Abstract
We describe a 40-year-old woman with severe, persistent macroglossia following prone positioning as part of treatment for COVID-19. We used the treatment method of lingual compression with satisfactory results.
Keywords: ear, nose and throat/otolaryngology; adult intensive care; mechanical ventilation
Background
Acute macroglossia is an uncommon and perplexing clinical problem. Previously cited aetiologies include trauma, medication side effects, allergic reactions, patient positioning, pressure packing of the oropharynx and oral surgery.1–8 It has been well described in the literature and is often self-resolving with conservative treatment including intravenous steroids and a bite block.2 4–9 Extreme cases may lead to dysphagia and airway compromise. In certain cases, physicians have resorted to partial glossectomy, a potentially morbid management strategy, associated with postoperative speech and swallowing difficulties.10 11 Non-operative management strategies may be a desirable alternative given the potential for postoperative morbidity.
Case presentation
The patient is a 40-year-old African American woman with a medical history of insulin dependent diabetes mellitus, pancreatic insufficiency, asthma, hypertension and ulcerative colitis. She presented to the emergency department with 1 week of fevers, shortness of breath and diarrhoea. The patient was found to be positive for COVID-19. Her respiratory function quickly worsened despite breathing treatments. She was intubated and admitted to the intensive care unit.
The patient was treated with a combination of hydroxychloroquine, methylprednisolone and tocilizumab. Despite medical management, she developed persistent, severe hypoxia and an acute respiratory distress syndrome-like picture with a partial pressure of oxygen to fraction of inspired oxygen (PaO2:FiO2) ratio <100. In order to improve oxygenation, prone positioning was used for a total of 11 days. Our institutional prone positioning protocol includes 16 hours of prone positioning, followed by 8 hours of supine positioning. Worsening lower facial oedema and macroglossia was noted as a result of patient positioning; however, the benefits of improved oxygenation were thought to outweigh any risks. At the conclusion of prone positioning, the patient’s macroglossia was severe, with the tongue nearly capable of resting on her chest. Thyroid stimulating hormone (TSH) was sent and noted to demonstrate a relatively hyperthyroid state at 0.10 uIU/mL. A free T4 was then checked reflexively and was normal at 1.22 ng/dL. Growth hormone was not checked. We attributed the patient’s macroglossia solely to prolonged prone positioning.
Otolaryngology was consulted. An additional 10-day course of methylprednisolone in addition to a bite block was recommended. However, this yielded only mild improvement. The patient’s tongue remained significantly edematous, protruding from the mouth with pressure injuries developing over the ventral surface where the tongue was in contact with teeth and the endotracheal tube. Tracheostomy was performed on hospital day 26 after approval to perform the procedure in the setting of active COVID-19 infection was obtained from intensive care unit leadership.
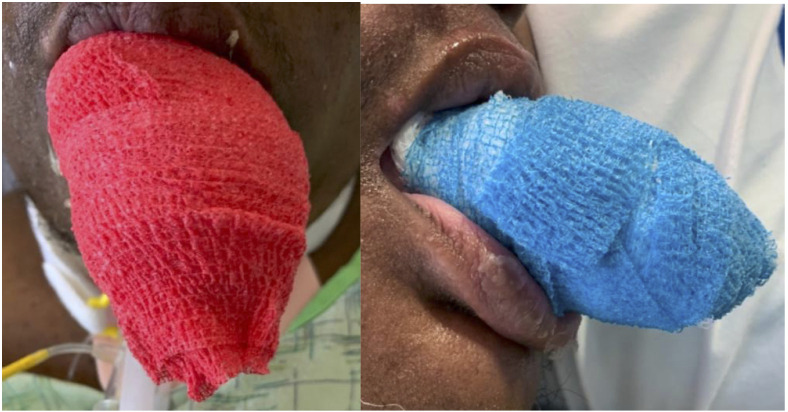
The patient’s macroglossia persisted despite our interventions. In an effort to avoid partial glossectomy, lingual compression was applied on hospital day 27. The wrap consisted of saline moistened gauze loosely wrapped around the tongue, followed by a compressive Coban wrap (3M, St. Paul, Minnesota, USA) applied distal to proximal (figure 1). Care was taken to not create a lingual tourniquet. Initially, the wrap was applied once daily and left in place for 12 hours at a time. Marked improvement was observed after the first wrapping and we continued to note improvement after subsequent treatments. However, lingual oedema was noted to worsen during the 12 hours periods following treatment. On treatment day 8, lingual compression was applied twice daily for a period of 8 hours, followed by 4 hours without lingual compression.
Figure 1.
Anterior and lateral view of lingual compressive wrap.
Outcome and follow-up
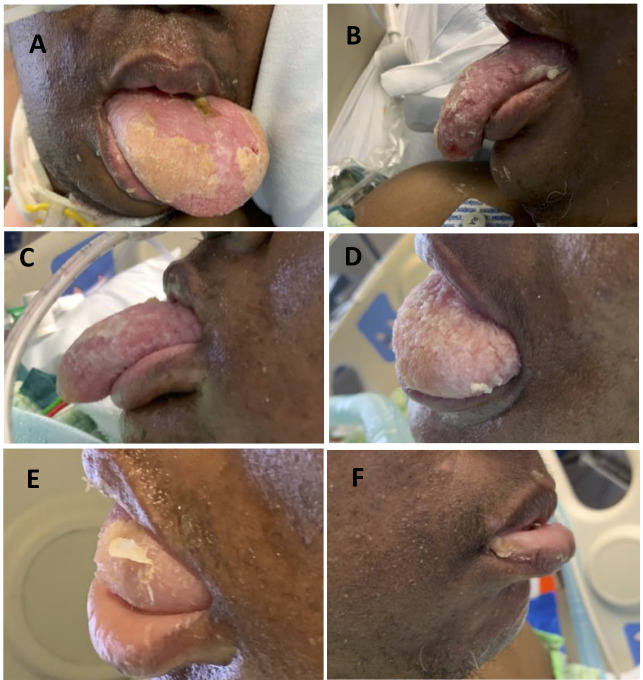
On treatment day 11, the patient was able to retract the tongue into her mouth without difficulty and lingual compression was discontinued (figure 2). There was no evidence of persistent injury to the tongue as a result of treatment. The patient was discharged to a long-term assisted care facility on hospital day 52.
Figure 2.
Progressive resolution of macroglossia with lingual compression. (A) Treatment day 1 prior to initiation of lingual compressive therapy; (B) treatment day 3; (C) treatment day 4; (D) treatment day 10; (E) treatment day 13 and (F) treatment day 14.
Discussion
Acute-onset macroglossia can present significant challenges and distress to the patient when unresponsive to traditional conservative measures. The most commonly cited treatment methods include intravenous steroids and bite blocks. A tracheostomy may be necessary to minimise external compression and preserve airway patency. It has been noted that endotracheal tubes and throat packing can result in lingual oedema due to disruption of venous drainage.2 4 5
Several previously published case reports discuss a variety of techniques for non-operative management of refractory macroglossia. Saah et al6 describe a technique in which they manually reduced the tongue into the oral cavity combined with a gauze head wrap to approximate the jaw and contain the tongue. In that report, the authors describe resolution of oedema within 48 hours after treatment. They hypothesise that reduction of the tongue alone relieves lymphovascular obstruction resulting in resolution of macroglossia. Shanti et al12 describe a slightly different technique involving manual lingual reduction followed by maxillary mandibular fixation. In this instance, fixation was maintained for 3 weeks with resolution of macroglossia at the conclusion of treatment.
In some cases, the extent of lingual oedema will not permit manual reduction. Foreman et al9 used bite blocks placed under anaesthesia. The persistent oedema in this case was believed to be secondary to extrinsic compression of the tongue by the teeth. The patient tolerated the bite blocks well and had resolution of the swelling within a few days. Additionally, Johnson et al13 used a wrapping compression technique for a patient with persistent angioedema from C1 esterase inhibitor deficiency. The author noted improvement following 4 days of compression for 12 hours each day.
Our patient’s macroglossia was the result of a prolonged course of prone positioning for treatment of COVID-19. This mechanism has previously been described in the literature following lengthy surgical cases.2 4 5 7 Her condition persisted despite first-line treatment steroids and bite blocks. Her macroglossia was too severe for manual reduction into the oral cavity. Application of a lingual compression was effective in resolving macroglossia while avoiding the need for partial glossectomy. We found that increasing time of compression from 12 hours daily, as described by Johnson et al,13 to a total compression time of 16 hours daily did not adversely affect the patient and may have shortened overall treatment duration.
Learning points.
Acute macroglossia is a rare clinical problem that can be distressing to both patients and providers.
Acute macroglossia is typically managed conservatively with steroids and bite blocks. If macroglossia is refractory or if partial glossectomy is being considered, lingual compression may be safely used with satisfactory results.
A scheduled protocol with 8 hours of compression followed by 4 hours without compression is safe and effective.
Acknowledgments
The authors would like to thank Stephanie Stebens for assistance in the preparation of this manuscript.
Footnotes
Contributors: EA wrote the manuscript with the assistance of AMA. JL assisted with editing and preparation of the final manuscript. AMA is the senior author.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Bozkurt S, Arslan ED, Köse A, et al. Lingual angioedema after alteplase treatment in a patient with acute ischemic stroke. World J Emerg Med 2015;6:74–6. 10.5847/wjem.j.1920-8642.2015.01.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.DePasse JM, Palumbo MA, Haque M, et al. Complications associated with prone positioning in elective spinal surgery. World J Orthop 2015;6:351–9. 10.5312/wjo.v6.i3.351 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gadban H, Gilbey P, Talmon Y, et al. Acute edema of the tongue: a life-threatening condition. Ann Otol Rhinol Laryngol 2003;112:651–3. 10.1177/000348940311200714 [DOI] [PubMed] [Google Scholar]
- 4.Kawaguchi M, Sakamoto T, Ohnishi H, et al. Pharyngeal packs can cause massive swelling of the tongue after neurosurgical procedures. Anesthesiology 1995;83:434–5. 10.1097/00000542-199508000-00037 [DOI] [PubMed] [Google Scholar]
- 5.Miura Y, Mimatsu K, Iwata H. Massive tongue swelling as a complication after spinal surgery. J Spinal Disord 1996;9:339–41. 10.1097/00002517-199608000-00012 [DOI] [PubMed] [Google Scholar]
- 6.Saah D, Braverman I, Elidan J, et al. Traumatic macroglossia. Ann Otol Rhinol Laryngol 1993;102:729–30. 10.1177/000348949310200915 [DOI] [PubMed] [Google Scholar]
- 7.Sinha A, Agarwal A, Gaur A, et al. Oropharyngeal swelling and macroglossia after cervical spine surgery in the prone position. J Neurosurg Anesthesiol 2001;13:237–9. 10.1097/00008506-200107000-00010 [DOI] [PubMed] [Google Scholar]
- 8.Norman JL, Holmes WL, Bell WA, et al. Life-Threatening ACE inhibitor-induced angioedema after eleven years on lisinopril. J Pharm Pract 2013;26:382–8. 10.1177/0897190012465990 [DOI] [PubMed] [Google Scholar]
- 9.Foreman A, He T, Chan Y, et al. Persistent, severe post-thrombolysis angioedema: simple management of a difficult problem. Am J Otolaryngol 2015;36:721–4. 10.1016/j.amjoto.2015.05.004 [DOI] [PubMed] [Google Scholar]
- 10.Alonso-Rodriguez E, Gómez E, Martín M, et al. Beckwith-Wiedemann syndrome: open bite evolution after tongue reduction. Med Oral Patol Oral Cir Bucal 2018;23:e225–9. 10.4317/medoral.21319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Magee RB. Macroglossia. A method of plastic repair. Am J Surg 1962;103:632–5. 10.1016/0002-9610(62)90535-4 [DOI] [PubMed] [Google Scholar]
- 12.Shanti RM, Braidy HF, Ziccardi VB. Application of Maxillomandibular fixation for management of traumatic macroglossia: a case report. Craniomaxillofac Trauma Reconstr 2015;8:352–5. 10.1055/s-0035-1546815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnson SM, Brown CS, Puscas L. Persistent acute onset macroglossia treated with compression therapy. Case Rep Otolaryngol 2017;2017:1–3. 10.1155/2017/6402413 [DOI] [PMC free article] [PubMed] [Google Scholar]