Description
A 45-year-old woman presented with atypical chest pain and palpitations. She had earlier tested positive for COVID-19 pneumonia 3 months back (figure 1A,B). Echocardiography showed normal ventricular functions. ECG was normal. In view of the recent SARS-Cov-2 infection, cardiac magnetic resonance (CMR) (1.5 T) was performed to detect any subclinical myocardial injury. It revealed normal ventricular sizes and functions without any regional wall motion abnormality (video 1). Mild pericardial effusion was also noted. Fat-suppressed T2-weighted images showed normal T2 signal intensity ratios in the entire myocardium (figure 1C,D). T1 mapping images revealed focally elevated T1 mapping values in the basal anteroseptal segment of the left ventricular and normal values in rest of the myocardium. T2 mapping values were normal. Late gadolinium enhancement (LGE) images revealed a linear subepicardial LGE in basal anteroseptal segment, suggestive of replacement fibrosis (figure 2). The T1 mapping values in remote myocardium were normal, ruling out diffuse interstitial fibrosis. There was no pericardial LGE. Since the patient did not have any history of myocarditis/cardiac disease, the current findings were attributed to COVID-19 related persistent myocardial damage. Troponin and NT-pro-brain natriuretic peptide levels were normal at the time of CMR.
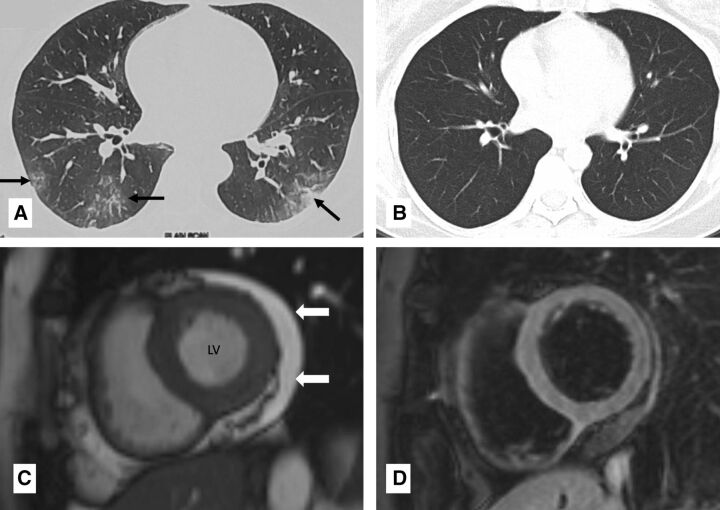
Figure 1.
Chest CT at admission and after recovery (A and B) and cardiac magnetic resonance (CMR) at 3 months post recovery from COVID-19 (C and D): axial CT chest at admission (A) showed ground glass opacities (black arrows) in bilateral lower lobes. Axial CT chest 20 days later (B) showed resolution of the lung opacities. CMR short axis cine (balanced steady state free precession) image (C) done 3 months later shows normal left ventricular (LV) size mild pericardial effusion around the LV (white block arrow). CMR fat-saturated T2-weighted image in short axis (D) showed normal signal intensity of the myocardium.
video 1.
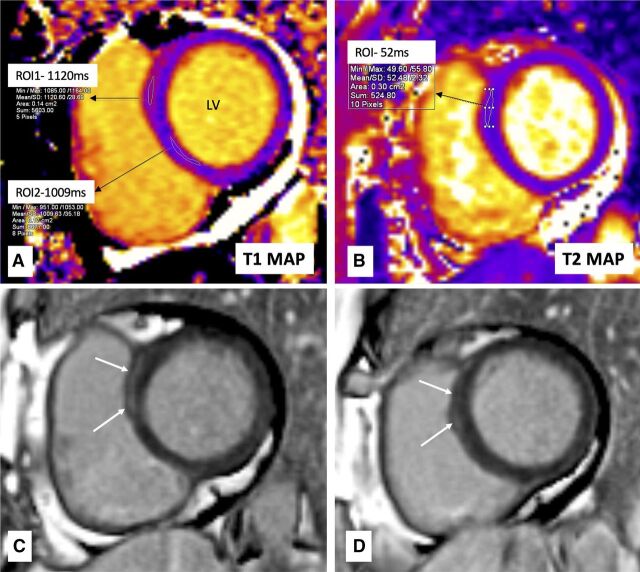
Figure 2.
Cardiac magnetic resonance (CMR) tissue characterisation done 3 months after recovery from COVID-19: CMR motion-corrected native T1 mapping image (A) shows raised T1 mapping value (1120 ms) in the basal anteroseptal segment of the left ventricle (LV) (Region of interest, ROI1) and normal value in inferoseptal segment (1009 ms) (ROI2). CMR motion-corrected T2 mapping image (B) shows normal T2 mapping value (52 ms) in the basal anteroseptal segment of LV (with increased T1 values), suggesting the absence of oedema. CMR late gadolinium enhancement (LGE) image in the same section as mapping images (C) and a segment below (D) shows the presence of linear subepicardial LGE (white arrows) in basal anteroseptal segment of the LV, suggestive of replacement fibrosis.
Myocardial fibrosis without oedema has been described in COVID-19 survivors, but less commonly compared with active myocarditis.1 In the study by Huang et al (n=26) in patients recovered from COVID-19, only 1 patient out of 15 patients with positive CMR findings showed LGE without myocardial oedema. Of note, all the patients had normal troponin levels at the time of CMR.1 In a larger cohort (n=100) of unselected patients recovered from COVID-9, raised mid-ventricular native T1 (diffuse inflammation/fibrosis) was seen in 73 patients, raised T2 (oedema/active inflammation) in 60 and LGE (replacement fibrosis) in 32 patients. Only 5% of the patients had elevated troponin levels during CMR.2 Notably, in both these studies, the ventricular function was seen to be less relevant for disease detection compared with tissue characterisation using LGE and mapping.1 2 Normal ventricular function in our patient also suggests that myocardial tissue abnormalities can precede functional abnormalities. Non-ischaemic patterns of LGE have been shown to be a strong predictor of poor outcome in myocarditis. Hence, appropriate attention should be paid to the possible myocardial involvement in COVID-19 survivors presenting with cardiac symptoms to allow appropriate management.
Learning points.
Myocardial fibrosis without active myocarditis is less common, but can be seen in COVID-19 survivors.
Myocardial tissue abnormalities can precede functional abnormalities of myocardium.
Late gadolinium enhancement is a strong predictor of poor outcome in myocarditis; however, its prognostic implications in COVID-19 are still unknown.
Footnotes
Contributors: PJ prepared the initial draft of the manuscript. VO performed the MRI examination and helped in preparing the initial draft of the manuscript. NN managed the patient and proofread the manuscript. SS proofread the final manuscript and supervised the process.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Huang L, Zhao P, Tang D, et al. Cardiac involvement in recovered COVID-19 patients identified by magnetic resonance imaging. J Am Coll Cardiol Img 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020. 10.1001/jamacardio.2020.3557 [DOI] [PMC free article] [PubMed] [Google Scholar]