Abstract
Vaccine hesitancy poses a significant global health challenge, fueled by misinformation and anti-vaccination campaigns on social media platforms (SMPs). This study examines the influence of social media on coronavirus disease 2019 (COVID-19) and non-COVID-19 vaccination in Asia during the peri-pandemic period. Through a comprehensive analysis of available literature, we aim to elucidate the role of SMPs in shaping vaccination attitudes and behaviors. The findings highlight the detrimental impact of social media on vaccination efforts and provide insights into addressing vaccine hesitancy during this critical period. A narrative review was conducted by searching the PubMed, Scopus, and Google Scholar databases from inception to May 26, 2022. Only English-language articles involving human participants from Asian countries were included in this review. Out of the 228 articles identified through the database search, 14 articles were included in the final analysis. The prevalence of COVID-19 vaccine hesitancy or negative attitudes towards COVID-19 vaccines in Asian countries was found to be high, ranging from 20% to 55% across countries. Notably, reliance on SMPs for vaccine-related information was associated with a higher likelihood of COVID-19 vaccine hesitancy. This trend coincided with the proliferation of misinformation and conspiracy theories that portrayed COVID-19 vaccines as harmful during the pandemic. Similar patterns were observed for other types of vaccines, including polio, measles mumps and rubella, and diphtheria-tetanus-pertussis vaccines. The use of SMPs was also found to be associated with increased fear among caregivers in Asian countries, as well as a 3–4 times higher likelihood of delayed immunization. SMPs negatively impact vaccine intent in Asia due to misinformation and anti-vaccination campaigns during the pandemic. However, they can be a powerful tool for healthcare providers and policymakers to promote informed decision-making. Efforts should focus on leveraging SMPs to disseminate reliable information and combat hesitancy, fostering a well-informed and vaccinated population in Asia.
Keywords: Social Media; Immunization, Misinformation; Vaccine Hesitancy
INTRODUCTION
Immunization is crucial for preventing infectious diseases, yet global vaccine coverage has stagnated in the past decade. The World Health Organization (WHO) identified vaccine hesitancy as a major threat to global health in 2019.1 This hesitancy has contributed to a resurgence of vaccine-preventable diseases (VPDs) in Asian countries and worldwide.2,3,4
The coronavirus disease 2019 (COVID-19) pandemic has had a significant impact on healthcare systems worldwide, leading to disruptions in access to healthcare.5 As a result, millions of children missed out on vaccination in 2020, surpassing the numbers from previous years. This decline in vaccination rates is occurring despite the well-established safety of vaccines.5,6 Various factors contribute to the hesitancy and reluctance towards vaccination, with one of the primary concerns being the perceived long-term safety of vaccines. This apprehension was especially prevalent during the initial stages of COVID-19 vaccination when limited information on vaccine safety was available. Additionally, low-income countries may experience higher levels of vaccine hesitancy, influenced by cultural contexts, healthcare systems, lack of trust in health authorities, and limited access to vaccines.7,8,9,10
Asians make up the majority of social media platform (SMP) users in the world, with many countries having over 90% rates of SMP penetration in their populations.11 During COVID-19 pandemic and post-pandemic period, SMPs were the primary source of information on COVID-19 and COVID-19 vaccines for the general Asian population. This is especially relevant for Asian countries where trust in the government is low. Unfortunately, SMPs are also where misinformation and propaganda campaigns are the most prevalent. Understanding of how SMPs have influenced Asian people’s decision to accept or reject vaccination is the first and arguably most important step towards building more robust vaccination policies to ensure that Asian people make vaccination decision based on accurate and complete information.
This review aims to assess the influence of social media on COVID-19 vaccination in Asia during the pandemic period. Additionally, we examine the impact of social media on non-COVID-19 vaccination efforts in Asia to provide a comprehensive understanding of vaccination hesitancy in the region.
SEARCH STRATEGY
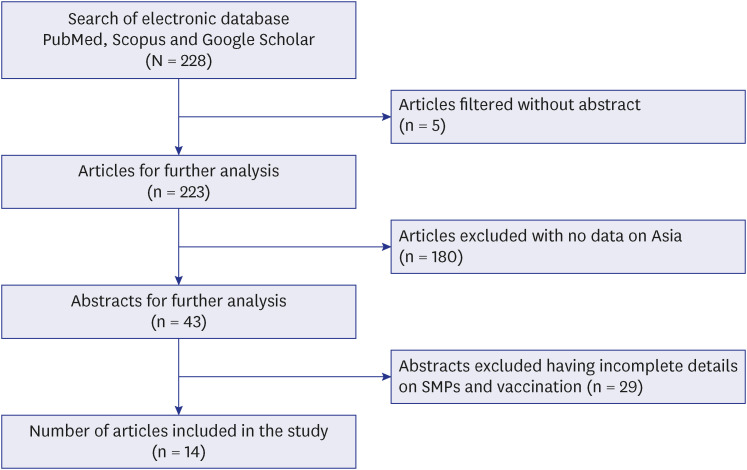
The literature search strategy followed the protocol previously proposed by Gasparyan et al.12 Briefly, we searched PubMed, Scopus, and Google Scholar databases from inception to May 26, 2022, using the following MeSH terms: ‘immunization,’ ‘vaccination,’ ‘vaccine hesitancy,’ ‘social media,’ ‘misinformation,’ and ‘Asia.’ These terms may appear anywhere in the article title or abstract. We searched for articles containing either ‘immunization,’ ‘vaccination,’ or ‘vaccine hesitancy’ AND at least one of the following terms: ‘social media,’ ‘misinformation,’ or ‘Asia.’ Research articles were considered for inclusion to this review, regardless of study design. Exclusion criteria included publications not in English language, publications not involving human subjects, publications with incomplete data, and publications that do not involve people living in Asian countries. Two researchers FR and LG assessed the initial batch of abstracts for their eligibility. Any disagreement were resolved by discussion and consensus between the two researchers. The initial database search identified 228 publications. Five articles had no abstract so they were filtered out. Of the remaining 223 publications, 180 were excluded as they did not have information regarding people living in Asian countries. Twenty-nine publications were further excluded as they had incomplete information. Finally, out of the 228 articles, 14 were included for review. The search strategy is summarized in Fig. 1.
Fig. 1. Search strategy for PubMed, Google Scholar, and Scopus databases. Flowchart representing search strategy utilized to search PubMed, Google Scholar, and Scopus databases.
VACCINE HESITANCY IN ASIA
Vaccine hesitancy, characterized by the reluctance or refusal to receive vaccines, is a significant concern in various regions worldwide, including Asia. However, the underlying factors contributing to vaccine hesitancy in Asia differ from those in other regions due to the region’s unique cultural, historical, political, and economic landscape. In Asia, the presence of traditional medicine and alternative therapies, driven by a cultural preference for natural remedies and skepticism towards modern medicine, contributes to vaccine hesitancy.13 Cultural beliefs and traditions play a substantial role in shaping vaccine resistance in certain Asian countries. Similar to global trends, concerns about the unnatural nature of vaccines and potential side effects contribute to vaccine hesitancy among many individuals in Asia.
Risk perception and vaccination intent during crises are strongly influenced by cultural values.14 In some Asian countries, such as Hong Kong and South Korea, parents express concerns about vaccinating their children against the human papillomavirus (HPV) vaccine, fearing it may condone early sexual initiation.15 The taboo nature of HPV infection in certain Asian countries, particularly where household decision-making is traditionally male-dominated, further contributes to vaccine hesitancy.3 , 16,17,18 Conversely, the tendency towards cultural collectivism in Asian societies can promote intentions to engage in protective behaviors, including vaccination.19 This cultural dichotomy between East and West is evident in SMPs.
A comparison between American Twitter users and Chinese Weibo users revealed that Twitter users were more likely to share personal experiences with vaccines, suggesting cultural differences in vaccine-related narratives. A recent study conducted in Hong Kong on COVID-19 vaccination also found a significant association between vaccine hesitancy and individualistic personal beliefs.20 These findings highlight the role of cultural factors in shaping vaccine attitudes and perceptions in Asian populations.
The perceptions of vaccines in Asia are also influenced by political and economic factors. The region’s political landscape is diverse, encompassing a range of political systems from highly developed democracies to authoritarian regimes. Recent political changes and reforms have further shaped the perceptions of vaccines.21 In Japan, for instance, there has been a long-standing distrust of vaccination programs due to historical events and compulsory vaccination laws imposed by the government in the past.22 This has led to widespread resistance and a general mistrust of the medical establishment.22 In Southeast Asian countries, a multinational study revealed significant mistrust and concerns about the government’s ability to provide adequate and equitable healthcare, resulting in suboptimal access to COVID-19 vaccination.23 Conversely, in authoritarian countries where vaccine mandates are strictly enforced, and an authoritarian mentality is prevalent in society, vaccine hesitancy appears to be low, as there is higher adherence to government policies.14
The economic context and healthcare system of a country also play a role in vaccine access.23 Countries without universal health coverage schemes may face challenges in ensuring vaccine affordability and accessibility, particularly for economically marginalized individuals. The cost of vaccines is a significant factor contributing to vaccine hesitancy in Asia, as it poses a barrier for those who cannot afford them. Overall, political and economic factors shape the perceptions of vaccines in Asia, influencing vaccine hesitancy, trust in healthcare systems, and access to vaccination services.
Vaccine hesitancy is a complex issue with varying factors across countries and communities. To address this challenge and promote vaccine uptake in Asia, it is crucial to understand the distinct cultural, historical, political, and economic factors at play. By recognizing and addressing these unique elements, targeted strategies can be developed to effectively tackle vaccine hesitancy in the region.
SMPs AND THE INFODEMIC DURING COVID-19 PANDEMIC
During the COVID-19 pandemic, SMPs is ground zero for the dissemination of anti-vaccination propaganda which affects the public’s perception of vaccination and consequently the course of the pandemic overall.24 Social media penetration rates in Asia is high. Given the large population, Asia is home to the majority of SMPs in the world. As of January 2022, the highest social media penetration in Asia was seen in the UAE, with an active penetration rate of 106.1% followed by Malaysia, South Korea, and Singapore, with an active penetration of 92%, 91%, and 90%, respectively.11 The most widely used SMP in Asia is Facebook, with 1.28 billion monthly active users in the Asia Pacific, followed by YouTube, Twitter, and Instagram.25 The most widely used social media in China, where other popular platforms have been banned, are Sina Weibo, with 248 million users as of 2021,26 WeChat, Qzone, Douyin, and QQ, among the numerous platforms. Users in Japan use Line as a social platform along with Twitter, Instagram, and Facebook.27
With the increasing accessibility of the internet, more and more people are turning to SMPs to seek health-related information.8 However, during the COVID-19 pandemic, an “infodemic” has emerged, characterized by the overwhelming volume of information, including inaccurate and misleading content, in both digital and physical environments. This infodemic creates chaos and promotes risky behaviors that can undermine public health campaigns, erode trust in health authorities, and hinder the effectiveness of public health responses.28 The freedom to communicate and share information on SMPs also provides a platform for fringe opinions, disinformation, and propaganda.29 One of the contributing factors to this issue is the algorithms employed by SMPs, which selectively present users with content that aligns with their pre-existing views, creating a “filter bubble” or “echo chamber” effect.30 A study analyzing the social dynamics of COVID-19 information on SMPs, based on 8 million comments and posts, found that the interaction patterns on each platform, coupled with user behavior, influenced the spread of information. These patterns can potentially be utilized to develop algorithms that predict factors contributing to the amplification of rumors and misinformation.31
Popular subjects like vaccines, infectious diseases, cancer, and COVID-19 are particularly susceptible to disinformation campaigns.24 Recent studies have shown that SMPs have the ability to shape an individual's thoughts, beliefs, and decision-making process.32 In Western countries, higher levels of active social media usage have been associated with increased negative attitudes towards childhood immunization and COVID-19 vaccination.29,30,32,33 While research on this issue in Asia is limited, it is likely that a similar problem exists due to the high usage of social media in the region and comparatively lower immunization coverage.
During the pandemic, with social distancing measures and lockdowns in place, people turned to online platforms for social interaction and information sharing, moving their personal networks from physical spaces to digital environments.34,35,36 Despite the presence of misinformation, SMPs remained a crucial source of information for researchers and scholars during the crisis.37 This shift in behavior affected both professionals and the general public, influencing their information-seeking behaviors and decision-making processes.37 Healthcare professionals (HCPs) expressing a positive attitude towards immunization on SMPs can play a role in enhancing vaccine acceptability among the general population. Providing HCPs with reliable information and motivating them to share accurate content can help reduce vaccine resistance.10
MISINFORMATION AND COVID-19 VACCINATION UPTAKES IN VARIOUS ASIAN COUNTRIES
Conspiracy theories related to COVID-19 have spread widely on SMPs worldwide. These theories include false claims that COVID-19 is a hoax, an artificially created disease, a result of secret research, or a deliberate scheme by government agencies.38 In some regions of Asia, concerns have also arisen regarding the introduction of nano-chips into individuals’ bodies through vaccines.39,40 Research conducted in Jordan revealed that rumours circulating on SMPs contributed to vaccine hesitancy, with claims such as vaccines being toxic to human DNA or causing infertility.41 Similarly, a study conducted in Punjab, Pakistan, identified propaganda against vaccines on SMPs, alleging that vaccines were part of a plot orchestrated by Western countries, their allies, or secret societies like the Illuminati.42 A study conducted in Hong Kong examined online discussions on a popular forum and found widespread concerns about vaccine safety and potential side effects.43 These instances highlight the influence of SMPs in spreading misinformation and creating apprehensions about COVID-19 vaccines.
A survey conducted in Israel involving 863 participants examined the relationship between the source of information and attitudes towards the COVID-19 vaccine. The study found that individuals who relied on mainstream media, government sources, and institutions for vaccine-related information generally held positive opinions about the benefits of COVID-19 vaccination. However, those who considered SMPs as a credible source of information displayed negative attitudes towards vaccination and expressed low levels of intention to get vaccinated.44 Similarly, in a comprehensive population-based study conducted in Qatar, the prevalence of vaccine resistance was estimated to be approximately 20% and was found to be associated with social media usage.45 These findings highlight the impact of different information sources, including social media, on individuals’ attitudes and intentions towards COVID-19 vaccination.
Vaccine hesitancy for the COVID-19 vaccine was higher in Jordan and Kuwait, compared to other Arab countries.46 A questionnaire-based survey was conducted on 3,414 respondents from middle-eastern and Arab countries. More than 40% of the participants believed that COVID-19 was a man-made disease that purported vaccines upon the masses. Over a quarter of those surveyed believed that vaccination was intended to inject microchips in humans.46 Another quarter of participants believed that COVID-19 caused infertility. A belief in conspiracy theories propagated mainly via SMPs was associated with a lower likelihood of vaccination in this study.46 Similar tendency was also observed in another study from Jordan, where 65% of the respondents belonging to non-medical professions believed in conspiracy theories on the SMPs and were hesitant to receive COVID-19 vaccine.41
In Lebanon, 85% of respondents reported exposure to disinformation or fake news related to COVID-19 and the COVID-19 vaccine. One-third of the participants were dependent on SMPs like WhatsApp (30%), Facebook (38%), and Instagram (40%) as the primary sources of COVID-19 and vaccine-related information.47 The highest-rated source of misinformation was reported as WhatsApp (74%), followed by Facebook or Instagram (61%).47 Trust in SMP-based information was associated with reduced intention to vaccinate, while reliance on official and government-based sources, such as the ministry of health, increased the choice to vaccinate.47 The ARCOVAX study by El Kibbi et al.10 assessed the acceptability of the COVID-19 vaccine among patients suffering chronically from rheumatic diseases and HCPs. It was found that around half of unvaccinated patients would be willing to take the vaccine if recommended by a physician. A third of unvaccinated HCPs were willing to take it if another physician recommended it. This study supported the utility of physicians' recommendation to improve vaccine acceptability.10
A nationally representative study conducted in Russia aimed to investigate the extent of vaccine acceptance and the factors influencing vaccine attitudes among 7,046 participants. The study revealed a higher prevalence of vaccine resistance to the COVID-19 vaccine in Russia compared to other countries, with 43% of respondents expressing hesitancy.48 The study also found that individuals who had lower levels of trust in government institutions were more likely to rely on SMPs for information, which in turn contributed to vaccine hesitancy.
CHALLENGES IN ADMINISTERING NON-COVID-19 IMMUNIZATION
Vaccine hesitancy and resistance were a challenge even in the pre-COVID-19 era. For instance, polio eradication campaigns were met with resistance, and the goal of eliminating polio by 2000 could not be met.49 In addition, claims regarding the Oral polio vaccine (OPV) sterilizing children were widespread on the SMPs.50
Immunization coverage in 2020 has declined in various regions globally,51 with South-East Asian and Eastern Mediterranean regions shows the greatest downward trend.51 The most significant decline in coverage in Asia was reported for the diphtheria tetanus toxoid and pertussis vaccine,52 with zero-dose children in South-East Asia as high as 24% in 2020.52 Asia also lags behind its elimination targets for several VPDs, including measles and maternal and neonatal tetanus.51
Inclination towards SMPs to seek information on vaccines during the COVID-19 pandemic played a significant role in parents' decision-making on children's immunization in countries like Saudi Arabia and Israel.53,54 A study was conducted on 577 caregivers of children aged < 2 years in Saudi Arabia to assess the predictors of delayed vaccine. Searching online for vaccine-related information or taking others' opinions was preferred by only 1% of respondents before the pandemic, but increased to 30% during the pandemic. The use of SMPs was also associated with increased fear of vaccines and increased odds of delayed vaccination by 3–4 times.53 Ashkenazi et al.54 concluded in a study evaluating measles vaccine hesitancy that the vaccination status was significantly associated with the primary source of information used for making decision. About 85% of parents acquiring knowledge from family physicians or paediatricians vaccinated their children, whereas half of the parents whose most trusted source was the internet or SMPs were vaccine hesitant.54
A qualitative study on 252 caregivers in South India evaluated the effect of SMP-based anti-vaccine influencers, including naturopaths and homeopaths, on caregivers’ decision on Immunization.55 Respondents reported being exposed to positive and negative opinions on SMPs like Facebook, YouTube, and WhatsApp, which led to confusion and skepticism towards immunization.55 In 2019, A fake video propagating adverse events of the polio vaccine surfaced on SMPs in Pakistan. Following this campaign, two million children remained unvaccinated in Pakistan, and a surge in vaccine refusals was observed. In the Pakistani city of Nowshera alone, cases rose from 256 in March 2020 to 88,000 in April 2020. This incident highlights how disinformation through SMPs can actively sabotage immunization programs.56
Results from a cross–sectional study conducted on 2,178 caregivers in China showed that increased reliance on SMPs for vaccine-related information lead to higher odds for vaccine hesitancy.57 Similar results were reported from Japan, where parents who trusted SMPs for vaccine-related information were thrice more likely to show no intention to vaccinate their children than parents who trusted validated sources.58 The same study suggested a gender-related tendency towards vaccine hesitancy, with mothers having higher odds of being vaccine-hesitant. Such behaviours were more likely prevalent in mothers with lower satisfaction with social relationships. A possible explanation for this behavior was that women with limited social relationships during the pandemic spent more time on the SMPs, which had become primary source of information for them.58 There were similar findings from a study conducted on 2,875 participants in Mongolia.59 Most participants in the Mongolian study who relied on official sources for vaccine-related information showed a higher intention to vaccinate, in contrast to participants acquiring knowledge from SMPs who showed less willingness to vaccinate,59 In another example, a study conducted on 360 women in Korea evaluating barriers to the HPV vaccine found that SMPs negatively influenced decisions regarding vaccine uptake.60
In a study based on survey data from the USA and China, information obtained through SMPs was more likely to negatively influence the intention to vaccinate in American women compared to Chinese women.61 At the same time, adherence to social norms in the latter was strongly associated with preferences to receive the vaccine, suggesting a stronger sense of collectivism in China. Countries in Asia that emphasizes societal collectivism tend to be more sensitive to fellow social media users’ approval or disapproval to avoid feeling alienated from their community.61 Following the Chinese government’s launch of rumor-refuting websites, rectification campaigns, and stringent policies against spreading misinformation on SMPs, a pro-vaccine stance culminated among Chinese nurses.61
Table 144,45,46,47,48,53,58,59,62 and Table 254,55,56,60,61 summarized studies of impacts of SMPs on uptakes of COVID-19 vaccine and non-COVID-19 vaccines, respectively.
Table 1. Summary of the studies on the impact of SMPs on COVID-19 vaccination uptake.
| No. | Region | Study population | Author | No. of participants | Results |
|---|---|---|---|---|---|
| 1 | Saudi Arabia | Primary caregivers of children up to 2 years of age in Saudi Arabia. | Baghdadi et al.53 | 577 | While most mothers sought information from trustworthy sources before the pandemic, there was a significant increase in SMPs usage for such information during the pandemic. |
| 2 | Russia | Population above 18 years of age. Data drawn from the Russian longitudinal monitoring survey | Roshchina et al.48 | 7,046 | Only 45% of the Russian population demonstrated positive attitudes toward the COVID-19 vaccination. |
| 3 | Israel | Israeli population between ages 18 to 55 years. | Zimand-Sheiner et al.44 | 863 | Results show that trust in SMPs trust generates negative attitude toward vaccine, whereas trust in mass media and official generate positive attitudes. |
| 4 | Jordan, Kuwait | Residents above 16 years of age in Jordan and other Arab Countries. | Sallam et al.46 | 3,414 | A reliance on social media as the primary source of information about COVID-19 vaccines was associated with vaccine hesitancy. |
| 5 | Qatar | Alabdulla et al.45 | 7,821 | This study reports an overall vaccine hesitancy of 20% toward the COVID-19 vaccine and the influence of social media on attitudes toward vaccination which is in keeping with emerging evidence. | |
| 6 | Lebanon | A random sample of population above 18 years of age. | Ghaddar et al.47 | 1,052 | Trust in specific information sources (WHO, MoPH, and TV) increased, while confidence in information from SMPs reduced vaccination intent against COVID-19. |
| 7 | Japan | Parents residing in Japan with children aged 3 to 14 years. | Horiuchi et al.58 | 1,200 | SMPs as the most trusted information source increased vaccine hesitancy in parents compared to those who trusted official information. |
| 8 | Mongolia | Population above 18 years of age in different districts of Mongolia. | Dambadarjaa et al.59 | 2,875 | Receiving COVID-19 vaccine information from official government pages was related to a higher acceptance rate. Reliance on social media as a source of COVID-19 vaccine information was associated with high vaccine hesitancy. |
| 9 | China | Healthcare workers from 2 participating hospitals in China | Xin et al.62 | 1,902 | Frequent social media exposure and interpersonal discussion potentially enhanced vaccination intentions via increased perceived vaccine efficacy. |
SMP = social media platform, COVID-19 = coronavirus disease 2019, WHO = World Health Organization, MoPH = Ministry of Public Health.
Table 2. Summary of the studies on the impact of SMPs on uptakes of non-COVID-19 vaccines.
| No. | Region | Study population | Author | No. of participants | Results |
|---|---|---|---|---|---|
| 1 | Israel | Parents in Israel with at least one child older than two years of age with no chronic illness and no history of measles. | Ashkenazi et al.54 | 399 | Internet and SMPs were the primary sources of information for one-third of respondents regarding measles/measles vaccine and half the respondents regarding the measles outbreak; SMPs were negatively associated with the correct knowledge. |
| 2 | Pakistan | - | Ittefaq et al.56 | - | Pakistan’s polio eradication program faces many challenges; propaganda campaigns on SMPs resulted in an upsurge in the active number of new polio cases. |
| 3 | India | In-depth interviews with doctors of different disciplines, religious teachers, Communication experts, and focused discussion groups with caregivers in Kerala. | Nair et al.55 | 252 | Anti-vaxxers use SMPs to influence caregivers' perceptions and beliefs. |
| 4 | Korea | Undergraduate college students in Seoul, unvaccinated for the HPV vaccine. | Kim60 | 323 | Multiple dimensions of perceived barriers showed differing impacts on vaccine acceptance. While the internet effectively reduced social barriers, SMPs harmed the intent to vaccinate. |
| 5 | China and the United States | Female participants above 18 years of age from China or the United States, unvaccinated for the HPV vaccine. | Pan et al.61 | 387 | The results show that exposure to contradictory information on social media had a more significant negative association with intentions to receive HPV vaccination among the United States participants than among the Chinese participants. |
SMP = social media platform, COVID-19 = coronavirus disease 2019, HPV = human papillomavirus.
Politics have influenced the uptake of vaccines across the globe directly or indirectly. For instance, the anti-vaccination movement that followed a research paper claiming an association between the measles mumps and rubella vaccines and autism was aggravated by supportive tweets from the former US president during the election campaign.63,64 This move led to increased hesitancy, distrust against the vaccine, and strengthened belief in conspiracy theories.
A CONSTRUCTIVE APPROACH TOWARDS SMPs FOR IMMUNIZATION
The SMPs offer two-way communication with target groups and individuals, increasing the availability, accessibility, and provision of a platform for low-cost and highly efficient vaccination policy advocacy opportunities.65 While the misinformation on the SMPs may negatively influence immunization campaigns, they also provide infinite opportunities to support public health initiatives with credible information like the Arab Adult Arthritis Awareness campaign on Facebook, Instagram and Twitter.66 They have the potential to become health promotion tools and encourage constructive practices.67 SMPs can be utilized to provide convincing details and generate healthy discussions to improve vaccine confidence and dispel uncertainty among caregivers effectively.55 In collaboration with interactive websites, SMPs outperform conventional care in improving vaccine acceptability.68 Policymakers can utilize SMPs to enhance vaccine uptake in Asia and around the globe. Accessibility to credible sources like the WHO website, Centers for Disease Control and Prevention’s vaccine and immunization web content, vaccine information statements, and the official healthcare departments in individual countries, should be improved when consulting a health expert becomes unfeasible.
LIMITATIONS
While we made an effort to include as many publications from Asia as possible, we fully acknowledge potential limitations of this review. Asia’s vast and diverse nature means that some populations may not have been covered by our search. Additionally, limiting our search to English language articles and omitting reputable databases like Web of Science and Embase could add further limitations. Some resource-limited countries might not have been included due to the absence of relevant studies in their populations.
Furthermore, it is essential to acknowledge that the landscape of SMPs is constantly evolving, and observations from a specific time period may not be applicable today. To deepen our understanding of how SMPs influence health decisions, a more comprehensive search strategy and regular monitoring are necessary. Encouraging greater participation from the research community will further this endeavor, ensuring that Asian individuals and healthcare providers can make well-informed decisions regarding vaccination.
CONCLUSION
The negative impact of SMPs on vaccine intent is evident in most Asian countries, although research on this topic is lacking in Central Asia. It is crucial to counter disinformation campaigns by reducing political interference and empowering health experts to promote global health effectively. Restoring trust in science and health experts is vital for strengthening global immunization efforts. Ensuring access to accurate information and leveraging the potential of reliable SMPs can greatly enhance immunization campaigns in Asia and worldwide. Further research is needed to investigate the influence of SMPs on immunization campaigns in countries with low vaccination intent. Vaccine resistance, influenced by SMP usage, remains a significant challenge across all regions of Asia.
Footnotes
Disclosure: The authors have no potential conflicts of interest to disclose.
- Conceptualisation: Rodrigues F, Jatuworapruk K, Gupta L.
- Data collection: Rodrigues F, Jatuworapruk K, Gupta L.
- Formal analysis: Rodrigues F, Ziade N, Jatuworapruk K, Caballero-Uribe CV.
- Visualization: Rodrigues F, Gupta L.
- Writing - original draft: Rodrigues F, Jatuworapruk K, Gupta L.
- Writing - review & editing: Rodrigues F, Ziade N, Jatuworapruk K, Caballero-Uribe CV, <underline>Khursheed T, </underline>Gupta L.
References
- 1.World Health Organization. Ten health issues WHO will tackle this year. [Accessed December 13, 2022]. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 .
- 2.Paules CI, Marston HD, Fauci AS. Measles in 2019 - going backward. N Engl J Med. 2019;380(23):2185–2187. doi: 10.1056/NEJMp1905099. [DOI] [PubMed] [Google Scholar]
- 3.Wong LP, Wong PF, AbuBakar S. Vaccine hesitancy and the resurgence of vaccine preventable diseases: the way forward for Malaysia, a Southeast Asian country. Hum Vaccin Immunother. 2020;16(7):1511–1520. doi: 10.1080/21645515.2019.1706935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sen P, Lilleker JB, Agarwal V, Kardes S, Milchert M, Gheita T, et al. Vaccine hesitancy in patients with autoimmune diseases: data from the coronavirus disease-2019 vaccination in autoimmune diseases study. Indian J Rheumatol. 2022;17(2):188–191. [Google Scholar]
- 5.World Health Organization. Immunization coverage. [Accessed December 13, 2022]. https://www.who.int/news-room/fact-sheets/detail/immunization-coverage .
- 6.Harris KM, Maurer J, Kellermann AL. Influenza vaccine--safe, effective, and mistrusted. N Engl J Med. 2010;363(23):2183–2185. doi: 10.1056/NEJMp1012333. [DOI] [PubMed] [Google Scholar]
- 7.Horne Z, Powell D, Hummel JE, Holyoak KJ. Countering antivaccination attitudes. Proc Natl Acad Sci U S A. 2015;112(33):10321–10324. doi: 10.1073/pnas.1504019112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hornsey MJ, Harris EA, Fielding KS. The psychological roots of anti-vaccination attitudes: a 24-nation investigation. Health Psychol. 2018;37(4):307–315. doi: 10.1037/hea0000586. [DOI] [PubMed] [Google Scholar]
- 9.Eberwein JD, Edochie I, Newhouse D, Cojocaru A, Deudibe G, Kakietek J, et al. COVID-19 Vaccine Hesitancy in 53 Developing Countries: Levels, Trends, and Reasons for Hesitancy. Washington, D.C., USA: World Bank; 2022. [Google Scholar]
- 10.El Kibbi L, Metawee M, Hmamouchi I, Abdulateef N, Halabi H, Eissa M, et al. Acceptability of the COVID-19 vaccine among patients with chronic rheumatic diseases and health-care professionals: a cross-sectional study in 19 Arab countries. Lancet Rheumatol. 2022;4(3):e160–e163. doi: 10.1016/S2665-9913(21)00368-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Statista. Social networks: penetration in selected countries 2022. [Accessed December 13, 2022]. https://www.statista.com/statistics/282846/regular-social-networking-usage-penetration-worldwide-by-country/
- 12.Gasparyan AY, Ayvazyan L, Blackmore H, Kitas GD. Writing a narrative biomedical review: considerations for authors, peer reviewers, and editors. Rheumatol Int. 2011;31(11):1409–1417. doi: 10.1007/s00296-011-1999-3. [DOI] [PubMed] [Google Scholar]
- 13.Hill J, Seguin R, Phanga T, Manda A, Chikasema M, Gopal S, et al. Facilitators and barriers to traditional medicine use among cancer patients in Malawi. PLoS One. 2019;14(10):e0223853. doi: 10.1371/journal.pone.0223853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lin F, Chen X, Cheng EW. Contextualized impacts of an infodemic on vaccine hesitancy: the moderating role of socioeconomic and cultural factors. Inf Process Manage. 2022;59(5):103013. doi: 10.1016/j.ipm.2022.103013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wong LP, Wong PF, Megat Hashim MM, Han L, Lin Y, Hu Z, et al. Multidimensional social and cultural norms influencing HPV vaccine hesitancy in Asia. Hum Vaccin Immunother. 2020;16(7):1611–1622. doi: 10.1080/21645515.2020.1756670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hussain S, Bharadwaj M, Nasare V, Kumari M, Sharma S, Hedau S, et al. Human papillomavirus infection among young adolescents in India: impact of vaccination. J Med Virol. 2012;84(2):298–305. doi: 10.1002/jmv.22261. [DOI] [PubMed] [Google Scholar]
- 17.Carnegie E, Whittaker A, Gray Brunton C, Hogg R, Kennedy C, Hilton S, et al. Development of a cross-cultural HPV community engagement model within Scotland. Health Educ J. 2017;76(4):398–410. doi: 10.1177/0017896916685592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ladner J, Besson MH, Audureau E, Rodrigues M, Saba J. Experiences and lessons learned from 29 HPV vaccination programs implemented in 19 low and middle-income countries, 2009-2014. BMC Health Serv Res. 2016;16(1):575. doi: 10.1186/s12913-016-1824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Castle C, Di Guilmi, C, Stavrunova O. Individualism and Collectivism as Predictors of Compliance with COVID-19 Public Health Safety Expectations. Ultimo, Australia: University of Technology Sydney; 2021. [Google Scholar]
- 20.Yu Y, Lau MM, Lau JT. Positive association between individualism and vaccination resistance against Covid-19 vaccination among Chinese adults: mediations via perceived personal and societal benefits. Vaccines (Basel) 2021;9(11):1225. doi: 10.3390/vaccines9111225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wikipedia. Politics of Asia. [Updated 2023]. [Accessed March 17, 2023]. https://en.wikipedia.org/w/index.php?title=Politics_of_Asia&oldid=1132990077 .
- 22.Nakayama T. Vaccine chronicle in Japan. J Infect Chemother. 2013;19(5):787–798. doi: 10.1007/s10156-013-0641-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Marzo RR, Sami W, Alam MZ, Acharya S, Jermsittiparsert K, Songwathana K, et al. Hesitancy in COVID-19 vaccine uptake and its associated factors among the general adult population: a cross-sectional study in six Southeast Asian countries. Trop Med Health. 2022;50(1):4. doi: 10.1186/s41182-021-00393-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fajardo E. COVID-19, a pandemic accompanied by infodemia. Glob Rheumatol. 2020;1(Jun-Dec):1–28. [Google Scholar]
- 25.StatCounter Global Stats. Social media stats Asia. [Accessed December 13, 2022]. https://gs.statcounter.com/social-media-stats/all/asia .
- 26.Statista. Weibo Corporation: DAUs 2022. [Accessed December 13, 2022]. https://www.statista.com/statistics/1058070/china-sina-weibo-dau/
- 27.Gaur PS, Gupta L. Social media for scholarly communication in central Asia and its neighbouring countries. J Korean Med Sci. 2021;36(4):e36. doi: 10.3346/jkms.2021.36.e36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization. Infodemic. [Accessed December 13, 2022]. https://www.who.int/health-topics/infodemic .
- 29.Wilson SL, Wiysonge C. Social media and vaccine hesitancy. BMJ Glob Health. 2020;5(10):e004206. doi: 10.1136/bmjgh-2020-004206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Puri N, Coomes EA, Haghbayan H, Gunaratne K. Social media and vaccine hesitancy: new updates for the era of COVID-19 and globalized infectious diseases. Hum Vaccin Immunother. 2020;16(11):2586–2593. doi: 10.1080/21645515.2020.1780846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cinelli M, Quattrociocchi W, Galeazzi A, Valensise CM, Brugnoli E, Schmidt AL, et al. The COVID-19 social media infodemic. Sci Rep. 2020;10:16598. doi: 10.1038/s41598-020-73510-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Power DJ, Phillips-Wren G. Impact of social media and Web 2.0 on decision-making. J Decis Syst. 2011;20(3):249–261. [Google Scholar]
- 33.Kouzy R, Abi Jaoude J, Kraitem A, Kraitem MB, Karam B, Adib E, et al. Coronavirus goes viral: quantifying the COVID-19 misinformation epidemic on Twitter. Cureus. 2020;12(3):e7255. doi: 10.7759/cureus.7255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Argyris YA, Kim Y, Roscizewski A, Song W. The mediating role of vaccine hesitancy between maternal engagement with anti- and pro-vaccine social media posts and adolescent HPV-vaccine uptake rates in the US: the perspective of loss aversion in emotion-laden decision circumstances. Soc Sci Med. 2021;282:114043. doi: 10.1016/j.socscimed.2021.114043. [DOI] [PubMed] [Google Scholar]
- 35.Southwell BG, Yzer MC. The roles of interpersonal communication in mass media campaigns. Ann Int Commun Assoc. 2007;31(1):420–462. [Google Scholar]
- 36.Ludolph R, Schulz PJ, Chen L. Investigating the effects of mass media exposure on the uptake of preventive measures by Hong Kong residents during the 2015 MERS outbreak: the mediating role of interpersonal communication and the perception of concern. J Health Commun. 2018;23(1):1–8. doi: 10.1080/10810730.2017.1388455. [DOI] [PubMed] [Google Scholar]
- 37.Jang K, Baek YM. When information from public health officials is untrustworthy: the use of online news, interpersonal networks, and social media during the MERS outbreak in South Korea. Health Commun. 2019;34(9):991–998. doi: 10.1080/10410236.2018.1449552. [DOI] [PubMed] [Google Scholar]
- 38.Gupta L, Gasparyan AY, Misra DP, Agarwal V, Zimba O, Yessirkepov M. Information and misinformation on COVID-19: a cross-sectional survey study. J Korean Med Sci. 2020;35(27):e256. doi: 10.3346/jkms.2020.35.e256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Khan YH, Mallhi TH, Alotaibi NH, Alzarea AI, Alanazi AS, Tanveer N, et al. Threat of COVID-19 vaccine hesitancy in Pakistan: the need for measures to neutralize misleading narratives. Am J Trop Med Hyg. 2020;103(2):603–604. doi: 10.4269/ajtmh.20-0654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chaudhary FA, Ahmad B, Khalid MD, Fazal A, Javaid MM, Butt DQ. Factors influencing COVID-19 vaccine hesitancy and acceptance among the Pakistani population. Hum Vaccin Immunother. 2021;17(10):3365–3370. doi: 10.1080/21645515.2021.1944743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Aloweidi A, Bsisu I, Suleiman A, Abu-Halaweh S, Almustafa M, Aqel M, et al. Hesitancy towards COVID-19 vaccines: an analytical cross-sectional study. Int J Environ Res Public Health. 2021;18(10):5111. doi: 10.3390/ijerph18105111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zakar R, Momina AU, Shahzad S, Hayee M, Shahzad R, Zakar MZ. COVID-19 vaccination hesitancy or acceptance and its associated factors: findings from post-vaccination cross-sectional survey from Punjab Pakistan. Int J Environ Res Public Health. 2022;19(3):1305. doi: 10.3390/ijerph19031305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Leung CH. A study on vaccination hesitancy caused by misinformation in Hong Kong. Int J Publ Soc Stud. 2022;7(1):19–27. [Google Scholar]
- 44.Zimand-Sheiner D, Kol O, Frydman S, Levy S. To be (vaccinated) or not to be: the effect of media exposure, institutional trust, and incentives on attitudes toward COVID-19 vaccination. Int J Environ Res Public Health. 2021;18(24):12894. doi: 10.3390/ijerph182412894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Alabdulla M, Reagu SM, Al-Khal A, Elzain M, Jones RM. COVID-19 vaccine hesitancy and attitudes in Qatar: a national cross-sectional survey of a migrant-majority population. Influenza Other Respi Viruses. 2021;15(3):361–370. doi: 10.1111/irv.12847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Sallam M, Dababseh D, Eid H, Al-Mahzoum K, Al-Haidar A, Taim D, et al. High rates of COVID-19 vaccine hesitancy and its association with conspiracy beliefs: a study in Jordan and Kuwait among other Arab countries. Vaccines (Basel) 2021;9(1):42. doi: 10.3390/vaccines9010042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Ghaddar A, Khandaqji S, Awad Z, Kansoun R. Conspiracy beliefs and vaccination intent for COVID-19 in an infodemic. PLoS One. 2022;17(1):e0261559. doi: 10.1371/journal.pone.0261559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Roshchina Y, Roshchin S, Rozhkova K. Determinants of COVID-19 vaccine hesitancy and resistance in Russia. Vaccine. 2022;40(39):5739–5747. doi: 10.1016/j.vaccine.2022.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.M A S. Emerging challenges to realizing global polio eradication and their solutions. East Mediterr Health J. 2022;28(7):515–520. doi: 10.26719/emhj.22.045. [DOI] [PubMed] [Google Scholar]
- 50.Gesser-Edelsburg A, Diamant A, Hijazi R, Mesch GS. Correcting misinformation by health organizations during measles outbreaks: a controlled experiment. PLoS One. 2018;13(12):e0209505. doi: 10.1371/journal.pone.0209505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.United Nations International Children’s Emergency Fund. Immunisation. [Accessed December 13, 2022]. https://www.unicef.org/rosa/what-we-do/health/immunisation .
- 52.Muhoza P, Danovaro-Holliday MC, Diallo MS, Murphy P, Sodha SV, Requejo JH, et al. Routine vaccination coverage - worldwide, 2020. MMWR Morb Mortal Wkly Rep. 2021;70(43):1495–1500. doi: 10.15585/mmwr.mm7043a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Baghdadi LR, Hassounah MM, Younis A, Al Suwaidan HI, Al Khalifah R. Caregivers’ sources of information about immunization as predictors of delayed childhood vaccinations in Saudi Arabia during the COVID-19 pandemic: a cross-sectional questionnaire study. Risk Manag Healthc Policy. 2021;14:3541–3550. doi: 10.2147/RMHP.S312148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ashkenazi S, Livni G, Klein A, Kremer N, Havlin A, Berkowitz O. The relationship between parental source of information and knowledge about measles / measles vaccine and vaccine hesitancy. Vaccine. 2020;38(46):7292–7298. doi: 10.1016/j.vaccine.2020.09.044. [DOI] [PubMed] [Google Scholar]
- 55.Nair AT, Nayar KR, Koya SF, Abraham M, Lordson J, Grace C, et al. Social media, vaccine hesitancy and trust deficit in immunization programs: a qualitative enquiry in Malappuram District of Kerala, India. Health Res Policy Syst. 2021;19(Suppl 2):56. doi: 10.1186/s12961-021-00698-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ittefaq M, Abwao M, Rafique S. Polio vaccine misinformation on social media: turning point in the fight against polio eradication in Pakistan. Hum Vaccin Immunother. 2021;17(8):2575–2577. doi: 10.1080/21645515.2021.1894897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Du F, Chantler T, Francis MR, Sun FY, Zhang X, Han K, et al. Access to vaccination information and confidence/hesitancy towards childhood vaccination: a cross-sectional survey in China. Vaccines (Basel) 2021;9(3):201. doi: 10.3390/vaccines9030201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Horiuchi S, Sakamoto H, Abe SK, Shinohara R, Kushima M, Otawa S, et al. Factors of parental COVID-19 vaccine hesitancy: a cross sectional study in Japan. PLoS One. 2021;16(12):e0261121. doi: 10.1371/journal.pone.0261121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Dambadarjaa D, Altankhuyag GE, Chandaga U, Khuyag SO, Batkhorol B, Khaidav N, et al. Factors associated with COVID-19 vaccine hesitancy in Mongolia: a web-based cross-sectional survey. Int J Environ Res Public Health. 2021;18(24):12903. doi: 10.3390/ijerph182412903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kim J. The relationship of health beliefs with information sources and HPV vaccine acceptance among young adults in Korea. Int J Environ Res Public Health. 2018;15(4):673. doi: 10.3390/ijerph15040673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Pan S, Zhang D, Zhang J. Caught in the crossfire: how contradictory information and norms on social media influence young women's intentions to receive HPV vaccination in the United States and China. Front Psychol. 2020;11:548365. doi: 10.3389/fpsyg.2020.548365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Xin M, Luo S, She R, Chen X, Li L, Li L, et al. The impact of social media exposure and interpersonal discussion on intention of COVID-19 vaccination among nurses. Vaccines (Basel) 2021;9(10):1204. doi: 10.3390/vaccines9101204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Khan H, Gasparyan AY, Gupta L. Lessons learned from publicizing and retracting an erroneous hypothesis on the mumps, measles, rubella (MMR) vaccination with unethical implications. J Korean Med Sci. 2021;36(19):e126. doi: 10.3346/jkms.2021.36.e126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Albrecht D. Vaccination, politics and COVID-19 impacts. BMC Public Health. 2022;22(1):96. doi: 10.1186/s12889-021-12432-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.European Centre for Disease Prevention and Control. Systematic scoping review on social media monitoring methods and interventions relating to vaccine hesitancy. [Accessed December 13, 2022]. https://www.ecdc.europa.eu/en/publications-data/systematic-scoping-review-social-media-monitoring-methods-and-interventions .
- 66.Arab Adult Arthritis Awareness Group. [Accessed March 17, 2023]. https://www.arabrheumatology.org/aaaa-group .
- 67.Korda H, Itani Z. Harnessing social media for health promotion and behavior change. Health Promot Pract. 2013;14(1):15–23. doi: 10.1177/1524839911405850. [DOI] [PubMed] [Google Scholar]
- 68.Daley MF, Narwaney KJ, Shoup JA, Wagner NM, Glanz JM. Addressing parents’ vaccine concerns: a randomized trial of a social media intervention. Am J Prev Med. 2018;55(1):44–54. doi: 10.1016/j.amepre.2018.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]