Abstract
Background:
Language concordance between Latinx patients and their clinicians has been shown to affect health outcomes. In addition, there is evidence that consistent continuity of care (COC) can improve health care outcomes. The relationship between language concordance and COC and their association with health equity in chronic disease is less clear. Our aim was to study the moderating effect of clinician and patient language concordance on the association between COC and asthma care quality in Latinx children.
Methods:
We utilized an electronic health record dataset from a multistate network of community health centers to compare influenza vaccinations and inhaled steroid prescriptions, by ethnicity and language concordance groups overall and stratified by COC.
Results:
We analyzed electronic health records for children with asthma (n = 38,442) age 3 to 17 years with ≥2 office visits between 2005 to 2017. Overall, 64% of children had low COC (defined as COC<0.5) while 21% had high COC (defined as >0.75). All Latinx children had higher rates and odds of receiving influenza vaccination compared with non-Hispanic White children. In addition, Spanish-preferring Latinx children had higher rates and odds of being prescribed inhaled steroids while English-preferring Latinx children had lower odds (OR = 0.85 95%CI = 0.73,0.98) compared with non-Hispanic White children.
Conclusion:
Overall, Latinx children regardless of COC category or language concordance were more likely to receive the influenza vaccine. English-preferring Latinx children with persistent asthma received fewer inhaled steroid prescriptions compared with non-Hispanic White children. Panel chart review and seeing a practice partner might be one way to combat these inequities. (J Am Board Fam Med 2023;36:616–625.)
Keywords: Asthma, Child, Health Equity, Language Concordance, Latinx, Outcome Assessment, Primary Health Care
Introduction
Language concordance in clinical visits (defined as a patient having an appointment their assigned primary care clinician who was highly proficient in the patient’s preferred language, eg, the same language spoken between patients and their clinicians), has been shown to improve patient-clinician communication and access to care1. This is important for children of Spanish-speaking parents who are known to have lower levels of communication with their clinician and lower levels of access to care compared with non-Hispanic White children with English-speaking parents.2 Language barriers also may contribute to poorer asthma management and knowledge among Latinx children.3 Latinx have more asthma exacerbations than non-Hispanic White patients, and Latinx are twice as likely to visit the emergency department for asthma as compared with non-Hispanic Whites.4–6 Asthma is a disease amenable to primary care intervention and management because much asthma care is administered in the primary care setting7, but there is still uncertainty concerning all the care factors that may influence this management.
Continuity of care (COC) is a foundational element of primary care and has demonstrated associations with a range of patient outcomes. Among adults, those with higher continuity have lower health care costs, fewer hospitalizations and emergency department visits, and greater patient satisfaction.6,8–10 Among adolescents, higher continuity was found to be associated with decreased hospitalization and emergency department visits,11 and children with a more consistent health care team in infancy have higher care quality and lower costs in early childhood than children with lower continuity.12 The same study found an association between children with low continuity and risk of developing asthma.5
Still unknown is the relationship of language concordance and COC with health equity in Latinx patients, especially among chronic disease-specific utilization measures in primary care. This knowledge void prevents health systems from optimally deploying and training their workforce to most effectively care for children with asthma or any chronic disease.
To address this specific gap, we seek to better understand the association between patient-clinician language concordance and COC with 2 important asthma care guidelines-receipt of influenza immunization and inhaled corticosteroid prescriptions. We hypothesized that when stratifying by differing levels of continuity, patient and clinician language concordance would be associated with increased odds of influenza vaccination in Latinx children with asthma and language discordance would be associated with lower odds of inhaled steroid prescription in Latinx children with persistent asthma. Understanding such complex multi-level relationships and interactions between predictors of health outcomes in Latinx children with asthma will allow us to better consider strategies and interventions that will improve the health of these children.
Methods
Data Source
We analyzed data from the Accelerating Data Value across a National Community Health Center (ADVANCE) Network, a Patient Centered Research Outcomes Network Clinical Research Network.13 It contains electronic health record (EHR) data from a network of community health centers (CHCs) in the United States; our dataset included data from 475 CHCs in 15 states.
Study Population
Our study population consisted of children 3 to 17 years old with ≥2 face-to-face primary care ambulatory visits to a study clinic from 1/1/2005–12/31/2017. All were either Non-Hispanic White or Latinx children with an asthma diagnosis in the EHR. Asthma diagnoses included an International Classification of Disease (ICD)-9 code of 493* or ICD-10 code of J45* as an encounter or problem list diagnosis during the study period. We conducted a secondary analysis that included only with children with persistent asthma and a minimum of 1 year in the study. Patients with cystic fibrosis were excluded from the study.
Dependent Variables
For the analysis using the full study population of children with asthma, the dependent variables were (1) a binary variable denoting if the child received an influenza vaccine ever in the study period, and (2) yearly rates of influenza vaccine.14,15 For the analysis of children with persistent asthma, our dependent variables were (1) a binary indicator denoting whether or not the child ever had an inhaled steroid prescription ordered within the study period, and (2) the yearly rates of prescribed inhaled steroids, as defined by number of prescriptions/refills on chart.16,17
Independent Variables
For the full study population of children with asthma, the main independent variable was patient and clinician language concordance. Patient-preferred language comes from a discrete language field in the EHR. For clinicians, there is a field in the EHR indicating if the clinician speaks Spanish. Clinicians included were MDs, DOs, NPs, PAs and Naturopaths seeing patients at a primary care visit. Patient-clinician language concordance groups were categorized into 4 mutually exclusive groups: (1) non-Hispanic Whites, (2) English-preferring Latinx, (3) Spanish-preferring Latinx with a non-Spanish-speaking clinician, and (4) Spanish-preferring Latinx with a Spanish-speaking clinician. While we use the term Latinx as it is often preferred by the patients in our sample, the actual variable collected in the EHR is “Hispanic” and “non-Hispanic.”
For the analysis subset to children with persistent asthma, low sample size limited our ability to construct patient-clinician language concordance groups as above. Instead, the main independent variable in the analysis limited to children with persistent asthma was patient language and ethnicity. This was categorized into 3 groups: (1) non-Hispanic Whites, (2) English-preferring Latinx, and (3) Spanish-preferring Latinx.
Continuity of Care Variable
To evaluate the moderating role of continuity of care on the association between patient-clinician language concordance and all study outcomes, we estimated patient and clinician COC using the Bice-Boxerman18. The Bice-Boxerman COC index is scored on a scale from 0 to 1, with higher scores indicating greater continuity.11 To aid in interpretability, we categorized the continuity scores into 0–0.5 (low), 0.5–0.75 (medium) and 0.75–1.0 (high) and used these categories to stratify analyses for both our primary and secondary outcomes.
Covariates
For all analyses, we adjusted for patient-level characteristics such as age in years at first clinic visit (3 to 5, 6 to 10, 11 to 17), sex (female or male), if the child ever had an albuterol prescription ordered in the study period (yes/no), number of visits per year (<2, 2 to 5, 6 to 10, >10), family income as a percent of the federal poverty level (always ≥138%, above and below 138%, always <138%, never documented). In analyses subset to those with persistent asthma, we also included if they ever received the influenza vaccine in the study period (yes/no).
Statistical Analysis
We conducted descriptive analyses of the overall sample and by patient-language concordance groups to examine our sample characteristics. Next, we conducted generalized estimating equations (GEE) logistic and GEE Poisson regression models adjusted for the above stated covariates. We fitted models with a compound symmetry correlation structure and empirical sandwich variance estimator to estimate adjusted odds ratios (ORs), adjusted rate ratios (RRs) and their corresponding 95% confidence intervals, accounting for clustering of individuals within CHCs. To evaluate the potential moderating role of COC, we performed similar GEE models described above on both of our study samples (children with asthma and children with persistent asthma) overall and stratified by the COC categories (low, medium, and high). Two-sided statistical significance was set at P<.05, and analyses were conducted using Rstudio version 4.2.1. This study was approved by the Oregon Health & Science University Institutional Review Board.
Results
Our study population consisted of 38,442 children with asthma (Table 1). Most children were male and either Spanish-preferring Latinx with non-Spanish-speaking clinicians or non-Hispanic Whites between ages 3 and 5 during their first visit. The majority of children had a low Bice-Boxerman COC index. Our secondary analysis, children with persistent asthma, included 5691 children (Appendix). Trends in this sample were similar to our larger group.
Table 1.
Population Characteristics of Children with Any Asthma Diagnosis Overall and by Ethnicity/Language Concordance Groups
| Overall | Non-Hispanic White | English- Preferring Latinx | Spanish-Preferring Latinx with a non-Spanish-speaking Clinician | Spanish-Preferring Latinx with a Spanish-speaking Clinician | |
|---|---|---|---|---|---|
|
| |||||
| N | 38,442 | 12,406 | 11,316 | 13,437 | 1283 |
| Age at first encounter | |||||
| 3 to 5 | 18,799(48.9) | 5264 (42.4) | 5319 (47.0) | 7535 (56.1) | 681 (53.1) |
| 6 to 10 | 13,019(33.9) | 4409 (35.5) | 3920 (34.6) | 4278 (31.8) | 412 (32.1) |
| 11 to 17 | 6624(17.2) | 2733 (22.0) | 2077 (18.4) | 1624 (12.1) | 190 (14.8) |
| Sex | |||||
| Female | 16,720 (43.5) | 5565 (44.9) | 4947 (43.7) | 5673 (42.2) | 535 (41.7) |
| Male | 21,722 (56.5) | 6841 (55.1) | 6369 (56.3) | 7764 (57.8) | 748 (58.3) |
| Number of visits/year | |||||
| <2 | 14,454 (37.6) | 5164 (41.6) | 4458 (39.4) | 4320 (32.2) | 512 (39.9) |
| 2 to 5 | 17,610(45.8) | 5283 (42.6) | 5114 (45.2) | 6626 (49.3) | 587 (45.8) |
| 6 to 10 | 4905 (12.8) | 1452 (11.7) | 1350 (11.9) | 1959 (14.6) | 144 (11.2) |
| >10 | 1473 (3.8) | 507 (4.1) | 394 (3.5) | 532 (4.0) | 40 (3.1) |
| Income as a percent of FPL | |||||
| Always ≥138% | 2666 (6.9) | 1262 (10.2) | 779 (6.9) | 592 (4.4) | 33 (2.6) |
| Above and Below | 4143 (10.8) | 1519 (12.2) | 864 (7.6) | 1506 (11.2) | 254 (19.8) |
| Always <138% | 25,253 (65.7) | 7232 (58.3) | 7490 (66.2) | 9748 (72.5) | 783 (61.0) |
| Never Documented | 6380 (16.6) | 2393 (19.3) | 2183 (19.3) | 1591 (11.8) | 213 (16.6) |
| Asthma ever on Problem List | |||||
| No | 8697 (22.6) | 2933 (23.6) | 2437 (21.5) | 2936 (21.9) | 391 (30.5) |
| Yes | 29,745 (77.4) | 9473 (76.4) | 8879 (78.5) | 10,501 (78.1) | 892 (69.5) |
| Albuterol ever prescribed | |||||
| Yes | 32038 (83.3) | 9965 (80.3) | 9141 (80.8) | 11720 (87.2) | 1212 (94.5) |
| No | 6404 (16.7) | 2441 (19.7) | 2175 (19.2) | 1717 (12.8) | 71 (5.5) |
| Bice Boxerman COC Index | |||||
| Low: 0–0.5 | 24,765 (64.4) | 8269 (66.7) | 6708 (59.3) | 8767 (65.2) | 1020 (79.5) |
| Medium: 0.5–0.75 | 5446 (14.2) | 1623 (13.1) | 1621 (14.3) | 2049 (15.2) | 153 (11.9) |
| High: >=0.75 | 8232 (21.4) | 2514 (20.3) | 2987 (26.4) | 2621 (15.2) | 110 (8.6) |
Abbreviations: COC, continuity of care; FPL, federal poverty level.
Table 2 and Figures 1 and 2 display the adjusted odds ratios and adjusted rate ratios of receiving the influenza vaccination during the study period among the full sample along with their corresponding 95% confidence intervals. Overall, all Latinx children, regardless of patient-clinician language concordance, had higher odds and rates of receiving the influenza vaccine compared with non-Hispanic Whites. Latinx children in each continuity category also had higher odds of receiving the influenza vaccine compared with non-Hispanic White children. All Latinx children in the high continuity category had higher rates of the influenza vaccine compared with non-Hispanic White children and those children in the low and middle continuity groups trended higher.
Table 2.
Adjusted Odds and Rate Ratios of Receipt of Influenza Vaccine and Inhaled Steroid Prescriptions
| Children with Any Asthma (n = 38,442), odds ratios of receiving the influenza vaccine, OR (95% CI) | ||||
|
| ||||
| Overall | COC 0–0.5 | COC 0.5–0.75 | COC 0.75–1 | |
|
| ||||
| Non-Hispanic White | Ref | Ref | Ref | Ref |
| English-preferring Latinxs | 1.43 (1.35,1.50) | 1.51 (1.41,1.62) | 1.53 (1.33,1.76) | 1.30 (1.16,1.45) |
| Spanish-preferring Latinxs with a non-Spanish-speaking clinician | 2.55 (2.42,2.69) | 2.66 (2.49,2.84) | 2.67 (2.31, 3.08) | 2.28 (2.03,2.56) |
| Spanish-preferring Latinxs with a Spanish-speaking clinician | 3.22 (2.82,3.68) | 3.16(2.71,3.68) | 3.96 (2.62,6.00) | 2.21 (1.50,3.26) |
|
| ||||
| Children with Persistent Asthma (n = 5691), odds ratios of prescribed inhaled steroids, OR (95% CI) | ||||
|
| ||||
| Overall | COC 0–0.5 | COC 0.5–0.75 | COC 0.75–1 | |
|
| ||||
| Non-Hispanic White | Ref | Ref | Ref | Ref |
| English-preferring Latinx | 0.85 (0.73,0.98) | 1.06 (0.88,1.27) | 1.24 (0.84,1.83) | 0.48 (0.35,0.66) |
| Spanish-preferring Latinx | 1.33 (1.15,1.53) | 1.30 (1.09,1.54) | 1.82 (1.56,2.62) | 1.07 (0.77,1.49) |
|
| ||||
| Children with Any Asthma (n = 38,442), rate ratios of receiving influenza vaccine, RR (95% CI) | ||||
|
| ||||
| Overall | COC 0–0.5 | COC 0.5–0.75 | COC 0.75–1 | |
|
| ||||
| Non-Hispanic White | Ref | Ref | Ref | Ref |
| English Speaking Latinxs | 1.10 (1.02,1.20) | 1.17(1.06,1.29) | 1.11 (0.90,1.37) | 1.00 (0.83,1.20) |
| Spanish-preferring Latinxs with a non-Spanish-speaking clinician | 1.41 (1.31,1.52) | 1.42 (1.30,1.55) | 1.51 (1.26,1.82) | 1.32 (1.09,1.6) |
| Spanish-preferring Latinxs with a Spanish-speaking clinician | 1.57 (1.37,1.80) | 1.62 (1.39,1.88) | 1.47 (0.95,2.25) | 1.18 (0.67,2.09) |
|
| ||||
| Children with Persistent Asthma (n = 5691), rate ratios of prescribed inhaled steroids, RR (95% CI) | ||||
|
| ||||
| Overall | COC 0–0.5 | COC 0.5–0.75 | COC 0.75–1 | |
|
| ||||
| Non-Hispanic White | Ref | Ref | Ref | Ref |
| English-preferring Latinx | 0.95 (0.85,1.07) | 1.11 (0.96,1.23) | 1.13 (0.82,1.56) | 0.54 (0.41,0.71) |
| Spanish-preferring Latinx | 1.19 (1.07,1.32) | 1.20 (1.06,1.35) | 1.53 (1.14,2.05) | 0.88 (0.69,1.13) |
Abbreviations: COC, consistent continuity of care; OR, odds ratio; RR, risk ratio; CI, confidence interval; GEE, generalized estimating equations.
Note: GEE logistic regression model adjusted for age, sex, number of visits per year, asthma ever on problem list, income as a percent of the federal poverty level, albuterol prescription ever for the influenza vaccine outcome.
Figure 1.
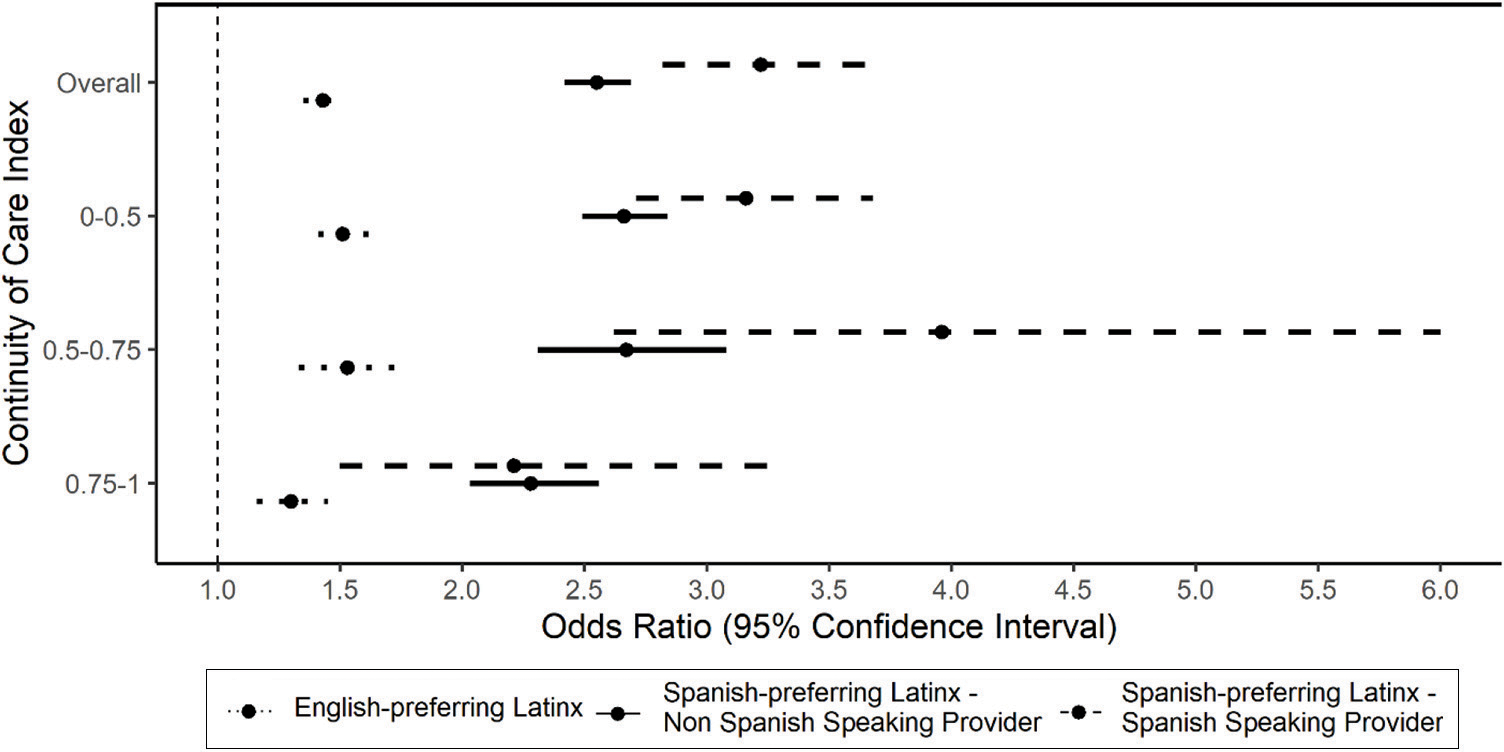
Odds ratios of ever receiving an influenza vaccination for all children with asthma (reference group is non-Hispanic white patients). Abbreviation: GEE, generalized estimating equations.
Note: GEE logistic regression model adjusted for age, sex, number of visits per year, asthma ever on problem list, income as a percent of the federal poverty level, albuterol prescription ever, clustered on patient’s primary clinic. Horizontal lines denote 95% confidence intervals.
Figure 2.

Rate ratios of ever receiving an influenza vaccination for all children with asthma (Reference group is non-Hispanic white patients). Abbreviation: GEE, generalized estimating equations.
Note: GEE logistic regression model adjusted for age, sex, number of visits per year, asthma ever on problem list, income as a percent of the federal poverty level, albuterol prescription ever, clustered on patient’s primary clinic. Horizontal lines denote 95% confidence intervals.
Figures 3 and 4 display the adjusted odds ratios and adjusted rate ratios of being prescribed inhaled steroids among patients with persistent asthma. Overall, Spanish-preferring Latinx children had higher odds and rates of prescription (OR [95%CI]: 1.33 [1.15,1.53], RR [95%CI]: 1.19 [1.07,1.32]) compared with non-Hispanic White children while English-preferring Latinx children had lower odds (OR [95%CI]: 0.85 [0.73,0.98]). In addition, English-preferring Latinx children with persistent asthma in the high COC groups have lower odds and rates of prescription (OR [95%CI]: 0.48 [0.35,0.66], RR [95%CI]: 0.54 [0.41,0.71]) (Table 2).
Figure 3.
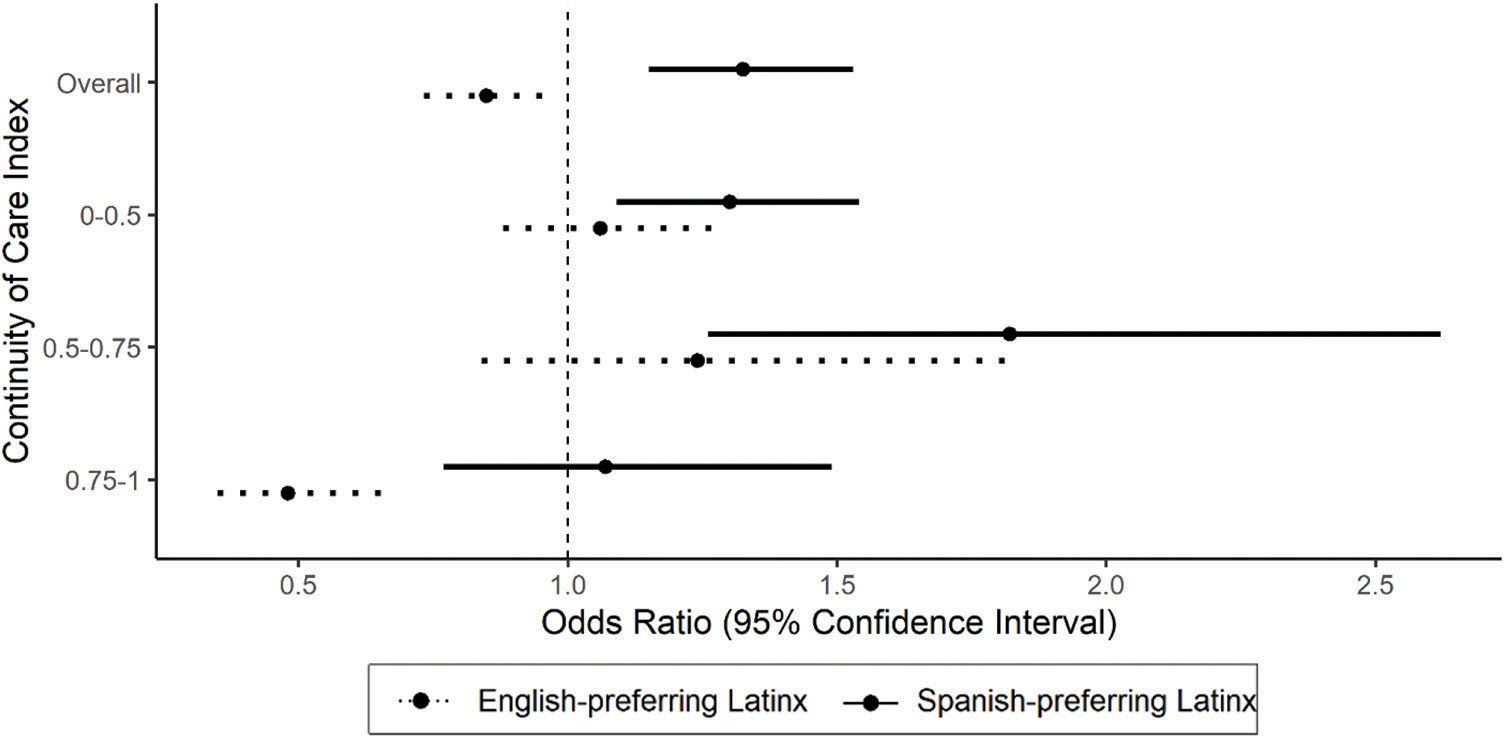
Odds ratios of ever being prescribed inhaled steroids for children with persistent asthma (reference group is non-Hispanic white patients). Abbreviation: GEE, generalized estimating equations.
Note: GEE logistic regression model adjusted for age, sex, number of visits per year, asthma ever on problem list, income as a percent of the federal poverty level, albuterol prescription ever and influenza vaccine, clustered on patient’s primary clinic. Horizontal lines denote 95% confidence intervals.
Figure 4.

Rate ratios of ever being prescribed inhaled steroids for children with persistent asthma (reference group is non-Hispanic white patients). Abbreviation: GEE, generalized estimating equations.
Note: GEE Poisson regression model adjusted for age, sex, number of visits per year, asthma ever on problem list, income as a percent of the federal poverty level, albuterol prescription ever and influenzavaccine, clustered on patient’s primary clinic. Horizontal lines denote 95% confidence intervals.
Discussion
This large, nation-wide study of Latinx children with asthma, conducted in 475 community health centers is the first in our knowledge to examine the association of language concordance and COC on care quality indicators in Latinx children with asthma. We found that Latinx children with asthma have higher odds of receiving the influenza vaccination compared with non-Hispanic White children regardless of clinician-patient language concordance or COC category. In addition, the odds and rates of an inhaled steroid prescription decreased with higher continuity among English-preferring Latinx children with persistent asthma in community health centers. This article adds to the literature about patient-clinician language concordance in the context of preventive and management services for minority populations. Our study population displayed similar trends found in other articles19 with Latinx children with asthma receiving the influenza vaccine more often than non-Hispanic White children.20,21 Latinx patients have been shown to have higher rates of influenza associated hospitalizations than non-Hispanic Whites,22 so this phenomenon (higher utilization of vaccines by Latinx patients) may be a response to a common health threat to the community, a high value for this type of preventive care, or a particular effectiveness of CHCs in delivering this care to this community. Clinicians need to be aware of these possible phenomena so they can encourage all patients, regardless of ethnicity, to receive the influenza vaccine. Considering that at present, services in some communities may not always account for characteristics of the clinician-patient relationship, including language concordance between clinician and patient, this could be a target area to consider when designing community-based care delivery systems that are better able to address health inequities.
Our results from the secondary analysis show that in the low and medium continuity groups, Spanish-preferring Latinx children are more likely to be prescribed inhaled steroids. English-preferring Latinx children with high continuity are less likely to be prescribed inhaled steroids compared with non-Hispanic White children. A cohort study from Quebec found continuity of care was not significantly associated with asthma-related emergency department visits for children, but they did not look specifically at patient language and ethnicity.23 This may mean that when it comes to some quality measures, another “set of eyes” may help (ie, seeing a practice partner or panel chart review by a team or committee) for quality assurance in chronic disease management, and these measures may be an important supplemental quality practice, even in a setting of high continuity. These findings also suggest that English-preferring Latinx children may be even more of a vulnerable group when it comes to appropriate care utilization because they are not receiving equitable and adequate care. Language-concordant education and suitable action plans are valued and desired by Spanish-preferring Latinxs.24 According to our data, Spanish-preferring Latinx children with persistent asthma tend to have higher odds of inhaled steroid prescription than non-Hispanic White children in the low and medium COC groups, meaning that Language-concordance education and actions plans could be working for this group of children. These types of resources may also be valued by English-preferring Latinx children with high continuity and should not be overlooked.
Limitations
Our findings may not be generalizable to all children with asthma because the data come entirely from CHCs, which serve primarily individuals with lower socio-economic status, however, many children in the US do receive asthma care at CHCs, which makes them a relevant setting for this research. Due to sample size issues, we were unable to create the same ethnicity/language concordance groups in our secondary more restricted analysis as our larger sample. In addition, our dataset does not contain prescription fill data, so while we are able to determine whether inhaled steroids were ordered by clinicians, we do not know if they were filled and/or used. Future research using pharmacy data may be able to examine whether medication use or adherence is related to COC. Lastly, we were unable to incorporate parent(s) language in our analysis which may influence study findings and this is an area of future research.
Conclusion
Overall Latinx children with asthma, regardless of individual or clinician language, are more likely to receive the influenza vaccine compared with non-Hispanic White children with asthma. English-preferring Latinx children with high continuity and persistent asthma are less likely to be prescribed inhaled steroids than non-Hispanic White children with high continuity. This indicates that regular panel/chart review may be an important component for ensuring these children have adequate care. English-preferring Latinx children with high continuity might benefit by having an action plan and having a better understanding of their disease. These findings are important to consider when designing a community-based care system to help find solutions for inequities in children with asthma.
Acknowledgments
This work was conducted with the Accelerating Data Value Across a National Community Health Center Network (ADVANCE) Clinical Research Network (CRN). ADVANCE is a CRN in PCORnet®, the National Patient Centered Outcomes Research Network. ADVANCE is led by OCHIN in partnership with Health Choice Network, Fenway Health, and Oregon Health & Science University. ADVANCE’s participation in PCORnet® is funded through the Patient-Centered Outcomes Research Institute (PCORI), contract number RI-OCHIN-01-MC.
Funding:
National Institute on Minority Health and Health Disparities (NIMHD), Grant number: R01MD011404 (JH).
Appendix.
Population Characteristics of Children with Persistent Asthma by Ethnicity and Language.
| Total | Non-Hispanic White | English-Preferring Latinx | Spanish-Preferring Latinx | |
|---|---|---|---|---|
|
| ||||
| N | 5691 | 1626 | 1837 | 2228 |
| Age | ||||
| 3 to 5 | 2967 (52.1) | 760 (46.7) | 930 (50.6) | 1277 (57.3) |
| 6 to 10 | 1847 (32.5) | 526 (32.3) | 621 (33.8) | 700 (31.4) |
| 11 to 17 | 877 (15.4) | 340 (20.9) | 286 (15.6) | 251 (11.3) |
| Sex | ||||
| Female | 2359 (41.5) | 684 (42.1) | 792 (43.1) | 883 (39.6) |
| Male | 3332 (58.5) | 942 (57.9) | 1045 (56.9) | 1345 (60.4) |
| Visits per year | ||||
| <2 | 782 (13.7) | 293 (18.0) | 281 (15.3) | 208 (9.3) |
| 2 to 5 | 2272 (39.9) | 692 (42.6) | 772 (42.0) | 808 (36.3) |
| 5 to 10 | 1743 (30.6) | 442 (27.2) | 529 (28.8) | 772 (34.6) |
| >10 | 894 (15.7) | 199 (12.2) | 255 (13.9) | 440 (19.7) |
| Income as a percent of FPL | ||||
| Sometimes Above 138% | 935 (16.4) | 343 (21.1) | 255 (13.9) | 337 (15.2) |
| Always Below 138% | 3926 (69.0) | 1014 (62.4) | 1287 (70.1) | 1625 (72.9) |
| Never Documented | 830 (14.6) | 269 (16.5) | 295 (16.1) | 266 (11.9) |
| Asthma ever on PL* | ||||
| Yes | 550 (9.7) | 1456 (89.5) | 1662 (90.5) | 2023 (90.8) |
| No | 5141 (90.3) | 170 (10.5) | 175 (9.5) | 205 (9.2) |
| Albuterol Prescription ever | ||||
| Yes | 4428 (77.8) | 1170 (72.0) | 1343 (73.1) | 1915 (86.0) |
| No | 1263 (22.2) | 456 (28.0) | 494 (26.9) | 313 (14.0) |
| Influenza Vaccination ever | ||||
| Yes | 3495 (61.4) | 817 (50.2) | 1071 (58.3) | 1607 (72.1) |
| No | 2196 (38.6) | 809 (49.8) | 766 (41.7) | 621 (27.9) |
| Bice Boxerman COC Index | ||||
| 0–0.5 (Low) | 3531 (62.0) | 1062 (65.3) | 1004 (54.7) | 1465 (65.8) |
| 0.5–0.75 (Medium) | 1300 (22.8) | 355 (21.8) | 560 (30.5) | 385 (17.3) |
| >=0.75 (High) | 860 (15.1) | 209 (12.9) | 273 (14.9) | 378 (17.0) |
Abbreviations: COC, continuity of care; FPL, Federal poverty level.
Footnotes
Conflict of interest: The authors have no conflicting or competing interests to declare.
Contributor Information
Tahlia Hodes, Department of Family Medicine, Oregon Health & Science University.
Miguel Marino, Department of Family Medicine, Oregon Health & Science University.
Jennifer A. Lucas, Department of Family Medicine, Oregon Health & Science University.
Andrew Bazemore, American Board of Family Medicine.
Lars Peterson, American Board of Family Medicine.
Michelle K. Trivedi, Division of Pediatric Pulmonology, Department of Pediatrics, University of Massachusetts Chan Medical School/UMass Memorial Children’s Medical Center).
Sophia Giebultowicz, OCHIN, Inc..
John Heintzman, Department of Family Medicine, Oregon Health & Science University; OCHIN, Inc..
References
- 1.Kanter MH, Abrams KM, Carrasco MR, Spiegel NH, Vogel RS, Coleman KJ. Patient-physician language concordance: a strategy for meeting the needs of Spanish-speaking patients in primary care. Perm J 2009;13:79–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Claudio L, Stingone JA. Primary household language and asthma care among Latinx children. J Health Care Poor Underserved 2009;20:766–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chan KS, Keeler E, Schonlau M, Rosen M, Mangione-Smith R. How do ethnicity and primary language spoken at home affect management practices and outcomes in children and adolescents with asthma? Arch Pediatr Adolesc Med 2005;159:283–9. [DOI] [PubMed] [Google Scholar]
- 4.Lara M, Akinbami L, Flores G, Morgenstern H. Heterogeneity of childhood asthma among Hispanic children: Puerto Rican children bear a disproportionate burden. Pediatrics 2006;117:43–53. [DOI] [PubMed] [Google Scholar]
- 5.Asthma and Hispanic Americans—The Office of Minority Health. Accessed December 8, 2021. Available from: https://minorityhealth.hhs.gov/omh/browse.aspx?lvl=4&lvlid=60. [Google Scholar]
- 6.Kaufmann J, Miguel M, Lucas JA, et al. Racial/ethnic disparities in acute care utilization for pediatric asthma. Ann Fam Med 2021;. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lucas JA, Marino M, Giebultowicz S, et al. Mobility and social deprivation on primary care utilisation among paediatric patients with asthma. Fam Med Com Health 2021;9:e001085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bazemore A, Petterson S, Peterson LE, Bruno R, Chung Y, Phillips RL. Higher primary care physician continuity is associated with lower costs and hospitalizations. Ann Fam Med 2018;16:492–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pandhi N, Saultz JW. Patients’ perceptions of interpersonal continuity of care. J Am Board Fam Med 2006;19:390–7. [DOI] [PubMed] [Google Scholar]
- 10.Hudson BF, Best S, Stone P, Noble TB. Impact of informational and relational continuity for people with palliative care needs: a mixed methods rapid review. BMJ Open 2019;9:e027323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cyr MC, Martens AC, Berbiche D, Perreault S, Blais L. Continuity of care in the ambulatory treatment of adolescents with asthma. J Adolesc Health Off Health 2006;39:926.e11–17–926.e17. [DOI] [PubMed] [Google Scholar]
- 12.Enlow E, Passarella M, Lorch SA. Continuity of care in infancy and early childhood health outcomes. Pediatrics 2017;140:e20170339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.DeVoe JE, Gold R, Cottrell E, et al. The ADVANCE network: Accelerating data value across a national community health center network. J Am Med Inform Assoc 2014;21:591–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.National Asthma Education and Prevention Program. Expert panel report 3 (EPR-3): Guidelines for the diagnosis and management of asthma—summary report 2007. J Allergy Clin Immunol 2007;120:S94–138. [DOI] [PubMed] [Google Scholar]
- 15.Grohskopf LA, Alyanak E, Ferdinands JM, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices, United States, 2021–22 Influenza Season. MMWR Recomm Rep 2021;70:1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Falk NP, Hughes SW, Rodgers BC. Medications for chronic asthma. Am Fam Physician 2016;94:454–62. [PubMed] [Google Scholar]
- 17.Guidelines for the diagnosis and management of asthma 2007 (EPR-3) j NHLBI, NIH. Accessed December 8, 2021. Available from: https://www.nhlbi.nih.gov/health-topics/guidelines-for-diagnosis-management-of-asthma.
- 18.Bice TW, Boxerman SB. A quantitative measure of continuity of care. Med Care 1977;15:347–9. [DOI] [PubMed] [Google Scholar]
- 19.Brotanek JM, Halterman J, Auinger P, Weitzman MM. inadequate access to care among children with asthma from Spanish-speaking families. J Health Care Poor Underserved 2005;16:63–73. [DOI] [PubMed] [Google Scholar]
- 20.Santibanez TA, Srivastav A, Zhai Y, Singleton JA. Trends in childhood influenza vaccination coverage, United States, 2012–2019. Public Health Rep 2020;135:640–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Influenza vaccination coverage, United States, 2019–20 influenza season | influenzavaxview | seasonal influenza (influenza) | CDC. October 1, 2020. Accessed February 8, 2022. Available from: https://www.cdc.gov/influenza/influenzavaxview/coverage-1920estimates.htm.
- 22.O’Halloran AC, Holstein R, Cummings C, et al. Rates of influenza-associated hospitalization, intensive care unit admission, and in-hospital death by race and ethnicity in the United States From 2009 to 2019. JAMA Netw Open 2021;4:e2121880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cooper S, Rahme E, Tse SM, Grad R, Dorais M, Li P. Are primary care and continuity of care associated with asthma-related acute outcomes amongst children? A retrospective population-based study. BMC Prim Care 2022;23:5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Riera A, Ocasio A, Tiyyagura G, et al. Latinx caregiver experiences with asthma health communication. Qual Health Res 2015;25:16–26. [DOI] [PubMed] [Google Scholar]


