Description
A 52-year-old man with a recent diagnosis of COVID-19 3 weeks ago presented to the hospital with multiple episodes of haemoptysis, intermittent cough and shortness of breath. There was no history of haematemesis, epistaxis, fever, chills, night sweats or weight loss. He had been discharged 1 week prior for right-sided segmental and subsegmental pulmonary emboli and right leg deep venous thrombosis, which was treated with apixaban. The initial CT scan of the chest also showed bilateral multifocal patchy airspace disease consistent with COVID-19 pneumonia (figure 1).
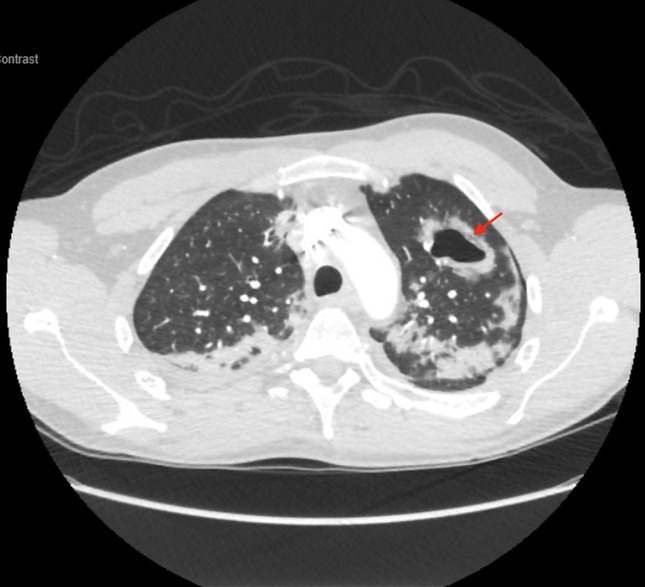
Figure 1.

CT scan of the chest with contrast showing bilateral multifocal patchy airspace disease.
Physical examination on admission revealed a few coarse crackles bilaterally. Repeated CT scan of the chest revealed opacity in the left upper lobe with cavitation (figure 2) and small left-sided pneumothorax, which were new from prior imaging. He maintained adequate oxygen saturation on room air and was discharged home on apixaban. He presented to the hospital 2 weeks later with recurrent haemoptysis and shortness of breath. CT scan of the chest revealed multiple new cavitary lesions bilaterally with the largest lesion in the left lower lobe (figure 3). Infectious diseases, rheumatology and pulmonology consultants recommended an extensive workup including mycobacterial, autoimmune, HIV and fungal tests that were negative. Laboratory workup was significant for mild eosinophilia and Antinuclear Antibody titres of 1:160. Peak C-Reactive Protein level was 259 mg/L, and peak oxygen requirement was noted to be 4 L/min. Reverse transcription-PCR assays for Severe Acute Respiratory Syndrome- Coronavirus-2 (SARS-CoV-2) were persistently positive. Bronchoscopy was performed, and bronchoalveolar lavage samples had no growth. He completed a 14-day course of amoxicillin–clavulanate. His symptoms and oxygen requirements gradually improved, and he was discharged home on apixaban with no further haemoptysis episodes.
Figure 2.
CT scan of the chest with contrast with opacity in the left upper lobe with cavitation.
Figure 3.

CT scan of the chest showing new 7×5 cm cavitary lesion in the left lower lobe along with previously noted left upper lobe cavitary lesion.
Cavitary lung lesions are usually related to mycobacterial, parasitic, fungal, autoimmune or neoplastic aetiologies. Typical CT imaging features of COVID-19 mainly include ground-glass and consolidative pulmonary opacities, primarily in the lower lobes. Notably, there is also the absence of cavitation, lymphadenopathy and pleural effusion.1 2 Lung cavitation following pulmonary embolism and infarction has been described previously in non-COVID-19 patients.3 4 In our case, cavitation predominantly occurred in the left lung, whereas pulmonary emboli were primarily noticed in the right lung. The velocity of the development of multiple cavitary lesions in a few weeks was felt to be atypical for Mycobacterium tuberculosis or fungal infections such as aspergillosis and most likely related to complications from COVID-19 pneumonia.
Lung cavitation due to COVID-19 pneumonia is uncommon.5 Although the exact mechanism of cavitation in COVID-19 pneumonia is unknown, it may be related to diffuse alveolar damage, intra-alveolar haemorrhage and necrosis of parenchymal cells based on prior autopsy reports.6 7 While most cases are self-limited and managed conservatively, as in our case, respiratory status must be monitored closely in patients with massive haemoptysis.
The clinical spectrum of disease secondary to SARS-CoV2 continues to evolve. Early and late complications associated with COVID-19 are still unknown. Common causes of cavitary lung lesions must be investigated appropriately in all patients. Clinicians must be aware of evolving CT findings of COVID-19 and must arrange appropriate follow-up of convalescent patients with COVID-19 to ensure complete recovery.
Learning points.
Cavitary lung lesions are usually related to fungal, mycobacterial, autoimmune, parasitic or neoplastic aetiologies.
While not routinely seen in patients with viral pneumonias, lung cavitation can occur in COVID-19.
Clinicians should be aware about evolving radiological findings of COVID-19 pneumonia.
Footnotes
Twitter: @Vj235
Contributors: VS was involved in writing the manuscript. KD-A was involved in obtaining informed consent and also revised the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Chung M, Bernheim A, Mei X, et al. Ct imaging features of 2019 novel coronavirus (2019-nCoV). Radiology 2020;295:202–7. 10.1148/radiol.2020200230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Haseli S, Khalili N, Bakhshayeshkaram M, et al. Lobar distribution of COVID-19 pneumonia based on chest computed tomography findings; a retrospective study. Arch Acad Emerg Med 2020;8:e55. [PMC free article] [PubMed] [Google Scholar]
- 3.Teng E, Bennett L, Morelli T, et al. An unusual presentation of pulmonary embolism leading to infarction, cavitation, abscess formation and bronchopleural fistulation [published correction appears in BMJ Case Rep. BMJ Case Rep 2018;2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koroscil MT, Hauser TR. Acute pulmonary embolism leading to cavitation and large pulmonary abscess: a rare complication of pulmonary infarction. Respir Med Case Rep 2017;20:72–4. 10.1016/j.rmcr.2016.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen Y, Chen W, Zhou J, et al. Large pulmonary cavity in COVID-19 cured patient case report. Ann Palliat Med 2020;9:5–452. 10.21037/apm-20-452 [DOI] [PubMed] [Google Scholar]
- 6.Menter T, Haslbauer JD, Nienhold R, et al. Post-Mortem examination of COVID19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings of lungs and other organs suggesting vascular dysfunction. Histopathology 2020. doi: 10.1111/his.14134. [Epub ahead of print: 04 May 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yao XH, Li TY, He ZC, et al. [A pathological report of three COVID-19 cases by minimal invasive autopsies]. Zhonghua Bing Li Xue Za Zhi 2020;49:411–7. 10.3760/cma.j.cn112151-20200312-00193 [DOI] [PubMed] [Google Scholar]


