Abstract
Enterococcus casseliflavus UC73 is a clinical blood isolate with high-level resistance to gentamicin. DNA preparations from UC73 failed to hybridize with intragenic probes for aac(6′)-Ie-aph(2")-Ia and aph(2")-Ic. A 4-kb fragment from UC73 was cloned and found to confer resistance to gentamicin in Escherichia coli DH5α transformants. Nucleotide sequence analysis revealed the presence of a 906-bp open reading frame whose deduced amino acid sequence had a region with homology to the aminoglycoside-modifying enzyme APH(2")-Ic and to the C-terminal domain of the bifunctional enzyme AAC(6′)-APH(2"). The gene is designated aph(2")-Id, and its observed phosphotransferase activity is designated APH(2")-Id. A PCR-generated intragenic probe hybridized to the genomic DNA from 17 of 118 enterococcal clinical isolates (108 with high-level gentamicin resistance) from five hospitals. All 17 were vancomycin-resistant Enterococcus faecium isolates, and pulsed-field typing revealed three distinct clones. The combination of ampicillin plus either amikacin or neomycin exhibited synergistic killing against E. casseliflavus UC73. Screening and interpretation of high-level aminoglycoside resistance in enterococci may need to be modified to include detection of APH(2")-Id.
High-level gentamicin resistance (MIC ≥ 2,000 μg/ml) in enterococci is known to be associated with the aac(6′)-Ie-aph(2")-Ia gene, which encodes the bifunctional aminoglycoside-modifying enzyme AAC(6′)-APH(2") (14). The presence of this gene eliminates the synergism between a cell wall-active agent, such as ampicillin or vancomycin, and virtually all commercially available aminoglycosides—including gentamicin, tobramycin, netilmicin, kanamycin, and amikacin—except streptomycin (17). aph(2")-Ic is a midlevel gentamicin resistance gene (MIC = 256 μg/ml), found less commonly than aac(6′)-Ie-aph(2")-Ia in enterococci, that eliminates the synergism between ampicillin and gentamicin (6). We describe a new high-level gentamicin resistance gene initially found in Enterococcus casseliflavus that is distinct from aac(6′)-Ie-aph(2")-Ia and aph(2")-Ic.
(This work was presented in part at the Infectious Diseases Society of America 34th Annual Meeting, New Orleans, La., 18 to 20 September 1996 [25], and the 97th General Meeting of the American Society for Microbiology, Miami Beach, Fla., 4 to 8 May 1997 [26].)
MATERIALS AND METHODS
Bacterial strains, media, and antimicrobial susceptibilities.
Enterococci were identified by conventional biochemical criteria (13). UC73 is an E. casseliflavus blood isolate from a patient in Chicago, Ill. (20). Escherichia coli DH5α was used as the recipient for electroporation and the host to maintain recombinant plasmids. Enterococcus faecium GE1 (12) and Enterococcus faecalis FA2-2 (7) were the recipient strains in mating experiments. Gentamicin was obtained from Fluka (Buchs, Switzerland). Netilmicin, 6′-N-ethylnetilmicin, and 5-episisomicin were a gift from Karen J. Shaw (Schering-Plough Research Institute, Kenilworth, N.J.). All other antimicrobial agents were obtained from Sigma Chemical Company (St. Louis, Mo.). Transformants from electroporation were selected on Luria-Bertani plates containing gentamicin (20 μg/ml). Filter matings were performed as previously described (23). Antimicrobial susceptibilities were determined by a standardized broth microdilution method (28). Tests of synergistic killing were performed at least in triplicate to ensure reproducibility of results and were done by previously described methods (19). Synergism was defined as a ≥2-log10 decrease in the number of CFU per milliliter between the combination (ampicillin plus aminoglycoside) and its most active constituent (ampicillin) after 24 h (the aminoglycoside had no effect on the growth curve); the number of surviving organisms in the presence of the combination was ≥2-log10 CFU/ml below that in the starting inoculum. One hundred eighteen enterococcal clinical isolates (108 with high-level gentamicin resistance) from five Detroit, Mich., area hospitals were obtained to screen for the presence of the new gene.
DNA preparation and cloning.
Plasmid DNA minipreparations and total genomic DNA were obtained by a modified alkaline lysis method (27). Restriction endonuclease digestion, agarose gel electrophoresis of DNA, contour-clamped homogeneous electric field (CHEF) electrophoresis of genomic DNA, and electroporation were performed as previously described (3, 10). DNA typing of isolates was done by visual inspection of gel bands by using published criteria (22). For detection of DNA-DNA homology, biotin-labeled probes were prepared as instructed by the manufacturer (GIBCO BRL Life Technologies, Gaithersburg, Md.). The probe for aac(6′)-Ie-aph(2")-Ia was a 1.5-kb AluI fragment from E. faecalis plasmid pSF815A (14). The probe for aph(2")-Ic was generated by PCR as previously reported (6). DNA was transferred to MagnaGraph nylon membranes (Micron Separation, Inc., Westboro, Mass.) by the method of Southern and exposed to probes for hybridization (11). DNA to be sequenced was obtained as described in the Qiagen plasmid handbook (Qiagen, Inc., Chatsworth, Calif.). The vector pBluescript II KS+ (Stratagene Cloning Systems, La Jolla, Calif.) was used in standard cloning experiments (3).
DNA sequencing and PCR.
Nested deletions of cloned DNA were made by using the Erase-a-Base System from Promega (Madison, Wis.). The nucleotide sequences of both strands were determined by a modification of the dideoxynucleotide chain termination method with a Sequenase kit (version 1.0; United States Biochemical, Cleveland, Ohio) and [α-32P]dATP (Amersham Life Science, Arlington Heights, Ill.) (15, 21). PCR was performed with a GeneAmp PCR Reagent kit with AmpliTaq DNA polymerase (Perkin-Elmer, Norwalk, Conn.) (15). Computer analysis was performed by using MacVector software, version 6.0, and AssemblyLIGN, version 1.0 (Oxford Molecular Group, Oxford, United Kingdom). The GenBank database was searched by using the BLAST program from the National Center for Biotechnology Information (1). Amino acid sequences were compared by using the Gap Analysis Program from the University of Wisconsin Genetics Computer Group, version 8.1 (9).
Enzyme assays.
Aminoglycoside phosphotransferase activity was confirmed through a modified phosphocellulose paper binding assay as previously described (6, 18). A substrate was considered to be modified if its radioactive counts were greater than five times those of negative controls (8).
Nucleotide sequence accession number.
The nucleotide sequence data for the new high-level gentamicin resistance gene, aph(2")-Id, are available from GenBank under accession no. AF016483.
RESULTS
Microbiological characterization.
Aminoglycoside MICs for E. casseliflavus UC73 are shown in Table 1. The ampicillin MIC was 1.0 μg/ml, and the streptomycin MIC was 32 μg/ml. Ampicillin at 0.5 μg/ml was used in synergy studies of UC73 because ampicillin alone at 1.0 μg/ml exhibited too much killing at 24 h to easily detect synergistic killing. Synergistic killing was not seen for UC73 in time-kill studies using ampicillin (0.5 μg/ml) and either gentamicin (16 μg/ml) or netilmicin (16 μg/ml). Synergistic killing was exhibited against UC73, however, when ampicillin (0.5 μg/ml) was combined with amikacin (8 and 16 μg/ml) or with neomycin (8 and 16 μg/ml).
TABLE 1.
Susceptibilities of E. casseliflavus UC73, E. coli NC95, and E. coli DH5α(pBluescript II KS+) to aminoglycosides
| Aminoglycoside | MIC (μg/ml)
|
||
|---|---|---|---|
| UC73 | NC95a | DH5α (pBluescript II KS+) | |
| Gentamicin | >2,000 | 128 | 0.25 |
| Dibekacin | >2,000 | 64 | 1 |
| Tobramycin | >2,000 | 16 | 0.25 |
| 6′-N-Ethylnetilmicin | >2,000 | 32 | 0.5 |
| Kanamycin | 1,024 | 16 | 1 |
| 5-Episisomicin | 1,024 | 32 | 0.12 |
| Netilmicin | 64 | 2 | 0.03 |
| Neomycin | 16 | 0.31 | 0.31 |
| Amikacin | 32 | 0.25 | 0.12 |
DH5α containing pBluescript II KS+ into which a 4-kb fragment containing aph(2")-Id had been cloned.
The probes for aac(6′)-Ie-aph(2")-Ia and aph(2")-Ic did not hybridize to Southern blots of total cellular DNA from E. casseliflavus UC73. Filter matings with UC73 as the donor and E. faecium GE1 or E. faecalis FA2-2 as the recipient did not result in transfer of gentamicin resistance (frequency, <10−9 per recipient CFU). Electroporation of a plasmid preparation from UC73 into competent E. faecalis FA2-2 cells also did not result in the selection of gentamicin-resistant transformants.
Cloning and expression of the gentamicin resistance gene.
Partial Sau3AI digestions of total genomic DNA from UC73 were ligated to pBluescript II KS+ digested with BamHI. After electroporation of the ligated products, selection for gentamicin-resistant transformants yielded an E. coli DH5α derivative that contained a 7.5-kb cloned fragment. Further subcloning resulted in a gentamicin-resistant transformant, named NC95, which contained a 4-kb cloned fragment. Aminoglycoside MICs for NC95 and DH5α(pBluescript II KS+) are shown in Table 1.
Nucleotide sequencing of the gentamicin resistance gene.
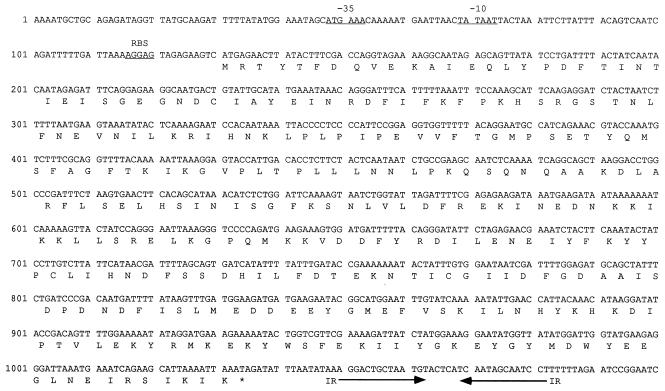
Nucleotide sequencing revealed the presence of only one open reading frame (ORF) whose predicted amino acid sequence showed homology with aminoglycoside-modifying enzymes (Fig. 1). Only recombinants that contained the entire ORF (906 bp), and not recombinants that contained a part of the ORF, were gentamicin resistant. Gap analysis revealed 54.4% similarity and 31.1% identity of APH(2")-Id with AAC(6′)-APH(2") and 48.6% similarity and 28% identity with APH(2")-Ic. This gentamicin resistance gene was designated aph(2")-Id.
FIG. 1.
Nucleotide sequence of aph(2")-Id from E. casseliflavus UC73. The potential −35 and −10 sites and the potential ribosome binding site (RBS) are underlined. The stop codon of the ORF is designated by an asterisk. Inverted repeats (IR) (two mismatched nucleotides) are designated by arrows.
Determination of phosphotransferase activity.
The crude extract prepared from negative-control E. coli DH5α(pBluescript II KS+) showed no phosphorylation of gentamicin over time (86, 95, and 95 cpm at 1, 5, and 15 min, respectively), whereas the reaction mixture containing extract from NC95 showed a significant increase in radioactivity observed over time (2,795, 6,215, and 6,415 cpm at 1, 5, and 15 min, respectively), thus showing that gentamicin phosphotransferase activity, designated APH(2")-Id, is associated with the presence of aph(2")-Id.
Identification of the new gentamicin resistance gene in E. faecium.
An 849-bp intragenic probe for aph(2")-Id was generated by PCR with synthetic oligonucleotide primers (5′-GACCAGGTAGAAAAGGCAATAGAGCAG-3′ and 5′-ATACCAATCCATATAACCATATTCCTT-3′). The probe hybridized to the Southern blots of total cellular DNA from 17 of 118 enterococcal clinical isolates. These 118 isolates were composed of 108 with high-level resistance to gentamicin (78 E. faecalis isolates, 28 E. faecium isolates, 1 E. raffinosus isolate, and 1 E. gallinarum isolate) and 10 that were gentamicin sensitive (1 E. faecalis isolate and 9 E. faecium isolates). Forty of the 118 isolates were vancomycin resistant (6 E. faecalis isolates, 33 E. faecium isolates, and 1 E. gallinarum isolate). All 17 isolates positive for the aph(2")-Id probe were vancomycin-resistant E. faecium and came from 16 patients in four of the five hospitals. The DNA from these 17 E. faecium isolates did not hybridize to the aac(6′)-Ie-aph(2")-Ia probe. CHEF gel electrophoresis showed three distinct strain types (data not shown). The probe also hybridized to the DNA on the CHEF gel from all 17 isolates. The 17 E. faecium isolates were ampicillin resistant (MIC range, 64 to 256 μg/ml). The amikacin MICs ranged from 256 to 512 μg/ml, and the netilmicin MICs ranged from 512 to ≥2,000 μg/ml. In contrast to results for E. casseliflavus UC73, tests of synergism performed on the two isolates (NC103 and SF13485) for which the ampicillin MICs were the lowest (64 μg/ml), in which ampicillin was used at 64 μg/ml and amikacin was used at 32 μg/ml, showed less than a 2-log10 difference in killing with the combination compared to the most active agent alone (average 1.34- and 0.65-log10 difference, respectively).
DISCUSSION
To date, high-level gentamicin resistance in enterococci has been associated only with the presence of the aac(6′)-Ie-aph(2")-Ia gene. Therefore, clinical laboratories test enterococcal isolates for high-level aminoglycoside resistance by using only gentamicin and streptomycin, since enterococci resistant to gentamicin are assumed to be resistant to the other clinically available aminoglycosides, except streptomycin. Our small survey showed that 16% (17 of 108) of enterococci with high-level gentamicin resistance possess aph(2")-Id and not aac(6′)-Ie-aph(2")-Ia. If these results are confirmed in more-extensive surveys, clinical laboratories may need to add amikacin to their screening protocols, since aph(2")-Id does not confer high-level resistance to amikacin and ampicillin-amikacin synergistic killing of E. casseliflavus UC73, which contains aph(2")-Id, has been shown. E. faecium NC103 and E. faecium SF13485 both contain aph(2")-Id, but the ampicillin and amikacin MICs for these strains were high, which may explain why they were not killed as effectively by ampicillin-amikacin as E. casseliflavus UC73 was. The high amikacin MICs (256 to 512 μg/ml) for the 17 E. faecium isolates containing aph(2")-Id may be due to the presence of another aminoglycoside resistance gene(s). Although an enterococcus for which the amikacin MIC is <256 μg/ml might contain aph(2")-Id and be susceptible to killing by ampicillin-amikacin, a low amikacin MIC does not always imply susceptibility to synergism. Enterococci that possess the aminoglycoside resistance gene aph(3′)-IIIa, aac(6′)-Ie-aph(2")-Ia, or ant(4′)-Ia are resistant to ampicillin-amikacin synergism but may not have high-level resistance to amikacin (MICs as low as 64 to 256 μg/ml) (2, 4, 5, 16, 17, 24). Tests for synergistic killing may thus prove to be a useful adjunct to confirm the utility of amikacin in combination therapy for isolates thought to contain aph(2")-Id. Alternatives might include the use of probes or PCR to test for the presence of aph(2")-Id and for the absence of the other three aminoglycoside resistance genes.
ACKNOWLEDGMENTS
This study was supported in part by the Department of Veterans’ Affairs; in part by the William Beaumont Hospital Research Institute; and in part by the General Clinical Research Center at the University of Michigan, funded by a grant (MO1RR00042) from the National Center for Research Resources, NIH, USPHS.
We thank Karen J. Shaw and Stephen A. Lerner for helpful discussions and Deborah D. Jaworski for assistance with computer analysis.
REFERENCES
- 1.Altschul S F, Gish W, Miller W, Myers E W, Lipman D J. Basic local alignment search tool. J Mol Biol. 1990;215:403–410. doi: 10.1016/S0022-2836(05)80360-2. [DOI] [PubMed] [Google Scholar]
- 2.Arduino R C, Murray B E. Enterococci: antimicrobial resistance. In: Mandell G L, Douglas R G, Bennett J E, editors. Update to principles and practice of infectious diseases. New York, N.Y: Churchill Livingstone Inc.; 1993. pp. 3–15. [Google Scholar]
- 3.Ausubel F M, Brent R, Kingston R E, Moore D D, Seidman J G, Smith J A, Struhl K. Current protocols in molecular biology. Vol. 1. New York, N.Y: John Wiley & Sons, Inc.; 1995. [Google Scholar]
- 4.Calderwood S B, Wennersten C, Moellering R C., Jr Resistance to antibiotic synergism in Streptococcus faecalis: further studies with amikacin and with a new amikacin derivative, 4′-deoxy, 6′-N-methylamikacin. Antimicrob Agents Chemother. 1981;19:549–555. doi: 10.1128/aac.19.4.549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Carlier C, Courvalin P. Emergence of 4′,4"-aminoglycoside nucleotidyltransferase in enterococci. Antimicrob Agents Chemother. 1990;34:1565–1569. doi: 10.1128/aac.34.8.1565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chow J W, Zervos M J, Lerner S A, Thal L A, Donabedian S M, Jaworski D D, Tsai S, Shaw K J, Clewell D B. A novel gentamicin resistance gene in Enterococcus. Antimicrob Agents Chemother. 1997;41:511–514. doi: 10.1128/aac.41.3.511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Clewell D B, Tomich P K, Gawron-Burke M C, Franke A E, Yagi Y, An F Y. Mapping of Streptococcus faecalis plasmids pAD1 and pAD2 and studies relating to transposition of Tn917. J Bacteriol. 1982;152:1220–1230. doi: 10.1128/jb.152.3.1220-1230.1982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cooksey R C, Metchock B G, Thornsberry C. Microplate phosphocellulose binding assay for aminoglycoside-modifying enzymes. Antimicrob Agents Chemother. 1986;30:883–887. doi: 10.1128/aac.30.6.883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Devereux J, Haeberli P, Smithies O. A comprehensive set of sequence analysis programs for the VAX. Nucleic Acids Res. 1984;12:387–395. doi: 10.1093/nar/12.1part1.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Donabedian S M, Chow J W, Boyce J M, McCabe R E, Markowitz S M, Coudron P E, Kuritza A, Pierson C L, Zervos M J. Molecular typing of ampicillin-resistant, non-β-lactamase-producing Enterococcus faecium from diverse geographic areas. J Clin Microbiol. 1992;30:2757–2761. doi: 10.1128/jcm.30.11.2757-2761.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Donabedian S M, Chow J W, Shlaes D M, Green M, Zervos M J. DNA hybridization and contour-clamped homogeneous electric field electrophoresis for identification of enterococci to the species level. J Clin Microbiol. 1995;33:141–145. doi: 10.1128/jcm.33.1.141-145.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eliopoulos G M, Wennersten C, Zighelboim-Daum S, Reiszner E, Goldmann D, Moellering R C., Jr High-level resistance to gentamicin in clinical isolates of Streptococcus (Enterococcus) faecium. Antimicrob Agents Chemother. 1988;32:1528–1532. doi: 10.1128/aac.32.10.1528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Facklam R R, Collins M D. Identification of Enterococcus species isolated from human infections by a conventional test scheme. J Clin Microbiol. 1989;27:731–734. doi: 10.1128/jcm.27.4.731-734.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ferretti J J, Gilmore K S, Courvalin P. Nucleotide sequence analysis of the gene specifying the bifunctional 6′-aminoglycoside acetyltransferase 2"-aminoglycoside phosphotransferase enzyme in Streptococcus faecalis and identification and cloning of gene regions specifying the two activities. J Bacteriol. 1986;167:631–638. doi: 10.1128/jb.167.2.631-638.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jaworski D D, Clewell D B. A functional origin of transfer (oriT) on the conjugative transposon Tn916. J Bacteriol. 1995;177:6644–6651. doi: 10.1128/jb.177.22.6644-6651.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Krogstad D J, Korfhagen R R, Moellering R C, Jr, Wennersten C, Swartz M N. Aminoglycoside-inactivating enzymes in clinical isolates of Streptococcus faecalis: an explanation for antibiotic synergism. J Clin Invest. 1978;62:480–486. doi: 10.1172/JCI109149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leclercq R, Dutka-Malen S, Brisson-Noël A, Molinas C, Derlot E, Arthur M, Duval J, Courvalin P. Resistance of enterococci to aminoglycosides and glycopeptides. Clin Infect Dis. 1992;15:495–501. doi: 10.1093/clind/15.3.495. [DOI] [PubMed] [Google Scholar]
- 18.Perlin M H, Lerner S A. Amikacin resistance associated with a plasmid-borne aminoglycoside phosphotransferase in Escherichia coli. Antimicrob Agents Chemother. 1979;16:598–604. doi: 10.1128/aac.16.5.598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Perri M B, Chow J W, Zervos M J. In vitro activity of sparfloxacin and clinafloxacin against multidrug-resistant enterococci. Diagn Microbiol Infect Dis. 1993;17:151–155. doi: 10.1016/0732-8893(93)90026-4. [DOI] [PubMed] [Google Scholar]
- 20.Sahm D F, Gilmore M S. Transferability and genetic relatedness of high-level gentamicin resistance among enterococci. Antimicrob Agents Chemother. 1994;38:1194–1196. doi: 10.1128/aac.38.5.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Su Y A, Clewell D B. Characterization of left four kilobases of conjugative transposon Tn916: determinants involved in excision. Plasmid. 1993;30:234–250. doi: 10.1006/plas.1993.1055. [DOI] [PubMed] [Google Scholar]
- 22.Tenover F C, Arbeit R D, Goering R V, Mickelsen P A, Murray B E, Persing D H, Swaminathan B. Interpreting chromosomal DNA restriction patterns produced by pulsed-field gel electrophoresis: criteria for bacterial strain typing. J Clin Microbiol. 1995;33:2233–2239. doi: 10.1128/jcm.33.9.2233-2239.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thal L A, Chow J W, Clewell D B, Zervos M J. Tn924, a chromosome-borne transposon encoding high-level gentamicin resistance in Enterococcus faecalis. Antimicrob Agents Chemother. 1994;38:1152–1156. doi: 10.1128/aac.38.5.1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Trieu-Cuot P, Courvalin P. Nucleotide sequence of the Streptococcus faecalis plasmid gene encoding the 3′5"-aminoglycoside phosphotransferase type III. Gene. 1983;23:331–341. doi: 10.1016/0378-1119(83)90022-7. [DOI] [PubMed] [Google Scholar]
- 25.Tsai S, Zervos M J, Clewell D B, Shaw K J, Sahm D F, Chow J W. Program and abstracts of the Infectious Diseases Society of America 34th Annual Meeting. 1996. A novel high-level gentamicin resistance gene in Enterococcus casseliflavus, abstr. 163; p. 14. [Google Scholar]
- 26.Tsai S, Zervos M J, Donabedian S, Clewell D B, Chow J W. Abstracts of the 97th General Meeting of the American Society for Microbiology 1997. Washington, D.C: American Society for Microbiology; 1997. Nucleotide sequence analysis of a new gentamicin resistance gene in Enterococcus casseliflavus, abstr. A-128; p. 23. [Google Scholar]
- 27.Wirth R, An F Y, Clewell D B. Highly efficient protoplast transformation system for Streptococcus faecalis and a new Escherichia coli-S. faecalis shuttle vector. J Bacteriol. 1986;165:831–836. doi: 10.1128/jb.165.3.831-836.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Woods G L, Washington J A. Antibacterial susceptibility tests: dilution and disk diffusion methods. In: Murray P R, Baron E J, Pfaller M A, Tenover F C, Yolken R H, editors. Manual of clinical microbiology. 6th ed. Washington, D.C: American Society for Microbiology; 1995. pp. 1327–1341. [Google Scholar]