, no complementary plain radiographs were undertaken during pregnancy and a clinical diagnosis of simple lower back pain was documented. Rest and pain medication were prescribed without particular instructions regarding weightbearing. Two months later, the patient gave birth to a healthy girl (2650 g, 46 cm) under epidural anaesthesia. After birth, the pain worsened and a second lumbar MRI revealed a progressive disc herniation without nerve compression. Six days after delivery, load bearing on the left hip became impossible and the patient was then referred to the orthopaedic surgeon for further assessment.
Investigations
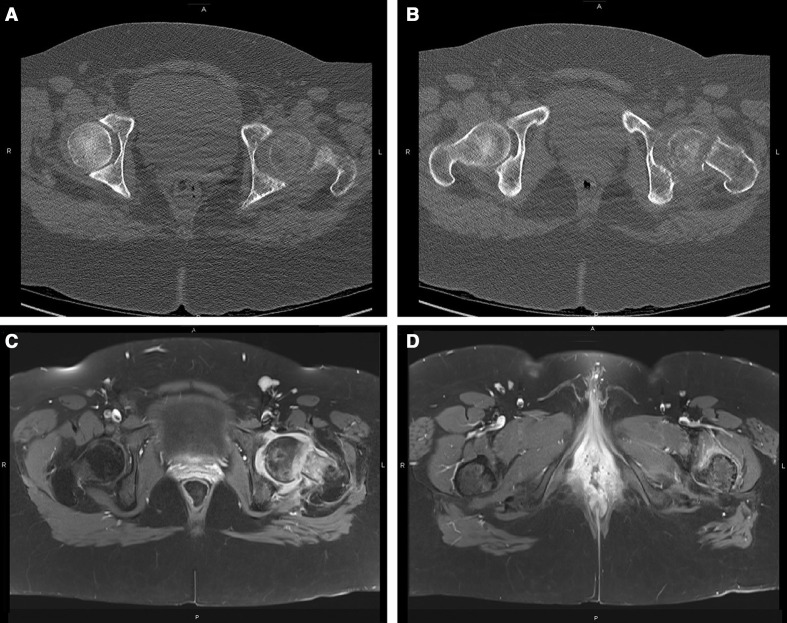
A pelvic radiograph (figure 1) demonstrated an unstable subcapital left NOF fracture associated with diffuse osteopaenia around the proximal femur and the acetabulum. The work-up was completed with CT scan and MRI in order to exclude an underlying pathological process (figure 2). All the elements were in keeping with the diagnosis of TOH complicated by a pathological NOF fracture.
Figure 1.
Radiograph of the pelvis showing a displaced left femoral neck fracture with diffuse osteopaenia around the proximal femur and the acetabulum.
Figure 2.
Axial CT scan demonstrating left hip osteopaenia with femoral head and neck hypodensity and neck fracture (A,B). Axial MRI T1 FAT SAT sequences with gadolinium contrast injection showing a hyposignal on the left femoral head with bone marrow oedema and joint effusion (C) as well as normalisation of the signal distally (D).
After surgery, bone density was measured by dual-energy X-ray absorptiometry and showed a lumbar Z-score of −2.2 SD and a T-score of −2.3 SD; both the Z-score and the T-score of the right hip were at −0.4 SD. The lumbar spine trabecular bone score was 1.2. These results suggested lumbar osteopaenia with slight alterations in bone structure. Pathological examination of the femoral head (figure 3) confirmed fracture signs with bone reparation and a few foci of subchondral osteonecrosis. On histology, no cytonuclear atypia was noted and the cartilage was normal. A rheumatological consultation and a detailed laboratory investigation, including phosphate–calcium balance, hepatic functions, vitamins (B9, B12, D), hormones (thyroid-stimulating hormone, parathyroid hormone and oestradiol), serology (HIV, syphilis, hepatitis, toxoplasmosis), electrophoresis and urine sample analysis, were normal. Non-specific inflammatory markers were slightly raised (C reactive protein: 18 mg/dL; erythrocyte sedimentation rate: 45 mm/hour) and attributed to the recent intervention and pregnancy.
Figure 3.
Left femoral head with shiny and smooth cartilage and numerous necrotic fragments.
Differential diagnosis
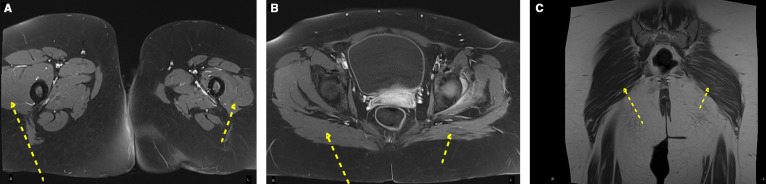
MRI is the gold standard investigation allowing the precise diagnosis of TOH and distinction of its differential diagnoses.3 5–7 It is more sensitive than plain radiographs and already shows signs of TOH 48 hours after the onset of pain.3 4 8 Differential diagnoses of TOH are avascular necrosis (AVN) of the femoral head, instability of the pubic symphysis, tumour, septic arthritis, stress fracture and osteomyelitis.9 10 MRI also gives some indirect sign of advanced TOH with gluteal and quadricipital atrophy4 as a result of limb inactivity (figure 4).
Figure 4.
Axial MRI T1 FAT SAT sequences with gadolinium injection showing left quadricipital (A, arrows) and gluteal (B, arrows) atrophy. Coronal MRI T1 demonstrating left gluteal atrophy (C, arrows).
It is particularly important to differentiate AVN of the femoral head from TOH. In the past, AVN was considered an advanced stage of TOH but this concept has been refuted.11 The treatment for these two entities is different, with surgical treatment in AVN and non-operative treatment in non-complicated TOH.4
In TOH, MRI shows a hypointense femoral head and neck signal in T1 and a hyperintense homogenous and diffuse signal (bone marrow oedema) in T2 with joint space preservation.8 T1 FAT SAT sequences with gadolinium contrast injection display a hyposignal on the femoral head with bone marrow oedema and joint effusion (figure 2). AVN of the femoral head presents two T2 signals representing sclerotic bone and vascularised tissue.4 Involvement is focal and not homogenous. Sometimes, a subchondral crescent sign can be seen in the femoral head, a pathognomonic sign of bone resorption and a direct threat for chondral collapse.3 4 6 8
Treatment
Once the complication of a pathological displaced NOF fracture was confirmed, the patient underwent urgent uncemented THA with hard-on-hard ceramic bearing. A classic posterior approach was undertaken under spinal anaesthesia. The THA was uneventful without complications. Physiotherapy was commenced the day after surgery and the patient was able to walk and to climb stairs rapidly after surgery with minimal pain and simple analgesia. Additional rheumatological advice was sought in order to confirm TOH and to exclude any other biological disorder. Ten days after surgery, the patient was discharged from hospital and returned home with her newborn.
Outcome and follow-up
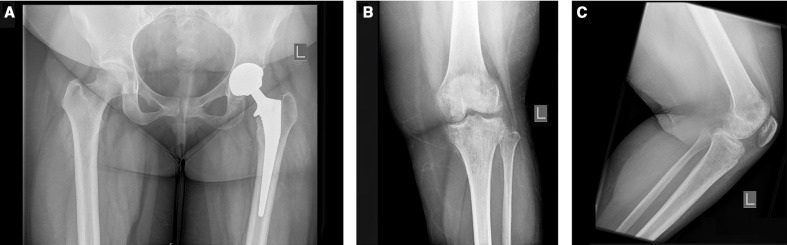
Six weeks after surgery, the plain radiographs showed a well-implanted uncemented left THA (figure 5). The osteopaenia of the proximal femur and the acetabulum were almost resolved. The patient still complained of left knee pain, with radiographs showing femorotibial and fibular osteopaenia (figure 5). After seeking further advice from rheumatology, the decision was made to follow the patient up on an annual basis without additional specific treatment.
Figure 5.
Radiographs at 6 weeks after left non-cemented total hip arthroplasty without signs of complications with almost resolved coxofemoral osteopaenia (A). Left knee showing a periarticular, femorotibial and fibular osteopaenia (B,C).
Discussion
TOH is a rare self-limiting disease with an unknown specific aetiology which is probably multifactorial.1 2 Although the hip joint is most frequently affected, transient osteoporosis can also occur in other localisations, notably on the knee, the lumbar vertebrae, the ankle and the foot.8 Transient osteoporosis concerns both genders, with a male to female ratio of 3:1. Middle-aged men between 40 and 60 years of age are primarily affected and women mostly during their first pregnancy at the end of the second trimester until a few weeks post partum.4 5 Of patients suffering from TOH 40% may develop the disease in other joints simultaneously or later on.6 The described case shows the association of transient osteoporosis of the hip and knee, which is known to be very rare.12
The first symptoms of TOH are groin pain of the affected side without any local or systemic inflammatory sign. Laboratory studies are usually non-contributive.5 9 13 Associated with pain, patients experience limitation in ROM of the hip (rotation and abduction) and painful or even impossible weightbearing.4 5 Trauma is rarely associated. The vast majority of patients with TOH have unilateral disease, but bilateral cases have also been described in the literature.1 5–7 14
The pathophysiology of pregnancy-related TOH is partially understood. An abnormal, exacerbated response of normal bone to hormonal changes is one of the hypotheses.1 Another is the role of pregnancy as a stressor that leads to a preosteoporotic condition.1 Further aetiological theories are transitory ischaemic episodes, hyperaemic states of adjacent bones,4 venous femoral stasis resulting from uterine pressure, obturator nerve compression by the fetus, viral infections, trauma or repetitive microtrauma.2
It is a known fact that pregnancy, tobacco abuse and low oral calcium intake are major risk factors for the development of TOH.1 3 8 Alcohol consumption and chronic corticosteroid use are risk factors mostly for AVN of the femoral head.13 Hadji et al2 led a case–control study comparing 33 pregnant patients suffering from TOH with 33 control cases. They found an association between dental issues, typically caries during childhood, and TOH (p=0.023, χ2 test). More patients with TOH were also overweight (30% vs 6%; p=0.023, χ2 test).
After diagnosis of TOH, some authors1 recommend stopping breast feeding, having a negative impact on the phosphocalcic balance resulting in bone loss. Oral calcium supplementation does not seem to compensate for this phenomenon. In this pathological state, Chalouhi et al5 found a higher risk for pathological fractures during lactation (56%) compared with pregnancy (41%) and delivery (6%). Non-weightbearing and supportive medication are the standard of care for TOH.5 6 Drugs and molecules such as calcitonin, bisphosphonates and teriparatide only proved to be efficient regarding the duration of symptoms (bone marrow oedema resorption) without evidence of any other therapeutic advantage.1 4 In general, TOH progresses and resolves spontaneously in three phases3 4:
First phase: 1–2 months of groin discomfort with variable degree of functional impairment. Plain radiographs are usually normal at this stage. The first radiographic signs are seen 4–8 weeks after the onset of pain.4 6 8
Second phase: the duration of this phase is approximately 3 months with frank radiographic osteopaenia.
Third phase: symptoms disappear progressively and normal bone mineralisation is obtained within 6–12 months.1
Complications of TOH such as fractures are almost always treated surgically. Willis-Owen et al7 reported the case of a 34-year-old patient, gravida 1, para 1, diagnosed with bilateral TOH complicated by bilateral NOF fractures. Both sides were treated by internal fixation with dynamic hip screws. The authors reported difficulties with full weightbearing during 3 months and satisfactory outcomes. Chalouhi et al5 described the condition of a patient with right groin pain at 32 weeks of gestation. Following investigations, TOH was diagnosed without signs of complications. After delivery by caesarean section at 36 weeks of gestation, the patient also developed contralateral groin pain. Imaging showed bilateral TOH complicated by a left NOF fracture. The fracture was treated by reduction and fixation with pins. One year after the intervention, the patient developed recurrent hip pain with a limp, limitation in ROM and leg length discrepancy. Coxarthrosis was confirmed on radiographs and the patient underwent THA with good outcome. Aynaci et al1 reported the case of a 23-year-old patient, primipara and breast feeding, 6 days post partum, who presented sudden pain in both hips with impossibility to walk. She was promptly hospitalised. Radiographs demonstrated marked osteoporosis with bilateral acetabular and NOF fractures. Because of the acetabular component, the patient was initially treated with skeletal traction. Densitometry was undertaken at diagnosis, and after 1 month of traction the osteoporosis showed marked improvement. The patient was then able to benefit from sequential bilateral THA with excellent results.
These cases reflect the complex circumstances of TOH, various manifestations and possible consequences of TOH. Some authors15 do not consider THA as the first line of treatment in young patients, even with displaced femoral neck fracture, and prefer anatomical reduction and fixation. However, in our case, the late diagnosis led to osteonecrosis (figure 3) and therefore THA was the best therapeutic option.
TOH is rare and pathological fractures are described in several cases in the literature1 6 and represent a devastating complication for young patients due to the high lifetime risk of further complications after THA. The diagnosis of TOH remains a challenge in the context of pregnancy, with frequent musculoskeletal and perineal complaints, most of which are not serious and non-specific.7 Clinicians must be aware of the condition with a high index of suspicion to make the diagnosis as early as possible to prevent pathological fractures.
Patient’s perspective.
I am 25 years old. I am a mother of a fourteen months old daughter and I had a difficult pregnancy. It all began in December 2018, when I started to feel pain in my left bottom and hip. After reporting this to my gynaecologist, she referred me to my general practitioner. During the next three months, I had also consulted a neurologist, an anaesthesiologist (pain clinic), and the emergency room. All of them tried to locate the origins of my symptoms. For the treatment of my pain, I took mild opioid medication. I also visited osteopaths, physiotherapists, and received acupuncture. Overall, nobody really knew from what I was suffering and the pregnancy limited radiographic assessments. The neurologist suspected neuritis and decided to do an MRI of the lumbar spine that showed a discretely herniated disk. Rest and pain killers were then prescribed. At the beginning, I had only a painful limp and I had to use elbow crutches in order to move. As it progressed, load bearing on the left leg became close to impossible and I started to see some serious impact on my daily activities. In March 2019, the gynaecologists in the hospital decided to induce labor because of low amniotic fluid. After the delivery, the pain began to worsen. Another MRI of the spine was undertaken and indicated that the disk herniation was larger. The doctors suggested treatment with anti-inflammatory drugs for five days. On day six in the maternity ward without any improvements, a physiotherapeutic evaluation was ordered and, following the examination, an orthopaedic opinion was asked. By the end of March, I had a pelvic radiograph, CT- and MRI-scan. The result was clear: I had a spontaneous and atraumatic displaced femoral neck fracture with signs of osteonecrosis. I was mentally relieved because now I knew that there was a solution to my pain. I benefited from a total left hip arthroplasty. The intervention as well as the post-operative care and rehabilitation went well. My life after the surgery changed not only because of the hip replacement but also because I became a mother. I had to organize and balance childcare, medical appointments, and physiotherapy. Six weeks after the surgery, my orthopaedic surgeon gave me the authorization to walk without support but, in the meantime, I started to feel pain in the left knee. After radiographs showed diffuse osteopenia, it was decided to continue with elbow crutches, physiotherapy sessions and close follow-up. Eventually, I was pain-free at the hip and knee in July 2019 and I started to live a normal life again. Nevertheless, I still have some issues knowing that I am living with a hip replacement and the scar is a constant reminder. Sometimes, when it is raining or windy, I feel a muscular discomfort around the prosthesis and, occasionally, I hear a squeak but I have adapted myself to the whole situation. Today, I consider myself a survivor and I am glad to be able to share my story with the scientific and medical community. With this report, I wish to make caregivers aware of transient osteoporosis of the hip and to help others to avoid a similar problem.
Learning points.
Uncomplicated transient osteoporosis of the hip (TOH) is a self-limiting disease of unclear origin which resolves spontaneously with partial and non-weightbearing.
Other joints such as the knee, lumbar vertebrae, ankle and foot can even be simultaneously affected.
Pregnancy-related TOH is often diagnosed late and possible complications can have long-term consequences for young patients.
Awareness and a high index of suspicion are important to thoroughly investigate perineal, lumbosacral and pelvic ring-related complaints in pregnancy.
MRI including the lumbar spine, pelvic ring, both hips and the neck of femur is the mandatory investigation of choice to diagnose TOH and to prevent complications.
Footnotes
Contributors: KA-D wrote the manuscript and collected most references. JC provided various references and reviewed the manuscript. SB acted as the second consultant on the case and reviewed the manuscript. ENL was the patient’s orthopaedic surgeon, gave the specifics about the case and helped with the writing.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Aynaci O, Kerimoglu S, Ozturk C, et al. Bilateral non-traumatic acetabular and femoral neck fractures due to pregnancy-associated osteoporosis. Arch Orthop Trauma Surg 2008;128:313–6. 10.1007/s00402-007-0439-z [DOI] [PubMed] [Google Scholar]
- 2.Hadji P, Boekhoff J, Hahn M, et al. Pregnancy-associated transient osteoporosis of the hip: results of a case-control study. Arch Osteoporos 2017;12:11. 10.1007/s11657-017-0310-y [DOI] [PubMed] [Google Scholar]
- 3.Asadipooya K, Graves L, Greene LW. Transient osteoporosis of the hip: review of the literature. Osteoporos Int 2017;28:1805–16. 10.1007/s00198-017-3952-0 [DOI] [PubMed] [Google Scholar]
- 4.Pallis D, Georgiou DF, Rizou S, et al. Bilateral transient osteoporosis of the hip. A case report and review of the literature. Clin Cases Mineral Bone Metabolism 2018;15:128–31. 10.11138/ccmbm/2017.15.1.128 [DOI] [Google Scholar]
- 5.Chalouhi GE, Harb C, Atallah D, et al. Total hip replacement at thirty years. Case report of crippling complications of a transient osteoporosis of the hip during pregnancy. Eur J Obstet Gynecol Reprod Biol 2010;149:226–7. 10.1016/j.ejogrb.2009.11.013 [DOI] [PubMed] [Google Scholar]
- 6.Patel V, Temkin S, O’Loughlin M. Transient osteoporosis of pregnancy in a 34-year-old female. Radiol Case Rep 2015;7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Willis-Owen CA, Daurka JS, Chen A, et al. Bilateral femoral neck fractures due to transient osteoporosis of pregnancy: a case report. Cases J 2008;1:120. 10.1186/1757-1626-1-120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reddy KB, Sareen A, Kanojia RK. Transient osteoporosis of the hip in a non-pregnant woman. Case Reports 2015;2015:bcr2015209287. 10.1136/bcr-2015-209287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ergin T, Selam B, Lembet A, et al. Transient osteoporosis of pregnancy: case report. J Turk Ger Gynecol Assoc 2010;11:163–4. 10.5152/jtgga.2010.27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hong CS, Bergen MA, Watters TS. Transient osteoporosis of the hip after bariatric surgery. Arthroplast Today 2019;5:32–7. 10.1016/j.artd.2018.10.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klontzas ME, Vassalou EE, Zibis AH, et al. MR imaging of transient osteoporosis of the hip: an update on 155 hip joints. Eur J Radiol 2015;84:431–6. 10.1016/j.ejrad.2014.11.022 [DOI] [PubMed] [Google Scholar]
- 12.Schapira D, Braun Moscovici Y, Gutierrez G, et al. Severe transient osteoporosis of the hip during pregnancy. Successful treatment with intravenous biphosphonates. Clin Exp Rheumatol 2003;21:107–10. [PubMed] [Google Scholar]
- 13.Petek D, Hannouche D, Suva D. Osteonecrosis of the femoral head: pathophysiology and current concepts of treatment. EFORT Open Rev 2019;4:85–97. 10.1302/2058-5241.4.180036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iannò B, De Gori M, Familiari F, et al. Transient osteoporosis of the hip with a contralateral delayed involvement: a case report. Clin Cases Miner Bone Metab 2017;14:83–6. 10.11138/ccmbm/2017.14.1.083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pauyo T, Drager J, Albers A, et al. Management of femoral neck fractures in the young patient: a critical analysis review. World J Orthop 2014;5:204–17. 10.5312/wjo.v5.i3.204 [DOI] [PMC free article] [PubMed] [Google Scholar]