Dear Editor,
Phacoemulsification (PhE) with intraocular lens implantation is the gold standard for cataract surgery. The design, material, optical properties of intraocular lenses (IOL) and possible options for their fixation have changed since 1949, when H. Ridley first implanted IOL. “In-the-bag” placement of an IOL provides satisfactory and stable surgical and refractive results. Absence of adequate capsule support is reason to look for possible fixation options.1, 2, 3 Anterior chamber IOLs can cause a number of complications, such as corneal dystrophy, uveitis, cystoid macular edema and glaucoma.4 The most physiological method is posterior chamber IOL implantation, while the IOL is fixed either to the iris or to the sclera.1, 2, 3
The techniques of iris IOL fixation, like any other, have advantages and disadvantages. The advantages include the ability to suture various IOL models through small incisions without damage of intact conjunctiva and sclera. Among the disadvantages of the method the main ones are the inacceptable shape of the pupil, frequent vitreous body and anterior chamber hemorrhages, iridodialysis, irritation of the iris.2,5, 6, 7 Moreover, the main condition for performing all iris fixation techniques is the presence of intact iris stroma, which is often damaged or atrophic due to trauma, uveitis, aniridia, pigment dispersion syndrome and pseudoexfoliative syndrome (PEХ).7, 8, 9 PEX is known to be a risk factor for various intra- and postoperative complications during PhE, including rupture of the zonules of Zinn and posterior capsule, vitreous body prolapse, anterior capsular contraction syndrome, IOL decentration and dislocation.9, 10 One of the main causes of intraoperative complications in PEX is zonular weakness. Frequency of its occurrence in PEX ranges from 8.4% to 10.6%.8,10
Scleral suture IOL fixation is a universal method for correcting aphakia and IOL dislocations, especially in patients with corneal diseases, iris atrophy, anterior chamber angle anomalies, and glaucoma.3,11,12 IOL position during transscleral fixation is almost similar to the natural position of the crystalline lens and has certain advantages. First of all, there is no contact with corneal endothelium and trabecular diaphragm. Moreover, the IOL creates a mechanical barrier between the anterior chamber and the vitreous body. Nevertheless, the erosion and failure of IOL fixing sutures with suture knots exposure continues to be a serious problem for various methods of transscleral IOL suture fixation.13,14 Incidence of externalization of sutures ranges from 6.7% to 73.0%.12,13,15 Thus, the search for a new method of transscleral IOL fixation in the absence of adequate capsule support remains to be up-to-date.
Two techniques that we often used – Hoffman pockets technique and a Z-suture technique – were the prototypes of the method that we propose. Both methods are associated with minimal or no risk of suture erosion and externalization.
The main idea of transscleral Z-suture method is knotless intrascleral fixation of the IOL in the ciliary sulcus. IOL fixation can be carried out in various ways, both ab interno and ab externo.16, 17, 18 Among the advantages of the method the main are the reliable fixation and minimal risk of suture erosion or externalization.16 The technique however has certain drawbacks including the need for conjunctiva dissecting and suturing and the difficulty of performing several intrascleral passes, especially in the hypotonic eye after vitrectomy.16, 17, 19, 20
The main idea of transscleral IOL fixation with Hoffman pockets is the formation of intrascleral pockets 3 mm long. In this case, IOL fixation can be carried out in various ways, both ab interno and ab externo.18 The disadvantages include the complexity of shaping the pockets of the required depth especially on the soft vitrectomized eye, and difficulties in burying the knot into the pocket.17,18 In attempt to prevent myopic shift IOL fixation should be carried out at least 2,5 mm from the limbus. It requires to create scleral pockets as far as 3.0 mm from the limbus.
To eliminate the aforementioned problems, we have developed a method of transscleral IOL fixation using limbal mini-pockets. The method implements both the idea of intrascleral suture pass and the idea of creating a pocket in the limbus. In this technique only one intrascleral pass is used and the size of the limbal pocket is as small as 1.5x1.5 mm.
In this technique two 1.5 x 1.5 mm triangular pockets are created in the middle layers of corneal limbus without dissecting conjunctiva. IOL fixation may be performed either ab interno or ab externo. After IOL fixation intrascleral pass is performed and polypropylene threads are drawn out from the mini-pockets. Surgical knots or flanges are buried in the pockets. This method provides minimal or no risk of suture erosion and externalization.
1. Methods description
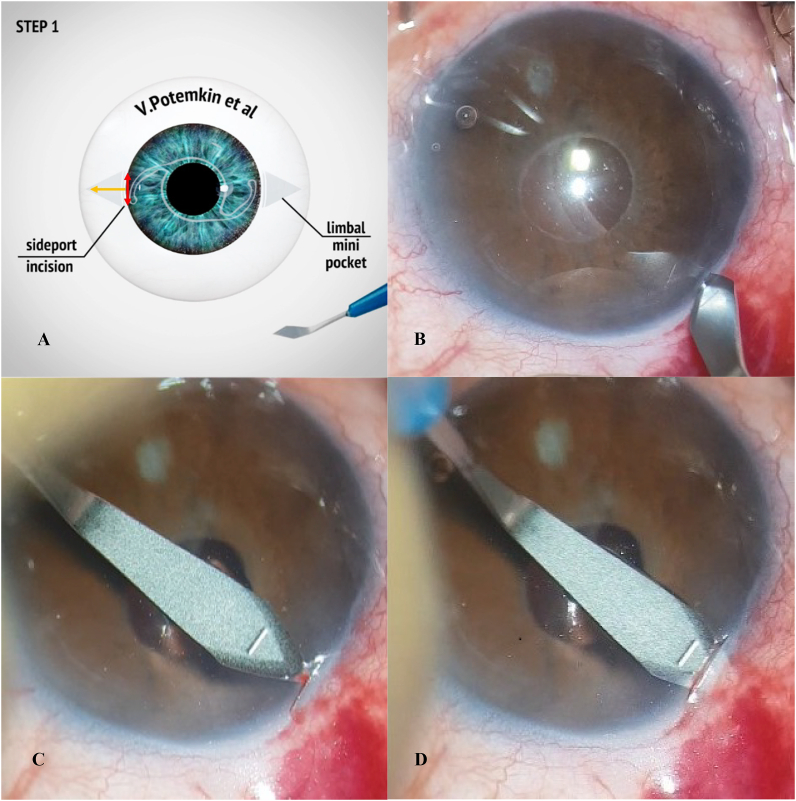
1.1. Step 1
Two half-thickness groove incisions about 1.5 mm in length are made in the peripheral cornea (corneal limbus) at 3 and 9 o'clock or in other opposite meridians depending on the location of IOL haptic elements (Fig. 1A, red arrow, Fig. 1B). Regular main incision keratome is used to create a pocket in the middle layer of limbus (Fig. 1C). The keratome should be pointed from the corneal groove towards the sclera (Fig. 1A, orange arrow). This action is similar to the creation of main incision in cataract surgery, but the blade is directed in opposite direction. The size of 1.5 by 1.5 mm provides enough space to bury the knot later on. (Fig. 1A–D). The same corneal groove is used to make a side port incision with the same knife.
Fig. 1.
Formation of two triangular pockets 1.5 × 1.5 mm in the middle layers of limbus without dissecting conjunctiva
A. schematic view. B. surgical view of groove incision. C/D. surgical view of mini pocket formation.
IOL suturing technique can be carried out ab interno or ab externo, with regular knots or with flanges, depending on surgeon preferences. Here we describe an ab externo technique that seems to the most reliable in our hands.
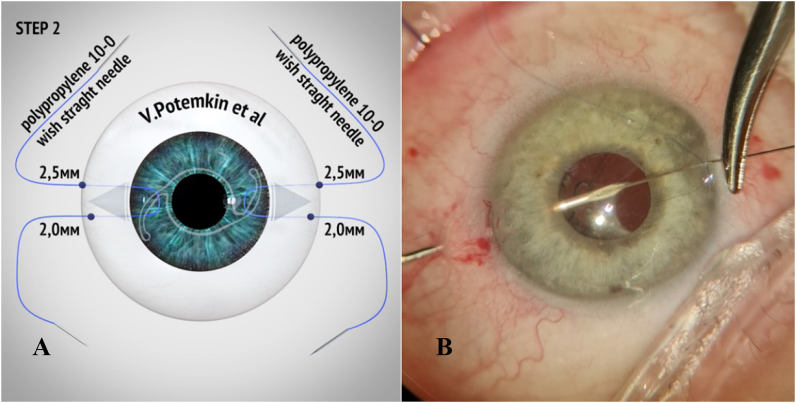
1.2. Step 2
27-G needle is used to perforate both conjunctiva and sclera in the meridian of mini-pocket in 2.5 mm from the limbus on emmetropic eye to prevent myopic shift. The needle is passed under the haptic of dislocated IOL. To “lasso” the haptic double-armed 10/00 or 9/00 polypropylene is used depending on surgeon preferences. One of the needles is inserted through the opposite side-port incision, docked in 27-G needle and externalized. Then 27-G needle is inserted in 2.0 mm from the limbus in 1 mm from the first entry point. These fixation points provide minimal or no IOL tilt after surgery. This needle is passed over the haptic. Second needle with polypropylene is docked in 27-G needle and pulled out. Thus, a loop is created on the IOL haptic (Fig. 2 a and b). The same is repeated on the opposite side.
Fig. 2.
The loop on the haptic is created using ab externo lasso technique
A. schematic view. B. surgical view.
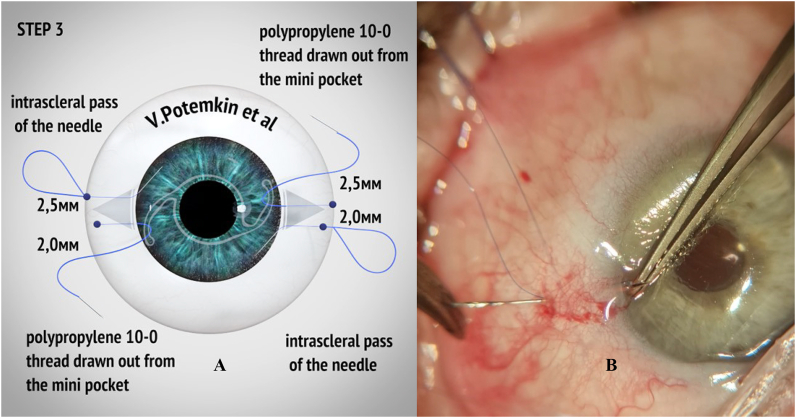
1.3. Step 3
On this step surgeon should pass all four needles to the limbal mini-pockets. To make this procedure easier straight needles are curved in about 2.5 mm from the end (Fig. 3).
Fig. 3.
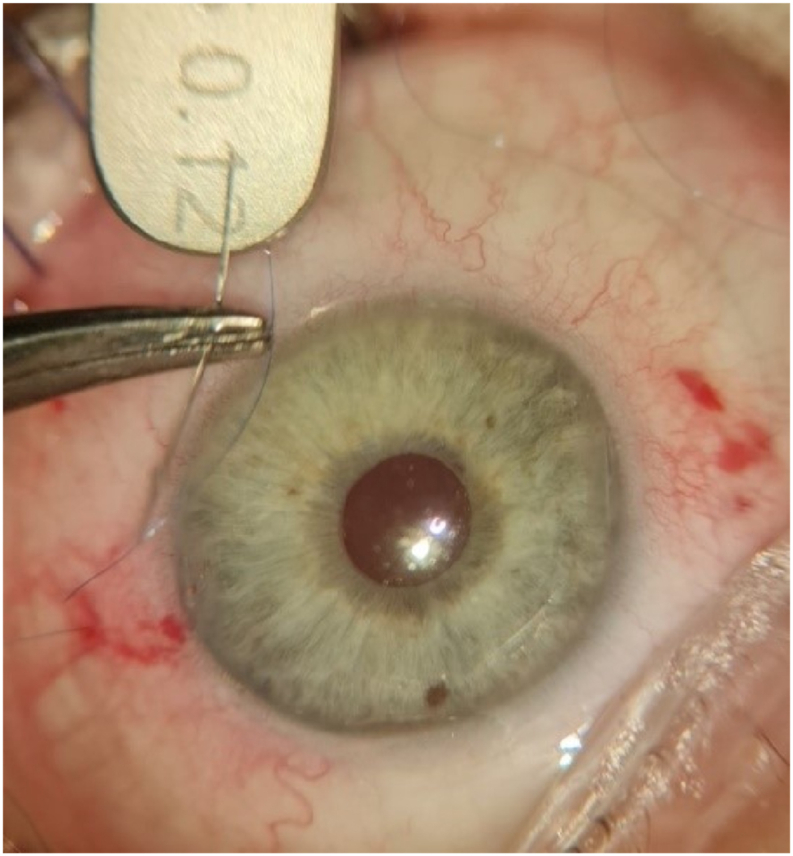
Straight needles are curved in 2.5 mm from the end to ease intrascleral pass to the mini-pocket.
Each needle in then passed through the sclera to the limbal mini-pocket and externalized. Gentle pressure on the cornea or insertion of the second instrument in the pocket helps it to open (Fig. 4 A and B).
Fig. 4.
Intrascleral pass is performed, and polypropylene threads are drawn out from the limbal mini-pockets
A. schematic view. B. surgical view. Gentle pressure on the cornea or insertion of the second instrument helps mini-pocket to open.
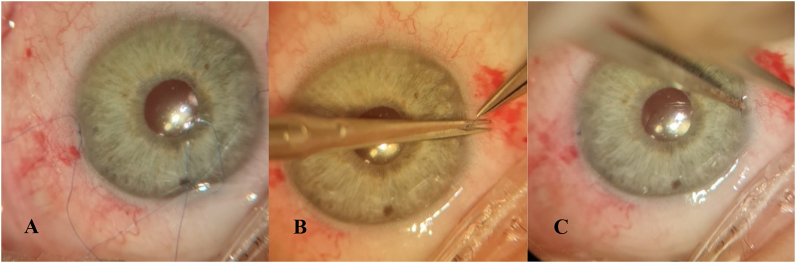
Surgeon can use these intrascleral passes for primary IOL centration before locking the knot or creating the flange. After IOL is well centered the knots are locked, cut shortly and buried in the pockets (Fig. 5A–C).
Fig. 5.
A. Surgical knots are locked. B. cut shortly. C. buried into the pockets.
After performing over 70 transscleral IOL fixations with limbal mini-pockets with at list one year of follow-up we did not have cases with suture knot erosion and externalization. The knot is usually invisible in the limbus (Fig. 6). Anterior segment optical coherence tomography illustrates perfect IOL centration with no tilt (Fig. 7).
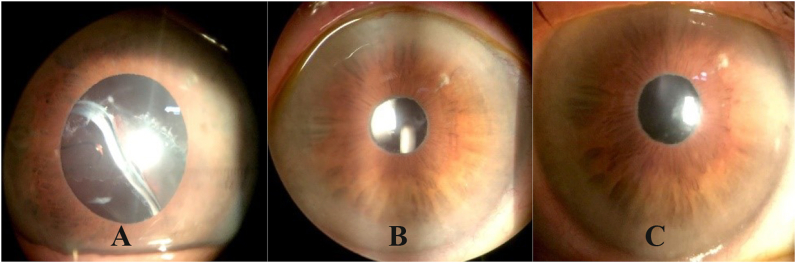
Fig. 6.
Anterior segment before surgery (A), 1 month (B) and 3 months (C) after surgery.
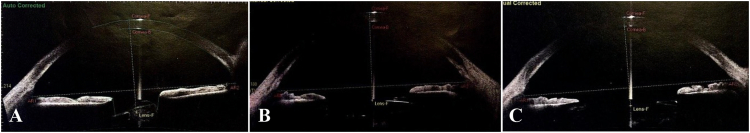
Fig. 7.
Anterior segment OCT (SS-1000, “Casia”, Tomey, Japan) before surgery (A), 1 month (B) and 3 months (C) after surgery.
2. Conclusions
Nowadays the rate of intraoperative complications of cataract surgery is minimal. Dislocation of intraocular lenses due to inadequate capsular bag support continues to be one of the main complications. In this article, a new method for scleral IOL fixation using limbal mini-pockets presented. The method of limbal mini-pockets provides perfect prophylaxis of suture knot or flange erosion. This surgical procedure is not technically challenging. It may be performed both ab externo or ab interno, with regular knots or with flanges. Intrascleral passes help to perform primary IOL centration, and fixation points of 2.5 and 2.0 mm from the limbus prevent myopic shift and IOL tilt.
Study Approval
The authors confirm that any aspect of the work covered in this manuscript that involved human patients was conducted with the ethical approval of all relevant bodies and the study was performed in accordance with the Declaration of Helsinki and the protocol was approved by the Ethics committee of City Ophthalmological Center № 2 of Saint-Petersburg (approval number: 011).
Author Contributions
The authors confirm contribution to the paper as follows:
Conception and design of study: Potemkin V., Astakhov S.; Data collection: Goltsman E., Van S.Yu.; Analysis and interpretation of results: Potemkin V., Goltsman E.; Drafting the manuscript: Potemkin V., Goltsman E.; All authors reviewed the results and approved the final version of the manuscript.
Acknowledgments
Thanks to all the peer reviewers for their opinions and suggestions.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.aopr.2022.100044.
Contributor Information
Vitaly Potemkin, Email: potem@inbox.ru.
Sergey Astakhov, Email: astakhov73@mail.ru.
Elena Goltsman, Email: ageeva_elena@inbox.ru.
Van Syao Yuan, Email: wangxiaoyuan20121017@gmail.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Ridley H. Intra-ocular acrylic lenses—past, present and future. Trans Ophthalmol Soc U K. 1964;84:5–14. [PubMed] [Google Scholar]
- 2.Long C., Wei Y., Yuan Z., et al. Modified technique for transscleral fixation of posterior chamber intraocular lenses. BMC Ophthalmol. 2015;15:127. doi: 10.1186/s12886-015-0118-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kjeka O., Bohnstedt J., Meberg K., et al. Implantation of scleral-fixated posterior chamber intraocular lenses in adults. Acta Ophthalmol. 2008;86(5):537–542. doi: 10.1111/j.1600-0420.2007.01095.x. [DOI] [PubMed] [Google Scholar]
- 4.Hostovsky A., Mandelcorn M., Mandelcorn E.D. Secondary posterior chamber intraocular lens fixation using flanged prolene sutures as an alternative to an anterior chamber intraocular lens implantation. Clin Ophthalmol. 2020;14:3481–3486. doi: 10.2147/OPTH.S276707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Soiberman U., Pan Q., Daoud Y., et al. Iris suture fixation of subluxated intraocular lenses. Am J Ophthalmol. 2015;159:353–359. doi: 10.1016/j.ajo.2014.11.009. [DOI] [PubMed] [Google Scholar]
- 6.Jayamadhury G., Potti S., Kumar K.V., et al. Retropupillary fixation of iris-claw lens in visual rehabilitation of aphakic eyes. Indian J Ophthalmol. 2016;64(10):743–746. doi: 10.4103/0301-4738.195012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Forlini M., Soliman W., Bratu A., et al. Long-term follow-up of retropupillary iris-claw intraocular lens implantation: a retrospective analysis. BMC Ophthalmol. 2015;15:143. doi: 10.1186/s12886-015-0146-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Potemkin V.V., Astakhov S.Yu, Goltsman E.V., et al. Assessment of risk factors for the development of late intraocular lens dislocation. Ophthalmol. Russia. 2021;18(1):103–109. doi: 10.18008/1816-5095-2021-1-103-109. (In Russ.) [DOI] [Google Scholar]
- 9.Hoffman R.S., Fine I.H., Packer M. Scleral fixation without conjunctival dissection. J Cataract Refract Surg. 2006;32(11):1907–1912. doi: 10.1016/j.jcrs.2006.05.029. [PubMed: 17081894] [DOI] [PubMed] [Google Scholar]
- 10.Potemkin V.V., Goltsman E.V. Zonular instability in patients with pseudoexfoliativ syndrome: the analysis of 1000 consecutive phacoemulsifications. Ophthal. J. 2018;11(1):41–46. doi: 10.17816/OV11141-46. [DOI] [Google Scholar]
- 11.Küchle M., Viestenz A., Martus P., et al. Anterior chamber depth and complications during cataract surgery in eyes with pseudoexfoliation syndrome. Am J Ophthalmol. 2000;129:281–285. doi: 10.1016/s0002-9394(99)00365-7. [DOI] [PubMed] [Google Scholar]
- 12.Hayashi K., Hirata A., Hayashi H. In-the-bag scleral suturing of intraocular lens in eyes with severe zonular dehiscence. Eye. 2012;26:88–95. doi: 10.1038/eye.2011.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ting Yu, Yu Mengting, Wu Wenjie, et al. Outcomes and complications of sutured scleral-fixated foldable intraocular lens implantation: a retrospective study of 5-year follow-up. J. Ophthalmol. 2021;2021 doi: 10.1155/2021/5525064. Article ID 5525064, 8 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Castaldelli G B., Firmino G C., Castaldelli V.A., et al. Use of techniques for scleral and Iris fixation in secondary implantation of intraocular lenses. Ophthalmic Res. 2021;64:1–9. doi: 10.1159/000507120. [DOI] [PubMed] [Google Scholar]
- 15.Mahmood S.A., Zafar S., Shakir M., et al. Visual acuity after trans-scleral sutured posterior chamber intraocular lens. J. Coll. Phys. Surg. Pak. 2014;24(12):922–926. [PubMed: 25523729] [PubMed] [Google Scholar]
- 16.Yalniz-Akkaya Z., Burcu A., Uney G.O., et al. Primary and secondary implantation of scleral-fixated posterior chamber intraocular lenses in adult patients. Middle East Afr J Ophthalmol. 2014;21(1):44–49. doi: 10.4103/0974-9233.124093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Por Y.M., Lavin M.J. Techniques of intraocular lens suspension in the absence of capsular/zonular support. Surv Ophthalmol. 2005;50:429–462. doi: 10.1016/j.survophthal.2005.06.010. [DOI] [PubMed] [Google Scholar]
- 18.Potemkin V.V., Goltsman E.V. Methods of surgical correction of intraocular lens dislocation and aphacia (review of literature) Sci. Notes Pavlov. Univ. 2019;26(1):20–28. doi: 10.24884/1607-4181-2019-26-1-20-28. (In Russ.) [DOI] [Google Scholar]
- 19.Szurman P., Petermeier K., Aisenbrey S., et al. Z-suture: a new knotless technique for transscleral suture fixation of intraocular implants. Br J Ophthalmol. 2010;94(2):167–169. doi: 10.1136/bjo.2009.162180. [PubMed: 20139289] [DOI] [PubMed] [Google Scholar]
- 20.Shahid S.M., Flores-Sánchez B.C., Chan E.W., et al. Scleral-fixated intraocular lens implants—evolution of surgical techniques and future developments. Eye. 2021;35:2930–2961. doi: 10.1038/s41433-021-01571-5∖. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.