Abstract
Scholars consistently find that renters have poorer health outcomes when compared with homeowners. Health disparities between renters and homeowners likely widen over the life course, yet few studies have examined this link among older adults, and the connection is not fully understood. Homeowners’ relative socioeconomic advantage may explain their better health; renters also more commonly experience adverse housing conditions and financial challenges, both of which can harm health. In this paper, we analyze the extent to which socioeconomic advantage, housing conditions, and financial strain explain the relationship between homeownership and health among adults over age 50, using Health and Retirement Study 2010/2012 data to assess cardiometabolic risk levels using biomarkers for inflammation, cardiovascular health, and metabolic function. We find that people living with poor housing conditions and financial strain have higher cardiometabolic risk levels, even taking socioeconomic advantage into account. This analysis sheds light on the housing-related health challenges of older adults, especially older renters.
Keywords: Homeownership, older adults, housing affordability, housing conditions, health, cardiometabolic risk
Introduction
While most older adults in the US own their homes, an increasing share of people over age 65 adults are renters (Joint Center for Housing Studies, 2019; Spader, 2019). Yet older renters—over 7 million households—have been largely overlooked in housing policy conversations. Renting has been linked with adverse health outcomes in terms of self-rated health (Bell et al., 2020; Moor et al., 2017), mental health (Baker et al., 2013; Szabo et al., 2018), cardiovascular disease (Woodward et al., 2003), chronic obstructive pulmonary disease (Coventry et al., 2011), stroke (Jackson et al., 2014), cancer (Sharpe et al., 2014), and even mortality (Laaksonen et al., 2008). This suggests that older renters are a vulnerable population who deserve more attention to understand their health challenges and risks.
There are two main hypotheses for why health disparities exist between homeowners and renters. One explanation is that socioeconomically advantaged people are more often able to purchase homes, so homeowners tend to be healthier than renters to begin with (Baker et al., 2013). Thus any differences in health may reflect socioeconomic advantage rather than housing status. Another explanation is that renters more commonly experience housing problems such as affordability challenges or poor housing quality and maintenance, and are more often exposed to mold, vermin, and cold in their homes (American Housing Survey, 2019). Both harmful exposures in the home environment and stress of dealing with housing problems can contribute to inflammation and the development of respiratory problems and chronic conditions such as asthma, diabetes, and cardiovascular disease (Bonnefoy et al., 2003; Rudnai et al., 2009; Webb et al., 2013). While there is a strong consensus that the compositional differences resulting from selection explain some of the association between homeownership and health, few studies have examined the extent to which housing conditions may also help to explain this relationship.
And few studies have examined health disparities between older homeowners and renters, though there is reason to suppose that they may widen with age (Szabo et al., 2018). Older adults are often more sensitive to harmful exposures such as cold (Ormandy & Ezratty, 2012), and have potentially had more total exposure over the life course. Homeowners’ and renters’ housing cost burdens diverge in later life; homeowners can potentially reduce their housing costs in old age by paying off their mortgages, while renters’ housing costs may stay steady or even rise. Compositional differences in health are also likely to become more pronounced at older ages with the accumulation of advantage or disadvantage over the life course (Willson et al., 2007).
In this paper, we examine the extent to which health disparities between renters and homeowners are related to differences in housing conditions and financial strain. We analyze the links between housing and health among adults over age 50, using Health and Retirement Study (HRS) 2010/2012 data to measure their cardiometabolic risk (CMR) levels based on eight biomarkers of inflammation, cardiovascular health, and metabolic function. We address three main research questions: First, do middle aged and older renters in the US have higher levels of CMR than homeowners? Second, to what extent do home conditions, financial strain, residential instability, and other housing problems help explain this relationship? Third, are specific aspects of CMR more sensitive to housing conditions?
Background
Scholars find evidence for the link between homeownership and health across a number of contexts, including the US, Britain, Europe, Asia, Australia and New Zealand. Homeownership often figures in studies of the material, psychosocial, and behavioral factors that help to explain the connections between socioeconomic status and health. Homeownership emerges as one of the strongest mediators between socioeconomic status and health in contexts as diverse as Scotland (Robertson et al., 2015) and Japan (Hiyoshi et al., 2014). Research in the US context also shows that homeownership partially mediates the association between race/ethnicity and health (Bell et al., 2020; Boen et al., 2020). While studies comparing older renters and homeowners are scarce, Szabo et al (2018) find that in New Zealand the health disparity between older homeowners and renters increases with age.
Selection into homeownership
There is debate about the underlying reasons for this connection. Some argue that the homeowner health advantage is entirely due to the selection of more advantaged, healthier people into homeownership (Baker et al., 2013). Selection is facilitated by the mortgage lending process, which excludes people with limited financial resources and poor credit. Differences in family wealth (Hall & Crowder, 2011; Lee et al., 2020), and racial discrimination in mortgage lending (Quillian et al., 2020) amplify disparities in access to homeownership. The association between homeownership and socioeconomic status is so strong that researchers sometimes treat homeownership as a proxy for socioeconomic status (Moor et al., 2017). Yet most studies that examine the link between homeownership and health among adults find that an association remains when accounting for differences in socioeconomic status (Ellaway et al., 2016; Jackson et al., 2014; Laaksonen et al., 2008; Macintyre et al., 1998). Some of the remaining association may be due to concrete differences between renters’ and homeowners’ housing situations. Studies of the benefits of parental homeownership for children have found that together, selection into homeownership and observable housing characteristics explain differences in outcomes between owners’ and renters’ children (Aaronson, 2000; Barker & Miller, 2009; Galster et al., 2007; Green & White, 1997). This may hold for older adults as well.
Housing conditions
Rental housing is often in worse condition than owner-occupied housing because rental housing tends to be older and less well-maintained (Survey of Construction, 2019; American Housing Survey, 2019; American Community Survey, 2015–19). Landlords are responsible for rental unit maintenance, yet they have fewer incentives to maintain their properties than homeowners, who benefit from both the investment and use value of their homes (Henderson & Ioannides, 1983). Renters usually cannot make repairs or resolve problems without their landlords’ cooperation.
A small handful of studies find that housing conditions are a key factor linking homeownership and health. Suggestively, Aldabe et al (2011) find that housing conditions—but not homeownership—are associated with self-rated health in the European context. Ellaway and Macintyre (1998) find that renters more commonly experience dampness, vibrations, noise, and other hazards, as well as difficulty heating their homes, and that these negative housing conditions are associated with depression and longstanding illness. Similarly, Ganesh et al (2018) find that children of renters are exposed to more smoke, musty smells, mold, leaks, and vermin than children of homeowners, and that both mold exposures and leaks are associate with heightened risk of asthma. Among older adults, Webb et al (2013) find that renters and those who have difficulty paying for heating fuel have worse respiratory health.
Aside from the link with homeownership, there is ample evidence that adverse housing conditions are related to poor health, especially for older adults. Wilkinson et al (2001) show that older homes in the UK are harder to heat and therefore colder, and find a connection between cold homes and excess winter deaths among older adults. In addition to inadequate heating, leaks, damp, and mold are associated with older adults’ respiratory problems and bone and joint conditions (Gibney et al., 2018). Older adults lacking elevators and adequate heating also have more limitations in physical functioning, including reduced agility, frailty, and exhaustion (García-Esquinas et al., 2016). Several studies include home inspections in addition to residents’ survey responses. In an in-depth face-to-face survey of housing conditions and health in Eastern Europe, Bonnefoy et al (2003) find that poor air quality, mold, temperatures, and noise are associated with asthma and allergies, respiratory conditions, self-rated health, and mental health. A World Health Organization study of housing conditions and health in eight European cities (Ormandy, 2009), provides evidence linking a range of health problems with noise (Niemann et al., 2009), indoor air pollution (Annesi-Maesano et al., 2009), damp and mold (Rudnai et al., 2009), and cold (Croxford, 2009).
Housing affordability and instability
Homeowners tend to have security of tenure, fixed mortgage payments, and relatively stable property tax bills; renters often face rent increases, and in most states their ability to remain in their home is subject to landlords’ decisions about whether to renew their lease (Fenelon & Mawhorter, 2020). The gap between homeowners’ and renters’ housing affordability widens at older ages, when more homeowners own their homes free and clear, while renters remain vulnerable to rising rents. Housing affordability challenges have been linked with poor health outcomes, especially among renters (Bentley et al., 2016; Kavanagh et al., 2016; Mason et al., 2013; Meltzer & Schwartz, 2016; Pollack et al., 2010) and those living in substandard housing conditions (Park & Seo, 2020).
Residential instability also appears to play a role in differences in health between homeowners and renters (Acolin, 2020). Morris (2018) finds that the ongoing stress of both housing cost increases and housing instability are key factors in the poor health outcomes of renters. Studies of housing assistance programs, which address both affordability problems and instability, have found improved health outcomes for public housing residents(Fenelon et al., 2017), and lower health care spending among both public housing residents and voucher recipients (Pfeiffer, 2018). Housing affordability and instability are thought to impact health by causing stress; these studies show links with both mental and physical health outcomes.
Conceptual framework
As shown in our conceptual model (Figure 1), we theorize that socioeconomic characteristics including education and race/ethnicity help determine housing tenure, and are linked with health through other material, psychosocial, and behavioral pathways. Housing tenure, in turn, is linked with housing circumstances such as physical home conditions, housing affordability, residential instability, neighborhood quality, and difficulty resolving housing problems. Adverse housing conditions can generate harmful exposures within the home and stress processes which can lead to inflammation, cardiovascular problems, and metabolic dysfunction.
Figure 1.
Conceptual model of the links between socioeconomic status, housing tenure, housing conditions, and health
Health measures
Most studies of housing tenure and health focus on self-rated health or diagnosed conditions. Both types of measures have drawbacks. Self-rated health can be somewhat unreliable, especially for disadvantaged groups (Zajacova & Dowd, 2011). Diagnosed conditions are long-term outcomes, which can develop over the course of years based on a number of genetic, behavioral, and environmental risk factors. Disadvantaged populations in the US may lack access to health care services, and are less likely to receive timely diagnoses for their conditions (Schwartz et al., 2003).
Recently scholars have turned to more proximal measures of health, using physical indicators and blood tests to detect fine-grained differences in health status (Crimmins et al., 2010; Mitchell et al., 2019; Seeman et al., 2004). These biomarkers are the same measures that doctors use to assess patients’ health, and can reveal increased risk for chronic conditions and disease before onset or diagnosis. In this paper, we combine biomarkers for inflammation, cardiovascular health, and metabolic function—all of which may be affected by housing conditions—to create a summary measure of physiological dysregulation reflecting multisystem health problems. This measure of cardiometabolic risk (CMR) offers a more reliable measure than self-rated health, and a more sensitive measure of health status than disease diagnoses.
Data and Methods
We use data from the Health and Retirement Study (HRS), a nationally-representative longitudinal survey of US adults over age 50 conducted every other year since 1992 to collect information on older adults’ economic circumstances and health as they age. Our analysis includes HRS respondents in the 2010/2012 biomarker sample (n = 13,066). The HRS collects biomarker data as part of enhanced face-to-face (EFTF) interviews. A random half of respondents are selected for EFTF interviews in one survey wave, with the other half selected for EFTF in the following survey wave. The two half samples can be combined and adjusted with specially-designed biomarker weights to form the full biomarker sample.
Our analytic sample includes middle aged along with older adults to compare people at different stages in the aging process, before the highest-risk respondents are excluded from the sample by selective mortality. We exclude respondents who live in retirement communities (n = 687) and those who live rent-free with family (n = 398). We also exclude mobile home residents (n = 698), since many own their mobile home but rent their site, a mixed form of housing tenure distinct from standard homeownership or renting. Of the remaining 11,371 respondents, 522 are missing information on housing tenure, our key variable of interest, 295 lack information on their home condition, 139 are missing information on the years since their last move, and 78 are missing a neighborhood safety measure. We further restrict the sample to the 8,281 respondents who have information from the leave-behind questionnaire on their difficulty in paying bills or ongoing housing problems. Less than 1% (49) are missing information on socioeconomic and health behavior variables in our analysis. The final analytic sample consists of 8,231 respondents, including 6,896 respondents living in owner-occupied housing and 1,335 respondents living in rental housing.
Cardiometabolic risk
We construct a count that represents CMR based on whether a respondent has a clinical level of risk according to eight biomarkers: C-reactive protein, systolic and diastolic blood pressure, heart rate, glycosylated hemoglobin, high-density lipoprotein and total cholesterol, and waist circumference. We use NHANES equivalent assay values, which have been adjusted for differences between the dried blood spot measures and conventional assays (see Crimmins et al., 2015 for more information). C-reactive protein is a marker of inflammation produced by the liver; values over 3 ug/mL are considered high risk. Systolic and diastolic blood pressure and resting heart rate are indicators of cardiovascular health. Systolic blood pressures over 140 mmHg, diastolic blood pressures over 90 mmHg, and resting heart rates over 90 beats per minute are considered high risk. Glycosylated hemoglobin, high-density lipoprotein (HDL) cholesterol, total cholesterol, and waist circumference are measures of metabolic functioning. Glycosylated hemoglobin, an indicator of blood sugar control, is considered a risk at values over 6.5%. Low values of HDL cholesterol (under 40 mg/dL) and high total cholesterol (over 240 mg/dL) are considered risk factors, as are waist circumferences over 35 inches for women and over 40 inches for men. After determining whether respondents are at risk for each of the biomarkers, we construct a CMR count measure reflecting the number of biomarkers for which a respondent is in the high risk category and ranging from 0 to 8.
Socioeconomic selection measures
We include two socioeconomic characteristics associated with selection into homeownership: educational attainment and race/ethnicity, both of which may confound the relationship between homeownership and health. Education is a marker of socioeconomic advantage earlier in life, and is closely linked with homeownership. We categorize the education measure to compare those without a high school degree, high school graduates, and college graduates. We compare non-Hispanic White, non-Hispanic Black, Hispanic, and non-Hispanic Other respondents since people who are not White may face discrimination in mortgage lending and other barriers to homeownership.
Housing and neighborhood measures
Home condition.
Our home condition measure is primarily based on interviewer observations of respondents’ homes. Interviewers rate the relative maintenance of the respondents’ home as ‘same,’ ‘better,’ or ‘worse’ compared with the maintenance of the surrounding buildings on a four-point scale: ‘very well,’ ‘mixed – could use a paint job,’ ‘poorly – need painting and minor repairs,’ and ‘very poorly – dilapidated.’ To measure the respondent’s home condition, we start with the maintenance of surrounding buildings, then adjust according to the relative upkeep of the respondents’ home. We then dichotomize the home condition variable to compare respondents with ‘poor or very poor’ versus those with ‘very good or mixed’ home condition.
Interviewers are not always able to visit respondents’ homes, and so 16% of the sample is missing interviewer observations. Rather than excluding these respondents, in these cases we use respondents’ own home condition rating, with the question, ‘How about the physical condition of your home, would you say it is in excellent, very good, good, fair, or poor condition?’ We assign respondents who rated their homes as in poor condition to the ‘poor or very poor’ category, and those with ‘fair’ or better condition to the ‘mixed or very good’ category. Responses to this question are somewhat correlated with interviewer ratings (corr. = .44), but we opted not to rely solely on respondents’ assessments because they are more likely to be subjective and inconsistent across respondents, and they are less timely, since this question is only asked in the wave after a respondent moves, or when they enter the study.
Current and ongoing housing problems.
Differences in the prevalence of current and ongoing problems between homeowners and renters are likely to reflect differences in their ability to avoid and resolve housing problems based on the legal frameworks around homeownership and renting in the US context. As part of the leave-behind questionnaire, the HRS includes a question about whether respondents face ‘current and ongoing housing problems lasting twelve months or longer,’ and asks ‘If the problem is happening to you, indicate how upsetting it has been.’ The multiple-choice responses include ‘no, didn’t happen,’ ‘yes, but not upsetting,’ ‘yes, somewhat upsetting,’ and ‘yes, very upsetting.’ We dichotomize this variable to compare those with versus without current and ongoing housing problems, regardless of how upsetting they are. This variable may represent problems with the physical condition, size, or layout of a home, housing affordability challenges, housing insecurity, problems with a landlord, or other housing-related problems.
Residential mobility.
To understand whether differences in residential mobility confound the relationship between homeownership and health among older adults, we construct a measure of the number of years since a respondent’s last move. In each survey wave, HRS respondents are asked whether they moved since the previous wave two years earlier, and if so, the year and month of their most recent move. The date of their most recent move is also asked in the year when they enter the study. We use these responses to determine whether respondents have lived in their current home for two years or less, for three to five years, or for over five years.
Neighborhood safety.
Housing conditions are closely linked with neighborhood conditions, and so we include a measure of the respondent’s perception of their neighborhood safety. We dichotomize neighborhood safety to compare those with ‘poor’ or ‘fair’ neighborhood safety ratings versus those with ‘good,’ ‘very good,’ or ‘excellent’ neighborhood safety ratings.
Financial measures
Income and wealth.
We log-normalize the measure of respondents’ annual household income. We also include wealth, to account for older adults who may have low incomes but enough savings for financial security. We indicate whether the respondent’s household holds above-median non-housing wealth, which includes the net value of checking, savings, and money market accounts, stocks, bonds, other investments, retirement savings, and other assets, minus non-mortgage debt. We exclude home equity because it generally cannot be used to pay for living expenses while owners remain in their homes.
Financial strain.
We include a measure of whether respondents have difficulty paying bills, to determine whether financial strain in part explains differences in CMR between renters and owners. A measure reflecting respondents’ experience of financial strain should be more closely linked with health outcomes than raw dollar amounts, since financial strain is theorized to impact health through stress pathways. In the leave-behind questionnaire as part of the EFTF interview, respondents answer the multiple-choice question, ‘How difficult is it for you or your family to meet monthly payments on your or your family’s bills?’ Responses include ‘not at all difficult,’ ‘not very difficult,’ ‘somewhat difficult,’ ‘very difficult,’ and ‘completely difficult.’ We dichotomize this measure to compare those who have no difficulty paying bills with all others. Since we take household income and wealth into account, this measure should reflect the relative burden of bills, including housing costs (the largest monthly bill for most households) as well as other living expenses.
Health resources and behavior
We expect that socioeconomic characteristics are linked with health outcomes through other material, psychosocial, and behavioral pathways besides housing conditions. We indicate whether a respondent has health insurance to account for homeowners’ advantages in financial resources and access to health care. Prior studies find that smoking behavior and physical activity help explain the link between socioeconomic status, homeownership, and health (Pollack et al., 2010; Robertson et al., 2015; Woodward et al., 2003), so we also include these measures.
Demographic control measures
Prior studies find differential relationships between homeownership and health between women and men (Aldabe et al., 2011; Sharpe et al., 2014; Woodward et al., 2003), so we adjust for gender in our analysis. We adjust for age with categories for ages 51 to 59, 60 to 69, 70 to 79, and 80 and over, and control for household size.
Statistical analysis
Our first objective is to determine whether older renters have higher levels of CMR than older homeowners. We then analyze whether this association is partially driven by housing conditions and finances, or whether it can be fully explained by the selection of more advantaged, healthier people into homeownership. Finally, we examine whether housing tenure and housing conditions are related to specific aspects of CMR, including inflammation, cardiovascular health, and metabolic function.
We conduct a series of Poisson regressions with the CMR count as the dependent variable. The first model examines CMR by housing tenure controlling for age, gender, and household size. The second model adjusts for socioeconomic characteristics related to selection into homeownership, as well as housing and neighborhood conditions. The third model adjusts for financial measures as well. The fourth model includes health resources and behavior. Since the CMR biomarkers represent various dimensions of cardiovascular and metabolic health, it is possible that housing conditions may have distinct relationships with each measure. We run separate logistic regressions for whether a respondent is at risk on each CMR biomarker. We apply HRS biomarker sample weights in all analyses.
Results
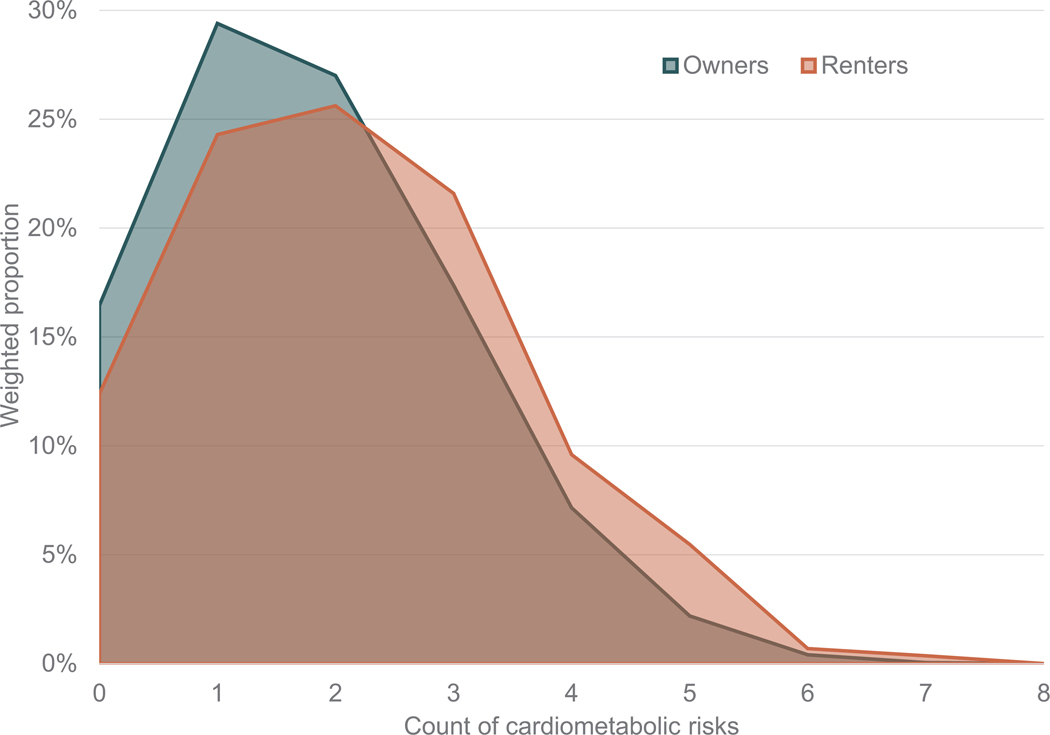
Table 1 reports the weighted sample characteristics, presented separately for people living in owner-occupied and rental housing. Owners (n = 6,896) make up the majority of the sample, though there are sufficient renters (n = 1,335) for statistical analysis. Owners are at risk for an average of 1.778 of the eight possible risk factors, while renters are at risk for an average of 2.127 risk factors (difference: .349, p < .001). We also examine the distribution of CMR scores for homeowners and renters, as shown in Figure 2. A larger share of owners have CMR scores of two or less, while a larger share of renters have CMR scores of three or more.
Table 1.
Weighted sample characteristics by housing tenure
| Health and Retirement Study 2010/2012 | Owners | Renters | Difference | |||
|---|---|---|---|---|---|---|
| Respondents in analytic sample (n = 8,231) | (n = 6,896) | (n = 1,335) | t-tests | |||
|
| ||||||
| Cardiometabolic Risk | Mean | S.E. | Mean | S.E. | Difference | |
|
| ||||||
| Mean count of risks (of 8 possible factors) | 1.778 | .021 | 2.127 | .051 | .349 | *** |
| Socioeconomic Selection Measures | Prop. | S.E. | Prop. | S.E. | Difference | |
|
| ||||||
| No high school degree | .09 | .00 | .21 | .01 | .12 | *** |
| High school graduate | .58 | .01 | .63 | .02 | .05 | ** |
| College graduate | .34 | .01 | .16 | .01 | −.17 | *** |
| White | .86 | .01 | .63 | .02 | −.23 | *** |
| Black | .06 | .00 | .20 | .02 | .14 | *** |
| Hispanic | .06 | .01 | .13 | .01 | .07 | *** |
| Other | .03 | .00 | .04 | .01 | .01 | |
| Housing and Neighborhood Measures | ||||||
|
| ||||||
| Home condition poor or very poor | .05 | .00 | .13 | .01 | .08 | *** |
| 2 years or less since last move | .06 | .00 | .35 | .02 | .29 | *** |
| 3 to 5 years since last move | .09 | .01 | .21 | .02 | .12 | *** |
| Over 5 years since last move | .85 | .01 | .44 | .02 | −.41 | *** |
| Current and ongoing housing problem | .13 | .00 | .33 | .02 | .20 | *** |
| Neighborhood safegy poor or fair | .07 | .01 | .19 | .02 | .12 | *** |
| Financial Measures | ||||||
|
| ||||||
| Household income, log-normalized (mean) | 11.01 | .02 | 10.22 | .04 | −.79 | *** |
| Above median non-housing wealth | .55 | .01 | .13 | .02 | −.42 | *** |
| Difficulty paying bills | .55 | .01 | .78 | .02 | .24 | *** |
| Health Resources and Behavior | ||||||
|
| ||||||
| Has health insurance | .95 | .00 | .83 | .02 | −.11 | *** |
| Smokes now or smoked in past | .53 | .01 | .66 | .01 | .13 | *** |
| Physical activity more than once per week | .61 | .01 | .51 | .02 | −.11 | *** |
| Demographic Control Measures | ||||||
|
| ||||||
| Age 51–59 | .35 | .01 | .46 | .02 | .12 | *** |
| 60–69 | .35 | .01 | .29 | .01 | −.06 | ** |
| 70–79 | .20 | .01 | .13 | .01 | −.07 | *** |
| 80–84 | .10 | .01 | .11 | .02 | .01 | |
| Female | .53 | .00 | .58 | .02 | .05 | ** |
| One person household | .18 | .01 | .38 | .02 | .20 | *** |
| Two person household | .58 | .01 | .33 | .02 | −.25 | *** |
| Three or more person household | .24 | .01 | .29 | .02 | .05 | * |
p < .05
p < .01
p < .001
Figure 2.
Weighted proportion of owners and renters by count of cardiometabolic risks
Renters and homeowners have widely different socioeconomic characteristics. The majority of both renters and homeowners are high school graduates, yet the share of renters who have college degrees is under half that of owners, and the share of renters who lack a high school degree is more than twice that of owners. Fully 86% of owners in the sample are White, while 63% of renters are White, a difference of 23 percentage points (p < .001). Twenty percent of renters are Black, 13% are Hispanic, and 4% have another race/ethnicity.
The differences in housing and financial measures by tenure are considerable. Figure 3 shows the detailed distribution of key housing, neighborhood, and financial characteristics by housing tenure. Three quarters of owners’ homes are in very good condition, while half of renters’ homes are in very good condition. Merely 5% of owners’ homes are in fair or poor condition, while 13% of renters’ homes are in fair or poor condition. Only 13% of owners face a current and ongoing housing problem, while a third of renters face housing problems. Fully 85% of owners have lived in their homes for more than five years, while under half of renters have lived in their homes that long, and over a third have moved within the past two years. In terms of neighborhoods, 7% of owners and 19% of renters rate their safety as poor or fair.
Figure 3.
Home condition, ongoing housing problems, neighborhood safety, and difficulty paying bills by housing tenure
Renters have lower household incomes than owners. More than half of homeowners (55%) have above-median non-housing wealth, while only 13% of renters have similar levels of household assets. Similarly, 55% of owners report difficulty paying bills, while 78% of renters are under financial strain. In terms of health resources and behavior, fewer renters have health insurance, more renters smoke or have smoked in the past, and a slightly higher proportion of owners engage in moderate or vigorous physical activity more than once per week. Renters tend to be younger than owners, a slightly higher share are women, and more renters live in one-person households or three or more-person households than owners, who mostly live in two-person households.
Cardiometabolic risk levels vary across these housing and financial characteristics as well as across housing tenure. Table 2 shows mean CMR levels for each of the housing and financial characteristics included in our analysis. As expected, those with worse home condition, difficulty paying bills, and current and ongoing housing problems are at risk for more of the CMR measures on average. Respondents who have moved within the past two years also have slightly higher CMR levels than those who have been in their homes for three to five years, though there is less of a contrast by residential mobility than for the other housing and financial measures.
Table 2.
Mean cardiometabolic risk levels by housing characteristics
| Health and Retirement Study 2010/2012 | CMR | Difference | ||
|---|---|---|---|---|
| Respondents in analytic sample (n = 8,231) | Mean | S.E. | t-tests | |
|
| ||||
| Housing tenure | ||||
| Owners | 1.778 | .021 | ||
| Renters | 2.127 | .051 | .349 | *** |
| Home maintenance | ||||
| Very good or mixed | 1.788 | .019 | ||
| Poor or very poor | 2.373 | .073 | .585 | *** |
| Current and ongoing housing problem | ||||
| No problem | 1.767 | .023 | ||
| Current and ongoing problem | 2.133 | .048 | .366 | *** |
| Years since last move | ||||
| 2 years or less | 1.933 | .056 | ||
| 3 to 5 years | 1.797 | .049 | −.136 | * |
| Over 5 years | 1.814 | .023 | .017 | |
| Neighborhood safety | ||||
| Good, very good, or excellent | 1.793 | .020 | ||
| Poor or fair | 2.156 | .060 | .363 | *** |
| Difficulty paying bills | ||||
| Not at all difficult | 1.667 | .027 | ||
| Difficult to pay bills | 1.938 | .026 | .271 | *** |
p < .05
p < .01
p < .001
Analysis: Cardiometabolic risk count
Table 3 presents the results of Poisson regressions for CMR scores. In the first model, adjusted for age, gender, and household size, the coefficient for renting is .193 (p < .001). Converted into predicted CMR scores, as shown in Figure 4, this means that owners have an average CMR score of 1.772, while renters have an average CMR score of 2.148, a difference of .376. In the second model incorporating socioeconomic selection measures and housing and neighborhood characteristics, the coefficient for renting is reduced to .078 (p < .05). Education is associated with lower CMR levels, while Black respondents have higher CMR levels. Those with homes in poor condition and those with current and ongoing housing problems have higher CMR levels. Neither residential stability or neighborhood safety have a measurable association with CMR. Socioeconomic advantage and housing conditions appear to explain much of the difference between renters’ and owners’ CMR levels.
Table 3.
Estimated coefficients from Poisson regressions measuring the association between cardiometabolic risk count and housing tenure, socioeconomic and demographic measures, housing and neighborhood measures, finances, and health resources and behaviors
| Poisson Regressions | Model 1 | Model 2 | Model 3 | Model 4 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DV: Count of Cardiometabolic Risks | Coef. | S.E. | Coef. | S.E. | Coef. | S.E. | Coef. | S.E. | ||||
|
| ||||||||||||
| Homeownership | ||||||||||||
| Rent home, ref. own home | .193 | *** | .026 | .078 | * | .031 | .042 | .031 | .036 | .030 | ||
| Socioeconomic Selection Measures | ||||||||||||
| Education, ref. no high school degree | ||||||||||||
| High school graduate | −.055 | * | .027 | −.032 | .027 | −.017 | .026 | |||||
| College graduate | −.255 | *** | .027 | −.196 | *** | .027 | −.159 | *** | .025 | |||
| Race and ethnicity, ref. White | ||||||||||||
| Black | .220 | *** | .022 | .186 | *** | .022 | .176 | *** | .022 | |||
| Hispanic | .048 | .027 | .017 | .028 | .022 | .027 | ||||||
| Other | .043 | .063 | .028 | .061 | .035 | .061 | ||||||
| Housing and Neighborhood Measures | ||||||||||||
| Home condition poor or very poor | .174 | *** | .034 | .145 | *** | .034 | .132 | *** | .034 | |||
| Current and ongoing housing problem | .106 | *** | .029 | .077 | ** | .029 | .072 | * | .029 | |||
| Years since last move, ref. 2 years or less | ||||||||||||
| 3 to 5 years | −.014 | .037 | −.008 | .036 | .003 | .036 | ||||||
| Over 5 years | −.007 | .035 | −.005 | .035 | .004 | .034 | ||||||
| Neighborhood safety poor or fair | .025 | .033 | .011 | .034 | −.001 | .033 | ||||||
| Financial Measures | ||||||||||||
| Household income, log-normalized | −.011 | .007 | −.002 | .008 | ||||||||
| Non-housing wealth above median | −.120 | *** | .024 | −.100 | *** | .024 | ||||||
| Difficulty paying bills | .057 | * | .022 | .049 | * | .022 | ||||||
| Health Resources and Behaviors | ||||||||||||
| Has health insurance | −.081 | * | .040 | |||||||||
| Smokes now or in past | .021 | .014 | ||||||||||
| Physical activity more than once per week | −.187 | *** | .019 | |||||||||
| Demographic Control Measures | ||||||||||||
| Age, ref. 51–59 years old | ||||||||||||
| 60–69 years old | .105 | *** | .030 | .101 | *** | .027 | .116 | *** | .026 | .108 | *** | .026 |
| 70–79 years old | .131 | *** | .025 | .117 | *** | .023 | .138 | *** | .023 | .124 | *** | .024 |
| 80 and older | .107 | ** | .034 | .091 | ** | .032 | .112 | *** | .030 | .092 | ** | .031 |
| Female, ref. male | −.020 | .018 | −.038 | * | .017 | −.039 | * | .017 | −.041 | * | .018 | |
| Household size, ref. one person household | ||||||||||||
| Two person household | .000 | .027 | .020 | .027 | .037 | .027 | .031 | .026 | ||||
| Three or more person household | .042 | .028 | .016 | .026 | .021 | .028 | .010 | .027 | ||||
|
| ||||||||||||
| Constant | .500 | *** | .033 | .584 | *** | .050 | .687 | *** | .091 | .752 | *** | .095 |
|
| ||||||||||||
| Obs. | 8,231 | Obs. | 8,231 | Obs. | 8,231 | Obs. | 8,231 | |||||
p < .05
p < .01
p < .001
Figure 4.
Predicted cardiometabolic risk for owners and renters
The question remains whether respondents’ finances and health resources and behaviors also help to explain the relationship between homeownership and CMR. In the third model, which includes financial measures, the coefficient for renting is further reduced to .042, and is no longer statistically significant. Those with above-median non-housing wealth have lower CMR, and those with difficulty paying bills have higher CMR. Income is not related to CMR, likely due to collinearity with the other socioeconomic variables in the model. The relationships between CMR and education, race, home condition, and housing problems remain.
The fourth model adds health resources and behaviors. Respondents who have health insurance and those who engage in frequent physical activity have lower CMR levels. Smoking does not have a measurable relationship with CMR. In this fully-specified model, the other coefficients remain relatively stable in magnitude and statistical significance. Renters do not have higher CMR levels than homeowners when socioeconomic, housing, financial, and health resources and behavior are accounted for. Those with poor or very poor home conditions have higher CMR scores (coefficient: .132, p < .001) as do those facing current and ongoing housing problems (coefficient: .072, p < .05) and difficulty paying bills (coefficient: .049, p < .05). These results suggest that together, compositional differences and disparities in housing conditions and finances explain renters’ health disadvantage.
Analysis: Individual cardiometabolic risk measures
Next we examine which specific aspects of CMR are related to homeownership and housing conditions. As shown in Figure 5, a larger share of renters have high risk C-reactive protein (difference: 9.3%, p < .001), systolic blood pressure (difference: 5.2%, p < .01), diastolic blood pressure (difference: 4.9%, p < .01), glycosylated hemoglobin (difference = 5.7%, p < .001), and waist circumference (difference = 5.7%, p < .01). There is no clear difference between owners’ and renters’ risk levels for heart rate, total cholesterol, and high density lipoprotein cholesterol. Our sample size may not be large enough to detect a difference in risk levels for heart rate, since such a small share of respondents are high risk on this measure. And differences in cholesterol levels have become less pronounced due to widespread statin medication use (Salami et al., 2017).
Figure 5.
Weighted proportions high risk status on cardiometabolic biomarkers by housing tenure
Health and Retirement Study 2010/2012 analytic sample (n = 8,231).
Note: CRP, C-reactive protein; SYS, systolic blood pressure; DIA, diastolic blood pressure; HR, heart rate; HbA1c, hemoglobin A1c; HDL, high density lipoprotein cholesterol; TC, total cholesterol; Waist, waist circumference.
Note: Stars indicate statistical significance of t-tests comparing owners' risk and renters' risk, * p < .05, ** p < .01, *** p < .001.
To test whether these relationships hold up when accounting for selection and housing conditions, we use logistic regression to estimate the relative odds of being at risk for each of the CMR biomarkers. Table 4 displays the results. Renters are not at higher risk on any of the CMR measures when taking selection factors, housing conditions, finances, and health resources and behavior into account.
Table 4.
Estimated odds ratios from logistic regressions for cardiometabolic risks by housing tenure, housing conditions, and difficulty paying bills
| DVs: High risk status for each CMR measure |
CRP | SYS | DIA | HR | Hb-A1C | HDL | TC | Waist | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | OR | OR | OR | OR | OR | OR | OR | |||||||||
| SE | SE | SE | SE | SE | SE | SE | SE | |||||||||
|
| ||||||||||||||||
| Rent home | 1.047 | 1.109 | 1.072 | 1.004 | 1.145 | .956 | 1.157 | 1.013 | ||||||||
| .096 | .105 | .121 | .182 | .118 | .133 | .123 | .099 | |||||||||
| Home condition poor or very poor |
1.223 | 1.348 | * | 1.590 | *** | .897 | 1.338 | ** | 1.278 | * | .966 | 1.080 | ||||
| .147 | .153 | .156 | .242 | .140 | .145 | .150 | .115 | |||||||||
| Current and ongoing housing problem |
1.154 | 1.182 | 1.223 | 1.395 | * | 1.109 | .984 | 1.050 | 1.102 | |||||||
| .099 | .133 | .158 | .229 | .151 | .103 | .107 | .110 | |||||||||
| Difficulty paying bills |
1.093 | .989 | .988 | 1.165 | 1.213 | * | 1.102 | 1.022 | 1.166 | * | ||||||
| .068 | .080 | .101 | .162 | .099 | .107 | .099 | .084 | |||||||||
Note:All models adjusted for age, gender, marital status, education, income, wealth, race/ethnicity, health insurance, smoking, and physical activity.
Note:CRP, C-reactive protein; SYS, systolic blood pressure; DIA, diastolic blood pressure; HR, heart rate; HbA1c, hemoglobin A1c; HDL, high density lipoprotein cholesterol; TC, total cholesterol; Waist, waist circumference. n = 8,231
p < .05
p < .01
p < .001
People living in homes in poor or very poor condition are at higher risk on systolic and diastolic blood pressure measures (SYS OR: 1.348, p < .05; DIA OR: 1.590, p < .001), glycosylated hemoglobin, a measure of blood sugar control (OR: 1.338, p < .01), and high-density lipoprotein cholesterol (OR: 1.278, p < .05). People facing current and ongoing housing problems are at higher risk on heart rate (OR:1.395, p < .05), as well as positive odds ratios for C-reactive protein, blood pressure, glycosylated hemoglobin, and waist circumference, though none of these others are statistically significant. People with difficulty paying bills are at higher risk on glycosylated hemoglobin (OR: 1.213, p < .05) and waist circumference (OR: 1.166, p < .05), both related to metabolic function.
Discussion
Our results reveal that while renters have higher levels of CMR than owners, the difference dissipates when socioeconomic characteristics, disparities in housing conditions, and finances are taken into account. Further, we find that people facing poor home conditions, housing problems, and financial strain have higher levels of CMR, even when accounting for socioeconomic advantage. Home conditions, housing problems, and financial strain are linked with certain individual CMR biomarkers for cardiovascular health and metabolic function. Rather than a single explanation, compositional differences, housing conditions, and finances together appear to explain the health disparities between homeowners and renters.
This study advances our understanding of the role of housing as a social determinant of health. Our findings add to mounting evidence that the housing conditions and financial challenges renters often face can have serious consequences, which become especially stark at older ages. The link between housing problems and health may help explain prior findings that a sense of control partly mediates the relationship between homeownership and physical and mental health (Lindblad & Quercia, 2015). While housing scholars usually interpret perceived control as a purely psychosocial aspect related to housing tenure, perceptions of control may reflect real differences in renters’ and homeowners’ ability to avoid and resolve housing-related problems—which can have practical implications for day-to-day quality of life and finances, and potentially health.
This study has limitations. In a cross-sectional, observational analysis, we cannot fully observe the factors that contributed to selection into homeownership, which mostly occurred decades earlier. Educational attainment is one measure from earlier in life, but income and wealth are current measures of financial status. This limits our ability to make causal inferences about homeownership. Another limitation is that home condition, housing problem, and financial strain measures in the HRS lack specificity, and so it is hard to know the exact mechanisms by which they may impact health. There may be other neighborhood factors that play a role in CMR and differ by homeownership that we were not able to examine in this study. As additional waves of biomarker data are released, this work could be extended by using longitudinal analysis to examine whether CMR changes with housing and financial situations.
This paper makes several key contributions. To our knowledge, this is the first large-scale study to address the connection between homeownership, housing conditions, and health among middle aged and older adults in the US context. The use of biomarkers to measure CMR gives us an especially sensitive and reliable measure of health status. This paper is a step toward understanding the concrete mechanisms through which socioeconomic advantage can translate to better health outcomes. Overall, the findings reinforce the idea that homeownership in itself may not lead to better health outcomes, but rather the adverse housing conditions that often go hand in hand with renting may damage health. Looking more closely at the underlying reasons for the homeowner health advantage, it becomes clearer that some older homeowners may be vulnerable to housing-related health problems, along with many older renters.
Nonetheless, our findings underscore the steep personal and societal costs of inequality in access to homeownership. On the whole, homeowners enjoy far better housing conditions than renters. Many long-term renters are exposed to potentially harmful housing conditions over the course of their lives. Along with the longstanding racial disparities in mortgage lending and financial resources, younger generations currently face multiple economic roadblocks to homebuying (Choi et al., 2018), which could contribute to widening health disparities as they age.
This research is relevant to current debates around government support for homeownership, and can inform policy decisions about landlord-tenant laws. Our findings should encourage policymakers to consider housing as a crucial component in policy proposals to increase the well-being of middle aged and older adults. Our findings also bolster calls to provide housing subsidies in order to reduce financial strain – especially for the growing population of older renters. Still, it is important to note that addressing housing affordability is not enough on its own; housing quality and maintenance must be considered as well. The good news is that our findings suggest that code enforcement and other programs to ensure housing quality and maintenance can have a positive impact on adult well-being and health.
Acknowledgments
Funding details: Support for this analysis was provided by the National Institute on Aging (P30 AG17265).
Biography
Sarah Mawhorter, PhD, MPL, is a Postdoctoral Research Associate at the University of Southern California Leonard Davis School of Gerontology in the USC/UCLA Center on Biodemography and Population Health. She studies how younger and older adults navigate expensive housing markets, and the consequences for their health and wellbeing. She combines methods from demography, sociology, economics, and geography to examine the demographic processes and planning practices which shape urban housing opportunities.
Eileen M. Crimmins, PhD, is a University Professor and the AARP Chair in Gerontology at the USC Leonard Davis School of Gerontology. She is a member of the National Academy of Sciences, the National Academy of Medicine, and a fellow of the American Association for the Advancement of Science. She is the co-director of the USC/UCLA Center on Biodemography and Population Health, a Demography of Aging Center supported by the U.S. National Institute on Aging. She is also the co-director of the Multidisciplinary Training in Gerontology Program and the NIA-sponsored Network on Biological Risk. Crimmins is a co-investigator of the Health and Retirement Study. Much of Crimmins’ research has focused on changes over time in health and mortality. Crimmins has been instrumental in organizing and promoting the recent integration of the measurement of biological indicators in large population surveys. She has served as co-chair of a Committee for the National Academy of Sciences to address why life expectancy in the U.S. is falling so far behind that of other countries. She has recently co-edited several books with a focus on international aging, mortality and health expectancy. She has received the Kleemeier Award for Research from the Gerontological Society of America.
Jennifer A. Ailshire, PhD, is an Associate Professor of Gerontology and Sociology and Assistant Dean of International Programs and Global Initiatives at the USC Leonard Davis School of Gerontology. Her research addresses questions that lie at the intersections of social stratification, urban sociology, and the sociology of health and aging. In particular, her research focuses on the importance of the neighborhood environment and social relationships in determining health over the life course. A consistent theme throughout her work is an interest in gender, socioeconomic, racial, and ethnic inequality in health. Current projects include research on the links between air pollution and health in older adults, neighborhood determinants of racial and ethnic health disparities, and social factors associated with poor sleep.
References
- Aaronson D. (2000). A Note on the Benefits of Homeownership. Journal of Urban Economics, 47(3), 356–369. 10.1006/juec.1999.2144 [DOI] [Google Scholar]
- Acolin A. (2020). Owning vs. Renting: The benefits of residential stability? Housing Studies, 0(0), 1–24. 10.1080/02673037.2020.1823332 [DOI] [Google Scholar]
- Aldabe B, Anderson R, Lyly-Yrjänäinen M, Parent-Thirion A, Vermeylen G, Kelleher CC, & Niedhammer I. (2011). Contribution of material, occupational, and psychosocial factors in the explanation of social inequalities in health in 28 countries in Europe. Journal of Epidemiology and Community Health (1979-), 65(12), 1123–1131. JSTOR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annesi-Maesano I, Moreau D, & Moreau D. (2009). Potential sources of indoor air pollution and asthma and allergic diseases. In Housing and Health in Europe (pp. 131–144). Routledge. 10.4324/9780203885239-16 [DOI] [Google Scholar]
- Baker E, Bentley R, & Mason K. (2013). The Mental Health Effects of Housing Tenure: Causal or Compositional? Urban Studies, 50(2), 426–442. 10.1177/0042098012446992 [DOI] [Google Scholar]
- Barker D, & Miller E. (2009). Homeownership and Child Welfare. Real Estate Economics, 37(2), 279–303. 10.1111/j.1540-6229.2009.00243.x [DOI] [Google Scholar]
- Bell CN, Sacks TK, Thomas Tobin CS, & Thorpe RJ (2020). Racial Non-equivalence of Socioeconomic Status and Self-rated Health among African Americans and Whites. SSM - Population Health, 10, 100561. 10.1016/j.ssmph.2020.100561 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bentley RJ, Pevalin D, Baker E, Mason K, Reeves A, & Beer A. (2016). Housing affordability, tenure and mental health in Australia and the United Kingdom: A comparative panel analysis. Housing Studies, 31(2), 208–222. 10.1080/02673037.2015.1070796 [DOI] [Google Scholar]
- Boen C, Keister L, & Aronson B. (2020). Beyond Net Worth: Racial Differences in Wealth Portfolios and Black–White Health Inequality across the Life Course. Journal of Health and Social Behavior, 61(2), 153–169. 10.1177/0022146520924811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonnefoy X, Braubach M, Krapavickaite D, Ormandy D, & Zurlyte I. (2003). Housing conditions and self-reported health status: A study in panel block buildings in three cities of Eastern Europe. Journal of Housing and the Built Environment, 18(4), 329–352. [Google Scholar]
- Choi J, Zhu J, Goodman L, Ganesh B, & Strochak S. (2018). Millennial Homeownership: Why Is It So Low, and How Can We Increase It? Urban Institute. [Google Scholar]
- Coventry PA, Gemmell I, & Todd CJ (2011). Psychosocial risk factors for hospital readmission in COPD patients on early discharge services: A cohort study. BMC Pulmonary Medicine; London, 11, 49. 10.1186/1471-2466-11-49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins EM, Faul J, Kim JK, & Weir D. (2015). Documentation of Biomarkers in the 2010 and 2012 Health and Retirement Study (pp. 1–15) [HRS Documentation Report]. University of Michigan Survey Research Center. https://hrs.isr.umich.edu/sites/default/files/biblio/Biomarker2010and2012.pdf [Google Scholar]
- Crimmins EM, Kim JK, & Vasunilashorn S. (2010). Biodemography: New approaches to understanding trendsand differences in population health and mortality. Demography, 47(1), S41–S64. 10.1353/dem.2010.0005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croxford B. (2009). The effect of cold homes on health: Evidence from the LARES study. In Housing and Health in Europe (pp. 142–154). Routledge. 10.4324/9780203885239-18 [DOI] [Google Scholar]
- Ellaway A, Macdonald L, & Kearns A. (2016). Are housing tenure and car access still associated with health? A repeat cross-sectional study of UK adults over a 13-year period. BMJ Open, 6(11), e012268. 10.1136/bmjopen-2016-012268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellaway A, & Macintyre S. (1998). Does housing tenure predict health in the UK because it exposes people to different levels of housing related hazards in the home or its surroundings? Health & Place, 4(2), 141–150. 10.1016/S1353-8292(98)00006-9 [DOI] [PubMed] [Google Scholar]
- Fenelon A, & Mawhorter S. (2020). Housing Affordability and Security Issues Facing Older Adults in the United States. Public Policy & Aging Report. 10.1093/ppar/praa038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenelon A, Mayne P, Simon AE, Rossen LM, Helms V, Lloyd P, Sperling J, & Steffen BL (2017). Housing Assistance Programs and Adult Health in the United States. American Journal of Public Health, 107(4), 571–578. 10.2105/AJPH.2016.303649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galster GC, Marcotte DE, Mandell MB, Wolman H, & Augustine N. (2007). The impact of parental homeownership on children’s outcomes during early adulthood. Housing Policy Debate, 18(4), 785–827. 10.1080/10511482.2007.9521621 [DOI] [Google Scholar]
- Ganesh B, Scally CP, Skopec L, & Zhu J. (2018). The Relationship between Housing and Asthma among School-Age Children (p. 29). Urban Institute. https://www.urban.org/sites/default/files/publication/93881/the-relationshi-between-housing-and-asthma_1.pdf [Google Scholar]
- García-Esquinas E, Pérez-Hernández B, Guallar-Castillón P, Banegas JR, Ayuso-Mateos JL, & Rodríguez-Artalejo F. (2016). Housing conditions and limitations in physical function among older adults. Journal of Epidemiology and Community Health (1979-), 70(10), 954–960. [DOI] [PubMed] [Google Scholar]
- Gibney S, Ward M, & Shannon S. (2018). Housing conditions and non-communicable diseases among older adults in Ireland. Quality in Ageing and Older Adults, 19(3), 191–204. 10.1108/QAOA-03-2018-0013 [DOI] [Google Scholar]
- Green RK, & White MJ (1997). Measuring the Benefits of Homeowning: Effects on Children. Journal of Urban Economics, 41(3), 441–461. 10.1006/juec.1996.2010 [DOI] [Google Scholar]
- Hall M, & Crowder K. (2011). Extended-family resources and racial inequality in the transition to homeownership. Social Science Research, 40(6), 1534–1546. 10.1016/j.ssresearch.2011.07.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson JV, & Ioannides YM (1983). A Model of Housing Tenure Choice. The American Economic Review, 73(1), 98–113. [Google Scholar]
- Hiyoshi A, Fukuda Y, Shipley MJ, & Brunner EJ (2014). Health inequalities in Japan: The role of material, psychosocial, social relational and behavioural factors. Social Science & Medicine, 104, 201–209. 10.1016/j.socscimed.2013.12.028 [DOI] [PubMed] [Google Scholar]
- Jackson CA, Jones M, & Mishra GD (2014). Educational and homeownership inequalities in stroke incidence: A population-based longitudinal study of mid-aged women. European Journal of Public Health, 24(2), 231–236. 10.1093/eurpub/ckt073 [DOI] [PubMed] [Google Scholar]
- Joint Center for Housing Studies. (2019). Housing America’s Older Adults. Harvard University. https://www.jchs.harvard.edu/housing-americas-older-adults-2019 [Google Scholar]
- Kavanagh AM, Aitken Z, Baker E, LaMontagne AD, Milner A, & Bentley R. (2016). Housing tenure and affordability and mental health following disability acquisition in adulthood. Social Science & Medicine, 151, 225–232. 10.1016/j.socscimed.2016.01.010 [DOI] [PubMed] [Google Scholar]
- Laaksonen M, Martikainen P, Nihtilä E, Rahkonen O, & Lahelma E. (2008). Home ownership and mortality: A register-based follow-up study of 300 000 Finns. Journal of Epidemiology and Community Health; London, 62(4), 293. 10.1136/jech.2007.061309 [DOI] [PubMed] [Google Scholar]
- Lee H, Myers D, Painter G, Thunell J, & Zissimopoulos J. (2020). The role of parental financial assistance in the transition to homeownership by young adults. Journal of Housing Economics, 47, 101597. 10.1016/j.jhe.2018.08.002 [DOI] [Google Scholar]
- Lindblad MR, & Quercia RG (2015). Why Is Homeownership Associated With Nonfinancial Benefits? A Path Analysis of Competing Mechanisms. Housing Policy Debate, 25(2), 263–288. 10.1080/10511482.2014.956776 [DOI] [Google Scholar]
- Macintyre S, Ellaway A, Der G, Ford G, & Hunt K. (1998). Do Housing Tenure and Car Access Predict Health Because They Are Simply Markers of Income or Self Esteem? A Scottish Study. Journal of Epidemiology and Community Health (1979-), 52(10), 657–664. JSTOR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mason KE, Baker E, Blakely T, & Bentley RJ (2013). Housing affordability and mental health: Does the relationship differ for renters and home purchasers? Social Science & Medicine, 94, 91–97. 10.1016/j.socscimed.2013.06.023 [DOI] [PubMed] [Google Scholar]
- Meltzer R, & Schwartz A. (2016). Housing Affordability and Health: Evidence From New York City. Housing Policy Debate, 26(1), 80–104. 10.1080/10511482.2015.1020321 [DOI] [Google Scholar]
- Mitchell UA, Ailshire JA, & Crimmins EM (2019). Change in Cardiometabolic Risk Among Blacks, Whites, and Hispanics: Findings From the Health and Retirement Study. The Journals of Gerontology: Series A, 74(2), 240–246. 10.1093/gerona/gly026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moor I, Spallek J, & Richter M. (2017). Explaining socioeconomic inequalities in self-rated health: A systematic review of the relative contribution of material, psychosocial and behavioural factors. Journal of Epidemiology and Community Health; London, 71(6), 565. 10.1136/jech-2016-207589 [DOI] [PubMed] [Google Scholar]
- Morris A. (2018). Housing tenure and the health of older Australians dependent on the age pension for their income. Housing Studies, 33(1), 77–95. 10.1080/02673037.2017.1344202 [DOI] [Google Scholar]
- Niemann H, Maschke C, & Maschke C. (2009). Noise effects and morbidity. In Housing and Health in Europe (pp. 275–294). Routledge. 10.4324/9780203885239-25 [DOI] [Google Scholar]
- Ormandy D. (2009). Housing and Health in Europe: The WHO LARES project. Routledge. 10.4324/9780203885239 [DOI] [Google Scholar]
- Ormandy D, & Ezratty V. (2012). Health and thermal comfort: From WHO guidance to housing strategies. Energy Policy, 49, 116–121. 10.1016/j.enpol.2011.09.003 [DOI] [Google Scholar]
- Park G-R, & Seo BK (2020). Revisiting the relationship among housing tenure, affordability and mental health: Do dwelling conditions matter? Health & Social Care in the Community, 28(6), 2225–2232. 10.1111/hsc.13035 [DOI] [PubMed] [Google Scholar]
- Pfeiffer D. (2018). Rental Housing Assistance and Health: Evidence From the Survey of Income and Program Participation. Housing Policy Debate, 28(4), 515–533. 10.1080/10511482.2017.1404480 [DOI] [Google Scholar]
- Pollack CE, Griffin BA, & Lynch J. (2010). Housing Affordability and Health Among Homeowners and Renters. American Journal of Preventive Medicine, 39(6), 515–521. 10.1016/j.amepre.2010.08.002 [DOI] [PubMed] [Google Scholar]
- Quillian L, Lee JJ, & Honoré B. (2020). Racial Discrimination in the U.S. Housing and Mortgage Lending Markets: A Quantitative Review of Trends, 1976–2016. Race and Social Problems, 12(1), 13–28. 10.1007/s12552-019-09276-x [DOI] [Google Scholar]
- Robertson T, Benzeval M, Whitley E, & Popham F. (2015). The role of material, psychosocial and behavioral factors in mediating the association between socioeconomic position and allostatic load (measured by cardiovascular, metabolic and inflammatory markers). Brain, Behavior, and Immunity, 45, 41–49. 10.1016/j.bbi.2014.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohe WM, & Basolo V. (1997). Long-Term Effects of Homeownership on the Self-Perceptions and Social Interaction of Low-Income Persons. Environment and Behavior, 29(6), 793–819. 10.1177/0013916597296004 [DOI] [Google Scholar]
- Rohe WM, & Stegman MA (1994). The Effects of Homeownership: On the Self-Esteem, Perceived Control and Life Satisfaction of Low-Income People. Journal of the American Planning Association, 60(2), 173–184. 10.1080/01944369408975571 [DOI] [Google Scholar]
- Rudnai P, Varro MJ, Malnasi T, Páldy A, & O’Dell SN and A. (2009). Damp, mould and health. In Housing and Health in Europe (pp. 125–141). Routledge. 10.4324/9780203885239-17 [DOI] [Google Scholar]
- Salami JA, Warraich H, Valero-Elizondo J, Spatz ES, Desai NR, Rana JS, Virani SS, Blankstein R, Khera A, Blaha MJ, Blumenthal RS, Lloyd-Jones D, & Nasir K. (2017). National Trends in Statin Use and Expenditures in the US Adult Population From 2002 to 2013: Insights From the Medical Expenditure Panel Survey. JAMA Cardiology, 2(1), 56. 10.1001/jamacardio.2016.4700 [DOI] [PubMed] [Google Scholar]
- Schwartz KL, Crossley-May H, Vigneau FD, Brown K, & Banerjee M. (2003). Race, socioeconomic status and stage at diagnosis for five common malignancies. Cancer Causes & Control, 14(8), 761–766. 10.1023/A:1026321923883 [DOI] [PubMed] [Google Scholar]
- Seeman TE, Crimmins EM, Huang M-H, Singer B, Bucur A, Gruenewald T, Berkman LF, & Reuben DB (2004). Cumulative biological risk and socio-economic differences in mortality: MacArthur Studies of Successful Aging. Social Science & Medicine, 58(10), 1985–1997. 10.1016/S0277-9536(03)00402-7 [DOI] [PubMed] [Google Scholar]
- Sharpe KH, McMahon AD, Raab GM, Brewster DH, & Conway DI (2014). Association between Socioeconomic Factors and Cancer Risk: A Population Cohort Study in Scotland (1991–2006). PLOS ONE, 9(2), e89513. 10.1371/journal.pone.0089513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spader J. (2019). Tenure Projections of Homeowner and Renter Households for 2018–2038 (p. 27) [Text]. Joint Center for Housing Studies, Harvard University. https://www.jchs.harvard.edu/research-areas/working-papers/tenure-projections-homeowner-and-renter-households-2018-2038-0 [Google Scholar]
- Szabo A, Allen J, Alpass F, & Stephens C. (2018). Longitudinal Trajectories of Quality of Life and Depression by Housing Tenure Status. The Journals of Gerontology: Series B, 73(8), e165–e174. 10.1093/geronb/gbx028 [DOI] [PubMed] [Google Scholar]
- Webb E, Blane D, & de Vries R. (2013). Housing and respiratory health at older ages. Journal of Epidemiology and Community Health, 67(3), 280. 10.1136/jech-2012-201458 [DOI] [PubMed] [Google Scholar]
- Wilkinson P, Armstrong B, Landon M, Stevenson S, Pattenden S, McKee M, & Fletcher T. (2001). Cold comfort: The social and environmental determinants of excess winter deaths in England, 1986–1996 (The Policy Press and the Joseph Rowntree Foundation). London School of Hygiene and Tropical Medicine. https://www.jrf.org.uk/report/cold-comfort-social-and-environmental-determinants-excess-winter-deaths-england-1986-1996 [Google Scholar]
- Willson AE, Shuey KM, & Elder Jr., Glen H. (2007). Cumulative Advantage Processes as Mechanisms of Inequality in Life Course Health. American Journal of Sociology, 112(6), 1886–1924. JSTOR. 10.1086/512712 [DOI] [Google Scholar]
- Woodward M, Oliphant J, Lowe G, & Tunstall-Pedoe H. (2003). Contribution of contemporaneous risk factors to social inequality in coronary heart disease and all causes mortality. Preventive Medicine, 36(5), 561–568. 10.1016/S0091-7435(03)00010-0 [DOI] [PubMed] [Google Scholar]
- Zajacova A, & Dowd JB (2011). Reliability of Self-rated Health in US Adults. American Journal of Epidemiology, 174(8), 977–983. 10.1093/aje/kwr204 [DOI] [PMC free article] [PubMed] [Google Scholar]