Abstract
Background:
Abdominoplasty techniques are well documented. The ideal position of the umbilicus has, however, received limited attention. Unfortunately, umbilicus position is not universally agreed upon in male cosmetic abdominoplasty. This study was conducted to determine the ideal umbilicus anthropometric measurements in young men, and the relationships between umbilical position and anterior trunk and torso reference points that may be applicable to intraoperative positioning. It is aimed also at investigating whether umbilicus position would be more accurately determined by considering nipple position instead of the abdominal crease, as recently proposed.
Methods:
Several anthropometric measurements of various anterior abdominal and thoracic landmarks were conducted on 60 young and middle-aged male volunteers and 30 cadavers at São Paulo city. All statistical analysis was completed using Stata software.
Results:
Of all the measured reference points, a much stronger correlation (0.513) was demonstrated between umbilicus-anterior axillary fold (U-AX) and inter-nipple (N-N) distances with a constant golden number ratio relationship (N-N = U-AX × 0.618) compared with the weak correlation of 0.034 between umbilicus-xiphisternum and umbilicus-abdominal crease. In 75% of volunteers, the calculated U-AX was within ±3 cm of actual measurement, and in 33.33% within ±1 cm.
Conclusions:
U-AX = 1.618 × N-N equation is more predictive of adequate umbilicus repositioning during abdominoplasty in male patients. Chest and abdomen of men are a single aesthetic unit. Proper positioning of the nipples and umbilicus, as well as harmonious abdominal and torso proportions are critical for an optimal final aesthetic outcome.
Takeaways
Question: What is the ideal anthropometric measure- ments of the umbilicus position during abdominoplasty in male patients?
Findings: The U-AX = 1.618 × N-N equation is more predictive of adequate umbilicus repositioning during abdomino- plasty in male patients.
Meaning: Proper positioning of the nipples and umbilicus, as well as harmonious abdominal and torso proportions, are critical for an optimal final aesthetic outcome.
INTRODUCTION
The umbilicus is a superficial scar and an essential aesthetic feature of abdominal appearance.1–4 Anecdotally, the painting Adam and Eve by Jean-Baptiste Santerre (1651–1717) lacking an umbilicus caused a scandal, which later led to the addition of an umbilicus to the painting.5 If absent or not well-positioned, it can result in an unnatural looking abdomen.2,4,6–9
Despite that its physiological and aesthetic importance have long been recognized, the umbilicus was routinely discarded during surgery until the late 1950s.10,11 With increasing appreciation of its importance in defining a harmonious anterior trunk, umbilical transposition performed toward the end of the surgery was described by Vernon in 1957.12 However, despite abundant literature on abdominoplasty, limited attention has been directed toward the ideal umbilicus position.3,13,14
Obviously, when judging an abdomen for its attractiveness, umbilicus position and shape cannot be ignored.6,15 Achieving a desirable result is obtained only by avoiding an undesirable high- or low-riding navel.16 Numerous techniques have been described for the restoration of the umbilicus in its new position15; there is, however, no universal consensus and standardization regarding ideal position and shape.17,18 Although some guidelines do exist, position remains dependent on individual surgeons’ artistic sensibility and subjective assessment of beauty.17
Increasing demand among young men for enhanced aesthetics of abdominal contour has been noted lately. With the increasing popularity of bariatric surgery, it is projected that the proportion of men seeking abdominoplasties will steadily increase.19 It is questionable, however, whether concepts of umbilical position and abdominal aesthetics that have been mostly determined by two-dimensional photographs of top female models, most probably edited, apply to the general population and, particularly, to male patients.13
Strongly believing that the anterior male trunk aesthetic unit encompasses both the abdomen and thorax and that the nipples and umbilicus, being the main visual aesthetic landmarks, should be in a harmonious relationship, we hypothesize that a fixed relationship between the umbilicus and nipple positions with some anterior trunk and torso reference points does exist. This relationship could be favorably applicable in male abdominoplasty for correct intraoperative umbilical positioning as well as for preoperative planning, particularly when the original umbilical location has been altered by weight change or previous surgery.
Describing the horizontal and vertical coordinates of nipple position in male patients, the senior author has previously reported a golden number correlation between N-N (inter-nipple) and U-AX (umbilicus-anterior axillary fold) distances (N-N = U-AX × 0.618),20–22 applicable also for determination of umbilicus position. In line with a study published by Visconti et al17 on female models, Graham et al23 proposed another formula after analysis of 81 online photographs of top male models to determine umbilicus position based on a golden number correlation between U-XI (umbilicus-xiphisternum) and U-ACr (umbilicus-abdominal crease) distances (U-XI = U-ACr × 1.618). We believe, however, that nipples are more obvious landmarks and easier to define than the abdominal crease and that inter-nipple distance is more appropriate for accurate determination of umbilical position in male abdominoplasty.
MATERIALS AND METHODS
Several anthropometric measurements of anterior abdominal and thoracic landmarks (Fig. 1) were conducted on two study groups. The first group consisted of 60 male volunteers without any history of previous abdominal or breast surgery, or massive weight loss. Subjects with skeletal thoracic or spinal deformity were excluded the same as men with grades III and IV gynecomastia. Measurements were made in the standing position. In case of discrepancy in measurement of paired landmarks, the mean was recorded. The study was conducted in accordance with the Declaration of Helsinki principles. Institutional review board approval was not required due to its noninterventional nature. Permission to use measurements for study purposes was obtained from all participants.
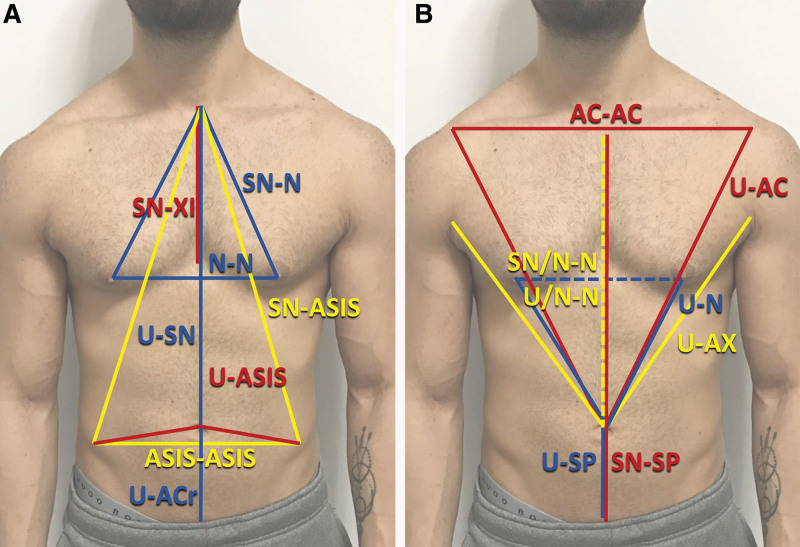
Fig. 1.
The 16 anthropometric measurements were made on standing male volunteers. A, SN-N: sternal notch-nipple distance; SN-XI: sternal notch-xiphoid distance; SN-ASIS: sternal notch-anterior superior iliac spine; U-SN: umbilicus-sternal notch distance; U-ASIS: anterior superior iliac spine distance; ASIS-ASIS: interanterior superior iliac spine. B, AC-AC: inter-acromion distance; U-AC: umbilicus acromion distance; U-N: umbilicus nipple distance; U-SP: umbilicus symphysis pubis; SN-SP: sternal notch symphysis pubis distance; SN/N-N: sternal notch to inter-nipple line; U/N-N: umbilicus to internipple line.
With the approval of the authority at the public morgue of São Paulo, associated with São Paulo University, similar measurements in the supine position were made on a second group of 30 male cadavers of mixed ethnicity, which were by law under the city’s jurisdiction before mandatory burial within 24 hours.
For both study groups, calculations and correlations were conducted. Appropriateness of the two equations under question were evaluated with statistical regressions. P values less than 0.01 determined statistical significance for multivariate analysis. A multiple linear regression model was also applied. Adjusted R-squared values of 0.13 or less indicated poor; 0.13–0.26, moderate; and 0.26 or more, high goodness of fit. All statistical analysis was completed using Stata software (StataCorp. 2021. Stata Statistical Software: Release 17. College Station, Tex.: StataCorp LLC).
RESULTS
The mean age of volunteers was 27.8 years, mean height, 1.79 m; mean weight, 78.9 kg; and mean body mass index (BMI), 24.75 kg per m2 (Table 1). The 95% confidence interval (CI) of the U-AX distance, determined by U-AX = 1.618 × N-N, and U-XI distance, determined by U-XI = U-ACr × 1.618, were calculated and were 1.032 ± 0.02, and 0.995 ± 0.04, respectively. Variance was found to be greater for U-XI/U-ACr compared with U-AX/N-N (0.023 versus 0.007), indicating that the equation described by Graham et al23 is less accurate. Correlation analysis to the golden mean relating the two equations was performed. Stronger correlation was demonstrated with U-AX/N-N (0.513) when compared with U-XI/U-ACr (0.034), indicating that the U-AX/N-N equation is more closely related to the golden mean. In 75% of volunteers, calculated U-AX was within ±3 cm of actual measurement, and in 33.33% within ±1 cm.
Table 1.
Descriptive Statistics of 60 Male Volunteers and 30 Cadavers
| Variable | Obs | Mean | SD | Min | Max |
|---|---|---|---|---|---|
| Male volunteers | |||||
| BMI | 60 | 24.69833 | 2.729096 | 21 | 31 |
| HT | 60 | 1.788 | 0.066079 | 1.6 | 1.91 |
| Age | 60 | 27.75 | 6.902775 | 19 | 49 |
| Cadavers | |||||
| BMI | 30 | 25.09006 | 3.622323 | 19.47715 | 33.95062 |
| HT | 30 | 1.698667 | 0.0671967 | 1.6 | 1.8 |
| Age | 30 | 70.86667 | 13.77838 | 19 | 95 |
R2 was determined to evaluate appropriateness of data fit of both equations. For U-AX/N-N, adjusted R2 was 0.251 with F(1, 58) = 20.8 and P = 0.000. It was significantly higher than for U-XI/U-ACr (adjusted R2 = 0.001, F(1, 58) = 0.07, P = 0.798) (Tables 2 and 3). Adjusted R2 for U-AX/N-N increases significantly (Table 4) when BMI is considered (adjusted R2 = 0.4319, F(2, 57) = 23.43, P = 0.000). Grouping data by BMI categories, 38 subjects were normal weight; 19, overweight; and three, obese. Regression analysis conducted with overweight and obese categories as dummy variables revealed a slight increase in adjusted R2, suggesting some small nonlinear effect (adjusted R2 = 0.457, F(3,56) = 17.59). Obesity had a larger effect than overweight (correlation coefficient 2.99 and 1.73, respectively). Regardless, this effect did not lead to a large difference, as the original regression showed BMI to positively correlate (Table 4). Regression within two BMI groups (normal weight and overweight) showed a nonsignificant change in U-AX. Though the correlation coefficient was greater for overweight (0.415 versus 0.210), the difference was not significant, as the CIs overlapped. Moreover, there was no correlation between N-N and BMI (0.034) in obese and overweight subjects, while a relatively small correlation (0.350) existed in normal weight subjects. Apparently, higher BMI has no effect on N-N distance and, subsequently, on calculations of umbilicus position (Fig. 2). Even though patient BMI does significantly impact the accuracy of the U-AX/N-N equation, it remains applicable to patients over a wide BMI range (Fig. 3).
Table 2.
U-AX = N-N × 1.618 Equation Regression
| Source | SS | df | MS | No. Obs = 60 F (1, 58) = 20.80 Prob > F = 0.0000* R-squared† = 0.2639 Adj R-squared‡ = 0.2512 Root MSE = 1.6972 |
||
|---|---|---|---|---|---|---|
| Model Residual |
59.9083547 167.074979 |
1 58 |
2.729096 0.066079 |
|||
| Total | 226.983333 | 59 | 6.902775 | |||
| N-N | Coefficient | SE | t | P > I t I | 95% CI | |
| U-AX | 0.3047996 | 0.0668363 | 40.56 | 00.000 | 0.1710122 | 0.435869 |
| _cons | 11.65899 | 2.64578 | 4.41 | 0.000 | 6.362886 | 16.9551 |
The data fit is highly significant (P = 0.0000).
Prob > F is the probability of obtaining the estimated F-statistics or greater (the P value).
R-squared is a statistical measure that indicates how much of the variation of a dependent variable is explained by an independent variable in a regression model.
Adjusted R-squared shows whether adding additional predictors improves a regression model or not.
Table 3.
U-XI = U-ACr × 1.618 Equation Regression
| Source | SS | df | MS | No. Obs = 60 F (1, 58) = 0.07 Prob > F = 0.7978 R-squared = 0.0011 Adj R-squared = –0.0161 Root MSE = 1.6547 |
||
|---|---|---|---|---|---|---|
| Model Residual | 0.181430775 158.801903 | 1 58 | 0.181430775 2.73796384 |
|||
| Total | 158.983333 | 59 | 2.69463277 | |||
| N-N | Coefficient | SE | t | P > I t I | 95% CI | |
| U-ACr | 0.0374084 | 0.1453207 | 0.26 | 0.798 | –0.2534827 | 0.3282995 |
| _cons | 17.26623 | 1.634347 | 10.56 | 0.000 | 13.99473 | 20.53773 |
The data fit is not significant (P = 0.7978).
Table 4.
U-AX = N-N x 1.618 Equation Regression Incorporating BMI, Overweight, and Obese Categories
| Source | SS | df | MS | No. obs = 60 F (1, 58) = 23.43 Prob > F = 0.000 R-squared = 0.4512 Adj R-squared = 0.4319 Root MSE = 1.4783 |
||
|---|---|---|---|---|---|---|
| Model Residual |
102.410546 124.572787 |
2 57 |
51.205273 2.1854875 |
|||
| Total | 226.982787 | 59 | 3.84717514 | |||
| N-N | Coefficient | SE | t | P > I t I | 95% CI | |
| U-AX | 0.2271854 | 0.0608186 | 3.74 | 0.000 | 0.1053983 | 0.3489724 |
| BMI | 0.3249018 | 0.0736751 | 4.41 | 0.000 | 0.17737 | 0.4724337 |
| _cons | 6.696336 | 2.564632 | 2.61 | 0.012 | 1.560749 | 11.83192 |
| Source | SS | df | MS | No. obs = 60 F (3, 56) = 17.59 Prob > F = 0.000 R-squared = 0.4852 Adj R-squared = 0.4576 Root MSE = 1.4446 |
||
| Model Residual |
110.124887 116.858446 |
3 56 |
36.7082957 2.08675797 |
|||
| Total | 226.983333 | 59 | 3.84717514 | |||
| N-N | Coefficient | SE | t | P > I t I | 95% CI | |
| U-AX | 0.2241769 | 0.0605102 | 3.70 | 0.000 | 0.1029604 | 0.3453935 |
| Over_weight | 1.726373 | 0.4092742 | 4.22 | 0.000 | 0.9064979 | 2.546247 |
| Obese | 2.992996 | 0.9192123 | 3.26 | 0.002 | 1.151593 | 4.8344 |
| _cons | 14.14322 | 2.366751 | 5.98 | 0.000 | 9.402046 | 18.88439 |
U-AX = N-N x 1.618 equation regression with BMI incorporated results in a net increase in R-squared, indicating how much of the variation in U-Ax is explained by BMI. Regression analysis with overweight and obese categories as dummy variables revealed a slight increase in adjusted R2 value, suggesting some small nonlinear effect.
Fig. 2.
Plot diagram of BMI and N-N of the volunteers in the study group (n = 60: normal, n = 38; overweight, n = 19; obese, n = 3). Higher BMI is not associated with a wider N-N distance.
Fig. 3.
Plot diagram of BMI, U-AX, and calculated U-AX of all the volunteers in the study group.
Adding height to the regression did not result in significant increase in R2 (adjusted R2 = 0,253, F(1,58) = 11.02) (Table 5). Conducting the regression with age as a variable without distinct grouping demonstrated that age did not have a significant effect on U-AX (adjusted R2 = 0.2381, F(2,57) = 10.22) (Table 6). With subjects grouped by age (≤30 years and >30 years), adjusted R2 was 0.374 and F(1,39) = 23.34 for the younger age group, whereas for subjects older than 30 years, adjusted R2 was 0.0656 and F(1,17) = 2.27 (Fig. 4).
Table 5.
U-AX = N-N × 1.618 Equation Regression with Height Incorporated Did Not Yield Any Increase in R-squared, Indicating That U-AX Is Independent of Height
| Source | SS | df | MS | No. Obs = 60 F (1, 58) = 11.02 Prob > F = 0.0001 R-squared = 0.2789 Adj R-squared = 0.2536 Root MSE = 1.6946 |
||
|---|---|---|---|---|---|---|
| Model Residual |
63.3037501 163.679583 |
2 57 |
31.6518751 2.87157164 |
|||
| Total | 226.983333 | 59 | 3.84717514 | |||
| N-N | Coefficient | SE | t | P > I t I | 95% CI | |
| U-AX | 0.3163596 | 0.0675729 | 4.68 | 0.000 | 0.1810471 | 0.451672 |
| ht | –3.647001 | 3.353903 | –1.09 | 0.281 | –10.36308 | 3.069074 |
| _cons | 17.72379 | 6.171341 | 2.87 | 0.006 | 5.365888 | 30.08168 |
Table 6.
U-AX = N-N × 1.618 Equation Regression with Age Incorporated Did Not Yield Any Increase in R-squared, Indicating That U-AX Is Independent of Age
| Source | SS | df | MS | No. Obs = 60 F (2, 57) = 10.22 Prob > F = 0.0002 R-squared = 0.2639 Adj R-squared = 0.2381 Root MSE = 1.712 |
||
|---|---|---|---|---|---|---|
| Model Residual |
59.909833 167.0735 |
2 57 |
29.9549165 2.93111404 |
|||
| Total | 226.983333 | 59 | 3.84717514 | |||
| NN | Coefficient | SE | t | P > I t I | 95% CI | |
| U-AX | 0.3045596 | 0.0682611 | 4.46 | 0.000 | 0.167869 | 0.4412502 |
| Age | 0.0007342 | 0.0326929 | 0.02 | 0.982 | –0.0647321 | 0.0662006 |
| _cons | 11.64808 | 2.7122715 | 4.29 | 0.000 | 6.215965 | 17.0802 |
Fig. 4.
Plot diagram of Age, U-AX, and calculated U-AX of all the volunteers in the study group.
Cadaver data descriptive statistics are shown in Table 1. Regression analysis of measurements did not demonstrate any significant correlation between umbilical position and N-N or U-ACr. Regression for the U-AX/N-N relationship showed R2 = 0.0406 and adjusted R2 = 0.0063 with a nonsignificant P value. Regression for U-XI/U-ACr resulted in R2 = 0.000 and adjusted R2 = -0.036 with a nonsignificant P value. When incorporating BMI, R2 of U-AX/N-N increased to 0.3617 with adjusted R2 = 0.3144; nevertheless, the P value was still not significant. Regression performed incorporating BMI for U-XI/U-ACr showed R2 = 0.029 and adjusted R2 = -0.043.
DISCUSSION
Though primarily determined by its deep anchoring,3 umbilicus cutaneous surface repositioning is a main step during abdominoplasty. Ideal position has been debated for decades, and general consensus is still lacking.6,10,17 Hoyos et al7,8 reported that three localization modalities are mostly favored: (1) at 60% of the distance between the pubis and xiphoid process, measured from distal to proximal24; (2) at the intersection between the midline and a line crossing both anterosuperior iliac spines25; and (3) at a point located 15 cm above the pubic bone.26
In many anatomical descriptions, the transumbilical plane is described at the level between the third and fourth lumbar vertebrae in the supine position regardless of gender.17,27 This, however, is of no practical value when performing surgery. Furthermore, with major reference points of abdominal surface topography being distorted or covered by surgical drapes, choosing the optimal site for naval repositioning is a real challenge.27–29
Downward umbilicus migration occurs with age together with “pooch” formation in men.6 Gravity also affects umbilicus level in standing position.30 Position also changes with scars, hernias, and pregnancy in women.15,30,31 Despite reports that BMI does not influence its location,26 a lower umbilicus is associated with increasing BMI.5,32 Position may also be influenced by ethnicity,17 as well as whether the patient is high waisted or low waisted.33 Although many reports indicate that height does not seem to have an impact, a tendency toward a higher umbilicus is reported in tall patients.26 Characterized as a midline structure, the umbilicus is also rarely in the midline17; asymmetries are common.3,30,34 Nevertheless, a recent computer-aided analysis of models’ photographs concluded that the location of the aesthetically pleasing umbilicus is absolutely midline.33
Umbilical stalk position is a constant reference point and a predetermined unique feature for each patient.1 It is generally recommended to place the umbilicus at the level of its pedicle base without any measurements.1,4,17,35–37 To aid in exact localization, a suture can be attached to the xiphoid for reference.38 Alternatively, use of a Lockwood marker,28 spherical stainless-steel device,39 magnet,40 or even a shaped wire41 have been described. However, unless the umbilicus is inset within the fascia and sutured to the abdominal flap exactly in correspondence with its projection,37 an abnormal location may develop postoperatively when the umbilical stalk is long. It is worth noting that umbilicus relocation at the original stalk in all patients may not be optimal. Some patients with a high-riding umbilicus would benefit from lowering by 2–6 cm.42
Various authors have mentioned that the umbilicus is best located at the level of the waistline or at the top level of the iliac crest.6,18,27,43 Umbilicopubic distance has been described to be consistently at 15 cm in patients 145–178 cm tall.26 Others have recommended placing the umbilicus 3 cm cephalad to the anterior iliac spine level44 or 4 cm below the waistline12; however, it is specifically recommended that final umbilical position should remain above the anterior superior iliac spine.44 Furthermore, it is also advocated to locate the umbilicus between one half and two-thirds of the xiphoid-pubis distance.1,18,45 The 15/10 rule and flap flipping technique defining an “expected zone” for umbilical positioning has been suggested, as well as an easy-to-use, intuitive yet precise, and simple guide.15
Abhyankar et al46 demonstrated that a 1.6:1 ratio approximating the golden ratio exists between xiphisternum-umbilicus and umbilicus-symphysis pubis; the same ratio exists between umbilicus to anterior superior iliac spine and interanterior superior iliac spine. Different ratios of similar reference measurements were, however, reported in subjects of different ethnicities; African American people have a lower lying umbilicus compared with White people.23,24,47–49 To accurately predict umbilicus-xyphoid distance, complex mathematical equations have also been proposed.30,50,51 These, however, are too complicated to have any significant practical application.
Considering that bony landmarks are not reliable as reference points, Visconti et al17 suggested that a golden ratio does not exist between the umbilicus-xyphoid and the umbilicus-symphysis pubis; it exists instead with the U-ACr that defines the abdominal aesthetic unit’s lower limit in women. This ratio was recently confirmed by an eye tracking and survey-based investigation.13 A recent analysis of photographs of top male underwear models has suggested that the same ratio exists in male subjects as well.23
Unfortunately, most reports about ideal umbilicus placement are based on measurements made in women. Very few articles have compared male-to-female umbilicus position.18,23,43,52 In young men, the abdomen has a more triangular shape with midline depression and well-defined paired rectus muscles. Laterally, it has a slight concavity extending to the flanks. In women, an hourglass appearance is most common. Despite some opinions to the contrary, men have a preference for a greater waist to hip ratio and lower navel location.2,5,16,18,19,31,37,43,52,53 Moreover, rectus abdominis diastases are less common in men. Significant gender differences have also been described in anthropometric characteristics and in measurements between the umbilicus and fixed bony reference points.30,37 Evidently, guidelines deduced from analysis of photographs that may have been edited of selected female models not representative of the general population31,33 may not apply to men.
Undoubtedly, validity of measurements relies largely on ability to accurately and precisely identify various landmarks.54 Serious doubts exist regarding accuracy of the determination of reference points such as the abdominal crease, symphysis pubis, and xiphoid on two-dimensional photographs. In a study conducted on female models, it was reported that pubic symphysis can be difficult to determine on images; the lower limit of the vulvar cleft was suggested instead as a more dependable landmark.33 Exact xyphoid tip and symphysis pubis are particularly difficult to determine even by palpation in some overweight patients. Determination of these landmarks on photographs would certainly be highly inaccurate and derived ratios, and formulas would be likewise.
Confirming that some bony landmarks do not constitute reliable reference points, Visconti et al17 reported that the xiphoid and the abdominal crease are best chosen as superior and inferior abdominal aesthetic limits and used for defining umbilicus positioning guidelines. However, despite recommendations that for clinical application, measurements should be obtained in a straight line, and not conforming to the three-dimensional abdominal anatomy, accurate intraoperative determination of abdominal crease during surgery is certainly not straightforward. Clinical practicality of the golden correlation of Visconti et al17 is questionable. The suggestion to use the Fibonacci caliper intraoperatively is highly ingenious55; however, this may not be practical.
We believe that in men, the upper aesthetic unit limit must be at the sternal notch, not the xiphisternum, and that intraoperative determination of U-AX and N-N can be made more readily than measuring U-ACr position. Unlike in women, optimal umbilicus and nipple positions seem to be aesthetically interrelated and function conjointly to enhance attractiveness of rejuvenated anterior male trunks when discordance is avoided.20 Although beauty and attractiveness are based on biology rather than on mathematics, optimal form and function are mysteriously bound by a “universal” divine proportion.56,57
Most reported studies have focused on preoperative evaluation and surgical planning. Umbilical position alterations after surgery have not been well investigated. A short communication about a limited study has shown that with time the umbilicus becomes displaced cephalically.58 Thus, efforts made intraoperatively for precise umbilicus reposition may be not very relevant because outcome stability is relative. As for midline placement, likelihood for reversion of umbilicus repositioning is high unless asymmetry and deep stalk position has been addressed by eccentric plication.3
As with most concepts of beauty and attractiveness, there is a spectrum of subjective opinions and personal preferences regarding optimal umbilicus relocation.31 Arguing that there is no universal agreement, some surgeons allow their patients to make their own choices.10 Similar to what has been described for vertical nipple level,20 defining a range for pleasant umbilicus positioning is probably more constructive. Hoyos et al7,8 have stressed that an ideal umbilicus zone would allow some freedom for preferred localization. By measuring male abdomens from xiphoid to pubis, this zone was defined by the overlapping area between the lower abdominal third and the upper three-quarters, without, however, any objective justification.
Lack of positive correlation of our equation with umbilicus position in older-aged cadavers is not really relevant because almost all patients seeking abdominal contouring look for abdominal rejuvenation irrespective of their chronologic age. As for BMI effect, we assume that abdomens with well-positioned umbilicus of young, fit, and healthy individuals would also be preferred by men with higher BMI.
Because determining normality is essential and averageness constitutes a key element in perception of human beauty,59–61 the main strength of this study is that it has been conducted on regular volunteers in the standing position and on cadavers in the supine position, not on two-dimensional photographs of idealized models. Nevertheless, there are some limitations to the study related to manual measurements by several investigators and the limited precision in determining bony and surface reference points. Moreover, because standing position measurements and subsequent calculations were not tested to be the same in supine position, validity of transposing these measurements intraoperatively may be questioned. Obviously, their intraoperative validity, as described in the simulation in Figure 5 is needed. Furthermore, whether umbilicus position determined by N-N/U-AX is most aesthetic and would fit ideal male beauty needs to be investigated. Validity of the formula in the presence of various degrees of male gynecomastia will also need to be determined.
Fig. 5.
Clinical simulation of ideal umbilical positioning that can be performed intraoperatively in the supine position. Step 1: measurement in the standing position of inter-nipple distance. Step 2: calculation of U-AX distance. Step 3: Intraoperative determination of umbilical position using a surgical thread or a measuring tape to transpose the calculated U-AX distance at the intersection with the midline.
CONCLUSIONS
Of all the measured reference points in male volunteers, a constant golden number relationship could be identified only between N-N and U-AX. This relationship has already been clinically tested and reported for determination of nipple position.17,59,61 Compared with the method described by Graham et al,23 it is more predictive of the most appropriate umbilicus position. Measurement of N-N is also more practical and accurate than U-ACr. Unlike in women, male umbilicus-nipples relationship indicates that the anterior trunk aesthetic unit encompasses both abdomen and thorax and that nipples and umbilicus are the main visual aesthetic landmarks. This relationship must be respected to avoid unaesthetic discordance.
DISCLOSURE
The authors have no financial interest to declare in relation to the content of this article.
Footnotes
Published online 16 October 2023.
Disclosure statements are at the end of this article, following the correspondence information.
Bishara S. Atiyeh and Saif E. Emsieh contributed equally.
REFERENCES
- 1.Srinivasan J, Soueid A. Where to position of the umbilicus during abdominoplasty?—look at the root! J Plast Reconstr Aesthet Surg. 2009;62:e536–e537. [DOI] [PubMed] [Google Scholar]
- 2.Sood R, Muhammad LN, Sasson DC, et al. Development and initial validation of a novel professional aesthetic scale for the female abdomen. Plast Reconstr Surg. 2022;150:546e–556e. [DOI] [PubMed] [Google Scholar]
- 3.Vavra JM, Kachare SD, Vivace BJ, et al. Centralizing the umbilicus in abdominoplasty: eccentric versus concentric fascial plication in addition to medializing at the skin. Plast Reconstr Surg. 2023;151:526–531. [DOI] [PubMed] [Google Scholar]
- 4.Çelik V, Tuluy Y, Sir E. Modified diamond-shaped umbilicoplasty in abdominoplasty. Aesthetic Plast Surg. 2023. [E-pub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 5.Delpierre V, Coquerel-Beghin D, Aktouf A, et al. Analyse biométrique et morphométrique de l’ombilic. À propos de 70 cas [Biometric and morphometric analyse of the umbilicus: about 70 cases]. Ann Chir Plast Esthet. 2012;57:575–579. French. [DOI] [PubMed] [Google Scholar]
- 6.Yu AY. Restoration liposuction of the abdomen: high-definition liposuction with umbilicus and lower abdomen improvement using polydioxanone threads. Aesthet Surg J. 2023;43:NP413–NP423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoyos AE, Perez ME, Mogollon IR, et al. H-wing neoumbilicoplasty: a new technique for advanced abdominoplasty and umbilical zones by gender. Plast Reconstr Surg. 2023;151:52–62. [DOI] [PubMed] [Google Scholar]
- 8.Hoyos A, Perez ME, Guarin DE, et al. A report of 736 high-definition lipoabdominoplasties performed in conjunction with circumferential VASER liposuction. Plast Reconstr Surg. 2018;142:662–675. [DOI] [PubMed] [Google Scholar]
- 9.Sisti A, Huayllani MT, Boczar D, et al. Umbilical reconstruction techniques: a literature review. Aesthetic Plast Surg. 2021;45:1078–1096. [DOI] [PubMed] [Google Scholar]
- 10.Martinez-Teixido L, Serra-Mestre JM, Serra-Renom JM. A new technique for creating a neo-umbilicus in abdominoplasty. J Plast Reconstr Aesthet Surg. 2017;70:1760–1767. [DOI] [PubMed] [Google Scholar]
- 11.Akbaş H, Güneren E, Eroğlu L, et al. Natural-looking umbilicus as an important part of abdominoplasty. Aesthetic Plast Surg. 2003;27:139–142. [DOI] [PubMed] [Google Scholar]
- 12.Vernon S. Umbilical transplantation upward and abdominal contouring in lipectomy. Am J Surg. 1957;94:490–492. [DOI] [PubMed] [Google Scholar]
- 13.Moellhoff N, Staiger TJ, Ehrl D, et al. Identifying the most attractive umbilical position—an eye tracking- and survey-based investigation. J Plast Surg Hand Surg. 2021;56:369–375. [DOI] [PubMed] [Google Scholar]
- 14.Craig SB, Faller MS, Puckett CL. In search of the ideal female umbilicus. Plast Reconstr Surg. 2000;105:389–392. [DOI] [PubMed] [Google Scholar]
- 15.Rysin R, Wolf Y. Facilitated umbilical positioning in abdominoplasty using the 15/10 rule and the “flap flipping” technique. Plast Reconstr Surg Glob Open. 2021;9:e3574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.O’Kelly N, Nguyen K, Gibstein A, et al. Standards and trends in lipoabdominoplasty. Plast Reconstr Surg Glob Open. 2020;8:e3144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Visconti G, Visconti E, Bonomo L, et al. Concepts in navel aesthetic: a comprehensive surface anatomy analysis. Aesthetic Plast Surg. 2015;39:43–50. [DOI] [PubMed] [Google Scholar]
- 18.Pallua N, Markowicz MP, Grosse F, et al. Aesthetically pleasant umbilicoplasty. Ann Plast Surg. 2010;64:722–725. [DOI] [PubMed] [Google Scholar]
- 19.Stein MJ, Matarasso A. The male abdominoplasty. Clin Plast Surg. 2022;49:285–291. [DOI] [PubMed] [Google Scholar]
- 20.Atiyeh BS, Dibo SA, El Chafic AH. Vertical and horizontal coordinates of the nipple-areola complex position in males. Ann Plast Surg. 2009;63:499–502. [DOI] [PubMed] [Google Scholar]
- 21.Atiyeh BS, Dibo SA, El Chafic AH. Determination of the nipple-areola complex position on the male thorax. Plast Reconstr Surg. 2009;123:156e–158e. [DOI] [PubMed] [Google Scholar]
- 22.Atiyeh BS, Dibo SA, Hayek SN. Contouring of the male anterior chest following bariatric surgery and massive weight loss. Aesthet Surg J. 2008;28:688–696. [DOI] [PubMed] [Google Scholar]
- 23.Graham KA, Livingston RJ. Ideal male umbilicus: an observational study of surface anatomy and introduction to the SHAPE classification. Aesthetic Plast Surg. 2022;46:2333–2341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oh S, Jeon H, Son D. Location of the umbilicus in Korean women and its changes after breast reconstruction with an ipsilateral pedicled rectus abdominis musculocutaneous flap. Arch Plast Surg. 2018;45:425–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee YT, Kwon C, Rhee SC, et al. Four flaps technique for neoumbilicoplasty. Arch Plast Surg. 2015;42:351–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rodriguez-Feliz JR, Makhijani S, Przybyla A, et al. Intraoperative assessment of the umbilicopubic distance: a reliable anatomic landmark for transposition of the umbilicus. Aesthetic Plast Surg. 2012;36:8–17. [DOI] [PubMed] [Google Scholar]
- 27.Dubou R, Ousterhout DK. Placement of the umbilicus in an abdominoplasty. Plast Reconstr Surg. 1978;61:291–293. [DOI] [PubMed] [Google Scholar]
- 28.Shoukas J, Christopoulos N, Kouris G, et al. Umbilical quest: a new technique for accurately identifying the new position of the umbilicus in abdominoplasty using a Lockwood marker. Plast Reconstr Surg. 2009;123:120e–121e. [DOI] [PubMed] [Google Scholar]
- 29.Mazzocchi M, Dessy LA, Figus A. A versatile technique for repositioning of the umbilicus in abdominoplasty. Plast Reconstr Surg. 2008;121:357e–358e. [DOI] [PubMed] [Google Scholar]
- 30.Duduković M, Kisić H, Baez ML, et al. Anatomical prediction for surgical positioning of the umbilicus in a Croatian population. Ann Plast Surg. 2015;75:135–139. [DOI] [PubMed] [Google Scholar]
- 31.Matarasso A, Matarasso DM, Matarasso EJ. Invited commentary of “concepts in navel aesthetic: a comprehensive surface anatomy analysis.” Aesthetic Plast Surg. 2015;39:51–52. [DOI] [PubMed] [Google Scholar]
- 32.Ambardar S, Cabot J, Cekic V, et al. Abdominal wall dimensions and umbilical position vary widely with BMI and should be taken into account when choosing port locations. Surg Endosc. 2009;23:1995–2000. [DOI] [PubMed] [Google Scholar]
- 33.Lee SJ, Garg S, Lee HP. Computer-aided analysis of the “beautiful” umbilicus. Aesthet Surg J. 2014;34:748–756. [DOI] [PubMed] [Google Scholar]
- 34.Rohrich RJ, Sorokin ES, Brown SA, et al. Is the umbilicus truly midline? Clinical and medicolegal implications. Plast Reconstr Surg. 2003;112:259–263; discussion 264–265. [DOI] [PubMed] [Google Scholar]
- 35.Baroudi R. Umbilicaplasty. Clin Plast Surg. 1975;2:431–448. [PubMed] [Google Scholar]
- 36.Pitanguy I. Abdominal lipectomy: an approach to it through an analysis of 300 consecutive cases. Plast Reconstr Surg. 1967;40:384–391. [Google Scholar]
- 37.Reho A, Randisi F, Ferrario A, et al. “Scarless reverse umbilicoplasty”: a new technique of umbilical transposition in abdominoplasty. J Plast Reconstr Aesthet Surg. 2019;72:656–661. [DOI] [PubMed] [Google Scholar]
- 38.Kurul S, Uzunismail A. A simple technique to determine the future location of the umbilicus in abdominoplasty. Plast Reconstr Surg. 1997;100:753–754. [DOI] [PubMed] [Google Scholar]
- 39.Mowlavi A, Huynh PM, Huynh DC, et al. A new technique involving a spherical stainless steel device to optimize positioning of the umbilicus. Aesthetic Plast Surg. 2012;36:1062–1065. [DOI] [PubMed] [Google Scholar]
- 40.Hoffman S. A simple technique for locating the umbilicus in abdominoplasty. Plast Reconstr Surg. 1989;83:537–538. [DOI] [PubMed] [Google Scholar]
- 41.Pitchon L, Rubinstein C. A (more) simple technique for locating the umbilicus in abdominoplasty. Aust N Z J Surg. 1993;63:42–43. [DOI] [PubMed] [Google Scholar]
- 42.Colwell AS, Kpodzo D, Gallico GG, III. Low scar abdominoplasty with inferior positioning of the umbilicus. Ann Plast Surg. 2010;64:639–644. [DOI] [PubMed] [Google Scholar]
- 43.Yu D, Novicoff WM, Gampper TJ. The average size and position of the umbilicus in young men and women. Ann Plast Surg. 2016;76:346–348. [DOI] [PubMed] [Google Scholar]
- 44.Wan D, Hubbard BA, Byrd HS. Achieving aesthetic results in the umbilical float mini-abdominoplasty: patient selection and surgical technique. Plast Reconstr Surg. 2019;143:722–732. [DOI] [PubMed] [Google Scholar]
- 45.Correia N, Jayyosi L, Chiriac S, et al. Morphometric analysis of the umbilicus according to age. Aesthet Surg J. 2018;38:627–634. [DOI] [PubMed] [Google Scholar]
- 46.Abhyankar SV, Rajguru AG, Patil PA. Anatomical localization of the umbilicus: an Indian study. Plast Reconstr Surg. 2006;117:1153–1157. [DOI] [PubMed] [Google Scholar]
- 47.Ribeiro RC, Saltz R, Ramirez C, et al. Anatomical position of umbilicus in Latin-American patients. Eur J Plast Surg 2019;42:351–358. [Google Scholar]
- 48.Parnell BA, Midia EC, Fielding JR, et al. Relationship between race and abdominal anatomy: effect on robotic port placement. Female Pelvic Med Reconstr Surg. 2013;19:165–168. [DOI] [PubMed] [Google Scholar]
- 49.Bilgen F, Duman Y, Ural A, et al. Determining anatomical position of the umbilicus in Turkish population. Indian J Surg. 2020;82:899–904. [Google Scholar]
- 50.Danilla S, Bonasic S. Anatomical localization of the umbilicus: a statistical analysis. Plast Reconstr Surg. 2007;119:1123–1124. [DOI] [PubMed] [Google Scholar]
- 51.Parnia R, Ghorbani L, Sepehrvand N, et al. Determining anatomical position of the umbilicus in Iranian girls, and providing quantitative indices and formula to determine neo-umbilicus during abdominoplasty. Indian J Plast Surg. 2012;45:94–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Freeman BS, Wiemer DR. Abdominoplasty with special attention to construction of the umbilicus: technique and complications. Aesthetic Plast Surg. 1978;2:65–74. [DOI] [PubMed] [Google Scholar]
- 53.Babaitis R, Villegas FJ, Hoyos AE, et al. TULUA male high-definition abdominoplasty. Plast Reconstr Surg. 2022;149:96–104. [DOI] [PubMed] [Google Scholar]
- 54.Bragança S, Arezes P, Miguel Carvalho M, et al. Current state of the art and enduring issues in anthropometric data collection. Dyna rev.fac.nac.minas 2016;83:22–30. [Google Scholar]
- 55.Visconti G, Salgarello M. The divine proportion “ace of spades” umbilicoplasty: a new method of navel positioning and plasty in abdominoplasty. Ann Plast Surg. 2016;76:265–269. [DOI] [PubMed] [Google Scholar]
- 56.Yalta K, Ozturk S, Yetkin E. Golden ratio and the heart: a review of divine aesthetics. Int J Cardiol. 2016;214:107–112. [DOI] [PubMed] [Google Scholar]
- 57.Hwang K, Park CY. The divine proportion: origins and usage in plastic surgery. Plast Reconstr Surg Glob Open. 2021;9:e3419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Chin SH, Martin WJ, Matarasso A. Do waistline and umbilical position really change after abdominoplasty? Plast Reconstr Surg. 2010;125:27e–28e. [DOI] [PubMed] [Google Scholar]
- 59.Yarosh DB. Perception and deception: human beauty and the brain. Behav Sci (Basel). 2019;9:34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Maymone MBC, Laughter M, Dover J, et al. The malleability of beauty: perceptual adaptation. Clin Demerol. 2019;37:592–596. [DOI] [PubMed] [Google Scholar]
- 61.Aly A. Editorial comment on “revision abdominoplasty and proper umbilical positioning.” Clin Plast Surg. 2010;37:547. [DOI] [PubMed] [Google Scholar]