Abstract
We describe a patient with COVID-19 who developed simultaneous pulmonary, intracardiac and peripheral arterial thrombosis. A 58-year-old man, without major comorbidity, was admitted with a 14-day history of breathlessness. Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection was confirmed by laboratory testing. Initial imaging revealed COVID-19 pneumonia but no pulmonary thromboembolism (PTE) on CT pulmonary angiography (CTPA). The patient subsequently developed respiratory failure and left foot ischaemia associated with a rising D-dimer. Repeat CTPA and lower limb CT angiography revealed simultaneous bilateral PTE, biventricular cardiac thrombi and bilateral lower limb arterial occlusions. This case highlights a broad range of vascular sequalae associated with COVID-19 and the fact that these can occur despite a combination of prophylactic and treatment dose anticoagulation.
Keywords: venous thromboembolism, pneumonia (infectious disease)
Background
COVID-19 is the clinical syndrome associated with Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection. Although respiratory failure is the most apparent feature of the disease, venous and arterial thrombosis are well-recognised sequalae.1–4 Expert guidance currently recommends higher than standard doses of prophylactic anticoagulation for patients with COVID-19 requiring critical care.1–4 We are not aware of any previously reported cases of COVID-19 associated with simultaneous pulmonary, intracardiac and peripheral arterial thrombosis. We present this case to highlight the extensive COVID-19-associated thrombotic complications that can occur, even despite periods of high-dose prophylactic and therapeutic anticoagulation.
Case presentation
A 58-year-old man presented with a 14-day history of intermittent fever and worsening shortness of breath on exertion. No history of chest pain was reported. The patient’s medical history was limited to well-controlled hypertension, obesity (body mass index of 31 kg/m2 on admission) and a spiral fracture of the right tibia and fibula 15 years previously, with no residual indwelling prosthetic material. There was no history of angina, venous thrombosis peripheral vascular disease. Pre-admission medications included amlodipine 10 mg once daily, indapamide 2.5 mg once daily and candesartan 4 mg once daily. The only family history of note was of maternal deep vein thrombosis provoked by pregnancy. The patient was an office worker but reported good functional status, regularly walking and swimming for recreation. He reported a smoking history of less than a single pack-year of cigarette consumption and approximately 24 units of alcohol per week.
Investigations
Initial clinical examination was unremarkable except for a notable oxygen requirement. A fraction of inspired oxygen (FiO2) of 0.35 was required to maintain a peripheral oxygen saturation above 90%. An initial chest radiograph revealed bilateral intrapulmonary opacities consistent with COVID-19 pneumonia, and SARS-CoV-2 infection was subsequently confirmed by reverse transcription PCR, based on a nasopharyngeal swab. Initial prothrombin time (PT) and activated partial thromboplastin time (APTT) were normal and C-reactive protein (CRP) was high (405 mg/L (0–10 mg/L)). D-dimer was significantly elevated at 508 ng/mL (0–230 ng/mL), prompting initiation of empirical treatment dose low molecular weight heparin (LMWH) pending CT pulmonary angiography (CTPA). This subsequently confirmed bilateral peripheral ground glass opacification (GGO), consistent with COVID-19 pneumonia, and mild coronary artery calcification. No pulmonary thromboembolism (PTE) was present. LMWH dosing was, therefore, reduced to a standard prophylactic regime for venous thromboembolism (VTE) (enoxaparin 40 mg once daily) on day 2.
On day 3, the patient developed an increasing oxygen requirement (FiO2 now 0.4) and was transferred to the high dependency unit (HDU) for consideration of continuous positive airway pressure (CPAP). Admission to HDU prompted an empirical increase in VTE prophylaxis dose (to enoxaparin 40 mg two times per day). This was based on recently published expert opinion advocating higher dose thromboprophylaxis in patients with COVID-19 perceived to be at higher VTE risk, including those transferred to critical care or requiring CPAP.4 Despite this, the patient developed a cold and painful left foot on day 4. On examination, dorsalis pedis and posterior tibial pulses were absent on the left. There was some loss of sensation; however, power appeared unaffected. D-dimer levels were noted to have risen to 992 ng/mL, while APTT and PT remained normal. Fibrinogen and platelet counts were slightly elevated (4.5 g/L (1.70–4.00 g/L) and 441×109/L (150×109–410×109/L), respectively) but troponin I was normal (6 ng/L (0–34 ng/L) and CRP was trending down. A clinical diagnosis of arterial embolism was made, prompting a return to treatment dose anticoagulation. Unfractionated heparin (UFH) was initially prescribed, followed by oral apixaban. Lower limb CT angiography was not performed at this point following discussion with vascular surgery, since the limb was deemed viable and a conservative approach was felt to be optimal.
The patient’s respiratory function stabilised after a short period of awake proning. CPAP did not need to be used. He was stepped down to the respiratory unit on day 6. By day 9, the patient still had a persistent moderate oxygen requirement (FiO2: 0.35–0.4) and presented with a cold, painful left great toe. D-dimer levels were noted to be steadily rising (now 3449 ng/mL), but serial coagulation screens and troponin levels were normal. The platelet count fell to 219×109/L. Repeat CTPA and bilateral lower limb CT angiography were performed and key images are presented in figure 1. The CTPA revealed bilateral segmental and subsegmental occlusive PTE with associated right ventricular strain (right ventricle to left ventricle ratio >1), large filling defects in the right and left ventricles consistent with biventricular thrombi and increasingly dense and confluent peripheral GGO, in keeping with the diagnosis of COVID-19. An echocardiogram was performed, which showed no intracardiac defect nor ventricular dysfunction. The lower limb CT angiography demonstrated a small left posterolateral endoluminal aortic thrombus, complete occlusion of the right tibioperoneal trunk extending into the proximal peroneal and posterior tibial arteries, and occlusion of the tibioperoneal trunk on the left, distal to occlusion of the popliteal artery just below the level of the knee joint. Furthermore, occlusion of the left anterior tibial artery, peroneal artery and multi-level occlusion of the posterior tibial artery was also demonstrated. Additional clot was observed in the left plantar arch.
Figure 1.
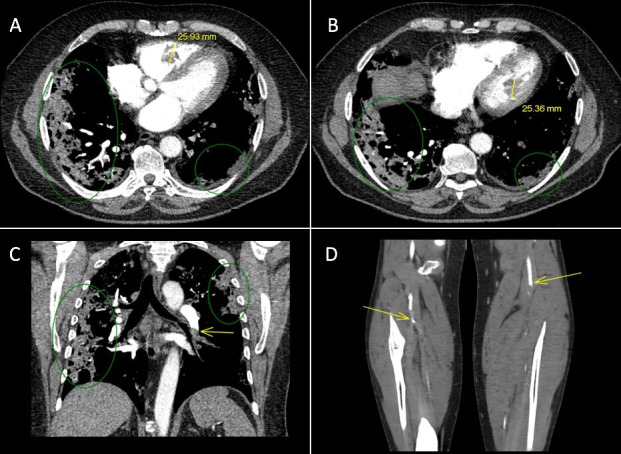
Key images from CT pulmonary angiography (CTPA) and lower limb CT angiography on day 9. Ventricular thrombi imaged on CTPA are highlighted in yellow in panels (A) (axial view of the right ventricle) and (B) (axial view of the left ventricle). Panel (C) highlights a left lower lobe segmental pulmonary thromboembolism visualised on CTPA (yellow arrow, coronal view). Green ovals in panels (A–C) highlight bilateral peripheral ground glass opacification, in keeping with a diagnosis of COVID-19. Panel (D) shows coronal views of right and left lower limb CT angiography. The yellow arrows demonstrate complete occlusion of the right tibioperoneal trunk and left popliteal artery just below the knee joint.
Treatment
The most striking feature of this case is the development of multiple thromboses, despite periods of appropriate prophylactic and therapeutic LMWH. Initially, UFH was initiated to treat his suspected ischaemic limb. However, a falling platelet count raised the possibility of heparin-induced thrombocytopenia (HIT). This could have potentially explained the breakthrough thrombosis demonstrated on the second CTPA, but HIT was quickly ruled out by antibody screen. After consultation with haematologist colleagues, warfarin was selected as definitive, long-term anticoagulation, with an elevated international normalised ratio (INR) target (2.5–3.5).
Outcome and follow-up
The patient was successfully discharged home on day 19. A duplex scan of the left lower leg was performed 2 weeks after discharge. This demonstrated ongoing occlusions of the left distal popliteal artery and tibioperoneal trunk. The posterior tibial artery remained occluded at the level of the ankle. On a positive note, there was recanalisation of the peroneal and anterior tibial arteries. The patient was deemed a good candidate for endovascular treatment but a conservative approach will be taken at present due to the recent acute illness and reduced service capacity during the COVID-19 outbreak. At telephone follow-up, 1 month following discharge, the patient is managing to walk 2 km/day, but still reports some dyspnoea when walking uphill. He has ongoing intermittent pain and paraesthesia of the left foot, but this is improving and will be followed up by the vascular team.
Discussion
COVID-19 infection causes hypoxaemia and a significant inflammatory response. These factors combined with reduced mobility contribute to high thromboembolic risk.5 In addition, SARS-CoV-2 binds to the host’s ACE2 receptor. This is widely expressed on vascular endothelial cells, as well as the respiratory tract, providing a direct route for vascular viral cytopathic effects and promotion of proinflammatory and procoagulant processes that could drive vascular injury, atherosclerosis and occlusion.5 In the case described here, diffuse thromboembolic complications developed despite higher dose VTE prophylaxis and periods of treatment dose anticoagulation prompted by clinical suspicion. This suggests that alternative thromboprophylaxis strategies may need to be considered to address these important complications of COVID-19.
D-dimers are degradation products of fibrin cross-linked by factor XIIIa, and may be elevated due to thrombosis, disseminated intravascular coagulation or secondary processes, including infection, pregnancy, recent trauma, and are frequently raised in the high dependency setting. In the case described here, D-dimer levels rose steadily throughout the admission and appeared to track the evolution of diffuse thromboembolism. In recent case series, elevated D-dimer levels were reported in 43%6 of the patients and were associated with disease severity and increased mortality.5 6 Zhou et al observed that a D-dimer level greater than 1.0 μg/mL on admission (equivalent to 1000 ng/mL) was associated with an OR for mortality of 18.42 (2.64–128.55, p=0.003) compared with patients with levels below 1.0 μg/mL.5
Several case series exist which explore the incidence of venous and arterial thrombosis in patients with COVID-19. In a cohort of 198 hospitalised patients with COVID-19 in the Netherlands, Middeldorp et al describe a 21-day VTE incidence rate of 59% in patients treated in the intensive care unit (ICU) and 9% in patients being treated on the wards, despite VTE prophylaxis.1 No distal arterial nor cardiac thromboses are reported in this series. Another Dutch study, in contrast, reported ischaemic strokes in 3.7% (95% CI 0% to 8.2%) of 184 ICU patients with COVID-19,2 while a small Italian series reported 4 cases of acute limb ischaemia—2 of which occurred in young patients without comorbidity.7 A separate report from Italy also described an increased incidence of acute limb ischaemia (defined as the proportion of all vascular interventions that were performed for acute limb ischaemia) between January 2020 and March 2020 compared with the same period in 2019 (22/141 (16.3%) vs 3/63 (1.8%), p<0.001), and reported a higher rate of revascularisation failure in these cases which were secondary to COVID-19.8 The binding of SARS-CoV-2 to vascular endothelial ACE2 receptors might explain the occurrence of distal arterial thrombosis in patients without preceding vascular disease via viral replication within the endothelium, inflammatory cell infiltration and development of a distinct SARS-CoV-2 viral endotheliitis.9 This process might also generate virus-loaded endothelial microparticles, which could provide a vehicle for further haematogenous viral spread and the propagation of endothelial injury.
Our patient was independently mobile throughout his hospital stay and, therefore, had no physical therapy input. However, physical therapy input should be encouraged in this patient’s group, where the risk of thromboembolism is high and hospital stays are often prolonged.
The high incidence of thrombotic complications in COVID-19 has prompted some groups to recommend high-dose thromobprophylaxis, for example, LMWH two times per day.1–4 This regime is supported by practices in other high-risk settings, such as orthopaedic surgery and by limited observational data using laboratory surrogates.10 The latter includes a study of 10 ICU patients with COVID-19 pneumonia in whom D-dimer levels and viscoelastic measures reduced in response to increased prophylactic dosing.10 However, it remains unproven whether such a strategy will translate into improved patient outcomes and acceptable bleeding risks. The current case highlights the importance of severe prothrombotic states in patients with COVID-19 and the urgent need for randomised clinical trials testing a range of prophylactic strategies. These may include antiviral therapies, immunomodulators and agents capable of stabilising endothelial dysfunction, such as a statins and ACE inhibitors.11–13
Patient’s perspective.
I was unwell at home with flu-like symptoms and was self-medicating with paracetamol. After much cajoling from my family, I visited hospital and was admitted. At that time, I did not feel too unwell and even when transferred to high dependency unit (HDU), I did not realise how ill I was. I was in HDU twice, saw multiple medical teams and received an exemplary level of care. I had multiple visits to the imaging department and had several ultrasound scans while in bed.
I am sure that the treatment that I received saved my life. What was apparent to me was that my condition was changing rapidly and unexpectedly, and the doctors involved with my care seemed to make the correct choices and decisions at each turn.
Learning points.
COVID-19 is associated with high thrombotic risk.
Current prophylactic anticoagulation strategies may not confer sufficient protection.
Clinicians should be wary of false reassurance of prophylactic anticoagulation in this patient group.
There is an urgent need for randomised control trials to test novel prophylactic strategies.
Acknowledgments
Dr Joe Sarvesvaran’s care and compassion were integral to this patient's journey to recovery and we would like to acknowledge his support with writing this case report, and for selecting the key images to include.
Footnotes
Twitter: @DrNatQuail, @kevingblyth
Contributors: NQ and KF contributed equally to writing this paper. KGB contributed to intellectual content of the case report and had overall supervision of the writing. PK provided support in writing the case and looked after the patient in hospital.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Middeldorp S, Coppens M, van Haaps TF, et al. Incidence of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost 2020. doi: 10.1111/jth.14888. [Epub ahead of print: 05 May 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Klok FA, Kruip MJHA, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res 2020;191:145–7. 10.1016/j.thromres.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lodigiani C, Iapichino G, Carenzo L, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res 2020;191:9–14. 10.1016/j.thromres.2020.04.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The British Thoracic Society . Bts guidance on venous thromboembolic disease in patients with COVID-19, 2020. Available: https://brit-thoracic.org.uk/about-us/covid-19-information-for-the-respiratory-community/
- 5.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–62. 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhang J-J, Dong X, Cao Y-Y, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy 2020;75:1730–41. 10.1111/all.14238 [DOI] [PubMed] [Google Scholar]
- 7.Perini P, Nabulsi B, Massoni CB, et al. Acute limb ischaemia in two young, non-atherosclerotic patients with COVID-19. Lancet 2020;395:1546. 10.1016/S0140-6736(20)31051-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bellosta R, Luzzani L, Natalini G, et al. Acute limb ischemia in patients with COVID-19 pneumonia. J Vasc Surg 2020. 10.1016/j.jvs.2020.04.483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Varga Z, Flammer AJ, Steiger P, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020;395:1417–8. 10.1016/S0140-6736(20)30937-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ranucci M, Ballotta A, Di Dedda U, et al. The procoagulant pattern of patients with COVID-19 acute respiratory distress syndrome. J Thromb Haemost 2020;18:1747–51. 10.1111/jth.14854 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Taddei S, Virdis A, Ghiadoni L, et al. Effects of angiotensin converting enzyme inhibition on endothelium-dependent vasodilatation in essential hypertensive patients. J Hypertens 1998;16:447–56. 10.1097/00004872-199816040-00006 [DOI] [PubMed] [Google Scholar]
- 12.Flammer AJ, Sudano I, Hermann F, et al. Angiotensin-Converting enzyme inhibition improves vascular function in rheumatoid arthritis. Circulation 2008;117:2262–9. 10.1161/CIRCULATIONAHA.107.734384 [DOI] [PubMed] [Google Scholar]
- 13.Hürlimann D, Forster A, Noll G, et al. Anti-Tumor necrosis factor-alpha treatment improves endothelial function in patients with rheumatoid arthritis. Circulation 2002;106:2184–7. 10.1161/01.CIR.0000037521.71373.44 [DOI] [PubMed] [Google Scholar]


