ABSTRACT
Objective:
to determine the prevalence and describe the main morphological and metric variations of the splenic artery in terms of its origin, path and polar and terminal branches.
Methods:
cross-sectional study, carried out at Hospital de Clínicas between July and November 2020. Computed tomography scans were analyzed with intravenous contrast of the patients seen at the Radiology and Diagnostic Imaging Service. The findings were categorized as to origin, path and splenic ramifications.
Results:
1,235 patients were evaluated. As for the origin, the splenic artery appears in the celiac trunk in 99.11% of the individuals. Of these, 5.95% have a bifurcated celiac pattern, 92.17% trifurcated and 1.88% tetrafurcated. The mean arterial diameter was 5.92mm (±1.2), the highest one being in white men. As for the path, the splenic artery was unique in the entire sample. The suprapancreatic course was found in 75.63% of the individuals, with a higher occurrence in women, 78.87% (p<0.001). The terminal splitting pattern of the splenic artery was characterized by the bifurcated type (95.47%). The terminal branches seen most frequently were those with three arteries (34.90%) and most individuals did not have polar branches.
Conclusion:
the splenic artery presents a highly variable pattern of origin and its average caliber is influenced by sex and color. The suprapancreatic path was the most characteristic and predominant in females. The bifurcated pattern of final division, with three terminal branches and the absence of polar arteries, occurs more frequently.
Keywords: Splenic Artery, Anatomic Variation, Anatomy, Surgery, Computed Tomography
RESUMO
Objetivo:
determinar a prevalência e descrever as principais variações morfológicas e métricas da artéria esplênica quanto a sua origem, trajeto e ramos terminais e polares.
Métodos:
estudo transversal, realizado no Hospital de Clínicas entre julho e novembro de 2020. Foram analisadas tomografias computadorizadas com contraste endovenoso dos pacientes atendidos no Serviço de Radiologia e Diagnóstico por Imagem. Os achados foram categorizados quanto à origem, trajeto e ramificações esplênicas.
Resultados:
foram avaliados 1.235 pacientes. Quanto à origem, a artéria esplênica surge no tronco celíaco em 99,11% dos indivíduos. Desses, 5,95% apresentam padrão celíaco bifurcado, 92,17% trifurcado e 1,88% tetrafurcado. O diâmetro arterial médio foi de 5,92mm (±1,2), sendo a maior média em homens brancos. Quanto ao trajeto, a artéria esplênica se apresentou única em toda a amostra. O curso suprapancreático esteve em 75,63% dos indivíduos, com maior ocorrência em mulheres 78,87% (p<0,001). O padrão de divisão terminal da artéria esplênica caracterizou-se pelo tipo bifurcado (95,47%). Os ramos terminais visualizados mais frequentemente foram os com três artérias (34,90%) e a maioria dos indivíduos não apresentou ramos polares.
Conclusão:
a artéria esplênica apresenta padrão de origem altamente variável e seu calibre médio é influenciado por sexo e cor. O trajeto suprapancreático foi o mais característico e predominou no sexo feminino. O padrão bifurcado de divisão final, com três ramos terminais e ausência de artérias polares, ocorre com maior frequência.
Palavras-chave: Artéria Esplênica, Variação Anatômica, Anatomia, Cirurgia, Tomografia Computadorizada
INTRODUCTION
The splenic artery (SA) supplies the spleen and is responsible for part of the gastric and pancreatic blood input 1 . Its conventional emergence occurs in the abdominal portion of the aorta, at the level of the twelfth thoracic vertebra. At this point, the celiac trunk (CTR) gives rise to the branches of the left gastric artery (LGA), SA, and the common hepatic artery (CHA). The SA tortuously travels along the superior and posterior margin of the pancreas to the spleen. However, anatomical variations of the CTR may occur, including a bifurcated presentation, a trifurcated one different from the hepatogastrosplenic, a tetrafurcated, and even the absence of a trunk 2 . After its origin, the SA follows its course retroperitoneally, along the superior and posterior margins of the body and tail of the pancreas, following a horizontal and tortuous course to cross the splenorenal ligament towards the splenic hilum 3 . On its way, the artery gives off branches that carry blood supply to the stomach and pancreas and, finally, enters the splenorenal ligament, near the tail of the pancreas, where it divides into several branches, grouped into superior and inferior. Each terminal branch gives off small arteries that penetrate the splenic hilum. The branches that migrate to the upper or lower end of the spleen are called polar 3 - 5 .
The presentation of SA has variations in origin, course, ramifications, and anatomical relationships, and knowledge about the vascular pattern systematizes and facilitates the recognition of its anomalies 6 . The identification of such anomalies has gained importance since 1590, when Franciscus Rosetti performed the first partial splenectomy. The origin of SA, as well as its collateral and terminal branches, are factors to be considered, since they influence the surgical tactic to be used in gastric, pancreatic, splenic, and portal hypertension procedures 6 . The rare studies on anatomical variations and the imprecision of morphological and metric data of SA motivated this study, with the objective of determining the prevalence and describing the main morphological and metric variations of the SA origin, course, and its terminal and polar branches.
METHODS
In compliance with Resolution 466/2012 of the National Health Council, the study protocol was approved by the Ethics Committee in Research with Human Beings of the Universidade Federal da Fronteira Sul. The study was exempted from the Free and Informed Consent Form (Registration number 3,929,428).
The study is characterized as cross-sectional and was carried out at Hospital de Clínicas de Passo Fundo (HCPF), State of Rio Grande do Sul, Brazil. The non-probabilistic sample was selected for convenience and consisted of patients of any age and both sexes, seen between August 1 and December 31, 2018, at the Radiology and Diagnostic Imaging Service of the HCPF. Considering an expected prevalence of 10% of alterations in the origin of the splenic artery and a confidence interval of 95%, the estimated sample size would be 139 participants. However, to increase results’ accuracy, we decided to include a greater number of patients, defining the population according to a determined period of patient care.
Thus, for the composition of the sample, the radiology service provided a list with 2,000 codes referring to patients. From this list, we excluded duplicated codes, as some patients underwent more than one CT scan in the period. Secondly we excluded CT scans of patients with a previous history of splenic surgery, in addition to those that did not use intravenous contrast and those that contained alterations that made it impossible to perform morphometric measurements.
Initially, we sought electronic medical records (PEP Software, MV2000) to exclude patients with a history of previous splenic surgery and to access demographic information. After this screening, we performed the tomographic evaluation using the Picture Archiving and Communication System (PACS®) Arya Aurora (Pixeon®, 2020). Through CT scans, we obtained the diameter of the splenic artery at its origin, the place of origin, course, number of splenic arterial branches, and polar arteries. Two physicians specialized in abdominal radiology carried out the evaluation, which were double-typed and validated using the EpiData® open-source software, version 3.1.
Statistical analysis included descriptive measurements and verification of the frequency distribution of the type of splenic artery course according to sex (Pearson chi-square, assuming an α error of 5%). Moreover, we compared the mean diameters at the SA origin according to sex and skin color (Student’s t test, α error of 5%). All analyzes were performed with the PSPP® open-source software.
RESULTS
The sample consisted of 1,235 participants, who were predominantly male (50.53%), white (93.96%), and aged between 60 and 69 years (24.21%).
The origin of the SA was observed from some conformation of the CTR in 99.11% of the sample. In the remaining, we observed direct emergence from the abdominal aorta (AA) in 0.65%, from the CHA in 0.16%, and from the superior mesenteric artery (SMA) in 0.08%. Of those originating from the CTR, 5.95% had a bifurcated celiac pattern, 92.17% trifurcated, and 1.88% tetrafurcated (Table 1).
Table 1. Características da artéria esplênica.
| Variables | n | % |
|---|---|---|
| Origin | ||
| Celiac trunk | 1,224 | 99.11 |
| Abdominal aorta | 8 | 0.65 |
| Superior mesenteric | 1 | 0.08 |
| Common hepatic | 2 | 0.16 |
| Type of celiac origin | ||
| Bifurcated | 73 | 5.95 |
| Variables | n | % |
| Trifurcated | 1,130 | 92.17 |
| Tetrafurcated | 23 | 1.88 |
| Course | ||
| Single | 1,235 | 100 |
| Course type | ||
| Suprapancreatic | 934 | 75.63 |
| Dorsal | 301 | 24.37 |
| Final branching pattern | ||
| Bifurcated | 1,179 | 95.47 |
| Trifurcated | 56 | 4.53 |
| Terminal splenic branches | ||
| 1 | 2 | 0.16 |
| 2 | 135 | 10.93 |
| 3 | 438 | 34.90 |
| 4 | 428 | 34.10 |
| 5 | 176 | 14.02 |
| 6 | 42 | 3.40 |
| 7 | 11 | 0.89 |
| 8 | 3 | 0.24 |
| Polar splenic branches | ||
| 0 | 1,113 | 90.12 |
| 1 | 113 | 9.15 |
| 2 | 8 | 0.65 |
| 3 | 1 | 0.08 |
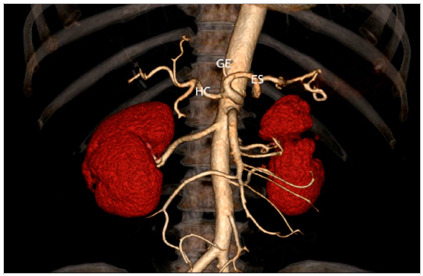
In those with trifurcated trunks, the classic presentation, formed by the common, splenic, and left gastric hepatic arteries (Figure 1) occurred in 98.94.
Figure 1. Three-dimensional reconstruction demonstrating the celiac trunk with usual branching into the left gastric (LGA), splenic (SA) and common hepatic (CHA) arteries.
The SA course was single in the entire sample, and regarding the course, it was classified as suprapancreatic and dorsal (Figure 2), being suprapancreatic in 75.63% and dorsal in 24.37% individuals (Table 1).
Figure 2. Computed tomography sagittal plane reconstructions demonstrating (A) dorsal course (white arrow) and (B) suprapancreatic course (white arrow) of the splenic artery.
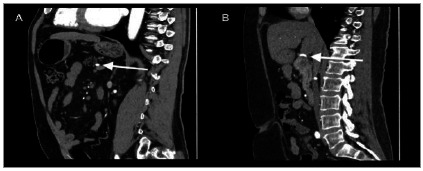
Table 2 shows the frequency of the SA course type according to patients’ sex. There was a predominance of the suprapancreatic course in relation to the dorsal course in both sexes, with the suprapancreatic distribution being more frequent in females compared with males (78.87% vs. 71.47%) and the dorsal course was more predominant in men (28.53% vs. 20.13%), p=0.001.
Table 2. Type and distribution of splenic artery course by sex.
| Suprapancreatic | Dorsal | p | |||
|---|---|---|---|---|---|
| Variable | n | % | n | % | |
| Sex | 0.001 | ||||
| Male | 446 | 71.47 | 178 | 28.53 | |
| Female | 488 | 78.87 | 123 | 20.13 | |
*Chi-square test.
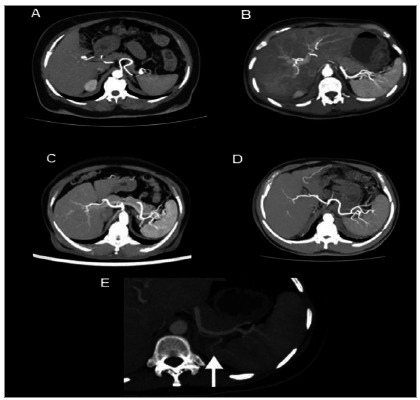
Regarding the splenic branches, the terminal arteries presented as one artery in 0.16% of the individuals, two in 10.93%, three in 34.90%, four in 34.10%, five in 14.02%, six in 3.40%, seven in 0.89%, and eight in 0.24%. We found polar splenic branches in 9.88% of the sample. We observed a single polar branch in 9.15% of the individuals, two in 0.65%, and three in 0.08%. That is, the most common terminal patterns were those that presented between two and five arteries and, among those that presented polar branches, a single branch was the most common (Table 1). Figure 3 shows the images of the most frequently observed patterns.
Figure 3. Maximum Intensity Projection (MIP) reconstructions in the axial computed tomography plane demonstrating (A) two terminal branches, (B) three terminal branches, (C) four terminal branches, (D) five terminal branches, and (E) polar artery (white arrow).
As for the metric findings, the mean diameter of the splenic artery at its origin was 5.92mm (±1.2), with a range of 2.81mm to 10.84mm. There was also a statistically significant difference in diameter variation in relation to sex and race. We found a higher mean diameter in males (6.16mm ±1.17; p<0.001) and in whites (5.93mm ±1.14; p=0.041) (Table 3).
Table 3. Diameter of the splenic artery at its origin by sex and race.
| Diameter (mm) | |||
|---|---|---|---|
| Variable | n (%) | Mean (±SD) | p |
| Sex | <0.001 | ||
| Male | 624 (50.53) | 6.16 ± 1.17 | |
| Female | 611 (49.47) | 5.67 ± 1.07 | |
| Race (n=1,226) | 0.041 | ||
| White | 1.152 (93.96) | 5.93 ± 1.14 | |
| Others | 74 (6.04) | 5.66 ± 1.05 | |
SD: standard deviation; *Student ‘s t test.
DISCUSSION
Origin
The exact identification of the splenic artery’s origin, as well as its metric characteristics, is essential not only for surgical planning, but also to avoid iatrogenic injuries during surgery. Thus, knowledge of its origin and diameter is essential in gastrointestinal operations and, especially, in the application of stents in endovascular surgery 7 . During embryogenesis, each metameric level gives rise to three pairs of arteries from the aorta. The posterior ones are parietal, the lateral ones are urogenital, and the anterior ones are intestinal. According to Tandler et al., the intestinal arteries are connected by an anterior longitudinal anastomosis (laengsanastomosis) 8 . Of the four arterial roots, two disappear and the remaining anastomoses give rise to the CHA, SA, and LHA 9 . The exacerbated growth or regression of these vessels is related to the occurrence of variations in the celiac trunk and in the superior mesenteric artery.
Méndez found that the emergence of SA from the CTR occurs in 88.46% 5 . Clement et al., in a survey with cadavers and imaging exams, observed 90.5% of occurrence of the classic pattern of trifurcation 10 . According to Song et al., the CTR classic presentation occurs in 89.1% 1 1 . In the present study, the splenic artery presented celiac origin in 99.11% of the patients and the classic presentation of the hepatogastrosplenic trunk occurred in 91.47%. The observation of higher frequencies may be due to the differences between the studied samples, especially regarding sample size and ethnic origin of the participants, in addition to the particularities of the methods used in the studies.
The SA emergence from the abdominal aorta occurred only in 0.65% of the sample, from the common hepatic artery in 0.16%, and from the superior mesenteric artery in 0.08%. These findings are similar to those of Indian studies 12 - 13 . The bifurcated celiac trunk, in different combinations, has been observed in up to 12% of the population 1 2 . In this study, CTR bifurcation was found in 5.95% of the sample.
The metric assessment of the splenic artery diameter at its origin resulted in an average of 5.92mm (± 1.2), with a variation from 2.81mm to 10.84mm. Méndez found that the mean SA length was 147mm, with a range from 81mm to 306mm and that its mean diameter was 8.6mm, with a range of 4 to 11mm 5 . In this study, male subjects had a higher mean arterial diameter than females (6.16 ± 1.17 : 5.67 ± 1.07), and white subjects had a higher mean than other races (5.93 ± 1.14 : 5.66 ± 1.05). We found no studies in the literature that evaluated the relationship between these variables.
Course
The course of SA can be classified as having two main patterns: the suprapancreatic course, where the artery curves and runs superior to the pancreas, and the dorsal course, where it runs relatively straight to the dorsal side of the pancreas. We observed a splenic artery single course throughout the sample, with no occurrence of its duplicated form. We found a suprapancreatic course in 75.63% and a dorsal one in 24.37% of the individuals. Such findings are in line with a study carried out on 320 cadavers, that recorded a suprapancreatic path in 74.1% 1 . Although we found no previous reports in the literature on the course type according to sex, we observed that the suprapancreatic path was more frequent in both sexes in our sample. However, when comparing the sexes within each pattern, there was a predominance of females and males, respectively, in the suprapancreatic and dorsal courses.
Knowledge of the path can influence the surgical technique used. The study carried out by Inoko et al. demonstrated that the safety of laparoscopic splenic-preserving distal pancreatectomy is associated with a previous study of the SA course and terminal branches 15 . The surgical technique used was decided according to the arterial path, and in cases where the course was suprapancreatic, the peritoneal incision was performed along the pancreatic border. In cases where the SA course was dorsal, the artery was exposed and protected by the inferior approach 15 - 19 .
Branching
Knowledge of the intraparenchymal division of the splenic artery is essential in partial splenectomy. Therefore, understanding the vascular network presentation facilitates its rapid identification and characterizes an important parameter for surgical guidance 20 .
The pattern of terminal division of the splenic artery was mostly characterized by the bifurcated type (95.47%). The trifurcated presentation was present in 4.53%. The findings are similar to those observed in a Brazilian study with 60 arteriographies, in which the bifurcated type appeared in 93.3%, and the trifurcated, in 6.7% 20 . Regarding terminal splenic ramifications, the most frequently found were those of three (34.90%) and four arteries (34.10%). A single branch occurred in 0.16% of the cases. In the observations carried out in an Indian study, the splenic artery divided into terminal branches in 97.2% and, in the remaining cases, it entered the splenic hilum without branching. Also in the same study, the authors identified a higher frequency of two (63.1%) and four (18.8%) terminal branches 1 . The absence of splenic polar arteries predominated in the sample. A single polar artery was present in 9.15%, two in 0.65%, and three in only 0.08% of the individuals.
The main strengths of this study include the detailed description of the anatomical course of the splenic artery, the variation in arterial diameter according to sex and race, as well as the difference observed in the type of course according to sex. In this context, it is important to emphasize that the analysis of arterial diameter, when performed, is carried out in cadavers, with a reduced sample number, or even in patients with arteries affected by some disease. In this case, our study included a sample of more than 1,200 cases, with arteries without clinical involvement. It is also noteworthy that the observation of a higher frequency of the suprapancreatic course in both sexes and a greater frequency of the dorsal course in men is unprecedented in the literature.
CONCLUSION
The splenic artery has a highly variable pattern of origin, and its average caliber is influenced by patients’ sex and skin color. Its course is mostly suprapancreatic and is even more common in females. The bifurcated pattern of final division, with three terminal branches and absence of polar arteries, was the most frequent.
Footnotes
Funding source: none.
REFERENCES
- 1.Moore KL, Dalley AF, Agur AMR. Anatomia orientada para a clínica. 7. Rio de Janeiro: Guanabara Koogan; 2014. [Google Scholar]
- 2.Araujo SA, Neto, Franca HA, Mello CF, Júnior, Silva EJ, Neto, Negromonte GRP, Duarte CMA. Variações anatômicas do tronco celíaco e sistema arterial hepático uma análise pela angiotomografia multidetectores. Radiol Bras. 2015;48(6):358–362. doi: 10.1590/0100-3984.2014.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Patel SR, Lowe S. Accessory Splenic Artery A Rare Cause of Upper Gastrointestinal Bleeding. Cardiovasc Intervent Radiol. 2017;40(7):1115–1117. doi: 10.1007/s00270-017-1592-6. [DOI] [PubMed] [Google Scholar]
- 4.Wada Y, Aoki T, Murakami M. Individualized procedures for splenic artery dissection during laparoscopic distal pancreatectomy. BMC Surg. 2020;20(32):1–5. doi: 10.1186/s12893-020-00694-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Casado Méndez PR. Variantes anatómicas de la arteria esplénica. Rev Med Electrón. 2018;40(2):346–359. [Google Scholar]
- 6.Manterola C, Otzen T. Incidental Splenic Injury and Splenectomy An Overview Based on Available Evidence. Int. J. Morphol. 2016;34(4):1553–1560. [Google Scholar]
- 7.Panagouli E, Lolis E, Venieratos D. A morphometric study concerning the branching points of the main arteries in humans relationships and correlations. Ann Anat. 2011;193(2):86–99. doi: 10.1016/j.aanat.2010.10.009. [DOI] [PubMed] [Google Scholar]
- 8.Tandler J. über die Varietäten der Arteria coeliaca und deren Entwickelung. Anatomische Hefte. 1904;25:473–500. [Google Scholar]
- 9.Yi S-Q, Terayama H, Naito M, Hayashi S, Moriyama H, Tsuchida A. A common celiacomesenteric trunk, and a brief review of the literature. Ann Anat. 2007;189(5):482–488. doi: 10.1016/j.aanat.2006.11.013. [DOI] [PubMed] [Google Scholar]
- 10.Marco-Clement I, Martinez-Barco A, Ahumada N, Simon C, Valderrama JM, Sanudo J. Anatomical variations of the celiac trunk cadaveric and radiological study. Surg Radiol Anat. 2016;38(4):501–510. doi: 10.1007/s00276-015-1542-4. [DOI] [PubMed] [Google Scholar]
- 11.Song SY, Chung JW, Yin YH, Jae HJ, Kim HC, Jeon UB. Celiac axis and common hepatic artery variations in 5002 patients systematic analysis with spiral CT and DSA. Radiology. 2010;255(1):278–288. doi: 10.1148/radiol.09090389. [DOI] [PubMed] [Google Scholar]
- 12.Skandalakis JE. Skandalakis 'Surgical Anatomy: The Embryologic and Anatomic Basis of Modern Surgery. 1 ed. Athens, Greece: PMP; 2004. [Google Scholar]
- 13.Sankar KD, Bhanu PS, Susan PJ. Variant Anatomy of the Celiac Trunk and its Branches Int. J. Morphol. 2011;29(2):581–584. [Google Scholar]
- 14.Pandey SK, Bhattacharya S, Mishra RN, Shukla VK. Variações anatômicas da artéria esplênica e suas implicações clínicas. Clin Anat. 2004;17(6):497–502. doi: 10.1002/ca.10220. [DOI] [PubMed] [Google Scholar]
- 15.Inoko K, Ebihara Y, Sakamoto K, Miyamoto N, Kurashima Y, Tamoto E. Strategic Approach to the Splenic Artery in Laparoscopic Spleen-preserving Distal Pancreatectomy. Surg Laparosc Endosc Percutan Tech. 2015;25(4):e122–e125. doi: 10.1097/SLE.0000000000000182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carrere N, Abid S, Julio CH. Spleen-preserving distal pancreatectomy with excision of splenic artery and vein a case-matched comparison with conventional distal pancreatectomy with splenectomy. World J Surg. 2007;31(2):375–382. doi: 10.1007/s00268-006-0425-6. [DOI] [PubMed] [Google Scholar]
- 17.Choi SH, Seo MA, Hwang HK. Is it worthwhile to preserve adult spleen in laparoscopic distal pancreatectomy? Perioperative and patient-reported outcome analysis. Surg Endosc. 2012;26:3149–3156. doi: 10.1007/s00464-012-2306-4. [DOI] [PubMed] [Google Scholar]
- 18.Mellemkjaer L, Olsen JH, Linet MS. Risk of cancer following splenectomy. Int J Cancer. 1996;66(5):611–616. doi: 10.1002/(SICI)1097-0215(19960529)66:5<611::AID-IJC5>3.0.CO;2-W.. [DOI] [PubMed] [Google Scholar]
- 19.Fernandez-Cruz L, Martinez I, Gilabert R. Laparoscopic distal pancreatectomy combined with preservation of the spleen for cystic neoplasms of the pancreas. J Gastrointest Surg. 2004;8:493–501. doi: 10.1016/j.gassur.2003.11.014. [DOI] [PubMed] [Google Scholar]
- 20.Silva LFA, Silveira LMA, Timbó PS, Pinheiro SR, Barros LV, Silva AR., Filho Estudo morfométrico da divisão arterial do baço comparado ao estudo radiológico Rev. Col. Bras. Cir. 2011;38(3):181–185. doi: 10.1590/S0100-69912011000300008. [DOI] [PubMed] [Google Scholar]


